Abstract
We present a case of toric implantable collamer lens (TICL) spontaneous rotation in a patient with myopic astigmatism. A 23-year-old female underwent TICL implantation. Preoperative uncorrected visual acuity (UCVA) was 20/800 and 20/1200, respectively, with −7.75 −4.25 × 0° and −8.25 −5.25 × 180°. The left eye achieved an UCVA of 20/30. After 3 months of successful implantation of TICL in the left eye, the patient presented with a sudden decrease in visual acuity in the left eye. UCVA was 20/100 with a refraction of +2.50 −4.50 × 165°. We observed the toric marks with a 30° rotation from the original position and decided to reposition the TICL, obtaining a final UCVA of 20/25, which remained stable at 6 months' follow-up. TICL can present a considerable rotation that compromises visual acuity. The relocation of TICL is a safe and effective procedure to recover visual acuity due to significant spontaneous TICL rotation.
Key Words: Astigmatism, Myopia, Rotation, Toric Implantable Collamer Lens, Intraocular lens complications
Introduction
The Visian Toric Implantable Collamer Lens (Visian TICL; STAAR Surgical, Monrovia, Calif., USA) is a foldable lens designed to correct myopia and astigmatism and is under clinical trials for United States Food and Drug Administration (FDA) approval [1, 2]. International available power varies from −3 to −23 for sphere and from +1 to +6 for cylinder. TICL rotation is considered to be around 2.06° (± 4.25°) depending on the case series [2,3,4]. There is scanty evidence about significant rotation of TICL [3]. Here we present a case of spontaneous rotation of a TICL that required repositioning to restore visual acuity.
Case Report
A 23-year-old female requested refractive surgery. Her medical and ophthalmological histories were unremarkable. The uncorrected visual acuity (UCVA) was 20/800 and 20/1200 with a refraction of −7.75 −4.25 × 0° and −8.25 −5.25 × 180°, respectively. Ophthalmological examination was normal in both eyes. We used Orbscan II (Bausch and Lomb, Salt Lake City, Utah, USA) measurements to calculate all our Toric Implantable Collamer Lens (TICL) cases. In both eyes we observed symmetric, orthogonal and enantiomorphic bow-ties in the surface maps; elevation and pachymetric maps were unremarkable (fig. 1). The anterior chamber depth (ACD) of both eyes was 3.37 and 3.42 mm. Right eye keratometric (K) values were 40.4 44.8 × 3°, and left eye keratometric values were 40.3 45.5 × 177°. White-to-white (WTW) distance was 11.6 and 11.7 mm, and central corneal thickness was 521 and 514 μm, respectively (we tended to use the thinnest value). Endothelial cell counts were 3,194 and 2,881 cells/mm2. Two weeks before surgery, 2 Nd:YAG laser iridotomies were performed on each eye. The TICL calculation software displayed model TICM120V4 with a power of −16.5 +5.5 × 91° and 18.5 +6.0 × 93°. Left eye TICL implantation software suggested rotating the TICL 3° clockwise after horizontal implantation (fig. 2A). Each eye underwent surgery on different dates; we performed the same technique in both eyes. Previous topical anesthesia marks on the 0–180° axis were performed, and then we marked the desired axis with a Mendez degree gauge (Katena Products, Inc., Denville, N.J., USA). We performed a 2.8-mm temporal clear corneal incision using a cohesive viscosurgical device to maintain ACD; 2 paracenteses, superior and inferior, were done. We injected the TICL under pharmacological mydriasis and placed the 4 haptics under the iris with a Batlle ICL manipulator (Asico LLC, Westmont, Ill., USA) and aspirated the viscosurgical device with a Simcoe cannula. Routinely, we preferred using a single 10-0 nylon suture to close the main wound; surgeries presented no incidents. We generally used a 7-day course of ciprofloxacine/dexamethasone ophthalmic solution and oral acetazolamide 250 mg tablets twice a day during 3 days. The right eye obtained a UCVA of 20/25, without any complication, and remained stable during 6 months of follow-up. On the first postoperative day, the left eye had a UCVA of 20/40 – achieving 20/30 after 1 week. The vault was ideal, around 700 μm, and the intraocular pressure was normal during follow-up. Follow-up was excellent at 1 week, 1 month and 2 months. During the third month, the patient presented as an emergency due to a sudden drop in visual acuity of the left eye in the morning after she woke up; she denied trauma or other conditions. The UCVA was 20/100 with a refraction of +2.50 −4.50 × 165°. After pupillary dilatation we observed a rotation of the TICL of approximately 35° from its original position (fig. 2B). We decided to plan the repositioning in the operating room. Under topical anesthesia, we performed a paracentesis at 1 o'clock clockwise. First using a small amount of a cohesive viscosurgical device, and then using the Batlle ICL manipulator, we realigned the TICL according to the desired axis (fig. 3). The following day we found a notable improvement with the UCVA reaching 20/25, where it remained stable during the next 6 months.
