Abstract
In this article, I make the case for using an integrative approach to health, broadly defined as social, emotional, mental, and physical well-being; for studying health among the young as an important marker for future health and well-being across the life course; and for understanding health disparities among the young as both causes and consequences of social stratification. An integrative approach bridges biomedical sciences with social and behavioral sciences by understanding the linkages between social, behavioral, psychological, and biological factors in health. It is furthermore vital that integration occur in all steps of the research process: in theory, design, data collection, and analysis. I use the National Longitudinal Study of Adolescent Health, or Add Health, as an example of an integrative approach to health and of the importance of adolescence and the transition to adulthood years for setting health trajectories into adulthood. Evidence is also presented on the linkages between health trajectories during adolescence and the transition to adulthood and social stratification in adulthood.
Health is and always has been a core area of population science. Although typically coupled with mortality and aging research, health is a key mechanism in reproduction, family planning, sexual behavior, birth outcomes, union formation, migration, education, and labor market behavior and outcomes. From one of the earliest demographic accounts by Louis Dublin, Alfred Lotka, and R.J. Horton in 1937 titled Twenty-Five Years of Health Progress, health remains central to the demographic processes, behaviors, and outcomes we study today.
One of the great strengths of population science is that it draws from diverse areas to solve puzzles of the time. Recently, there has been increasing scholarly interest in the puzzles of health. One indication of this is the increasing number of paper submissions to the Health and Mortality topic in the Call for Papers for the annual Population Association of America (PAA) meetings. Over the past seven years, submissions to Health and Mortality have increased by 50%—the largest growth in submissions across all topics of the PAA. What is this new interest in health, and how did it come about? I argue that it is due to five fairly recent trends: (1) more data on health; (2) increased funding for research on health; (3) a broadening of the definition of health; (4) rising research and political interest in health disparities; and (5) the aging of industrialized populations.
DATA ON HEALTH
Beginning in the 1980s, but greatly expanding in the 1990s, several demographic and social surveys broadened collection of health data, including, for example, the Panel Study of Income Dynamics (PSID), the National Longitudinal Survey of Youth (NLSY79), the Indonesian Family Life Survey (IFLS), the Los Angeles Family and Neighborhood Survey (L.A.FANS), and at the older ages, the Health and Retirement Study (HRS), the Wisconsin Longitudinal Study (WLS), National Social Life, Health and Aging Project (NSHAP), National Study of Midlife Development in the United States (MIDUS), and the Social Environment and Biomarkers of Aging Study (SEBAS). And in the mid-1990s, a new study was launched by the name of “Add Health,” or the National Longitudinal Study of Adolescent Health, developed in response to a 1993 congressional mandate to the National Institutes of Health (NIH) to fund a study of adolescent health.
In addition to the increasing number of studies with health information, data collected were more diverse and comprehensive of health status and health behaviors. For example, in addition to reports of chronic illness, disease diagnoses, and disability, Add Health collected data on safe vehicle use, sun exposure, sleep, unintentional injury, body image, eating disorders, diet and nutrition, exercise and physical activity, TV and video watching, dental health, and height and weight, in addition to some of the standards on physical and mental health, smoking, drinking, drug use, violence, suicide, and sexually transmitted infections.
FUNDING FOR RESEARCH ON HEALTH
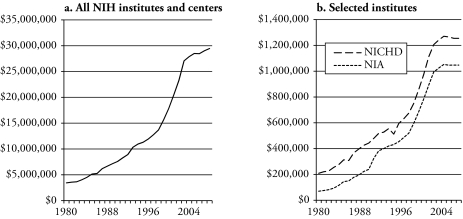
Funding for health-related research increased dramatically during the 1990s and is partly responsible for the growth in health-related data. The left panel of Figure 1 shows the increase in NIH appropriations across all institutes and centers, rising from $3.4 billion in 1980 to $29.5 billion in 2008. Much of this funding is for biomedical research, but if we focus on the two main institutes that support population research, NICHD and NIA (shown in the right panel of Figure 1), we see a similar pattern of increasing funding, especially during the 1990s.
Figure 1.
Congressional Appropriations to the National Institutes of Health (real dollars in thousands): 1980–2008
Source: Office of Budget, National Institutes of Health.
Other funding sources reflect similar increases in health-focused research. The Robert Wood Johnson Foundation is dedicated to improving the health and health care of all Americans and, in the 1990s, expanded its postdoctoral program to encourage interdisciplinary training of young scholars in the social and health sciences with their Health and Society and Health Policy Fellowship programs. The Hewlett and Gates Foundations have large population programs that focus on reproductive health and global health issues.
Although funding is not necessarily critical for health research, it certainly is needed to collect new and expanded data on health, to survey large representative samples to capture the population prevalence of lesser-known health conditions and the emergence and patterns of potential health problems, and to provide evidence on the basis of which health and social policies can be developed—all strengths of the research designs that population science brings to knowledge about health. But what do we mean by health?
DEFINITION OF HEALTH
An important change in the study of health has been a broadening of the definition of health for research and programmatic purposes. Within the social science research community in particular, the concept of health has broadened beyond the presence or absence of illness to incorporate the notion of well-being—including social, economic, and psychological well-being. This broad concept of health has roots in the World Health Organization’s 1948 definition of health: “Health is a state of complete physical, mental and social well-being and not merely the absence of disease or infirmity” (WHO 1948). In 1975, Dr. Mahler, then Director-General of WHO, argued that we must consider health in the broader context of its contribution to social development and expanded the definition to include the ability to lead a socially and economically productive life (Mahler 1975). In 1990, Evans and Stoddart critiqued the various frameworks that identify the fundamental elements of health and inform health policy. They developed a framework that incorporated biological and environmental components into the definition of health status, but focused primarily on the adult ages. A 2004 National Research Council report that was centered on children’s health proposed that child health is the extent to which individual children are able to develop and realize their potential, satisfy their needs, and develop the capacities that allow them to interact successfully with their biological, physical, and social environments.
Underlying this broadening conception of health is growing knowledge of the integral role that physical and mental health play in the causes and consequences of social and demographic behavior, social and emotional development, and social and economic status across the life course (e.g., Adler et al. 1993; Bongaarts and Potter 1983; Halfon and Hochstein 2002; Lindau et al. 2007; Palloni 2006; Waite 1995). The conceptualization of health has also expanded beyond the individual to represent the social contexts in which individuals live and social interactions within these contexts, such as healthy relationships, healthy families, healthy marriage, healthy workplace, and healthy neighborhoods (e.g., Dion 2005; Lavoie-Tremblay 2004; Sampson 2003; Smith and Christakis 2008; Waller and Swisher 2006). These applications of the notion of health to various levels of the social environment have helped identify the multiple potential sources of health disparities.
HEALTH DISPARITIES
In tandem with increasing data on health, funding for health, and embracing a broad definition of health, was dramatic growth in research on health disparities. Health disparities refer to gaps in the quality of health and health care across racial, ethnic, and socioeconomic groups (U.S. Department of Health and Human Services 2000). More broadly, the Health Resources and Services Administration defines health disparities as “population-specific differences in the presence of disease, health outcomes, or access to health care” (Goldberg, Hayes, and Huntley 2004:3).
One will quickly recognize that throughout the history of demographic scholarship, population scholars have been studying “health disparities,” focusing in particular on the most fundamental health outcome of all, death, with a rich and deep literature on mortality differentials. Indeed, Dublin et al.’s Twenty-Five Years of Health Progress (1937) analyzed deaths among the wage-earning population of the United States and Canada between the years 1911 and 1935 by cause of death, sex, age, and race. A wealth of demographic research has examined socioeconomic differentials—including income, educational, occupational, and social class differences—in mortality, and by extension morbidity and disability. And at the very origins of our discipline are life tables, and how life table parameters vary by age, sex, race, ethnicity, and socioeconomic status (Glass 1973). So, what is so new about this concept of health disparities?
