Abstract
Background
Studies have shown that delayed treatment of several non-hepatobiliary (HB) malignancies is associated with adverse effects on disease progression and survival. Delayed treatment of HB malignancies has not been thoroughly investigated.
Methods
We performed a retrospective institutional review of patients referred to the Hepatobiliary Surgery Service at Beth Israel Deaconess Medical Center (BIDMC) for hepatobiliary malignancies from 2002 to 2008. Primary outcomes included the time delays (TD) in patient workup. Secondary outcomes were reasons for delay as well as disparities in TD based on demographic factors.
Results
Multivariate-adjusted linear regression showed a significant trend of increasing time from presentation until referral to a HB surgeon over the 7-year period (P = 0.001). There were no differences in TD by gender, age or education level. Multivariate-adjusted linear regression showed a significant trend of increasing number of imaging tests performed prior to referral [computerized tomography (CT), magnetic resonance imaging (MRI), positron emission tomography (PET) and ultrasound and endoscopic ultrasound (US/EUS)] (P < 0.001). Multivariate-adjusted linear regression in resectable patients showed a significant difference in overall length of survival in those with a TD1 > 30 days compared with those with a TD1 (TD from presentation until referral) <30 days (P = 0.042).
Conclusions
Delays were associated with an increase in imaging studies and delays adversely affect survival in resected patients. Referring physicians are encouraged to expedite the evaluation and early referral of all patients to an HB surgeon for evaluation and treatment.
Keywords: hepatobiliary, time delay, referral
Introduction
Annually in the United States, there are approximately 15 000 new cases of hepatobiliary (HB) malignancies resulting in significant morbidity and nearly 12 000 deaths.1 Currently there is little data examining time delays (TD) in the care of patients with HB malignancies and their effects on patient outcomes. Furthermore there is no consensus on what constitutes a significant TD for cancer patients, although some expert reviews have suggested that a time between presentation and referral for definitive treatment of >30 days is unreasonable and therefore should be defined as constituting a delay in treatment.2 Delayed treatment of many non-HB malignancies is associated with negative effects on survival and disease progression.3–9 Treatment delay in hepatocellular carcinoma (HCC) of >3 months has been associated with tumour progression and decreased survival rates.10 A delay in treatment of pancreatic cancer has been associated with a lower probability of resectability.11 As surgery provides the only possibility of a cure, it is important that patients are seen for surgical assessment in a timely fashion.
Previous studies have investigated reasons for delay in cancer patients and have suggested lack of concrete follow-up times or long waiting times for investigations as several possible factors.12 While it is necessary to perform appropriate investigations to adequately assess the presence and clinical stage of hepatobiliary malignancies, these tests should not inordinately delay referral to HB surgeons so that access to potentially curative procedures can be performed. Our institution has noticed more patients presenting for surgical evaluation over 3 months after their initial presentation. The aim of the present study was to examine if there has, in fact, been an increase in TD from 2002 to 2008, to identify possible reasons for these delays and to determine if any disparities in TD based on demographic and socioeconomic factors exist.