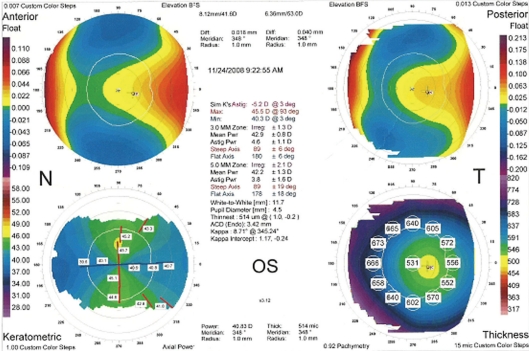
Fig. 1.
Left eye Orbscan II topography showing a symmetric and orthogonal bow-tie. Topographic values necessary for TICL calculation: keratometry K1: 40.3 at 3°, K2: 45.5 at 93°; ACD: 3.42 mm (endothelial); corneal thickness: 0.514 mm; WTW: 11.7 mm.
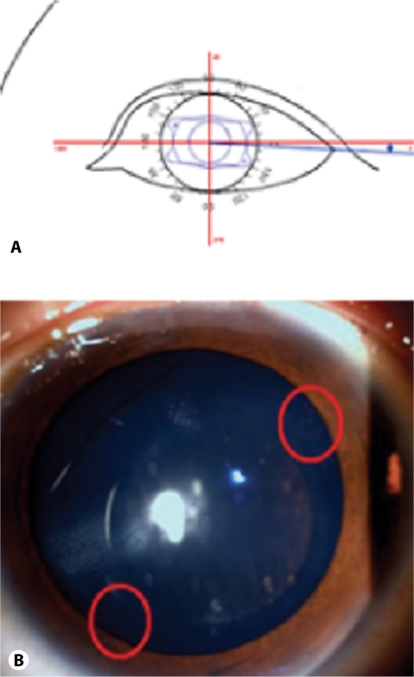
Fig. 2.
TICL software-suggested position for the left eye, the TICL model was TICM120V4 with a power of −18.5 +6.0 × 93° and overall diameter of 12.0 mm (A). Slit-lamp image showing a patent iridotomy and the TICL rotation more than 30° from its original position; red circles emphasize toric rhomboidal shape axis marks (B).
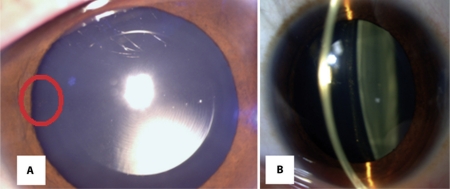
Fig. 3.
Slit-lamp image after repositioning procedure (A), notice an axis mark (circled in red) orientated as the original suggested axis. An adequate vault persisted after repositioning (B).
Discussion
It is well accepted that a rotation in the cylinder axis of more than 30° is enough to decrease the optical effect and once again achieve 100% of the cylinder power [5,6,7]. Here we presented a case of TICL spontaneous rotation of 35° from its original surgical position 3 months after surgery. In our case, the original refraction was −8.25 −5.25 × 180° achieving −0.75 −0.75 × 178°; after TICL rotation it presented as +2.50 −4.50 × 165°.
Toric intraocular lenses can provide excellent vision [1], and new designs are improving the risk of rotation. Even when studies have shown that the toric Artisan/Verisyse phakic intraocular lens did not have a significant rotation percentage [8], it can dislocate after ocular contusion [9]. Recently, there was a case report of ICL dislocation after occipital trauma [10]. In our case, the only factor mentioned by the patient, after we inquired about any precipitating factors, was that she noticed she had slept on her fist the night before the rotation. Nevertheless, ICL have shown stability even after intense trauma [11]. Another factor noticed by Kong et al. [10] was that ICL dislocation occurred in a dark room, where pupil dilatation can play an important role in ICL movement. Another hypothetical cause of rotation is that a haptic of the TICL remained slightly folded and after mechanical trauma became unfolded and changed the alignment.
In a case series of 35 eyes, Hashem et al. [3] reported a case of TICL that rotated 66°, representing significant rotation in 2.85% of the cases; that patient underwent repositioning of the TICL. In our facility we have implanted more than 250 TICL (according to our files and our distributor's database) and this case is the first case of significant rotation that we have seen, representing an average of 0.4%. Hamdi [12] presented a case of intraoperative misalignment corrected with PRK after rotation. If misalignment or rotation is found, we recommend first to realign the TICL before changing the corneal surface astigmatism with LVC, which is an irreversible process. Even though some authors showed no rotation [2, 4] of more than 30° in 240 cases, our patient presented a rotation of almost 40°.
ICL implantation has shown to be as effective as LASIK and surface ablation [13,14,15]. Although TICL is a safe, effective and excellent alternative in patients with myopic astigmatism, rotation can occur with time. However, rotation can easily be solved by repositioning the TICL.