Growing research interest in health disparities is due to a number of recent trends beginning in the 1990s. As mentioned previously, there are now more data on health besides death. A second important trend has been the increasing diversity of the U.S. population, fueled by the massive waves of immigration from Latin America and Asia that exploded in the 1990s (Alba and Nee 2005), increasing racial and ethnic diversity and bringing attention to health disparities among the growing minority populations in the United States. Finally, during the 1990s, there was increasing political awareness of persistent disparities by race, ethnicity, gender, and socioeconomic status as a result of the previous two trends.
In the United States, large and persistent racial, ethnic, and socioeconomic disparities in health exist across the life course (Bergner 1993; Kington and Nickens 2001; National Center for Health Statistics 2002, 2009; Pamuk et al. 1998; Rogers 1992; Williams and Collins 1995). As more evidence of the scope and persistence of such disparities across an array of health and well-being indicators filtered into the public arena throughout the 1990s, the reduction and ultimate elimination of health disparities was identified as one of the major public health goals of the decade (Satcher and Higginbotham 2008).
In 1998, President Clinton articulated this goal in the “President’s Initiative on Race” when he committed federal funds to eliminate racial and ethnic disparities in health by the year 2010. The Department of Health and Human Services incorporated the President’s Initiative in Healthy People 2010, the nation’s promotion and disease prevention strategy for the first decade of the twenty-first century, with the goal to “eliminate health disparities that occur by gender, race or ethnicity, education or income, disability, living in rural localities, or sexual orientation” (U.S. Department of Health and Human Services 2000:11).
In response to the President’s Initiative, the NIH developed its own “Program of Action to Address Health Disparities Via Research,” and by 2000, all NIH institutes had developed a research program for addressing health disparities (U.S. Department of Health and Human Services 2002). At the end of 2000, President Clinton also signed into law the establishment of the National Center on Minority Health and Health Disparities to lead, coordinate, support, and assess the NIH effort to eliminate health disparities. These cultural and political events that brought attention to minority health and health disparities and that created an infrastructure for research support have energized research in this area.
While there has been a long tradition of research documenting sex, race, and socio economic disparities in health care, health, and risk behavior, and certainly within population science, mortality, morbidity, and disability differentials, public attention to health disparities and program support for understanding how to reduce them greatly increased since the President’s Initiative. For example, a literature search on PubMed found 29 articles on the topic of “health disparities” between 1990 and 1999 (none before 1990), but 1,818 between 2000 and 2009, reflecting the impact of the President’s Initiative in 1998.
One point to note about this burgeoning research on health disparities, and on health in general, is that most of this research focuses on adult health, health among the elderly (adults over age 50), and child health (infants and children under 10 years). Much of the focus on adults and the elderly reflects the well-documented aging of industrialized populations and its consequences (Uhlenberg 2009), the fifth trend behind rising research interest in health that I noted in the introduction.1 Only about one-quarter of the articles on health disparities published in the past nine years in the PubMed search examined health among adolescents or during the transition to adulthood. The point in the life course when young people begin to make their own decisions about their health and health behavior during adolescence and early adulthood is a much less researched area and, I argue, is critical to understanding adult health and the development of social stratification trajectories across the life course.
With colleagues Udry, Gordon-Larsen, and Chantala, I published one such article in which we used data from Add Health to document trends in health disparities by race and ethnicity as young people made the transition from adolescence into young adulthood (Harris et al. 2006). We examined 20 leading health indicators identified in Healthy People 2010 as most crucial to the healthy development of young people. We used repeated measures of health and health behavior on the same individuals across time, in adolescence when the sample was aged 12–19 in 1995–1996, and six years later in young adulthood when the sample was 18–26 years old. We fit longitudinal regression models to assess the developmental trends in health indicators among racial/ethnic groups, controlling for socioeconomic status at the individual and contextual levels. This research was unique in that the trends show changes in health for the same individuals in racial and ethnic groups over time, as young people age from adolescence into early adulthood, rather than snapshots of different cohorts at a point in time.
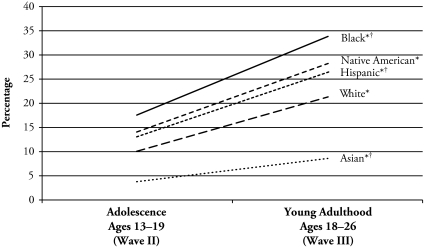
Here I show two of the more critical trends in health among young people that have important consequences for adult health. Figure 2 shows the trends in obesity among females. Obesity is measured similarly throughout this article using body mass index (BMI), calculated as measured weight in kilograms divided by measured height in meters squared. To handle the discrepant obesity definitions for adolescents and adults, the International Obesity Task Force reference is used. This reference links childhood and adolescent BMI centiles to the adult BMI cut point of 30 to determine obesity prevalence (Cole et al. 2000). In adolescence, black females have the highest rates of obesity, followed by Native American and Hispanic females, with whites and Asians having the lowest rates. As adolescents age into young adulthood, obesity increases for all ethnic groups, but more so for black, Native American, and Hispanic females than for white and especially Asian females. In addition, the disparities increase during this transition as the lines fan out.
Figure 2.
Trends in Obesity From Adolescence to Young Adulthood for Females, by Race and Ethnicity (N = 5,719)
Source: Based on data from Harris et al. (2006).
*The Wave III estimate is significantly different from the Wave II estimate (p < .05).
†The change over time is significantly different from the change for whites (p < .05).
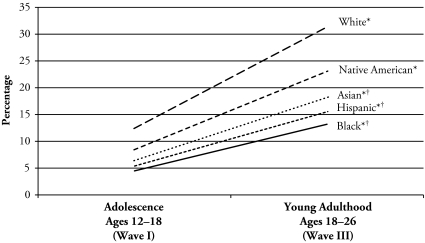
Trends in regular smoking, defined as smoking at least one whole cigarette daily during the past 30 days, are shown in Figure 3. The trends reveal a dramatic rise in smoking among young males as they transition from adolescence into young adulthood, but here white males have the highest level of smoking in adolescence, and their rate of smoking increases more so than that of the other racial and ethnic groups. Again, there is a widening of the disparities over time.
Figure 3.
Trends in Regular Smoking From Adolescence to Young Adulthood for Males, by Race and Ethnicity (N = 6,725)
Source: Based on data from Harris et al. (2006).
*The Wave III estimate is significantly different from the Wave I estimate (p < .05).
†The change over time is significantly different from the change for whites (p < .05).
These findings are indicative of a general trend of worsening health during the transition to adulthood, a result we did not expect. On the positive side, we found levels of depression, suicidal thoughts, violence, and self-reports of poor health to decline between adolescence and young adulthood. The more dominant pattern, however, was declining health. As adolescents age into their early and mid-20s, they are less likely to eat breakfast; are more likely to eat fast food, exercise less, become obese, and have no health insurance; are more likely not to get regular physical check-up, dental check-ups, or health care when needed; and are more likely to have asthma, have STDs, smoke cigarettes, use marijuana, use hard drugs, and binge drink (Harris et al. 2006). We drew two conclusions from this research. First, the transition to adulthood may be an especially critical period for setting health trajectories for the adult life course. Second, increasing disparities during this period suggest that health may be a marker for social stratification as young people move into adulthood.