Materials and methods
After approval from the BIDMC Institutional Review Board a retrospective review was performed on all patients (n = 350) who were referred to the Hepatobiliary Surgery Service at Beth Israel Deaconess Medical Center (BIDMC) in Boston, MA, USA, for hepatobiliary malignancies between 1 January 2002 and 31 October 2008. Patients with non-malignant diagnoses were excluded. Both patients who did not and those who did go on to receive surgical treatment were included. Patients were identified from a database maintained in the Transplant Institute. The paper charts and electronic medical records of all patients were reviewed. HP malignancies were defined as having a diagnosis of cholangiocarcinoma, pancreatic cancer, gallbladder cancer, hepatocellular carcinoma (HCC) and secondary malignant neoplasms of the liver (e.g. colon, breast, ovarian, pancreatic, etc.). We examined age, gender, race, education background, diagnosis, and number and type of imaging studies performed. The primary outcomes were TD in patient workup. TD were divided into three intervals: TD from presentation until referral (TD1), TD from referral until seen by an HB surgeon (TD2) and TD from being seen by an HB surgeon until surgery (TD3). Secondary outcomes were reasons for delay as well as disparities in TD based on demographic factors. Imaging tests were defined as computerized tomography (CT), magnetic resonance imaging (MRI), positron emission tomography (PET), ultrasound (US) and endoscopic ultrasound (EUS). The number of imaging tests (CT, MRI, PET and US/EUS) performed between presentation and referral to an HB surgeon was examined. Time between presentation and referral (TD1) >30 days was defined as constituting a delay in diagnosis. Patients who had time delay >30 days were examined to determine the reasons for delay. The reasons for delay were assigned to one of five categories: external workup, internal (BIDMC) workup, chemotherapy, medical factors and patient factors. Overall length of survival from the date of presentation was determined for all patients by both chart review and from the Social Security Death Index (SSDI) at http://www.rootsweb.com.
Statistical analyses were performed using STATA version 10.0 software (STATA Corp. College Station, TX, USA). Statistical tests included multivariate-adjusted linear regression or multivariate-adjusted logistic regression. All statistical tests adjusted for the following parameters: age, gender, race, education status and cancer diagnosis. Time delays were log-transformed in the analysis.
Results
A total of 350 patients with HB malignancies were referred to Hepatobiliary Surgery Service. Patient characteristics are summarized in Table 1. The median time from presentation until referral to an HB surgeon (TD1) by year can be seen in Fig. 1. The median TD1 over the 7-year period was 33 days. A total of 163 patients had a TD1 greater >30 days (46.6%).The median time from referral until being seen by an HB surgeon (TD2) was 6 days. The median time from being seen by an HB surgeon until surgery (TD3) was 16 days. These delays reflect patients requiring further intervention pre-operatively such as percutaneous transhepatic cholangiography for cholangiocarcinoma patients, portal vein embolization for patients undergoing extensive hepatic resection or patients on chemotherapy (e.g. Avastin) in whom a delay in surgery is necessary.
Table 1.
Patient demographics
| Age at presentation | Mean | SD | Min | Max |
|---|---|---|---|---|
| 61.1 | 12.928 | 21.95 | 89.42 | |
| N = 350 | Percent | |||
| Gender | Female | 153 | 43.71 | |
| Male | 197 | 56.29 | ||
| Race | Asian | 35 | 10 | |
| Black/African-American | 17 | 4.86 | ||
| Caucasian | 266 | 76 | ||
| Hispanic or Latino | 8 | 2.29 | ||
| Other | 4 | 1.14 | ||
| Unknown | 20 | 5.71 | ||
| Education | <High School | 20 | 5.71 | |
| High School | 63 | 18 | ||
| College | 94 | 26.86 | ||
| Graduate/Professor degree | 23 | 6.57 | ||
| Unknown | 150 | 5.71 | ||
| Diagnosis | Cholangiocarcinoma | 68 | 19.43 | |
| Intrahepatic Cholangiocarcinoma | 8 | 2.29 | ||
| Pancreatic head cancer | 32 | 9.14 | ||
| Pancreatic body cancer | 2 | 0.57 | ||
| Gallbladder cancer | 20 | 5.71 | ||
| Hepatocellular carcinoma | 83 | 23.71 | ||
| Secondary malignant neoplasm liver (colon) | 76 | 21.71 | ||
| Secondary malignant neoplasm liver (other) | 43 | 12.29 | ||
| Other | 18 | 5.14 | ||
Figure 1.
