Ling et al. identify human hepatocyte growth factor (hHGFR) as a novel receptor/coreceptor necessary for AAV3 entry into liver-specific cells. Using a variety of methods, the authors show that interference with the cell surface expression of HGFR significantly reduces the transduction efficiency of AAV3 vectors. Subsequent in vitro and in vivo experiments revealed that AAV3 specifically utilizes human HGFR (hHGFR), and not mouse HGFR (mHGFR).
Abstract
Adeno-associated viruses (AAVs) use a variety of cellular receptors/coreceptors to gain entry into cells. A number of AAV serotypes are now available, and the cognate receptors/coreceptors for only a handful of those have been identified thus far. Of the 10 commonly used AAV serotypes, AAV3 is by far the least efficient in transducing cells in general. However, in our more recent studies, we observed that AAV3 vectors transduced human liver cancer cells remarkably well, which led to the hypothesis that AAV3 uses hepatocyte growth factor receptor (HGFR) as a cellular coreceptor for viral entry. AAV3 infection of human liver cancer cell lines was strongly inhibited by hepatocyte growth factor, HGFR-specific small interfering RNA, and anti-HGFR antibody, which corroborated this hypothesis. However, AAV3 vectors failed to transduce murine hepatocytes, both in vitro and in vivo, suggesting that AAV3 specifically uses human HGFR, but not murine HGFR, as a cellular coreceptor for transduction. AAV3 may prove to be a useful vector for targeting human liver cancers for the potential gene therapy.
Introduction
Recombinant vectors based on a nonpathogenic human parvovirus, adeno-associated virus 2 (AAV2), have been developed and are currently in use in a number of gene therapy clinical trials (Daya and Berns, 2008). More recently, a number of additional AAV serotypes have also been isolated (Muramatsu et al., 1996; Chiorini et al., 1997, 1999; Rutledge et al., 1998; Gao et al., 2002, 2004), which have been shown to exhibit selective tissue tropism in various small and large animal models (Zincarelli et al., 2008). Whereas a number of cellular receptors/coreceptors have been identified for AAV2 (Summerford and Samulski, 1998; Qing et al., 1999; Summerford et al., 1999; Kashiwakura et al., 2005; Asokan et al., 2006), only a handful of receptors/coreceptors for other AAV serotypes have been described (Kaludov et al., 2001; Walters et al., 2001; Di Pasquale et al., 2003; Akache et al., 2006; Wu et al., 2006).
We reported that of the 10 commonly used serotypes, AAV3 vectors were by far the most efficient in transducing established human hepatoblastoma (HB) and human hepatocellular carcinoma (HCC) cell lines as well as primary human hepatocytes (Glushakova et al., 2009). Although transduction by AAV3 serotype vectors has been reported to be inhibited by heparin, heparan sulfate, and fibroblast growth factor receptor-1 (FGFR1) (Rabinowitz et al., 2004; Blackburn et al., 2006), the true identity of a cellular receptor/coreceptor remains unclear. Because HB and HCC cells express elevated levels of hepatocyte growth factor receptor (HGFR) (Grigioni et al., 1995; Okano et al., 1999), we hypothesized that AAV3 uses HGFR as a possible receptor/coreceptor for entry into liver-specific cells. In this brief report, using a variety of methods, we document that interference with the cell surface presence or expression of HGFR significantly reduces the transduction efficiency of AAV3 vectors. Furthermore, both in vitro and in vivo data suggest that AAV3 specifically uses human HGFR (hHGFR), and not mouse HGFR (mHGFR), as a cellular coreceptor to gain entry into cells.
Materials and Methods
Cell lines and cultures
Human cervical cancer (HeLa) and hepatocellular carcinoma (Huh7), and murine adult hepatocyte (H2.35) cell lines were purchased from the American Type Culture Collection (Manassas, VA) and maintained in complete Dulbecco's modified Eagle's medium (DMEM; Mediatech, Manassas, VA) supplemented with 10% heat-inactivated fetal bovine serum (FBS; Sigma-Aldrich, St. Louis, MO) and 1% penicillin and streptomycin (P/S; Lonza, Walkersville, MD). A newly established human hepatoblastoma (Hep293TT) cell line was generously provided by G.E. Tomlinson (University of Texas Health Science Center at San Antonio, San Antonio, TX) and was maintained in complete RPMI medium 1640 (Invitrogen, Carlsbad, CA) supplemented with 15% heat-inactivated FBS (Sigma-Aldrich) and 1% P/S (Lonza). Cells were grown as adherent cultures in a humidified atmosphere at 37°C in 5% CO2 and were subcultured after treatment with trypsin–Versene mixture (Lonza) for 2–5 min at room temperature, washed, and resuspended in complete medium.
