Abstract
INTRODUCTION:
To establish disease severity at admission can be performed by way of the mortality prognostic. Nowadays the prognostic scores make part of quality control and research. The Pediatric Risk of Mortality (PRISM) is one of the scores used in the pediatric intensive care units.
OBJECTIVES:
The purpose of this study is the utilization of the PRISM and determination of mortality risk factors in a tertiary pediatric intensive care unit.
METHODS
: Retrospective cohort study, in a period of one year, at a general tertiary pediatric intensive care unit. The pediatric risk of mortality scores corresponding to the first 24 hours of hospitalization were recorded; additional data were collected to characterize the study population.
RESULTS:
359 patients were included; the variables that were found to be risk factors for death were multiple organ dysfunction syndrome on admission, mechanical ventilation, use of vasoactive drugs, hospital‐acquired infection, parenteral nutrition and duration of hospitalization (p < 0,0001). Fifty‐four patients (15%) died; median pediatric risk of mortality score was significantly lower in patients who survived (p = 0,0001). The ROC curve yielded a value of 0.76 (CI 95% 0,69–0,83) and the calibration was shown to be adequate.
DISCUSSION:
It is imperative for pediatric intensive care units to implement strict quality controls to identify groups at risk of death and to ensure the adequacy of treatment. Although some authors have shown that the PRISM score overestimates mortality and that it is not appropriate in specific pediatric populations, in this study pediatric risk of mortality showed satisfactory discriminatory performance in differentiating between survivors and non‐survivors.
CONCLUSIONS:
The pediatric risk of mortality score showed adequate discriminatory capacity and thus constitutes a useful tool for the assessment of prognosis for pediatric patients admitted to a tertiary pediatric intensive care units.
Keywords: Quality of care, Prognostic scores, Multiple organ dysfunction syndrome, Critical care, Mortality rate
INTRODUCTION
Technological advances in pediatric intensive care units (PICU), resulted to a more sophisticated care for children and adolescents, thus making these units prepared to treat cases of high complexity at a high cost. However, the technology available has not always succeeded in improving the quality of patient care and higher ability to augment life expectancy becomes an instrument that could increase the suffering and prolong the death process1. Thus, it became necessary to characterize the disease severity at admission, assessing its prognosis2. This procedure can be performed through the mortality prognostic scores that objectively quantify the severity of the patient, estimating the probability of death according to their clinical state3 and could aid in various areas of treatment and care, such as selection of treatments, ethical issues and economic strategies.4 Furthermore, comparing the mortality to the severity of illness, they can be also used to classify patients and may be used to compare clinical studies and technological resources.5
At admission it is difficult to establish clinical and laboratorial criteria that allow an estimative of the number and intensity of organ dysfunction and need for therapeutic intervention.
Ever since the introduction of mortality scores in the ICU, they have been used more frequently and nowadays the scores are part of the methodology of quality control and research.6 They are useful for evaluating the quality of care, prognosis, to estimate the risk of mortality and to compare different services according to the complexity of the underlying disease.7,8
The Pediatric Risk of Mortality (PRISM) score is one of the main indicators used in the pediatric intensive care unit.2 It was obtained and validated from the Physiologic Stability Index (PSI)9 with 1415 patients evaluated for nine U.S. PICU between 1984 and 1985, and the mortality rate was of 116. Statistical analysis eliminated the insignificant PSI categories, thus reducing the number of physiological parameters, creating and validating the PRISM. It uses 14 parameters (physiological and laboratory data) and for each one was used the highest severity value recorded in the first 24 hours. The risk of death is calculated by a logistic regression equation using the value of the PRISM, patient age and need of surgery on admission to the PICU,2 but performance was not significantly influenced by the post operative status of the patients. It presents an excellent discriminatory performance and prediction, being used in many PICUs as a prognostic score to assess gravity of disease. Some studies show that PRISM has the ability to assess indication of mortality rate7,10-12 while other studies show that PRISM overestimates mortality.13-16
Besides PRISM, the prognostic score which is being used in the medical literature is Pediatric Index of Mortality (PIM).17,18 This score was validated in PICU in New Zealand, Australia and United Kingdom; the data are collected in the first hour of admission and the risk of death is calculated by a logistic regression equation that uses physiological variables, operative status, presence of underlying disease and reason for hospitalization.