HEALTH AMONG THE YOUNG
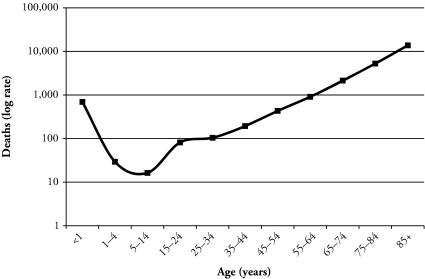
Much of health research focuses on health at the very beginning of life and the end of life, when health and mortality risks are greatest, shown in the familiar J-shaped mortality curve for all deaths in 2005 in Figure 4. This focus makes sense, but recent social, economic, developmental, and epidemiologic changes call for a better understanding of health at the point in life when young people begin to make their own decisions about their behavior and begin to choose their own environments, at the point when mortality begins to turn upward, after age 14 or so.
Figure 4.
Total Number of Deaths, by Age: United States, 2005
Source: National Vital Statistics System–Mortality, CDC/National Center for Health Statistics.
I want to make a case for the importance of the life stage of adolescence and the transition to adulthood for understanding health across the life course. Adolescence is a transitional stage of physical and mental human development that occurs between childhood and adulthood and is the point in the life course when young people begin to gain some autonomy to make decisions that impact their health. Adolescence is characterized by establishing independence from one’s parents and family, exploring new lifestyles and environments, and developing new friendships and intimate relationships (Furstenberg 2000).
As parental monitoring loosens, adolescents gain more control over their environments and select their friends and friendship networks, romantic and sexual partners, school and community activities, cultural contexts, and educational tracks. They also begin to make behavioral choices involving schoolwork and studying and how to spend leisure time in both healthy (reading, exercise, arts, safe sex) and unhealthy ways (drugs, smoking, drinking, watching TV, eating junk food, risky sex). These developmental experiences are normative and help prepare the adolescent for adulthood. However, recent decades have witnessed a lengthening in the transition from adolescence to adulthood, with important implications for health.
Transitions that typically mark the onset of adulthood—leaving home, finishing school, starting work, getting married, and having children—have been occurring at later and later ages, and in a more diverse and disordered sequence (Rindfuss 1991; Settersten, Furstenberg, and Rumbaut 2005). As a result, the transition from adolescence to adulthood has continued well into the third decade of life. As this transition has lengthened, so has the period of time during which young people continue to engage in health-risk behavior and expose themselves to health risks, with potential health consequences in adulthood (Bachman et al. 1997; Schulenberg, Maggs, and Hurrelmann 1997). Findings from our research on health disparities during the transition to adulthood provide substantial evidence of continuing and, in most cases, increased involvement in risk behavior and rising health risks as adolescents transition to adulthood (Harris et al. 2006).
At the same time that we observe these health patterns during the lengthening transition to adulthood, there is evidence that disease onset has shifted down the age spectrum into these young ages for a number of crucial health conditions. Diabetes has become more prevalent at younger and younger ages, reflecting the dramatic rise in obesity in the United States (Cook et al. 2003; Duncan 2006; Pinhas-Hamiel et al. 1996). In the past decade, diabetes has increased by 63% among 20- to 39-year-olds, compared with an increase of 22% for older ages (Centers for Disease Control and Prevention 2008; National Center for Health Statistics 2009). Hypertension and kidney disease, diseases typically associated with aging, are becoming more common among young people (Coresh et al. 2005; Muntner et al. 2004). In the past decade, hypertension increased by 30% among 20- to 34-year-old males, compared with 23% for older males; and poor kidney function increased by 49% for 20- to 39-year-olds, compared with no change for those in the adjacent 40–59 age group (National Center for Health Statistics 2009). Inactivity and lack of physical exercise historically increase with age. During the 1990s, however, the drop-off in physical exercise has migrated into the adolescent and young adult ages (Andersen et al. 1998). These changes in the social, behavioral, and epidemiologic contexts of young people’s lives will have important implications for adult health and well-being, the focus of the remainder of this article.
AN INTEGRATIVE APPROACH TO HEALTH
To understand health among the young and its implications for future health and well-being across the life course, I advocate for using an approach that bridges biomedical sciences with social and behavioral sciences by bringing together the disciplinary strengths of each. Biomedical scientists have monopolized the health field and much of the early research on health disparities because health outcomes were primarily disease-focused, with more emphasis on cure than on prevention (National Research Council 2001). As biomedical scientists began to identify some of the proximate causes of disease, there was a growing recognition of the importance of social and behavioral factors. Some examples are quite obvious: smoking increases one’s risk of lung cancer, diet is related to diabetes, and stress is an underlying factor in heart disease. Missing from biomedical science, however, were the social, psychological, and behavioral factors that influence smoking, diet, and stress.
In parallel but separate spheres of research, social scientists were building an impressive literature on the role of social factors in health. Important findings about the roles of social support (House, Landis, and Umberson 1988), neighborhood and family dis advantage (Marmot and Wilkinson 2005; Williams and Collins 2001), education (Kimbro et al. 2008), and discrimination (Williams, Neighbors, and Jackson 2003) on health outcomes demonstrate the fundamental import of the social world in health trajectories (House 2002; Marmot 2004; Williams and Jackson 2005). Missing in this research, however, are the biological mechanisms that social factors interact with or operate through to affect health.
There are always exceptions, especially in our field. Researchers who study aging, in particular, have been leaders in recognizing the importance of incorporating data and analysis of biological processes in models of aging (National Research Council 2000, 2008). But for the most part, researchers tend to work within the confines of their disciplinary theory, study designs, and data, even though the topics they study are studied by researchers in other disciplines with other but related theories and data. To break down these disciplinary barriers, we need an integrative approach, and here I acknowledge the National Academy of Sciences monograph on New Horizons in Health (National Research Council 2001), edited by Burton Singer and Carol Ryff, that spells out the various themes and strategies for achieving an integrative approach.
To understand health, broadly defined, we must understand the linkages between social, behavioral, psychological, and biological factors in health. Within these domains, integration should also occur at multiple levels of influence, at both the individual and contextual levels. To achieve these goals requires integration of these factors in all steps of the research process: in theory, design, data collection, and analysis. Finally, integration needs to occur across the life course. That is, to understand adult health, we need to understand the origins of health trajectories in early life to map out predisease pathways—defined as the biological influences and related links to behavioral, psychological, and social influences that precede morbidity and mortality.
To make my case for using an integrative approach in theory, design, data, and analysis, I will use Add Health as an example of what can be achieved with an integrative approach and to illustrate the importance of studying health among the young to identify the origins of predisease pathways. Add Health is a national longitudinal study of more than 20,000 adolescents in grades 7–12 in 1995 who have been followed into young adulthood with three follow-up waves of interviews. Waves I and II occurred in 1995–1996, when the sample was in adolescence, the majority of whom were aged 12–19; Wave III occurred in 2001–2002, when the Add Health cohort was aged 18–26 and making their transition to adulthood. The recent Wave IV was completed in 2008, when the cohort was aged 24–32 and settling into adulthood. (For more details on the design of Add Health, see Harris et al. 2009.)
THEORY AND DESIGN FOUNDATIONS OF AN INTEGRATIVE APPROACH
An integrative approach begins with theory and study design. The purpose of Add Health, as mandated by Congress, was to explore how the social contexts of adolescent life influence the health and health behavior of young people. Theory suggested that the social environment becomes especially important during adolescence as young people begin to choose their environments and spend more time outside the family setting (Furstenberg 2000; National Research Council 1993). The design of Add Health captured the theoretical sources of environmental influence by measuring key factors in the social contexts of adolescent life, including the family, peer, school, neighborhood, community, and romantic and sexual relationship. Unique to Add Health as a social and behavioral study is that it captured the social, psychological, and behavioral domains at these multiple levels, and it included the biological domain in its original design. The following sections provide a few illustrations of this integrative design.