Recombinant AAV vectors
Highly purified stocks of self-complementary AAV2 (scAAV2) and scAAV3 vectors carrying the enhanced green fluorescence protein (EGFP) gene driven by the chicken β-actin promoter were packaged by the calcium phosphate triple-plasmid transfection protocol described previously (Auricchio et al., 2001; Wu et al., 2007). Physical particle titers of recombinant vector stocks were determined by quantitative DNA slot-blot analyses (Kube and Srivastava, 1997).
AAV vector transduction in vitro
Huh7 or HeLa cells were seeded in 96-well plates at a concentration of 5000 cells per well in complete DMEM. AAV infections were performed in serum- and antibiotic-free DMEM. Hep293TT cells were seeded in 96-well plates at a concentration of 10,000 cells per well in complete RPMI medium. Infections were performed in serum- and antibiotic-free RPMI medium. Expression of EGFP was analyzed either by flow cytometry or by direct fluorescence imaging 72 hr after transduction.
Animal handling
All animal experiments were performed according to the guidelines for animal care specified by the Animal Care Services at the University of Florida (Gainesville, FL). Ten-week-old C57BL/6J male mice were purchased from Jackson Laboratory (Bar Harbor, ME) and maintained at the University of Florida College of Medicine (Gainesville, FL). The Institutional Animal Care and Use Committee approved all protocols for the care and use of these mice.
Recombinant AAV vector transduction in vivo
scAAV-EGFP vectors were injected intravenously via the tail vein into C57BL/6 mice at 1 × 1010 vector genomes (VG) per animal. Phosphate-buffered saline (PBS)-injected mice were used as an appropriate control. Livers were harvested from mice 8 weeks after vector administration, and thin sections from each hepatic lobes were mounted on slides and visualized by fluorescence microscopy. Four representative sections of each lobe were examined to determine transduction efficiency, using National Institutes of Health (NIH, Bethesda, MD) ImageJ software.
Statistical analysis
Results are presented as means ± standard deviation (SD). Differences between groups were identified by Student t test, using a grouped-unpaired two-tailed distribution. p < 0.05 was considered statistically significant.
Results
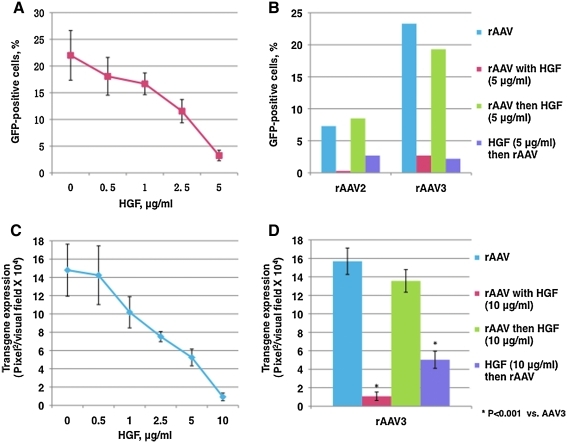
AAV3 infection is strongly inhibited by HGF
To test our hypothesis that AAV3 uses hepatocyte growth factor receptor (HGFR) as a putative cellular coreceptor, we evaluated the effect of hepatocyte growth factor (HGF), the ligand for HGFR, on AAV3 transduction. Huh7, a human hepatocellular carcinoma (HCC) cell line, was transduced with self-complementary (sc) AAV3-EGFP vectors in the absence or presence of increasing concentrations of HGF (Invitrogen) at 37°C for 2 hr and then rinsed twice with PBS. Transgene expression was analyzed by flow cytometry 72 hr posttransduction. These results, shown in Fig. 1A, indicate that HGF reduced scAAV3 vector-mediated transgene expression in a dose-dependent manner. HGF concentration as low as 5 μg/ml resulted in greater than 85% inhibition. Next, to rule out any possible nonspecific nature of this inhibition, preincubation and postincubation studies were performed as follows. Huh7 cells were first incubated with HGF (5 μg/ml) at 37°C for 2 hr, washed extensively, and then infected with scAAV3-EGFP vectors, or cells were first infected with scAAV3-EGFP vectors, washed extensively, and then incubated with HGF (5 μg/ml) at 37°C for 2 hr. scAAV2-EGFP vectors were also included as appropriate controls because HGFR has previously been shown to be a coreceptor for AAV2 (Kashiwakura et al., 2005). These results, shown in Fig. 1B, indicate that AAV3 vectors transduce Huh7 cells more efficiently than AAV2 vectors, which is consistent with our previously published studies (Glushakova et al., 2009). Whereas preincubation with HGF led to significant inhibition of transduction by both AAV2 and AAV3 vectors, postincubation with HGF had no significant effect. These data suggest that AAV3 interacts directly with HGFR, and that HGF inhibits an early event in viral infection.