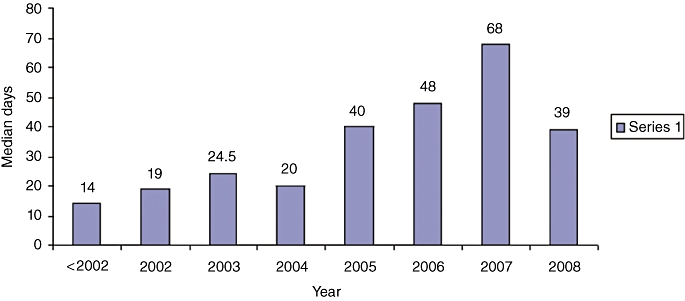
Time delay (TD) between presentation and referral to an HB surgeon (TD1) by year
Multivariate-adjusted linear regression showed a significant trend of increasing time from presentation until referral to an HB surgeon (TD1) from 2002 to 2008 (P = 0.001). Sensitivity analysis was performed by removing all extreme outliers (TD1 > 250 days) and then repeating the analysis; all significant trends were still present. There was no change in time from referral until being seen by an HB surgeon (TD2), and time from being seen by an HB surgeon until surgery (TD3) from 2002 to 2008. Non-significant trends for prediction of time delay between presentation and referral included Black/African American race (P = 0.085) and Latino race (P = 0.068). There were no significant differences in time delay by gender, age or education level. The number and types of cancer diagnosis can be seen in Table 1. There was no significant difference in TD in patients with cholangiocarcinoma, pancreatic cancer, gallbladder cancer and hepatocellular carcinoma. A secondary neoplasm of the liver was associated with an increased TD between presentation and referral (TD1) (P = 0.007).
Multivariate-adjusted linear regression showed a significant trend of increasing number of imaging tests from 2002–08 (P < 0.001). The mean number of tests by year can be seen in Fig. 2. The mean number of imaging tests per patient over the 7-year period was 2.12 (±1.14) (Table 2). The mean number of imaging tests in patients whose TD was <30 days was 1.68 (±0.899). The mean number of imaging tests in patients whose TD was >30 days was 2.52 (±1.16). The difference between these two groups was statistically different (P < 0.001).
Figure 2.
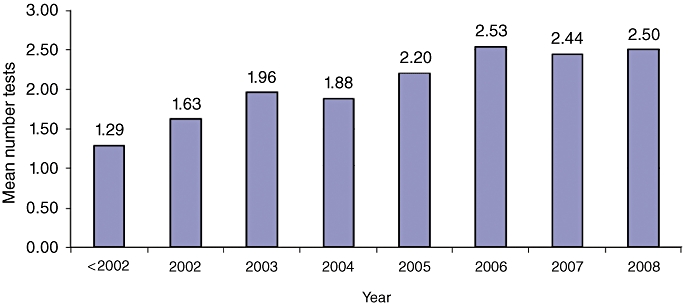
Number of imaging tests by year
Table 2.
Number of imaging tests by year
| Year | Mean number of imaging tests | SD |
|---|---|---|
| <2002 | 1.29 | 0.76 |
| 2002 | 1.63 | 1.05 |
| 2003 | 1.96 | 1.04 |
| 2004 | 1.88 | 1.00 |
| 2005 | 2.20 | 1.12 |
| 2006 | 2.53 | 1.14 |
| 2007 | 2.44 | 1.20 |
| 2008 | 2.50 | 1.21 |
| Total | 2.12 | 1.14 |
Patients who had time delay >30 days were examined to determine the reason for delay. The reason for delay was categorized into five categories: external workup, internal (internal BIDMC) workup, chemotherapy, medical factors and patient factors. When the proportion of patients within each of the five categories was compared from year to year there were no significant differences in the proportions of patients within each of the five categories, respectively.
While the proportion of patients within the external workup group did not change over the 7 years, there was a significant increase in time from presentation until referral (TD1) within this group over the 7-year period (P < 0.05). The requirement for imaging to be repeated after first being seen by an HB surgeon was examined with multivariate-adjusted logistic regression. There was no change in the odds of repeat imaging over the 7-year period.