Scores PRISM and PIM have already been compared in the literature.7,15,19,20 However, these studies were performed in the secondary care level PICU and the results obtained were not conclusive.
Using a practical and objective scoring system to provide clinical and / or laboratorial criteria to evaluate if a delayed treatment is a factor of impact on quality of care for critically ill patients is very important. The ideal score should be easy to use, does not require extensive experience of the observer, easy to reproduce, low cost, minimally invasive and accurate.21
The purpose of this study is to evaluate the use of a prognostic score of mortality (PRISM) in a Tertiary Pediatric Intensive Care Unit.
MATERIALS AND METHODS
Population
A retrospective cohort study was conducted in the Pediatric Intensive Care Unit of the Instituto da Criança, Hospital das Clinicas, University of São Paulo. This is a tertiary care unit that receives highly complex pediatric diseases, both clinical and surgical. Our PICU doesn't attend trauma patients. It has 15 beds and provides care to children from one month to 18 years of age. We studied all patients admitted to the Pediatric Intensive Care Unit from April 2007 to April 2008.
The study was approved by the Ethics Committee for Analysis of Research Projects of the Clinical Board of the Hospital das Clinicas and School of Medicine, University of São Paulo. Because the study consisted of reviewing medical records, it received a waiver of informed consent accompanied by a signed agreement to maintain confidentiality regarding patient identification and data.
Methodology
Medical records were analyzed and the PRISM scores corresponding to the first 24 hours of hospitalization were recorded. The scores were calculated according to the equation described by Pollack et al. (1988)2. Patients who died within the first eight hours after admission or who were discharged from the ICU within 24 hours were excluded from the study.
Additional data were gathered to better characterize the study population: age at admission, gender, underlying disease, readmission (up to 48 hours after discharge), multiple organ dysfunction syndrome (Goldstein 2005)22 (MODS, defined as involvement of two or more organs), type of admission (clinical or surgical), occurrence of nosocomial infection during hospitalization, mechanical ventilation (MV), treatment with vasoactive drugs and parenteral nutrition therapy (PNT). These variables were selected based on previous studies of risk factors for death in patients with similar characteristics who were admitted to the Intensive Care Unit.17,23
Data were tabulated and analyzed in a spreadsheet using STATA ®. The PRISM score values were analyzed to obtain the median. Categorical variables were analyzed using the chi‐square test. In the case of continuous categorical variables, we opted for the chi‐square trend test. Means were compared according to the Mann‐Whitney test. Logistic regression was used to calculate the odds ratios (OR) and respective p values. Finally, the univariate linear regression Pearson correlation was used to study the association between risk factors and PRISM score.
P ≤ 0.05 was considered indicative of statistical significance. The discriminative power of the model (i.e., its ability to distinguish patients who would survive from those who would die) was calculated based on the ROC curve (area under the diagnostic yield curve). Calibration (i.e., the accuracy of the expected risk of death) was calculated using the Hosmer‐Lemeshow chi‐square test to compare actual vs. predicted mortality. The calibration test yielded a p value > 0.05, indicating a good fit (the higher the p value, the better the fit of the model).
RESULTS
During the study period there were 398 admissions in the Pediatric Intensive Care Unit but 39 patients met exclusion criteria: 10 patients died within the first eight hours, 26 were discharged within 24 hours and three were excluded for lack of medical records. Thus, 359 patients were included; the median age was 31 months; the majority of patients was clinical (78%) and had underlying disease (86%), the most frequent were hepatological (23%) and oncological (19%), required the use of mechanical ventilation (63%) and vasoactive drugs (35%); the characteristics of the sample population studied are detailed in Table 1.
Table 1.