FIG. 1.
(A) AAV3 vector-mediated transgene expression in Huh7 cells in the presence of various concentrations of HGF. Cells were transduced with vector at 1 × 104 VG/cell, and EGFP-positive cells were enumerated 72 hr posttransduction. (B) Effect of pre- and postincubation of Huh7 cells with HGF (5 μg/ml) on the transduction efficiency of AAV2 and AAV3 serotype vectors. (C) AAV3 vector-mediated transgene expression in Hep293TT cells in the presence of various concentrations of HGF. Cells were transduced with vector at 2 × 103 VG/cell, and EGFP-positive cells were enumerated 72 hr posttransduction. (D) Effect of pre- and postincubation of Hep293TT cells with HGF (10 μg/ml) on the transduction efficiency of and AAV3 serotype vectors.
In addition to Huh7 cells, which were established nearly 30 years ago (Nakabayashi et al., 1982), we wished to investigate whether AAV3 vectors could also transduce human liver cancer cells that were established more recently from primary tumor tissue, to rule out any tissue culture artifact. For this purpose, Hep293TT, a recently established cell line resected from a child with an aggressive hepatoblastoma (HB) (Chen et al., 2009; Glushakova et al., 2009), was transduced with scAAV3-EGFP vectors in the absence or presence of increasing concentrations of HGF as described previously. Seventy-two hours postinfection, the transduction efficiency of AAV3 was measured by GFP imaging, using a fluorescence microscope (DMI 4000E; Leica Microsystems, Wetzlar, Germany). Images from three wells of vector-infected cells were analyzed quantitatively with ImageJ analysis software (NIH). Transgene expression was assessed as total area of green fluorescence (pixel2) per visual field. These results, shown in Fig. 1C, indicate that AAV3 vectors transduced Hep293TT as efficiently as Huh7 cells, and that this transduction was strongly inhibited by coincubation with HGF. Consistent with results obtained with Huh7 cells, incubation of Hep293TT cells with HGF postinfection by AAV3 vectors had little effect on transduction efficiency (Fig. 1D).
HGFR small interfering RNA and HGFR antibody also strongly inhibit transduction by AAV3 vectors
We next used HGFR-specific small interfering RNA (siRNA) to knock down HGFR expression, and evaluated the impact on AAV3 vector-mediated transduction in Huh7 cells. The expression of HGFR after transfection with 10 pmol of negative control siRNA or HGFR-specific siRNA (Invitrogen) was analyzed by fluorescence-activated cell sorting (FACS) using anti-human HGFR antibody, which indicated that HGFR expression was reduced from 89.6 to 7.5% (data not shown). Negative control siRNA- and HGFR-specific siRNA-transfected Huh7 cells were transduced with scAAV3-EGFP vectors as described previously. Transgene expression was analyzed by flow cytometry 72 hr posttransduction. The transduction efficiency of AAV3 vectors was decreased from ∼23% in negative control siRNA-transfected cells to ∼8% in HGFR-specific siRNA-transfected cells (Fig. 2A). AAV3 vector-mediated transduction of Huh7 cells was also strongly inhibited by coincubation of cells with a 100-μg/ml concentration of anti-HGFR polyclonal antibodies (R&D Systems, Minneapolis, MN), specific for the extracellular domain of hHGFR (Fig. 2B).
FIG. 2.
(A) Effect of transfection with 10 pmol of either negative control siRNA or HGFR-specific siRNA on AAV3 vector-mediated transduction of Huh7 cells. (B) AAV3 vector-mediated transgene expression in Huh7 cells in the absence or presence (100 μg/ml) of anti-HGFR antibody. Transgene expression was determined 72 hr posttransduction.