Social
Add Health measured social, demographic, economic, and cultural factors of the individual and his and her social environment, including the family, peer, romantic and sexual relationships, school, work, neighborhood, and government and policy contexts. Reflecting a strength of population science, the Add Health design obtained independent measures of characteristics of friends and peer networks, family, school, neighborhood, and the larger community by including these clusters as part of the sampling design and not depending on self-reports of the characteristics of these contexts.
Psychological
Add Health captured the emotional, mental, and cognitive dimensions of individuals, and these factors can also be measured at the family, peer, school, and neighborhood levels. Examples of factors in the psychological domain are personality, temperament, verbal aptitude, affect, learning disabilities, future expectations, positive orientation, self-esteem, and self-efficacy.
Behavioral
Add Health focused on health and attainment behaviors, beginning in adolescence and incorporating adult behaviors as the cohort aged. Coverage includes prosocial, healthy, and health-risk behaviors; educational achievement; and demographic behavior. Behavioral factors are also measured at multiple contextual levels of the family, school, peer network, and neighborhood.
Biological
Because of the theoretical role that biology plays in health, the Add Health design included the biological domain from the start by embedding a genetic sample of over 3,000 pairs of adolescents with varying degrees of genetic resemblance, including identical and fraternal twins, full siblings, half siblings, cousins, and adolescents growing up in the same household with no biological relationship. Theory specifies that environmental effects, such as parenting or peer and neighborhood influences, on child outcomes are confounded with genetic effects because parents and children share genes, and there is increasing evidence that genes play a role in the selection of one’s social environments (Khoury, Beaty, and Cohen 1993; Plomin et al. 2001). When only the environmental effect is measured, the genetic effect is included in the estimated environmental effect. The embedded genetic sample in Add Health, however, allows researchers to parse out environmental from genetic influence on health outcomes.
In adolescence, we also included standard indicators of physical development and height and weight, from which we have been able to track body mass index and obesity into adulthood. As the Add Health cohort aged, our design continued to incorporate the biological domain that was theoretically relevant to the developmental stage of the cohort, just as we did for factors in the social, psychological, and behavioral domains. At Wave III, when the cohort was aged 18–26, the ages of highest risk for sexually transmitted infections, we collected biospecimens to test for sexually transmitted infections (STIs) and HIV. To strengthen our genetic design, we collected buccal cell DNA for molecular analysis of genetic and gene-environment interaction effects in health and health behavior.
At Wave IV, we focused on the major health risks of the cohort at this time: health-risk behavior, obesity, and stress are the leading causes of present and future disease in persons aged 24–32. Certain biological processes play roles in these diseases, and specific biomarkers can be used to characterize these processes (Crimmins and Seeman 2000). Known methods offer feasible ways of measuring these biomarkers in large, nonclinical field settings such as Add Health, and we used these methods to greatly expand the biological domain at Wave IV to obtain objective measures of health status. For example, we obtained markers of metabolic function (e.g., waist circumference, cholesterol, and blood sugar), inflammation, immune function, and cardiovascular health (blood pressure and pulse rate). We expanded our DNA collection to the entire sample and collected information about prescription medications.
This integrative approach continues to capture the key theoretical social, behavioral, psychological, and biological processes represented in the major health issues for the ages of the Add Health cohort as they progress into adulthood. Moreover, the integrative approach in theory and design allows for the integration of data to improve measurement—two aspects we care a lot about in population research. Table 1 shows prevalence estimates of hypertension and diabetes based on preliminary data collected in Wave IV of Add Health, when the sample was 24–32 years old. By combining self-reports with objective biological measures and pharmacologic data, we obtain a more valid estimate of prevalence.
Table 1.
Prevalence Estimates of Selected Health Conditions Using Survey, Biomarker, and Pharmacologic Data: Young Adults Aged 24–32
| Health Condition | Percentage |
|---|---|
| Hypertension | |
| Use medication | 3.4 |
| Self-reported | 10.6 |
| Use medication or self-reported | 11.4 |
| Use medication, self-reported, SBP ≥ 160 or DBP ≥ 100a | 13.3 |
| Use medication, self-reported, SBP ≥ 140 or DBP ≥ 90a | 24.8 |
| Diabetes | |
| Use medication | 1.4 |
| Self-reported | 2.9 |
| Use medication or self-reported | 3.2 |
| Use medication, self-reported, or glucose ≥ 200b | 3.9 |
| Use medication, self-reported, glucose ≥ 200, or HbA1c ≥ 6.5b | 6.4 |
Source: National Longitudinal Study of Adolescent Health (Wave IV).
Note: Estimates are based on preliminary unweighted Wave IV data (N ranges from 200 to 15,000).
Stage 2 hypertension is classified as SBP ≥ 160 or DBP ≥ 100; stage 1 hypertension is classified as SBP ≥ 140 or DBP ≥ 90 (Aram et al. 2003).
Random (nonfasting) glucose values ≥ 200mg/dL and HbA1c values ≥ 6.5% are cutoffs for classification of diabetes (American Diabetes Association 2007).
Self-reports of hypertension indicate that 10.6% of this adult population reported receiving a diagnosis of hypertension. When we combine this report with medication use for high blood pressure, prevalence rises slightly to 11.4%. When we combine these survey measures with objective biological measures from blood pressure (BP) readings and use standard BP cutoffs recommended by the American Heart Association, the prevalence of stage 2 hypertension rises to 13.3%; and those with stage 1 hypertension are almost one-quarter of young people aged 24–32. We see similar gains in measuring all cases with diabetes. Based on self-reports and medication use for diabetes, 3.2% are diabetic. Combining the survey data with objective biological measures of diabetes risk from glucose and glycosylated hemoglobin (HbA1c) assays on a blood drop from a finger stick, the percentage with diabetes doubles to 6.4% in the 24- to 32-year-old population.
Self-reports severely underestimate the prevalence of these serious and growing health conditions within the young adult population. Moreover, these health conditions lead to future chronic illness and disease, and with an integrative design, we have the ability to identify the social, psychological, behavioral, and biological precursors that make up predisease pathways. In the next section, I show some glimpses of these early pathways with preliminary data from Wave IV in Add Health.
PREDISEASE PATHWAYS AMONG THE YOUNG
Recent analyses of the causes of deaths in the United States indicate that the single greatest opportunity to improve health and reduce premature deaths lies in personal behavior (McGinnis and Foege 1993; Mokdad et al. 2004, 2005). Unhealthy behaviors account for 40% of premature deaths in the United States, with obesity, physical inactivity, and smoking singled out as the most prevalent behavioral causes (Mokdad et al. 2004, 2005). I now return to health during adolescence and young adulthood and focus on these particular behaviors—smoking, physical inactivity, and obesity—among young people because of their significant consequences for adult health and premature death.
Earlier, I argued that greater involvement in health-risk behavior during the prolongation of the transition to adulthood, and the creeping of health problems into the young ages, have consequences for adulthood health in two ways. First, there is substantial evidence that health tracks across the life course (Halfon and Hochstein 2002). Recall the worsening trends in health status, behavior, and health care during the transition to adulthood that I summarized earlier from our health disparities research (Harris et al. 2006). Health patterns during the transition to adulthood may set health trajectories into adulthood. Second, health during the transition to adulthood has important consequences for key social and economic outcomes, including marriage, fertility, education, occupation, and income. Health in young adulthood may increasingly become an important marker of social stratification. Below, I show some hints of these two important consequences.