Characteristics of study population.
| Variables | n° (%) | median (P25‐P75) |
| Total patients | 359 | |
| Age (months) | 31 (11 – 94) | |
| Length of stay in ICU (days) | 5 (3 – 10) | |
| Gender | ||
| Male | 198 (55) | |
| Female | 161 (45) | |
| Patients | ||
| Clinical | 280 (78) | |
| Surgical | 79 (22) | |
| Underlying disease (main) | ||
| N | 49 (14) | |
| Y | 310 (86) | |
| Hepatological | 70 (23) | |
| Oncology | 60 (19) | |
| Neurology | 49 (16) | |
| Respiratory | 34 (11) | |
| Others | 97 (31) | |
| Use of mechanical ventilation | ||
| N | 134 (37) | |
| Y | 225 (63) | |
| Use of vasoactive drugs | ||
| N | 231 (65) | |
| Y | 128 (35) | |
| 1 drug | 60 (47) | |
| 2 drugs | 31 (24) | |
| ≥ 3 drugs | 37 (29) | |
| Deaths | 54 (15) |
ICU = Intensive Care Unit; N = no; Y = yes
Of the 359 patients studied, 54 (15%) died. The median mortality‐associated PRISM score was eight points whereas the median PRISM score was significantly lower in patients who survived (Table 2).
Table 2.
PRISM comparison between patients who died and survivors
| Patient | PRISM Median (P25‐P75) | p |
| General | 8 (4 – 14) | |
| Deaths | 15 (8 – 21) | 0,0001 * |
| Survivors | 7 (3 – 12) |
p between patients who died and survivors; Mann‐Whitney test
The variables that were found to be risk factors for death were MODS on admission, mechanical ventilation (MV), use of vasoactive drugs, hospital‐acquired infection, PNT and duration of hospital stay (p < 0,0001). The use of vasoactive drugs and each additional day in the hospital carried a mortality OR of 4.38 (CI 95% 3,16–6,09; p<0,0001) and 1.02 (CI 95% 1,00–1,03; p = 0,015), respectively (Table 3).
Table 3.
Risk factors for death.
| Variable | Category | Deaths | OR (CI 95%) | p |
| n (%) | ||||
| Gender | F | 23 (14,2) | 0,718 * | |
| M | 31 (15,6) | |||
| Age | < 1 year | 13 (12,5) | 0,390 * | |
| > 1 year | 41 (16,0) | |||
| Readmission | Y | 4 (26,6) | 0,198 * | |
| N | 50 (14,5) | |||
| MODS on admission | Y | 35 (33,6) | < 0,0001* | |
| N | 19 (7,45) | |||
| Type of admission | Clinical | 47 (16,7) | 0,082 * | |
| Surgical | 7 (8,8) | |||
| Underlying disease | Y | 50 (16,1) | 0,147 * | |
| N | 4 (8,1) | |||
| Use of MV | Y | 54 (24,0) | < 0,0001* | |
| N | 0 (0,0) | |||
| Use of vasoactive drugs | Y | 47 (36,7) | < 0,0001* | |
| N | 7 (3,0) | |||
| Number of vasoactive drugs used | 0 | 7 (3,0) | < 0,0001** | |
| 1 | 7 (11,6) | |||
| 2 | 14 (45,1) | |||
| ≥ 3 | 26 (70,2) | |||
| add 1 drug | 4,38 (3,16‐6,09) | < 0,0001*** | ||
| Nosocomial infection | Y | 30 (33,3) | < 0,0001* | |
| N | 24 (8,9) | |||
| Use of PNT | Y | 15 (46,8) | < 0,0001* | |
| N | 39 (11,9) | |||
| Duration of PICU stay | until 3 days | 10 (8,1) | < 0,0001** | |
| 3 ‐ 7 days | 7 (7,0) | |||
| > 7 days | 37 (27,0) | |||
| add 1 day | 1,02 (1,00‐1,03) | 0,015*** |
F = female; M = male; N = no; Y = yes; MV = mechanical ventilation; PNT = parenteral nutrition; PICU = pediatric intensive care unit; MODS = multiple organ dysfunction syndrome
chi‐square test
chi‐square trend test
Wald test
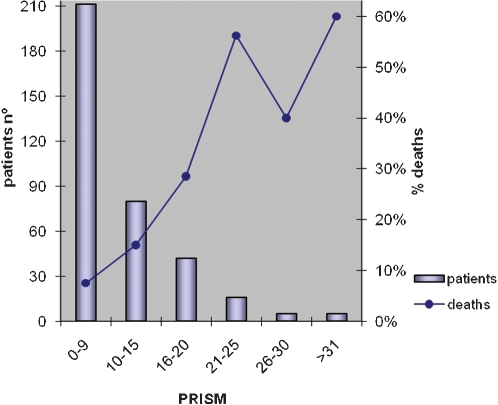
Figure 1 shows the relationship between the value of the PRISM and the number of deaths.