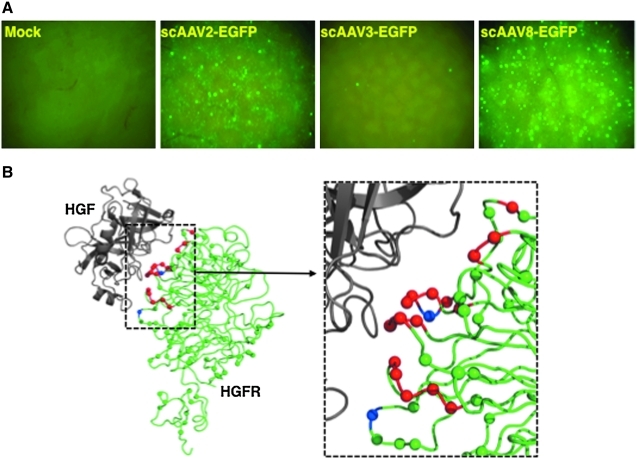
AAV3 vectors transduce murine hepatocytes inefficiently, both in vitro and in vivo
We next wished to examine whether AAV3 uses murine HGFR as a coreceptor in an animal model in vivo, especially because HGFR has been shown to be a coreceptor for AAV2 (Kashiwakura et al., 2005), and because transduction by both AAV2 and AAV3 serotype vectors has been shown to be inhibited by heparin, implying that heparan sulfate proteoglycan (HSPG) serves as a cellular receptor for both AAV2 and AAV3 (Rabinowitz et al., 2004; Blackburn et al., 2006). To this end, ∼1 × 1010 VG of scAAV3-EGFP vector were injected via the tail vein into male C57BL6/J mice, and transgene expression was evaluated in liver tissues 8 weeks postinjection. scAAV2-EGFP and scAAV8-EGFP vectors, known to transduce murine hepatocytes at low and high efficiencies, respectively (Gao et al., 2002; Thomas et al., 2004), were included as appropriate controls. These results, shown in Fig. 3A, clearly indicate that whereas efficient transduction of primary murine hepatocytes occurred with AAV8, followed by AAV2 vectors, transduction by AAV3 vectors was largely inefficient. In in vitro experiments, AAV2 vectors transduced either Hep293TT or H2.35, a mouse adult hepatocyte cell line, at the same efficiency. However, the efficiency of AAV3 vector-mediated transduction of H2.35 cells was reduced by several orders of magnitude compared with that of Hep293TT (data not shown).
FIG. 3.
(A) Transduction efficiency of scAAV2, scAAV3, and scAAV8 serotype vectors in murine hepatocytes in vivo. Male C57BL/6J mice were either mock-injected, or injected with 1 × 1010 VG each of scAAV2-CBAp-EGFP, scAAV3-CBAp-EGFP, or scAAV8-CBAp-EGFP vectors via the tail vein. Eight weeks postinjection, liver tissues were harvested and sections of each of the lobes were examined for EGFP expression, using a fluorescence microscope. Original magnification, × 100. (B) Crystal structure of the HGF β chain (gray) in complex with the Sema (extracellular) domain of hHGFR (green). In hHGFR, the Cα positions of amino acids that differ from mHGFR are depicted as green spheres; the amino acids that contact HGF in the crystal structure are depicted as red spheres; and amino acids that differ between hHGFR and mHGFR, and also make contact with HGF, are depicted as blue spheres. A close-up of the HGF and hHGFR contact region is also shown. The RCSB Protein Data Bank accession code for the coordinates used for this image is 1SHY. The program used to generate this image was PyMol.
Discussion
Ever since the realization that infection by AAV serotype 2 (AAV2) is receptor mediated (Ponnazhagan et al., 1996), concerted efforts have been made to identify the cellular receptor for AAV2, and heparan sulfate proteoglycan (HSPG) was documented to be the primary receptor for AAV2 (Summerford and Samulski, 1998). Further studies revealed that HSPG alone is insufficient, and that AAV2 also requires cellular coreceptors that mediate a successful infection (Qing et al., 1999; Summerford et al., 1999). To date, at least four additional cellular coreceptors have been identified for AAV2, including HGFR (Walters et al., 2001; Kashiwakura et al., 2005; Akache et al., 2006; Wu et al., 2006; Kurzeder et al., 2007). This is of interest because additional AAV serotypes have also been reported to use cellular growth factor receptors as coreceptors (Di Pasquale et al., 2003; Blackburn et al., 2006; Weller et al., 2010).