HEALTH TRACKS ACROSS THE LIFE COURSE
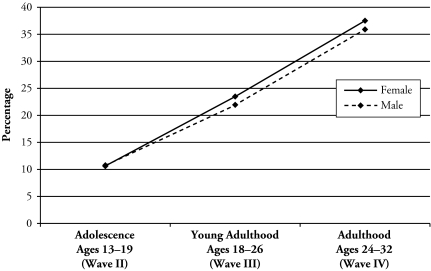
The next set of figures presents evidence of how health tracks across the life course. Figure 5 extends the trajectory of obesity that I showed earlier for the adolescent and young adulthood ages by adding the next point in adulthood at ages 24–32 for males and females in Add Health. From adolescence into young adulthood, obesity doubled from 11% to 22% for both sexes. Over the next six years, the trajectory continued its upward climb into adulthood, where obesity rose to 36% for males and 38% for females, with a slightly growing and statistically significant sex gap. These aggregate patterns are the result of both individual stability and increasing rates of entry into obesity. For example, compared with those not obese, obese adolescents are nine times more likely to be obese adults, and the rate of becoming obese increases 42% across these ages.
Figure 5.
Trends in Obesity From Adolescence to Adulthood, by Sex*
Source: Add Health data (N∼14,000–15,000 at each wave; preliminary Wave IV data).
*The sex difference in the obesity trend is significant at p < .05.
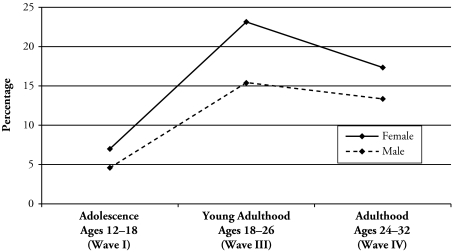
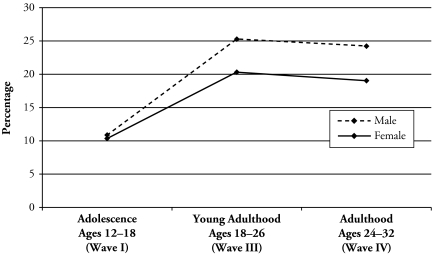
Figure 6 shows the cohort trajectory for levels of no bouts of physical activity from adolescence into adulthood by sex. Physical activity is measured using a standard physical activity behavior recall (Anderson et al. 1998). Lack of exercise, or no physical activity, is defined by self-reports of no bouts of moderate to vigorous physical activity (5–8 metabolic equivalents) per week. There is a dramatic drop-off in physical activity during the transition to young adulthood, when the percentage who get no exercise increases from 7% to 23% for females and from 5% to 15% for males. Physical activity levels improve slightly in adulthood, and the sex gap narrows somewhat but remains significant. More importantly, the relatively high levels of no exercise are set coming out of adolescence. Figure 7 presents the trends for regular smoking. Again, we see that the prevalence of smoking levels off in adulthood, but the levels are set and the significant sex disparity emerges in the transition from adolescence into young adulthood.
Figure 6.
Trends in No Bouts of Physical Activity From Adolescence to Adulthood, by Sex*
Source: Add Health data (N∼14,000–15,000 at each wave; preliminary Wave IV data).
*The sex difference in the physical inactivity trend is significant at p < .05.
Figure 7.
Trends in Regular Smoking From Adolescence to Adulthood, by Sex*
Source: Add Health data (N∼14,000–15,000 at each wave; preliminary Wave IV data).
*The sex difference in the regular smoking trend is significant at p < .05.
Two important findings come out of these data. First, the largest increase in poor health—as indicated by obesity, smoking, and lack of physical activity—occurred during the transition from adolescence into young adulthood. As young people settle into adulthood, levels of poor health behavior stabilize, with the exception of obesity, but that level is set coming out of adolescence, a vulnerable time for health in early life. Second, disparities by sex grow with age, and there is evidence of widening disparities in these health behaviors across age for other population characteristics, such as race, ethnicity, and socioeconomic status (Harris et al. 2006, 2009; Lee, Harris, and Gordon-Larsen 2009).
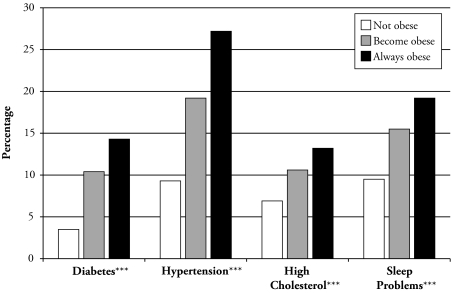
I have provided evidence that adolescence and the transition to adulthood can set health trajectories into adulthood, but do these patterns matter for general health and disease risk given that young people are generally healthy, with low prevalence of disease or chronic illness? I now turn to whether health trajectories from adolescence into young adulthood are related to health outcomes in adulthood to further explore how health tracks across the life course. In Figure 8, I examine the relationship between the obesity trajectory from adolescence into young adulthood and markers of future disease in adulthood to begin to map predisease pathways. Markers of future disease are measured in Wave IV, when the Add Health sample was 24–32 years old, by indicators of (1) diabetes, (2) hypertension, (3) high cholesterol, and (4) sleep problems. Diabetes is indicated by whether the respondent self-reported diabetes diagnosis, is taking medication for diabetes, had a random glucose assay result of 200 or greater, or had a glycosylated hemoglobin (HbA1c) assay result of 6.5 or greater (see Table 1). Hypertension is measured by self-report of hypertension diagnosis, using medication for hypertension, having a systolic blood pressure (SBP) reading greater than or equal to 160, or having a diastolic blood pressure (DBP) reading of 100 or greater (i.e., stage 2 hypertension, see Table 1). Cholesterol is measured by self-report only.2 Sleep problems are based on three questions that asked respondents whether they have trouble falling asleep once per week or more; whether they have trouble staying asleep through the night once per week or more; and whether they snore or stop breathing during sleep. Severe sleep problems are indicated by those who have all three of these problems (11%). Individual obesity trajectories from adolescence (when the Add Health cohort was aged 13–19 in Wave II) to young adulthood (when they were aged 18–26 at Wave III) are categorized into three groups: not obese (those who were never obese or lost weight, 82%); become obese (those who became obese during the transition to young adulthood, 10%); or always obese (those who were obese throughout adolescence and young adulthood, 8%).
Figure 8.
Obesity Trajectory From Adolescence to Young Adulthood Is Associated With Markers of Future Disease in Adulthood (N∼11,600)
Source: Add Health data (diabetes, hypertension, cholesterol, and sleep problems based on preliminary Wave IV data).
***The change in health outcome by obesity trajectory is significant at p < .001.
The results in Figure 8 generally show an increasing percentage that have diabetes, hypertension, high cholesterol, and sleep problems, with increasing time obese in adolescence and young adulthood. Poor metabolic function, represented by high cholesterol and diabetes, is generally uncommon for young people aged 24–32, but those who are obese as they enter adulthood, and especially those who begin their obesity trajectory in adolescence, face much higher risks of these metabolic disorders in early adulthood. The increase in hypertension is particularly dramatic among those in obese trajectories, doubling the percentage of 9.2% for those not obese to 19.2% for those becoming obese in young adulthood, and tripling the percentage to 27.2% for those obese throughout adolescence and young adulthood. The impact of obesity on quality of life and general health is furthermore seen by the increase in severe sleep problems with longer obese trajectories.