Figure 1.
Relationship between PRISM and the number of deaths.
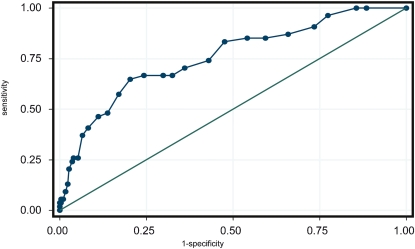
Assessment of the discriminatory performance of the PRISM score as measured by the area under the ROC curve yielded a value of 0.76 (CI 95% 0,69–0,83) (Figure 2). The calibration, calculated using the Hosmer‐Lemeshow chi‐square test, was shown to be adequate (x2 = 12,96; p = 0,11).
Figure 2.
PRISM ROC Curve = 0,76 (IC 95% 0,69‐0,83).
Variables that were associated with the PRISM score were MODS on admission, mechanical ventilation, vasoactive medication, hospital‐acquired infection and duration of hospital stay (Table 4).
Table 4.
Univariate linear regression of the association between risk factors and the PRISM.
| Variables | r2 | β [CI 95%] |
| Gender | 0,0002 | ‐0,03 [‐1,82 ‐ 5,93] |
| Age | 0,0037 | 0,03 [‐0,02 – 0,10] |
| Readmission | 0,0030 | 2,05 [‐0,25 ‐ 0,19] |
| MODS on admission | 0,1773 | 0,99 [0,77 ‐ 1,21] |
| Type of admission | 0,0029 | ‐0,13 [‐0,40 ‐ 0,13] |
| Underlying disease | 0,0070 | 0,26 [‐0,06 ‐ 0,58] |
| MV | 0,0556 | 0,52 [0,29 ‐ 0,74] |
| Vasoactive drug | 0,1180 | 0,76 [0,55 ‐ 0,98] |
| Nosocomial infection | 0,0651 | 0,63 [0,38 ‐ 0,88] |
| PNT | 0,0054 | 0,27 [‐0,11 ‐ 0,66] |
| Duration of ICU stay | 0,0234 | 0,01 [0,003 ‐ 0,019] |
r2 – Pearson correlation coefficient
DISCUSSION
Given the improvement in pediatric care in the Pediatric Intensive Care Unit, it is imperative that there be strict quality control to identify groups at greatest risk of death and to ensure the adequacy of treatment and the planning and rational use of resources. Differences in mortality rates within the PICU can be explained by the severity of illness of patients treated in each service.24 The use of prognostic indicators is an essential quality criterion in the care of critically ill patients.
The comparison between PRISM and PIM scores have already been made in studies of secondary care level PICU.7,15,19,20 However, traditionally the PRISM score is the most used in PICU and, therefore, we chose to use it.
This study presents the characteristics of a population hospitalized in a predominantly clinical tertiary Intensive Care Unit with mostly symptomatic patients. Parametric analysis showed no relationship of patient type and underlying disease with risk of death, similar to the findings of Tan et al (1998).25 The severity of disease in patients with an average mortality rate of 15% can be determined by the high prevalence of use of mechanical ventilation and vasoactive drugs.
Aragão et al. (2001) observed that male patients had a higher risk of death, although this trend was not observed in the current study.26 Other reports,27 including the same author,26 showed that patients between 12 and 24 months of age had a higher risk of death compared to patients older than seven years. The median age of patients in our dataset was 31 months and we did not find age to be an important risk factor when comparing different age groups, including patients older than seven years as was done in the study by Tan et al. (1998).25
Typpo et al. (2009) demonstrated that the presence of MODS on the first day of hospitalization was related to higher mortality and prolonged length of stay in the intensive care unit.28 In this study, a parametric analysis, MODS was also identified as a significant risk factor for death. Univariate linear regression analysis showed that MODS was associated with PRISM scores, as was also found in other studies.10,27 Bellad et al. (2009) showed that, among the variables that affect prognosis, the number of dysfunctional organs was moderately correlated with the PRISM score (r2 = 0,586, p<0,001).10
The use of mechanical ventilation and vasoactive drugs were risk factors for death, corroborating the findings of other authors who showed a higher mortality rate in patients undergoing these procedures.25,26,29-32 Regarding the use of vasoactive drugs, this study demonstrated that adding a drug with cardiac and/or vascular effects increased the risk of death by approximately four‐fold (Wald test; table 2). Other factors that were significantly associated with mortality were the presence of nosocomial infection, use of PNT and duration of hospitalization. Williams et al. (2010) showed that in the adult Intensive Care Unit, the duration of hospitalization is not an independent risk factor for mortality;33 however, in our study, each additional day of hospitalization increased the risk of death by approximately 2% (Wald test; table 2).