Multivariate-adjusted logistic regression did not show a difference in the odds of resectability with increasing time from presentation until referral to an HB surgeon. Multivariate-adjusted linear regression in resectable patients showed a significant difference in survival in those with a TD1 greater than 30 days compared with those with a TD1 less than 30 days (P = 0.042). A non-significant trend of increasing stage of disease was seen in those with a TD1 greater than 30 days compared with those with a TD1 less than 30 days (P = 0.065).
Discussion
Previous guidelines have set 4 weeks as the maximum time needed to diagnose cancer after a patient presenting to their family physician.2 It is clear from our data that a significant number of patients are not being referred within this time frame and that this number of patients has increased over the past 7 years. In particular there was a noticeable jump in delay times (TD1) between 2004 and 2005. The drop in delay times from 2007 to 2008 may be a result of the fact that some patients who presented in 2008 had still not been referred on to an HPB surgeon at the time the study was conducted. This would particularly be the case for those with a long delay time.
The mean TD is longer than the median in each year, suggesting that our data is positively skewed.
Previous authors have shown that most delays in cancer diagnosis occur outside the hospital and split between general practitioner and patient delay.13 As our data shows the number of investigations being performed prior to referral has also increased over this time period and could certainly be a major contributor to this delay. Patients with delays >30 days had a statistically significant higher number of imaging tests being performed. Previous authors have suggested waiting times for investigations as a major source of delay in malignancy workup.12 Investigations are clearly necessary prior to referral particularly in patients with atypical presentations, but must be undertaken in a timely manner to avoid delay. General practitioners may feel pressure to have a definitive diagnosis prior to referral on to an HPB specialist. However, if initial scans reveal a lesion that will ultimately lead to referral, then a referral should be placed and the need for further diagnostic tests can be made by the specialist themselves.
Predetermined follow-up appointments must be made to ensure that workup is as efficient as possible and once a malignant diagnosis is likely an urgent surgical specialist referral should be made.
While delay times increased for all patients a non-significant trend of delay was evident in minorities such as Blacks and Latinos. Previous studies have found Black HCC patients have more advanced tumour stage at diagnosis and lower rates of both surgical interventions and survival.14 Delayed referral for surgery has been suggested as a possible contributor to this disparity. We did not find any difference in time delay by education status; however, we had a significant amount of missing information. Despite attempts to address inequalities in patient care it appears that there continues to be disparities in referral times by race.
TD has been shown to be correlated with disease progression in several non-HB cancers as well as with HCC and pancreatic cancer in previous studies.3–11 While the present study did not show a significant difference in resectability with longer time delay (TD1), the biological nature of the HPB tumours studied would leave one to speculate that disease progression is inevitable with lengthy delays. It is possible that our data has some unmeasured confounding as a result of the retrospective nature of this study. In those patients who were resectable, a significant difference in survival in those with a TD1 > 30 days compared with those with a TD1 < 30 days was observed. A non-significant trend of increasing stage of disease was seen in those with a TD1 > 30 days compared with those with TD1 < 30 days. It is possible, therefore, that while delays may not immediately effect resectability, they ultimately lead to reduced survival in those who are resected.
In conclusion, in our institution there has been a significant trend of increasing time from initial presentation until referral to an HB surgeon over the past 7 years. There has been an increase in the number of imaging tests prior to referral. Patients with delays >30 days had a statistically significant higher number of imaging tests being performed. A significant difference in survival in those with a TD1 > 30 days compared with those with a TD1 < 30 days has also been shown. While it is necessary to perform an investigation to adequately assess presence and stage of hepatobiliary cancer, these tests should not delay referral on to HPB surgeons so that access to potentially curative procedures can be performed. Once general practitioners determine that a patient has a lesion that will ultimately lead to referral, then a referral should be placed and the need for further diagnositic tests can be made by the specialist themselves. The information in the present study will be used to help in streamlining the time from initial presentation until referral on to HB surgeons in order to give patients the best opportunity of a cure.