However, because the transduction efficiency of AAV3 vectors in general has been reported to be particularly low, both in vitro and in vivo, our observation that these vectors transduce human liver cancer cell lines exceedingly well (Glushakova et al., 2009) prompted us to hypothesize that AAV3 uses human HGFR as a putative cellular coreceptor. From the data presented here, we surmise that AAV3 does not use murine HGFR (mHGFR) as a coreceptor, despite 88% shared identity between hHGFR and mHGFR, most likely because the variations are localized in the extracellular domains, the most probable virus interaction site, and because mHGF has been shown to be an ineffective ligand for hHGFR (Rong et al., 1992; Okano et al., 1999). Indeed, mapping of mHGFR and hHGFR amino acid differences onto the crystal structure of the extracellular domain of hHGFR in complex with the α domain of HGF (Stamos et al., 2004), depicted in Fig. 3B, shows the distribution of the differing residues on the outer surface of hHGFR and a clustering at the interaction interface. The location of amino acid differences along the interaction interface, including residues observed to contact HGF, may account for the lack of use of mHGFR as a cellular coreceptor by AAV3, if a similar HGFR interaction site is used by the virus. Additional studies on AAV3–hHGFR interactions, using the labeled virus, transfection experiments using a human HGFR expression plasmid in a murine liver cancer cell line in vitro, and hydrodynamic injection of a human HGFR plasmid in a mouse model in vivo, beyond the scope of the current study, will further corroborate the current observation that AAV3 preferentially uses human HGFR as a cellular coreceptor. However, it remains possible that AAV3 does not use HSPG as a cellular receptor in vivo, even though transduction by AAV3 vectors has been shown to be inhibited by heparin in vitro (Blackburn et al., 2006). It should be emphasized that in those experiments, a relatively large dose (100 μg/ml) of heparin was used to achieve partial inhibition. In our studies, on the other hand, use of a low dose of heparin (5 μg/ml) led to an ∼2- to 3-fold increase in the transduction efficiency of AAV3 vectors (data not shown).
Although additional studies are warranted to further characterize the precise role of HSPG in the life cycle of AAV3, the evidence presented here that hHGFR is a receptor/coreceptor for AAV3 promises to lead to the development of a useful murine xenograft model to evaluate the safety and efficacy of AAV3 vectors for the potential gene therapy of human hepatoblastoma and hepatocellular carcinoma, especially because AAV3 vectors efficiently transduce primary human hepatocytes, and because transgene expression can be restricted only to liver cancer cells (Glushakova et al., 2009). This possibility has gained further support from our observations that site-directed mutagenesis of surface-exposed tyrosine residues in the AAV3 capsid further improves the transduction efficiency of AAV3 serotype vectors in human liver cancer cells as well (our unpublished data), which is consistent with our published studies with tyrosine-mutant AAV2, AAV6, AAV8, and AAV9 serotype vectors (Zhong et al., 2008; Petrs-Silva et al., 2009; Jayandharan et al., 2010; Kauss et al., 2010; Li et al., 2010; Markusic et al., 2010; Ojano-Dirain et al., 2010; Petrs-Silva et al., 2010; Qiao et al., 2010).
Acknowledgments
We thank Drs. R. Jude Samulski, James M. Wilson, and Xiao Xiao for their kind gifts of recombinant AAV3, AAV8, and pdsCBAp-EGFP plasmids, respectively, and Dr. Gail Tomlinson for generously providing Hep293TT cells. This research was supported in part by grant 8187368876 from the Roche Foundation for Anemia Research, a research grant from the Fanconi Anemia Research Fund, institutional research grant IRG-01-188-04 from the American Cancer Society (to L.Z.); Public Health Service grant P01 HL59412 from the National Institutes of Health (to M.A.-M.); and Public Health Service grants R01 HL-076901, R01 HL-097088, and P01 DK-058327 (Project 1) from the National Institutes of Health (to A.S.). G.R.J. was supported in part by an Overseas Associate Fellowship—2006 from the Department of Biotechnology, Government of India.
Author Disclosure Statement
None of the authors has any competing financial interest, or anything to disclose.