Evidence indicates that cigarette smoking and sleep problems characterize predisease pathways for cardiovascular disease risk (Young et al. 2002). Indeed, I find that smoking during adolescence and the transition to adulthood and sleep problems in adulthood are associated with hypertension in adulthood. Stage 1 hypertension (SBP ≥ 140 or DBP ≥ 90) is higher in adulthood for those who smoked regularly during adolescence and young adulthood (25.2%) and higher for those who had sleep problems (29.7%) compared with those who neither smoked nor had sleep problems (22.9%); but hypertension is highest for those who both smoked throughout the transition from adolescence into young adulthood and report sleep problems in adulthood (37.2%) (results not shown, but available on request). These descriptive relationships between health trajectories in adolescence and the transition to adulthood and markers of future disease at such an early age in adulthood forebode profound implications for future morbidity and chronic illness throughout adulthood, as well as substantial medical care costs for the individual and society as a whole.
HEALTH IS A MARKER OF SOCIAL STRATIFICATION
Finally, I end with some hints of how health trajectories from adolescence into young adulthood are associated with demographic outcomes and markers of social stratification in adulthood. Table 2 provides descriptive data on the relationships among the three behavioral trajectories of obesity, physical activity, and regular smoking from adolescence to young adulthood, with indicators of socioeconomic status and income at Wave IV in adulthood. In this table, I contrast trajectories of good or improving health3 (not obese, physically active, and not a regular smoker) with poor health (always obese, never physically active, and always a regular smoker) throughout adolescence and young adulthood. The rows for overall health in Table 2 combine these three health behavior trajectories to characterize a “good health” trajectory as having none of these health behaviors throughout adolescence and into young adulthood (representing about one-half of the sample) compared with a “poor health” trajectory with some or all of these behaviors. Social stratification measures are binary indicators of ever attended college, finished college, ever married, and home ownership, all measured at Wave IV. Income measures are presented as household income (respondent income and income of everyone in the household who contributes to the household budget), personal earnings (of those employed), and household assets (total value of respondent assets and assets of everyone in the household who contributes to the household budget).
Table 2.
Health Trajectories From Adolescence Into Young Adulthood and Associated Markers of Social Stratification in Adulthood
| Health Trajectory, Wave I–Wave III | Wave IV Socioeconomic Status (%) |
Wave IV Income Indicators (mean $) |
|||||
|---|---|---|---|---|---|---|---|
| Attended College | Finished College | Ever Married | Own Home | Household Income | Personal Earnings | Household Assets | |
| Obesity | |||||||
| Not obese | 69.3*** | 37.1*** | 48.7*** | 41.2*** | 65,894*** | 41,484*** | 93,615*** |
| Always obese | 57.4 | 20.2 | 42.2 | 31.7 | 54,064 | 34,525 | 68,916 |
| Physical Activity | |||||||
| Active | 68.5*** | 34.8*** | 49.3 | 41.3*** | 64,237*** | 40,987*** | 90,551*** |
| Never active | 51.0 | 20.2 | 51.8 | 35.6 | 52,899 | 34,179 | 68,274 |
| Smoking | |||||||
| Not regular smoker | 71.4*** | 39.4*** | 48.5*** | 41.1*** | 64,992*** | 41,561*** | 91,899*** |
| Always regular smoker | 45.5 | 8.5 | 55.7 | 44.0 | 54,899 | 33,696 | 72,212 |
| Overall Health | |||||||
| Gooda | 76.4*** | 46.5*** | 48.4 | 43.3** | 69,270 | 44,146 | 101,833*** |
| Poorb | 58.0 | 21.8 | 48.9 | 37.6 | 57,519 | 35,863 | 74,398 |
| N | 11,445 | 11,445 | 11,432 | 11,427 | 10,714 | 9,029 | 10,285 |
Source: National Longitudinal Study of Adolescent Health (Waves I–III, preliminary Wave IV data).
None of the following characteristics throughout adolescence and into young adulthood: obese, not physically active, or regular smoker.
One or more of the following characteristics throughout adolescence and into young adulthood: obese, not physically active, or regular smoker.
Significant difference at p < .01;
significant difference at p < .001.
The overall findings show a strong and significant relationship between longitudinal poor health trajectories in adolescence and through the transition to young adulthood and social and economic outcomes in adulthood. For example, compared with those who were not obese, young people who were obese during adolescence and the transition to adulthood were significantly less likely to attend college (57.4% vs. 69.3%), finish college (20.2% vs. 37.1%), ever marry (42.2% vs. 48.7%), and own their own home (31.7% vs. 41.2%) in the adulthood ages 24–32. Obesity is also associated with lower income; those who were obese from adolescence into young adulthood had lower average household income ($54,064 vs. $65,894) and personal earnings ($34,525 vs. $41,484), and substantially lower total household assets than those not obese.
Never engaging in physical activity from adolescence and into adulthood was also associated with a lower likelihood of attending college, finishing college, and owning a home, as well as lower average household income, personal earnings, and total assets compared with those who were physically active in adolescence and young adulthood. Adolescent to young adulthood trajectories of regular smoking show the same negative relationship with college attendance, college completion, and income indicators in adulthood, but have a slightly positive association with ever married and home ownership compared with the trajectory for not being a regular smoker.
Finally, longitudinal patterns of overall health based on the combination of these three health trajectories shown in the rows for overall health in the table indicate higher social status (with the exception of ever married) and income among those with “good” health trajectories (i.e., those who were not obese, were physically active, and never smoked regularly throughout adolescence and the transition to young adulthood), compared with those who experienced any of these poor health behaviors during this life stage. The overall consistency and strength of these descriptive results suggest the importance of health among the young as a marker for social stratification early in the adult life course.
CONCLUSION
I have tried to make the case for using an integrative approach to health, broadly defined as social, emotional, mental, and physical well-being; for studying health among the young as an important marker for future health and well-being across the life course; and for understanding health disparities among the young as both causes and consequences of social stratification.
I want to encourage population scientists to embrace an integrative approach in their research because population scientists bring strengths to this approach that other disciplines do not. Population training and research is inherently transdisciplinary, so these barriers are less of a problem in our field. We bring strengths in study design, measurement, data collection, and analytic tools that are required to achieve an integrative approach.
Population scientists are ideally positioned to show that behavioral and social processes have broader significance and are fundamental to a comprehensive understanding of disease etiology as well as the promotion of health and well-being. When behavioral and social sciences are implicated in health, understanding becomes less disease-focused and emphasizes the importance of “upstream” determinants of health and the opportunity to intervene, modify risk factors, and foster prevention to promote health and well-being. Incorporating the biological dimensions of health improves our understanding of the social and behavioral dimensions of health and lends credibility to our findings that biomedical scientists cannot ignore. But an integrative approach involves more than sticking biological measures in with social, psychological, and behavioral measures in our models; it is more than collecting biomarker data just because we can. An integrative approach brings together biological sciences with social and behavioral sciences in its theory and design, data collection, measurement, and analysis.
Many demographers have written about and conduct research that brings biology into our models of social and behavioral phenomena, and there are two monographs on the collection of biological data in social surveys (National Research Council 2000, 2008). In this article, I have tried to articulate this integration as a research process and to advocate for this integration in the study of health among the young. Research from Add Health suggests that an especially critical time that sets health trajectories into adulthood occurs during the transition from adolescence into young adulthood, when young people exercise more control over the selection of their social environments and make behavioral choices regarding their health. With an integrative foundation in theory and design, we will better understand the social, psychological, behavioral, and biological origins and tracking of predisease pathways that offer the promise of reducing future disease and chronic illness, as well as social and economic inequalities.