By validating the PRISM score, Pollack et al. (1988) identified the physiological variables that contribute directly to the risk of death without adjustment for diagnosis2. If the patient sample in which an index is applied is different from the original sample, the fit of the model may not be appropriate, resulting in an unreliable estimation of mortality risk. It is therefore important to validate models before applying them in a given population.
The median age of patients in this study (31 months) was similar to that of the population used in the validation of PRISM by Pollack et al. (1988), which was 33 months.2
Although some authors have shown that the PRISM score overestimated mortality13-16 and that it is not appropriate in specific pediatric populations, such as post‐trauma patients,34 patients with acute renal failure35 and related to Plasmodium falciparum malaria,36 in this study PRISM showed satisfactory discriminatory performance in differentiating survivors from non‐survivors, supporting the conclusion that higher PRISM scores are correlated with increased risk of death, similar other studies.7,10-12,27
Martha et al. (2005) evaluated the PRISM scores of 421 patients and showed good discriminatory performance with proper calibration.7 Brakel et al. (2000) and Leuteurtre et al. (2001) showed that the PRISM score provides good discriminatory power for patients with meningococcal disease and in children with meningococcal septic shock.11,12
In addition to MODS, other variables that were associated with PRISM included: mechanical ventilation, vasoactive medication, hospital‐acquired infection and length of stay in intensive care. Some authors have shown that, although the PRISM score is not an independent factor for nosocomial infection,37,38 patients with higher values on admission are more likely to acquire infections during their hospitalization.37,39,40 Carroll et al. (1993 and 2003) showed that the PRISM score in the first 24 hours after liver transplantation is a prognostic indicator for the length of stay in intensive care.41,42
CONCLUSION
The PRISM score showed adequate discriminatory capacity and calibration and thus constitutes a useful tool for the assessment of prognosis for pediatric patients admitted to a tertiary Pediatric Intensive Care Unit. In this study the variables that were identified as risk factors for death were admission with MODS, VM, use of vasoactive drugs, hospital‐acquired infection, PNT and duration of hospital stay.
REFERENCES
- 1. Batista CC, Gattass CA, Calheiros TP, Moura RB. Avaliação prognóstica individual na UTI: é possível diferenciar insistência terapêutica de obstinação terapêutica? Rev Bras Ter Intensiva. 2009;21:247–54. 10.1590/S0103‐507X2009000300003 [PubMed] [Google Scholar]
- 2. Pollack MM, Ruttimann E, Getson PR. Pediatric risk of mortality (PRISM) score. Crit Care Med. 1988;16:1110–6. doi: 10.1097/00003246-198811000-00006. 10.1097/00003246‐198811000‐00006 [DOI] [PubMed] [Google Scholar]
- 3. Gunning K, Rowan K. ABC of intensive care: outcome data and scoring systems. BMJ. 1999;319:241–4. doi: 10.1136/bmj.319.7204.241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Kalil Filho WJ, Delgado AF, Schvartsman B, Kimura HM. Análise Clínica e Prognóstica da Síndrome de Disfunção Orgânica Múltipla. Pediatria (São Paulo) 1995;17:143–7. [Google Scholar]