References
- Akache B. Grimm D. Pandey K. Yant S.R. Xu H. Kay M.A. The 37/67-kilodalton laminin receptor is a receptor for adeno-associated virus serotypes 8, 2, 3, and 9. J. Virol. 2006;80:9831–9836. doi: 10.1128/JVI.00878-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Asokan A. Hamra J.B. Govindasamy L. Agbandje-McKenna M. Samulski R.J. Adeno-associated virus type 2 contains an integrin α5β1 binding domain essential for viral cell entry. J. Virol. 2006;80:8961–8969. doi: 10.1128/JVI.00843-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Auricchio A. Hildinger M. O'Connor E. Gao G.P. Wilson J.M. Isolation of highly infectious and pure adeno-associated virus type 2 vectors with a single-step gravity-flow column. Hum. Gene Ther. 2001;12:71–76. doi: 10.1089/104303401450988. [DOI] [PubMed] [Google Scholar]
- Blackburn S.D. Steadman R.A. Johnson F.B. Attachment of adeno-associated virus type 3H to fibroblast growth factor receptor 1. Arch. Virol. 2006;151:617–623. doi: 10.1007/s00705-005-0650-6. [DOI] [PubMed] [Google Scholar]
- Chen T.T. Rakheja D. Hung J.Y. Hornsby P.J. Tabaczewski P. Malogolowkin M. Feusner J. Miskevich F. Schultz R. Tomlinson G.E. Establishment and characterization of a cancer cell line derived from an aggressive childhood liver tumor. Pediatr. Blood Cancer. 2009;53:1040–1047. doi: 10.1002/pbc.22187. [DOI] [PubMed] [Google Scholar]
- Chiorini J.A. Yang L. Liu Y. Safer B. Kotin R.M. Cloning of adeno-associated virus type 4 (AAV4) and generation of recombinant AAV4 particles. J. Virol. 1997;71:6823–6833. doi: 10.1128/jvi.71.9.6823-6833.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chiorini J.A. Kim F. Yang L. Kotin R.M. Cloning and characterization of adeno-associated virus type 5. J. Virol. 1999;73:1309–1319. doi: 10.1128/jvi.73.2.1309-1319.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Daya S. Berns K.I. Gene therapy using adeno-associated virus vectors. Clin. Microbiol. Rev. 2008;21:583–593. doi: 10.1128/CMR.00008-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Di Pasquale G. Davidson B.L. Stein C.S. Martins I. Scudiero D. Monks A. Chiorini J.A. Identification of PDGFR as a receptor for AAV-5 transduction. Nat. Med. 2003;9:1306–1312. doi: 10.1038/nm929. [DOI] [PubMed] [Google Scholar]
- Gao G. Vandenberghe L.H. Alvira M.R. Lu Y. Calcedo R. Zhou X. Wilson J.M. Clades of adeno-associated viruses are widely disseminated in human tissues. J. Virol. 2004;78:6381–6388. doi: 10.1128/JVI.78.12.6381-6388.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gao G.P. Alvira M.R. Wang L. Calcedo R. Johnston J. Wilson J.M. Novel adeno-associated viruses from rhesus monkeys as vectors for human gene therapy. Proc. Natl. Acad. Sci. U.S.A. 2002;99:11854–11859. doi: 10.1073/pnas.182412299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Glushakova L.G. Lisankie M.J. Eruslanov E.B. Ojano-Dirain C. Zolotukhin I. Liu C. Srivastava A. Stacpoole P.W. AAV3-mediated transfer and expression of the pyruvate dehydrogenase E1α subunit gene causes metabolic remodeling and apoptosis of human liver cancer cells. Mol. Genet. Metab. 2009;98:289–299. doi: 10.1016/j.ymgme.2009.05.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grigioni W.F. Fiorentino M. D'Errico A. Ponzetto A. Crepaldi T. Prat M. Comoglio P.M. Overexpression of c-met protooncogene product and raised Ki67 index in hepatocellular carcinomas with respect to benign liver conditions. Hepatology. 1995;21:1543–1546. [PubMed] [Google Scholar]
- Jayandharan G.R. Zhong L. Sack B.K. Rivers A.E. Li M. Li B. Herzog R. Srivastava A. Optimized adeno-associated virus (AAV)-protein phosphatase-S helper viruses for efficient liver transduction by single-stranded AAV vectors: therapeutic expression of factor IX at reduced vector doses. Hum. Gene Ther. 2010;21:271–283. doi: 10.1089/hum.2009.100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaludov N. Brown K.E. Walters R.W. Zabner J. Chiorini J.A. Adeno-associated virus serotype 4 (AAV4) and AAV5 both require sialic acid binding for hemagglutination and efficient transduction but differ in sialic acid linkage specificity. J. Virol. 2001;75:6884–6893. doi: 10.1128/JVI.75.15.6884-6893.