Disclosure Statement
The authors have no proprietary interest in the materials presented herein.
Footnotes
This is an Open Access article licensed under the terms of the Creative Commons Attribution-NonCommercial-NoDerivs 3.0 License (www.karger.com/OA-license), applicable to the online version of the article only. Distribution for non-commercial purposes only.
References
- 1.Horn JD. Status of toric intraocular lenses. Curr Opin Ophthalmol. 2007;18:58–61. doi: 10.1097/ICU.0b013e328011f9bf. [DOI] [PubMed] [Google Scholar]
- 2.Sanders DR, Schneider D, Martin R, et al. Toric implantable collamer lens for moderate to high myopic astigmatism. Ophthalmology. 2007;114:54–61. doi: 10.1016/j.ophtha.2006.08.049. [DOI] [PubMed] [Google Scholar]
- 3.Hashem AN, El Danasoury AM, Anwar HM. Axis alignment and rotational stability after implantation of the toric implantable collamer lens for myopic astigmatism. J Refract Surg. 2009;25:S939–S943. doi: 10.3928/1081597X-20090915-08. [DOI] [PubMed] [Google Scholar]
- 4.Park SC, Kwun TK, Chung ES, et al. Postoperative astigmatism and axis stability after implantation of the STAAR implantable collamer lens. J Refract Surg. 2009;25:403–409. doi: 10.3928/1081597X-20090422-01. [DOI] [PubMed] [Google Scholar]
- 5.Ma JJ, Tseng SS. Simple method for accurate alignment in toric phakic and aphakic intraocular lens implantation. J Cataract Refract Surg. 2008;34:1631–1636. doi: 10.1016/j.jcrs.2008.04.041. [DOI] [PubMed] [Google Scholar]
- 6.Sanders DR, Sarver EJ. Standardized analyses of correction of astigmatism with the visian toric phakic implantable collamer lens. J Refract Surg. 2007;23:649–660. doi: 10.3928/1081-597X-20070901-03. [DOI] [PubMed] [Google Scholar]
- 7.Langenbucher A, Viestenz A, Szentmáry N, et al. Toric intraocular lenses – theory, matrix calculations, and clinical practice. J Refract Surg. 2009;25:611–622. doi: 10.3928/1081597X-20090610-07. [DOI] [PubMed] [Google Scholar]
- 8.Tehrani M, Dick HB, Schwenn O, et al. Postoperative astigmatism and rotational stability after artisan toric phakic intraocular lens implantation. J Cataract Refract Surg. 2003;29:1761–1766. doi: 10.1016/s0886-3350(03)00014-2. [DOI] [PubMed] [Google Scholar]
- 9.Güell JL, Morral M, Gris O, et al. Five-year follow-up of 399 phakic Artisan-Verisyse implantation for myopia, hyperopia, and/or astigmatism. Ophthalmology. 2008;115:1002–1012. doi: 10.1016/j.ophtha.2007.08.022. [DOI] [PubMed] [Google Scholar]
- 10.Kong J, Qin XJ, Li XY, et al. Implantable collamer lens dislocation. Ophthalmology. 2010;117:399.e1. doi: 10.1016/j.ophtha.2009.09.010. [DOI] [PubMed] [Google Scholar]
- 11.McCauley MB, Anderson DM, Johnson AJ. Posterior chamber visian implantable collamer lens: stability and evaluation following traumatic grenade explosion. J Refract Surg. 2008;24:648–651. doi: 10.3928/1081597X-20080601-17. [DOI] [PubMed] [Google Scholar]
- 12.Hamdi IM. Visual and optical performance before and after rotation of a misaligned STAAR Toric Implantable Collamer Lens. J Refract Surg. 2009;25:S934–S938. doi: 10.3928/1081597X-20090915-07. [DOI] [PubMed] [Google Scholar]
- 13.Huang D, Schallhorn SC, Sugar A, et al. Phakic intraocular lens implantation for the correction of myopia: a report by the American Academy of Ophthalmology. Ophthalmology. 2009;116:2244–2258. doi: 10.1016/j.ophtha.2009.08.018. [DOI] [PubMed] [Google Scholar]
- 14.Sanders D, Vukich JA. Comparison of implantable collamer lens (ICL) and laser-assisted in situ keratomileusis (LASIK) for low myopia. Cornea. 2006;25:1139–1146. doi: 10.1097/ICO.0b013e31802cbf3c. [DOI] [PubMed] [Google Scholar]
- 15.Schallhorn S, Tanzer D, Sanders DR, et al. Randomized prospective comparison of visian toric implantable collamer lens and conventional photorefractive keratectomy for moderate to high myopic astigmatism. J Refract Surg. 2007;23:853–867. doi: 10.3928/1081-597X-20071101-01. [DOI] [PubMed] [Google Scholar]