Conflicts of interest
None declared.
References
- 1.Surveillance, Epidemiology, and End Results (SEER) Program. http://www.seer.cancer.gov. SEER*Stat Database [accessed January 2009]
- 2.Draft Synthesis report. Canadian Strategy for Cancer Control; 2001 Jan 18. http://www.hc-sc.gc.ca/hppb/cscc/work_reports.html[accessed January 2009]
- 3.Caplan LS, Heszlsouer KJ. Delay in breast cancer: a review of the literature. Public Heath Rev. 1992;20:187–214. –1993. [PubMed] [Google Scholar]
- 4.Sainsbury R, Johnston C, Haward B. Effect on survival of delays in referral of patients with breast cancer symptoms: a retrospective analysis. Lancet. 1999;353:1132–1135. doi: 10.1016/s0140-6736(99)02374-0. [DOI] [PubMed] [Google Scholar]
- 5.Coates AS. Breast cancer: delays, dilemmas, and delusions. Lancet. 1999;353:1112–1113. doi: 10.1016/S0140-6736(99)00082-3. [DOI] [PubMed] [Google Scholar]
- 6.Richard MA, Grob JJ, Avril MF, Delaunay M, Gouvernet J, Wolkenstein P, et al. Delay in diagnosis and melanoma prognosis: I. The role of patients. Int J Cancer. 2000;89:271–279. [PubMed] [Google Scholar]
- 7.Roncoroni L, Pietra N, Violi V, Sarli L, Choua O, Peracchia A. Delay in the diagnosis and outcome of colorectal cancer: a prospective study. Eur J Surg Oncol. 1999;25:173–178. doi: 10.1053/ejso.1998.0622. [DOI] [PubMed] [Google Scholar]
- 8.Wurtz LD, Peabody TD, Simon MA. Delay in the diagnosis and treatment of primary bone sarcoma of the pelvis. J Bone Joint Surg Am. 1999;81:317–325. doi: 10.2106/00004623-199903000-00003. [DOI] [PubMed] [Google Scholar]
- 9.Christensen ED, Harvald T, Jendresen M, Aggestrup S, Petterson G. The impact of delayed diagnosis of lung cancer on the stage at the time of operation. Eur J Cardiothorac Surg. 1997;12:880–884. doi: 10.1016/s1010-7940(97)00275-3. [DOI] [PubMed] [Google Scholar]
- 10.Huo TI, Huang YH, Chiang JH, Wu JC, Lee PC, Chi CW, et al. Survival impact of delayed treatment in patients with hepatocellular carcinoma undergoing locoregional therapy: is there a lead-time bias? Scand J Gastroenterol. 2007;42:485–492. doi: 10.1080/00365520600931402. [DOI] [PubMed] [Google Scholar]
- 11.Picozzi VJ, Delgado EC, Neil NJ, Malpass TW. Delay in diagnosis of pancreatic cancer: the experience of a tertiary referral center. 2009. Gastrointestinal Cancers Symposium.
- 12.Bjerager M, Palshof T, Dahl R, Vedsted P, Olesen F. Delay in diagnosis of lung cancer in general practice. Br J Gen Pract. 2006;56:863–868. [PMC free article] [PubMed] [Google Scholar]
- 13.Holliday HW, Hardcastle JD. Delay in diagnosis and treatment of symptomatic colorectal cancer. Lancet. 1979;1:309–311. doi: 10.1016/s0140-6736(79)90718-9. [DOI] [PubMed] [Google Scholar]
- 14.Sloane D, Chen H, Howell C. Racial disparity in primary hepatocellular carcinoma: tumor stage at presentation, surgical treatment and survival. J Natl Med Assoc. 2006;98:1934–1939. [PMC free article] [PubMed] [Google Scholar]