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kashiwakura Y. Tamayose K. Iwabuchi K. Hirai Y. Shimada T. Matsumoto K. Nakamura T. Watanabe M. Oshimi K. Daida H. Hepatocyte growth factor receptor is a coreceptor for adeno-associated virus type 2 infection. J. Virol. 2005;79:609–614. doi: 10.1128/JVI.79.1.609-614.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kauss M.A. Smith L.J. Zhong L. Srivastava A. Wong K.K., Jr. Chatterjee S. Enhanced long-term transduction and multilineage engraftment of human hematopoietic stem cells transduced with tyrosine-modified recombinant adeno-associated virus serotype 2. Hum. Gene Ther. 2010;21:1129–1136. doi: 10.1089/hum.2010.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kube D.M. Srivastava A. Quantitative DNA slot blot analysis: Inhibition of DNA binding to membranes by magnesium ions. Nucleic Acids Res. 1997;25:3375–3376. doi: 10.1093/nar/25.16.3375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kurzeder C. Koppold B. Sauer G. Pabst S. Kreienberg R. Deissler H. CD9 promotes adeno-associated virus type 2 infection of mammary carcinoma cells with low cell surface expression of heparan sulphate proteoglycans. Int. J. Mol. Med. 2007;19:325–333. [PubMed] [Google Scholar]
- Li M. Jayandharan G.R. Li B. Ling C. Ma W. Srivastava A. Zhong L. High-efficiency transduction of fibroblasts and mesenchymal stem cells by tyrosine-mutant AAV2 vectors for their potential use in cellular therapy. Hum. Gene Ther. 2010;21:1527–1543. doi: 10.1089/hum.2010.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Markusic D.M. Herzog R.W. Aslanidi G.V. Hoffman B.E. Li B. Li M. Jayandharan G.R. Ling C. Zolotukhin I. Ma W. Zolotukhin S. Srivastava A. Zhong L. High-efficiency transduction and correction of murine hemophilia B using AAV2 vectors devoid of multiple surface-exposed tyrosines. Mol. Ther. 2010 Aug 24; doi: 10.1038/mt.2010.172. [Epub ahead of print] PMID: 20736929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muramatsu S. Mizukami H. Young N.S. Brown K.E. Nucleotide sequencing and generation of an infectious clone of adeno-associated virus 3. Virology. 1996;221:208–217. doi: 10.1006/viro.1996.0367. [DOI] [PubMed] [Google Scholar]
- Nakabayashi H. Taketa K. Miyano K. Yamane T. Sato J. Growth of human hepatoma cells lines with differentiated functions in chemically defined medium. Cancer Res. 1982;42:3858–3863. [PubMed] [Google Scholar]
- Ojano-Dirain C. Glushakova L.G. Zhong L. Zolotukhin S. Muzyczka N. Srivastava A. Stacpoole P.W. An animal model of PDH deficiency using AAV8-siRNA vector-mediated knockdown of pyruvate dehydrogenase E1α. Mol. Genet. Metab. 2010;101:183–191. doi: 10.1016/j.ymgme.2010.07.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Okano J. Shiota G. Kawasaki H. Expression of hepatocyte growth factor (HGF) and HGF receptor (c-Met) proteins in liver diseases: An immunohistochemical study. Liver. 1999;19:151–159. doi: 10.1111/j.1478-3231.1999.tb00025.x. [DOI] [PubMed] [Google Scholar]
- Petrs-Silva H. Dinculescu A. Li Q. Min S.H. Chiodo V. Pang J.J. Zhong L. Zolotukhin S. Srivastava A. Lewin A.S. Hauswirth W.W. High-efficiency transduction of the mouse retina by tyrosine-mutant AAV serotype vectors. Mol. Ther. 2009;17:463–471. doi: 10.1038/mt.2008.269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Petrs-Silva H. Dinculescu A. Li Q. Deng W.T. Pang J.J. Min S.H. Chiodo V. Neeley A.W. Govindasamy L. Bennett A. Agbandje-McKenna M. Zhong L. Li B. Jayandharan G.R. Srivastava A. Lewin A.S. Hauswirth W.W. Novel properties of tyrosine-mutant AAV2 vectors in the mouse retina. Mol. Ther. 2010 Nov 2; doi: 10.1038/mt.2010.234. [Epub ahead of print] PMID: 21045809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ponnazhagan S. Wang X.S. Woody M.J. Luo F. Kang L.Y. Nallari M.L. Munshi N.C. Zhou S.Z. Srivastava A. Differential expression in human cells from the p6 promoter of human parvovirus B19 following plasmid transfection and recombinant adeno-associated virus 2 (AAV) infection: Human megakaryocytic leukaemia cells are non-permissive for AAV infection. J. Gen. Virol. 1996;77:1111–1122. doi: 10.1099/0022-1317-77-6-1111. [DOI] [PubMed] [Google Scholar]