The empirical examples I have used in this article primarily focus on individual health trajectories over time and highlight the biological measures expanded in Wave IV of Add Health. Other empirical evidence from Add Health illustrates the theoretical importance of the social contexts for health trajectories that are facilitated in an integrative design. Research has documented associations with obesity for peer networks (e.g., Cohen-Cole and Fletcher 2008; Trogdon, Nonnemaker, and Pais 2008) and school context (e.g., Richmond and Subramanian 2008). Health-risk behavior is associated with peers (e.g., Cleveland and Wiebe 2003; Duncan, Harris and Boisjoly 2001), school context (Guilamo-Ramos et al. 2005), and neighborhood context (e.g., Nowlin and Colder 2007); and neighborhood effects are related to sexual behavior (Cubbin et al. 2005). Moreover, exploration of the genetic data in Add Health uncovered a gene-environment interaction of the dopamine transporter gene, DAT1, with the proportion of the high school population who had had sex by age 16 in relation to the number of lifetime sex partners (Guo, Tong, and Cai 2008). Such evidence of the role that peer, school, and neighborhood contexts play in health and health behavior early in the life course emphasizes the need to track health trajectories as young people move into and through adulthood in order to understand the enduring influence of social context as a key element of the integrative approach to health.
Add Health is not the only study with an integrative approach, and it is not the only study that allows population scholars to bridge biomedical and social sciences in their research. I mentioned just a few of the rich and innovative studies breaking ground in this area at the beginning of this article. Add Health is not the only study that begins to examine health early in the life; the recent launching of the National Children’s Study is a good example. The antecedents of predisease pathways likely begin before adolescence, in childhood, at birth, in the womb, and in the health behavior and genetic profiles of parents. To the extent that social, behavioral, psychological, and biological data can be collected retrospectively or during these critical life stages, these rich data sources will further the development and knowledge to be gained from an integrative approach for understanding health trajectories of children. Inter- and intragenerational data from the biological and extended family of origin (e.g., parents, siblings, children) will further add to the value of the integrative design, and these data are possible in Add Health and other studies. These and other exciting research opportunities are becoming available, and I expect population scholars will become the leaders in this new scientific frontier.
To quote then President-Elect Obama in a 2008 address on his goals for his science team, “The highest purpose of science is the search for knowledge, truth and a greater understanding of the world around us” (Science Team Rollout Radio Address, Chicago, IL, December 17, 2008). Bringing it all together isn’t easy. Think big, but start small and build. Putting the pieces together in an integrative approach from theory to design to data and analysis will contribute more to science than the sum of its parts; it will advance knowledge about the world around us and change the future for health research, politics, and policy.
Acknowledgments
I gratefully acknowledge research support from the National Institute of Child Health and Human Development through Grant P01 HD31921, the Add Health program project that I direct. This research uses data from Add Health, a program project designed by J. Richard Udry, Peter S. Bearman, and Kathleen Mullan Harris, and funded by Grant P01-HD31921 from the National Institute of Child Health and Human Development, with cooperative funding from 17 other agencies. Special acknowledgment is due Ronald R. Rindfuss and Barbara Entwisle for assistance in the original design.
Footnotes
I do not elaborate on this trend here because it is has been so widely documented in population science over the past 40 years.
Blood spots were collected for assay of lipids in Add Health Wave IV, but these results were not available at the time this article was prepared.
An improving health trajectory includes those who have poor health in adolescence but better health by young adulthood (e.g., obese in adolescence but not obese in young adulthood). This trajectory is relatively uncommon.
REFERENCES
- Adler NE, Boyce WT, Chesney M, Folkman S, Syme L. “Socioeconomic Inequalities in Health: No Easy Solution”. Journal of the American Medical Association. 1993;269:3140–45. [PubMed] [Google Scholar]
- Alba R, Nee V. Remaking the American Mainstream: Assimilation and Contemporary Immigration. Cambridge, MA: Harvard University Press; 2005. [Google Scholar]
- American Diabetes Association “Diagnosis and Classification of Diabetes Mellitus”. Diabetes Care. 2007;30(S1):S42–S47. doi: 10.2337/dc07-S042. [DOI] [PubMed] [Google Scholar]
- Andersen RE, Crespo CH, Bartlett SJ, Cheskin LJ, Pratt M. “Relationship of Physical Activity and Television Watching With Body Weight and Level of Fatness Among Children: Results From the Third National Health and Nutrition Examination Survey”. Journal of the American Medical Association. 1998;279:938–42. doi: 10.1001/jama.279.12.938. [DOI] [PubMed] [Google Scholar]
- Aram V, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL, Jr, Jones DW, Materson BJ, Oparil S, Wright JT, Jr, Roccella EJ, the National High Blood Pressure Education Program Coordinating Committee “Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure”. Hypertension. 2003;42:1206–52. doi: 10.1161/01.HYP.0000107251.49515.c2. [DOI] [PubMed] [Google Scholar]
- Bachman JG, Wadsworth KN, O’Malley PM, Johnson LD, Schulenberg JE. Smoking, Drinking, and Drug Use in Young Adulthood. Mahwah, NJ: Lawrence Erlbaum Associates; 1997. [Google Scholar]
- Bergner L. “Race, Health, and Health Services”. American Journal of Public Health. 1993;7:939–41. doi: 10.2105/ajph.83.7.939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bongaarts J, Potter RG. Fertility, Biology, and Behavior: An Analysis of the Proximate Determinants. New York and London: Academic Press; 1983. [Google Scholar]
- Centers for Disease Control and Prevention . National Diabetes Fact Sheet: General Information and National Estimates on Diabetes in the United States, 2007. Atlanta, GA: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention; 2008. [Google Scholar]
- Cleveland HH, Wiebe RP. “The Moderation of Adolescent-to-Peer Similarity in Tobacco and Alcohol Use by School Levels of Substance Use”. Child Development. 2003;74:279–91. doi: 10.1111/1467-8624.00535. [DOI] [PubMed] [Google Scholar]
- Cohen-Cole E, Fletcher JM. “Is Obesity Contagious? Social Networks vs. Environmental Factors in the Obesity Epidemic”. Journal of Health Economics. 2008;27:1382–87. doi: 10.1016/j.jhealeco.2008.04.005. [DOI] [PubMed] [Google Scholar]
- Cole TJ, Bellizi MC, Flegal KM, Dietz WH. “Establishing a Standard Definition for Child Overweight and Obesity Worldwide: International Survey”. British Medical Journal. 2000;320:1240–43. doi: 10.1136/bmj.320.7244.1240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cook S, Weitzman M, Auinger P, Nguyen M, Dietz WH. “Prevalence of a Metabolic Syndrome Phenotype in Adolescents”. Archives of Pediatrics & Adolescent Medicine. 2003;157:821–27. doi: 10.1001/archpedi.157.8.821. [DOI] [PubMed] [Google Scholar]
- Coresh J, Byrd-Holt D, Astor BC, Briggs JP, Eggers PW, Lacher DA, Hostetter TH. “Chronic Kidney Disease Awareness, Prevalence, and Trends Among U.S. Adults, 1999 to 2000”. American Society of Nephrology. 2005;16:180–88. doi: 10.1681/ASN.2004070539. [DOI] [PubMed] [Google Scholar]