- 5. Seneff M, Knaus WA. Predicting patient outcome from intensive care: a guide to APACHE, MPM, SAPS, PRISM, and other prognostic scoring systems. J Intensive Care Med. 1990;5:33–52. 10.1177/088506669000500107 [Google Scholar]
- 6. Shann F. Are we doing a good job: PRISM, PIM and all that. Intensive Care Med. 2002;28:105–7. doi: 10.1007/s00134-001-1186-1. 10.1007/s00134‐001‐1186‐1 [DOI] [PubMed] [Google Scholar]
- 7. Martha VF, Garcia PCR, Piva JP, Einloft PR, Bruno F, Rampon V. Comparação entre dois escores prognósticos (PRISM e PIM) em uma unidade de terapia intensiva pediátrica. J Pediatr (Rio J) 2005;81:259–64. [PubMed] [Google Scholar]
- 8. Lacroix J, Cotting J. Severity of illness and organ dysfunction scoring in children. Pediatr Crit Care Med. 2005;6:S126–34. doi: 10.1097/01.PCC.0000161287.61028.D4. 10.1097/01.PCC.0000161287.61028.D4 [DOI] [PubMed] [Google Scholar]
- 9. Yeh TS, Pollack MM, Ruttimann UE, Holbrook PR, Fields AI. Validation of a physiologic stability index for use in critically ill infants and children. Pediatr Res. 1984;18:445–51. doi: 10.1203/00006450-198405000-00011. 10.1203/00006450‐198405000‐00011 [DOI] [PubMed] [Google Scholar]
- 10. Bellad R, Rao S, Patil VD, Mahantshetti NS. Outcome of intensive care unit patients using pediatric risk of mortality (PRISM) score. Indian Pediatr. 2009;46:1091–2. [PubMed] [Google Scholar]
- 11. Van Brakel MJM, Vught AJ, Gemke RJBJ. Pediatric risk of mortality (PRISM) score in meningococcal disease. Eur J Pediatr. 2000;159:232–6. doi: 10.1007/s004310050060. [DOI] [PubMed] [Google Scholar]
- 12. Leteurtre S, Leclerc F, Martinot A, Cremer R, Fourier C, Sadik A, et al. Can generic scores (Pediatric Risk of Mortality and Pediatric Index of Mortality) replace specific scores in predicting the outcome of presumed meningococcal septic shock in children? Crit Care Med. 2001;29:1239–46. doi: 10.1097/00003246-200106000-00033. 10.1097/00003246‐200106000‐00033 [DOI] [PubMed] [Google Scholar]
- 13. Espuñes SP, Cid JL, Galán CR, Villanueva AM, Torre AC, Camblor P. Índices prognósticos de mortalidad em cuidados intensivos pediátricos. An Pediatr (Barc) 2007;66:345–50. doi: 10.1157/13101237. 10.1157/13101237 [DOI] [PubMed] [Google Scholar]
- 14. Eulmesekian DP, Pérez A, Minces P, Ferrero H, Bimbi TF. Validación de dos modelos de predicción de mortalidad, PRISM y PIM2, en una Unidad de Cuidados Intensivos Pediátricos. Arch Argent Pediatr. 2006;104:387–92. [Google Scholar]
- 15. Slater A, Shann F. The suitability of the pediatric index of mortality (PIM), PIM2, the pediatric risk of mortality (PRISM), and PRISM III for monitoring the quality of pediatric intensive care in Australia and New Zealand. Pediatr Crit Care Med. 2004;5:447–54. doi: 10.1097/01.PCC.0000138557.31831.65. 10.1097/01.PCC.0000138557.31831.65 [DOI] [PubMed] [Google Scholar]
- 16. Goddard JM. Pediatric risk of mortality scoring overestimates severity off illness in infants. Crit Care Med. 1992;20:1662–5. 10.1097/00003246‐199212000‐00010 [PubMed] [Google Scholar]
- 17. Shann F, Pearson G, Slater A, Wilkinson K. Paediatric index of Mortality (PIM): a mortality prediction model for children in intensive care. Intensive Care Med. 1997;23:201–7. doi: 10.1007/s001340050317. 10.1007/s001340050317 [DOI] [PubMed] [Google Scholar]
- 18. Slater A, Shann F, Pearson G. PIM2: a revised version of the Pediatric Index of Mortality. Intensive Care Med. 2003;29:278–85. doi: 10.1007/s00134-002-1601-2. [DOI] [PubMed] [Google Scholar]