- Qiao C. Zhang W. Yuan Z. Shin J.H. Li J. Jayandharan G.R. Zhong L. Srivastava A. Xiao X. Duan D. Adeno-associated virus serotype 6 capsid tyrosine-to-phenylalanine mutations improve gene transfer to skeletal muscle. Hum. Gene Ther. 2010;21:1343–1348. doi: 10.1089/hum.2010.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Qing K. Mah C. Hansen J. Zhou S. Dwarki V. Srivastava A. Human fibroblast growth factor receptor 1 is a co-receptor for infection by adeno-associated virus 2. Nat. Med. 1999;5:71–77. doi: 10.1038/4758. [DOI] [PubMed] [Google Scholar]
- Rabinowitz J.E. Bowles D.E. Faust S.M. Ledford J.G. Cunningham S.E. Samulski R.J. Cross-dressing the virion: The transcapsidation of adeno-associated virus serotypes functionally defines subgroups. J. Virol. 2004;78:4421–4432. doi: 10.1128/JVI.78.9.4421-4432.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rong S. Bodescot M. Blair D. Dunn J. Nakamura T. Mizuno K. Park M. Chan A. Aaronson S. Vande Woude G.F. Tumorigenicity of the met proto-oncogene and the gene for hepatocyte growth factor. Mol. Cell. Biol. 1992;12:5152–5158. doi: 10.1128/mcb.12.11.5152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rutledge E.A. Halbert C.L. Russell D.W. Infectious clones and vectors derived from adeno-associated virus (AAV) serotypes other than AAV type 2. J. Virol. 1998;72:309–319. doi: 10.1128/jvi.72.1.309-319.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stamos J. Lazarus R.A. Yao X. Kirchhofer D. Wiesmann C. Crystal structure of the HGF β-chain in complex with the Sema domain of the Met receptor. EMBO J. 2004;23:2325–2335. doi: 10.1038/sj.emboj.7600243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Summerford C. Samulski R.J. Membrane-associated heparan sulfate proteoglycan is a receptor for adeno-associated virus type 2 virions. J. Virol. 1998;72:1438–1445. doi: 10.1128/jvi.72.2.1438-1445.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Summerford C. Bartlett J.S. Samulski R.J. αVβ5 integrin: A co-receptor for adeno-associated virus type 2 infection. Nat. Med. 1999;5:78–82. doi: 10.1038/4768. [DOI] [PubMed] [Google Scholar]
- Thomas C.E. Storm T.A. Huang Z. Kay M.A. Rapid uncoating of vector genomes is the key to efficient liver transduction with pseudotyped adeno-associated virus vectors. J. Virol. 2004;78:3110–3122. doi: 10.1128/JVI.78.6.3110-3122.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walters R.W. Yi S.M. Keshavjee S. Brown K.E. Welsh M.J. Chiorini J.A. Zabner J. Binding of adeno-associated virus type 5 to 2,3-linked sialic acid is required for gene transfer. J. Biol. Chem. 2001;276:20610–20616. doi: 10.1074/jbc.M101559200. [DOI] [PubMed] [Google Scholar]
- Weller M.L. Amornphimoltham P. Schmidt M. Wilson P.A. Gutkind J.S. Chiorini A. Epidermal growth factor receptor is a co-receptor for adeno-associated virus serotype 6. Nat. Med. 2010;16:662–664. doi: 10.1038/nm.2145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu J. Zhao W. Zhong L. Han Z. Li B. Ma W. Weigel-Kelley K.A. Warrington K.H. Srivastava A. Self-complementary recombinant adeno-associated viral vectors: Packaging capacity and the role of Rep proteins in vector purity. Hum. Gene Ther. 2007;18:171–182. doi: 10.1089/hum.2006.088. [DOI] [PubMed] [Google Scholar]
- Wu Z. Miller E. Agbandje-McKenna M. Samulski R.J. α2,3 and α2,6 N-linked sialic acids facilitate efficient binding and transduction by adeno-associated virus types 1 and 6. J. Virol. 2006;80:9093–9103. doi: 10.1128/JVI.00895-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhong L. Li B. Mah C.S. Govindasamy L. Agbandje-McKenna M. Cooper M. Herzog R.W. Zolotukhin I. Warrington K.H., Jr. Weigel-Van Aken K.A. Hobbs J.A. Zolotukhin S. Muzyczka N. Srivastava A. Next generation of adeno-associated virus 2 vectors: Point mutations in tyrosines lead to high-efficiency transduction at lower doses. Proc. Natl. Acad. Sci. U.S.A. 2008;105:7827–7832. doi: 10.1073/pnas.0802866105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zincarelli C. Soltys S. Rengo G. Rabinowitz J.E. Analysis of AAV serotypes 1–9 mediated gene expression and tropism in mice after systemic injection. Mol. Ther. 2008;16:1073–1080. doi: 10.1038/mt.2008.76. [DOI] [PubMed] [Google Scholar]