- 19. Wolfler A, Silvani P, Musicco M, Salvo I. Pediatric index of mortality 2 score in Italy: a multicenter, prospective, observational study. Intensive Care Med. 2007;33:1407–13. doi: 10.1007/s00134-007-0694-z. 10.1007/s00134‐007‐0694‐z [DOI] [PubMed] [Google Scholar]
- 20. Ozer EA, Kizilgunesker A, Sarioglu B, Haliciolgu O, Sutcuoglu S, Yaprak I. The Comparison of PRISM and PIM scoring systems for mortality risk in infantile intensive care. J Trop Ped. 2004;50:334–8. doi: 10.1093/tropej/50.6.334. [DOI] [PubMed] [Google Scholar]
- 21. Pollack MM, Patel KM, Ruttimann UE. PRISM III: An update Pediatric Risk of Mortality score. Crit Care Med. 1996;24:743–52. doi: 10.1097/00003246-199605000-00004. 10.1097/00003246‐199605000‐00004 [DOI] [PubMed] [Google Scholar]
- 22. Goldstein B, Giroir B, Randolph A. International pediatric sepsis consensus conference: Definitions for sepsis and organ dysfunction in pediatrics. Pediatr Crit Care Med. 2005;6:2–8. doi: 10.1097/01.PCC.0000149131.72248.E6. 10.1097/01.PCC.0000149131.72248.e6",-1,"xxx/72248.e6 [DOI] [PubMed] [Google Scholar]
- 23. Pollack MM, Yeh TS, Ruttimann EU, Holbrook PR, Fields AI. Evaluation of pediatric intensive care unit. Crit Care Med. 1984;12:376–83. doi: 10.1097/00003246-198404000-00008. 10.1097/00003246‐198404000‐00008 [DOI] [PubMed] [Google Scholar]
- 24. Pollack MM, Ruttimann UE, Getson PR. Accurate prediction of the outcome of pediatric intensive care. A new quantitative method. N Engl J Med. 1987;316:134–9. doi: 10.1056/NEJM198701153160304. [DOI] [PubMed] [Google Scholar]
- 25. Tan GH, Tan TH, Goh DYT, Yap HK. Risk factors for predicting mortality in a paediatric intensive care unit. Ann Acad Med Singapore. 1998;27:813–8. [PubMed] [Google Scholar]
- 26. Aragão RCF, Albuquerque MFPM, Mello MJG, Ximenes RAA. Risk factors associated with death in children admitted to a paediatric intensive care unit. J Trop Pediatr. 2001;47:86–91. doi: 10.1093/tropej/47.2.86. 10.1093/tropej/47.2.86 [DOI] [PubMed] [Google Scholar]
- 27. El‐Nawawy A. Evaluation of the outcome of patients admitted to the pediatric intensive care unit in Alexandria using the pediatric risk of mortality (PRISM) score. J Trop Pediatr. 2003;49:109–14. doi: 10.1093/tropej/49.2.109. 10.1093/tropej/49.2.109 [DOI] [PubMed] [Google Scholar]
- 28. Typpo KV, Petersen NJ, Hallman M, Markovitz BP, Mariscalco M. Day 1 multiple organ dysfunction syndrome is associated with poor functional outcome and mortality in the pediatric intensive care unit. Pediatr Crit Care Med. 2009;10:562–70. doi: 10.1097/PCC.0b013e3181a64be1. 10.1097/PCC.0b013e3181a64be1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Dursun O, Hazar V, Karasu GT, Uygun V, Tosun O, Yesilipek A. Prognostic factors in pediatric cancer patients admitted to the pediatric intensive care unit. J Pediatr Hematol Oncol. 2009;31:481–4. doi: 10.1097/MPH.0b013e3181a330ef. 10.1097/MPH.0b013e3181a330ef [DOI] [PubMed] [Google Scholar]
- 30. Waiser AP, Chevret L, Essouri S, Durand P, Chevret S, Devictor D. Pneumococcal meningitis in a pediatric intensive care unit: Prognostic factors in a series of 49 children. Pediatr Crit Care Med. 2005;6:568–72. doi: 10.1097/01.pcc.0000170611.85012.01. 10.1097/01.PCC.0000170611.85012.01 [DOI] [PubMed] [Google Scholar]
- 31. Brandão MB, Lopes CE, Morcillo AM, Baracat EC. Risck factors of death in children with diarrhea and shock admitted to the intensive care unit. Rev Assoc Med Bras. 2005;51:237–40. doi: 10.1590/s0104-42302005000400022. 10.1590/S0104‐42302005000400022 [DOI] [PubMed] [Google Scholar]
- 32. Huang AR, He SJ, Jin YM, Yahg HM, Shan XO. Risk factors for death in children with septic shock. Zhongguo Dang Dai Er Ke Za Zhi. 2009;11:280–2. [PubMed] [Google Scholar]
- 33. Williams TA, Ho KM, Dobb GJ, Finn JC, Knuiman M, Webb SAR. Effect of length of stay in intensive care unit on hospital and long‐term mortality of critically ill adult patients. Br J Anaesth. 2010 doi: 10.1093/bja/aeq025. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 34. Castello FV, Cassano A, Gregory P, Hammond J. The Pediatric Risk of Mortality (PRISM) score and Injury Severity Score (ISS) for predicting resource utilization and outcome of intensive care in pediatric trauma. Crit Care Med. 1999;27:985–8. doi: 10.1097/00003246-199905000-00041. 10.1097/00003246‐199905000‐00041 [DOI] [PubMed] [Google Scholar]
- 35. Fargason CA, Langman CB. Limitations of the Pediatric Risk of Mortality score in assessing children with acute renal failure. Pediatr Nephrol. 1993;7:703–7. doi: 10.1007/BF01213327. 10.1007/BF01213327 [DOI] [PubMed] [Google Scholar]
- 36. Gérardin P, Rogier C, Leteurtre S, Jouvencel P, Ka AS, Imbert P. Evaluation of Pediatric Risk of Mortality (PRISM) scoring in African children with falciparum malaria. Pediatr Crit Care Med. 2006;7:45–7. doi: 10.1097/01.pcc.0000192321.66637.e6. 10.1097/01.PCC.0000192321.66637.e6",-1,"xxx/66637.e6 [DOI] [PubMed] [Google Scholar]
- 37. Arantes A, Carvalho ES, Medeiros EAS, Farhat CK, Mantese OC. Pediatric Risk of Mortality and hospital infection. Infect Control Hosp Epidemiol. 2004;25:783–5. doi: 10.1086/502478. 10.1086/502478 [DOI] [PubMed] [Google Scholar]
- 38. Gilio AE, Stape A, Pereira CR, Cardoso MF, Silva CV, Troster EJ. Risk factors for nosocomial infections in a critically ill pediatric population: a 25‐months prospective cohort study. Infect Control Hosp Epidemiol. 2000;21:340–2. doi: 10.1086/501770. 10.1086/501770 [DOI] [PubMed] [Google Scholar]
- 39. Pollock E, Ford‐Jones EL, Corey M, Barker G, Mindorf CM, Gold R, et al. Use of the Pediatric Risk of Mortality score to predict nosocomial infection in a pediatric intensive care unit. Crit Care Med. 1991;19:160–5. doi: 10.1097/00003246-199102000-00008. 10.1097/00003246‐199102000‐00008 [DOI] [PubMed] [Google Scholar]
- 40. Singh‐Naz N, Sprague BM, Patel KM, Pollack MM. Risk factors for nosocomial infection in critically ill children: A prospective cohort study. Crit Care Med. 1996;24:875–8. doi: 10.1097/00003246-199605000-00024. 10.1097/00003246‐199605000‐00024 [DOI] [PubMed] [Google Scholar]
- 41. Carroll CL, Goodman DM, Superina RA, Alonso EM. Pediatric risk of mortality (PRISM) scores predict outcomes in pediatric liver transplant recipients. J Pediatr Gastroenterol Nutr. 1999;29:507. doi: 10.1034/j.1399-3046.2003.00084.x. 10.1097/00005176‐199910000‐00100 [DOI] [PubMed] [Google Scholar]
- 42. Carroll CL, Goodman DM, Superina RA, Whitington PF, Alonso EM. Timed Pediatric Risk of Mortality Scores predict outcomes in pediatric liver transplant recipients. Pediatr Transplant. 2003;7:289–95. doi: 10.1034/j.1399-3046.2003.00084.x. 10.1034/j.1399‐3046.2003.00084.x [DOI] [PubMed] [Google Scholar]