- Crimmins EM, Seeman T. “Integrating Biology Into Demographic Research on Health and Aging.”. In: Finch CE, Vaupel JW, Kinsella K, Committee on Population, Commission on Behavioral and Social Sciences and Education, National Research Council, editors. Cells and Surveys: Should Biological Measures Be Included in Social Science Research? Washington, DC: National Academies Press; 2000. pp. 9–41. [PubMed] [Google Scholar]
- Cubbin C, Santelli J, Brindis CD, Braveman P. “Neighborhood Context and Sexual Behaviors Among Adolescents: Findings From the National Longitudinal Study of Adolescent Health”. Perspectives on Sexual and Reproductive Health. 2005;37:125–34. doi: 10.1363/psrh.37.125.05. [DOI] [PubMed] [Google Scholar]
- Dion MR. “Healthy Marriage Programs: Learning What Works”. The Future of Children. 2005;15:139–56. doi: 10.1353/foc.2005.0016. [DOI] [PubMed] [Google Scholar]
- Dublin LI, Lotka AJ, Horton RJ. Twenty-Five Years of Health Progress. New York: Metropolitan Life Insurance Company; 1937. [Google Scholar]
- Duncan GE. “Prevalence of Diabetes and Impaired Fasting Glucose Levels Among US Adolescents: National Health and Nutrition Examination Survey, 1999–2002”. Archives of Pediatrics and Adolescent Medicine. 2006;160:523–28. doi: 10.1001/archpedi.160.5.523. [DOI] [PubMed] [Google Scholar]
- Duncan GJ, Harris KM, Boisjoly J. “Sibling, Peer, Neighbor and Schoolmate Correlations as Indicators of the Importance of Context for Adolescent Development”. Demography. 2001;38:437–47. doi: 10.1353/dem.2001.0026. [DOI] [PubMed] [Google Scholar]
- Evans RG, Stoddart GL. “Producing Health, Consuming Health Care”. Social Science and Medicine. 1990;31:1347–63. doi: 10.1016/0277-9536(90)90074-3. [DOI] [PubMed] [Google Scholar]
- Furstenberg FF., Jr “The Sociology of Adolescence and Youth in the 1990s: A Critical Commentary”. Journal of Marriage and the Family. 2000;62:896–910. [Google Scholar]
- Glass DV. The Development of Population Statistics. Farnborough, England: Greg International; 1973. [Google Scholar]
- Goldberg J, Hayes W, Huntley J.2004“Understanding Health Disparities.” Background paper (November). Health Policy Institute of Ohio; Columbus, OH [Google Scholar]
- Guilamo-Ramos V, Jaccard J, Turrisi R, Johansson M. “Parental and School Correlates of Binge Drinking Among Middle School Students”. American Journal of Public Health. 2005;95:894–99. doi: 10.2105/AJPH.2003.018952. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guo G, Tong Y, Cai T. “Gene by Social-Context Interactions for Number of Sexual Partners Among White Male Youths: Genetics-Informed Sociology”. American Journal of Sociology. 2008;114(Suppl.):S36–S66. doi: 10.1086/592207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Halfon N, Hochstein M. “Life Course Health Development: An Integrated Framework for Developing Health, Policy, and Research”. The Milbank Quarterly. 2002;80:433–79. doi: 10.1111/1468-0009.00019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harris KM, Gordon-Larsen P, Chantala K, Udry JR. “Longitudinal Trends in Race and Ethnic Disparities in Leading Health Indicators From Adolescence to Young Adulthood”. Archives of Pediatrics and Adolescent Medicine. 2006;160:74–81. doi: 10.1001/archpedi.160.1.74. [DOI] [PubMed] [Google Scholar]
- Harris KM, Halpern CT, Whitsel E, Hussey J, Tabor J, Entzel P, Udry JR.2009The National Longitudinal Study of Adolescent Health: Research Design Available online at http://www.cpc.unc.edu/projects/addhealth/design
- House JS. “Understanding Social Factors and Inequalities in Health: 20th Century Progress and 21st Century Prospects”. Journal of Health and Social Behavior. 2002;43:125–42. [PubMed] [Google Scholar]
- House JS, Landis K, Umberson D. “Social Relationships and Health”. Science. 1988;241:540–45. doi: 10.1126/science.3399889. [DOI] [PubMed] [Google Scholar]
- Khoury MJ, Beaty TH, Cohen BH. Fundamentals of Genetic Epidemiology. New York: Oxford University Press; 1993. [Google Scholar]
- Kimbro RT, Bzostek S, Goldman N, Rodriguez G. “Race, Ethnicity, and the Education Gradient in Health”. Health Affairs. 2008;27:361–72. doi: 10.1377/hlthaff.27.2.361. [DOI] [PubMed] [Google Scholar]
- Kington RS, Nickens HW. “Racial and Ethnic Differences in Health: Recent Trends, Current Patterns, Future Directions.”. In: Smelser NJ, Wilson WJ, Mitchell F, editors. America Becoming: Racial Trends and Their Consequences. II. Washington, DC: National Academies Press; 2001. pp. 253–310. [Google Scholar]
- Lavoie-Tremblay M. “Creating a Healthy Workplace: A Participatory Organizational Intervention”. Journal of Nursing Administration. 2004;34:469–74. doi: 10.1097/00005110-200410000-00008. [DOI] [PubMed] [Google Scholar]
- Lee H, Harris KM, Gordon-Larsen P. “Life Course Perspectives on the Links Between Poverty and Obesity During the Transition to Young Adulthood”. Population Research and Policy Review. 2009;28:505–32. doi: 10.1007/s11113-008-9115-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lindau, Tessler S, Schumm P, Laumann EO, Levinson W, O’Muircheartaigh CA, Waite LJ. “A National Study of Sexuality and Health Among Older Adults in the U.S”. New England Journal of Medicine. 2007;357:762–74. doi: 10.1056/NEJMoa067423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mahler H. “Health for All by the Year 2000”. WHO Chronicle. 1975;29:457–61. [PubMed] [Google Scholar]
- Marmot M. Status Syndrome. London: Bloomsbury; 2004. [Google Scholar]
- Marmot M, Wilkinson RG, editors. Social Determinants of Health. Oxford: Oxford University Press; 2005. [Google Scholar]
- McGinnis JM, Foege WH. “Actual Causes of Death in the United States”. Journal of the American Medical Association. 1993;270:2207–12. [PubMed] [Google Scholar]
- Mokdad AH, Marks JS, Stroup DF, Gerberding JL. “Actual Causes of Death in the United States, 2000”. Journal of the American Medical Association. 2004;291:1238–45. doi: 10.1001/jama.291.10.1238. [DOI] [PubMed] [Google Scholar]
- Mokdad AH, Marks JS, Stroup DF, Gerberding JL. “Correction: Actual Causes of Death in the United States, 2000”. Journal of the American Medical Association. 2005;293:293–94. doi: 10.1001/jama.293.3.293. [DOI] [PubMed] [Google Scholar]
- Muntner P, He J, Cutler JA, Wildman RP, Whelton PK. “Trends in Blood Pressure Among Children and Adolescents”. Journal of the American Medical Association. 2004;291:2107–13. doi: 10.1001/jama.291.17.2107. [DOI] [PubMed] [Google Scholar]
- National Center for Health Statistics . Health, United States, 2002. Hyattsville, MD: National Center for Health Statistics; 2002. [Google Scholar]
- National Center for Health Statistics . Health, United States, 2008. Hyattsville, MD: National Center for Health Statistics; 2009. [Google Scholar]
- National Research Council 1993Losing Generations: Adolescents in High-Risk Settings. Panel on High-Risk Youth, Commission on Behavioral and Social Sciences and Education. Washington, DC: National Academies Press [Google Scholar]
- National Research Council . In: Cells and Surveys: Should Biological Measures Be Included in Social Science Research? Finch CE, Vaupel JW, Kinsella K, Committee on Population; Commission on Behavioral and Social Sciences and Education, National Research Council, editors. Washington, DC: National Academies Press; 2000. [PubMed] [Google Scholar]
- National Research Council . In: New Horizons in Health: An Integrative Approach. Singer BH, Ryff CD, Committee on Future Directions for Behavioral and Social Science Research at the National Institutes of Health, editors. Washington, DC: National Academies Press; 2001. [PubMed] [Google Scholar]
- National Research Council 2004Children’s Health, the Nation’s Wealth: Assessing and Improving Child HealthCommittee on Evaluation of Children’s Health, Board on Children, Youth, and Families.Washington, DC: National Academies Press [Google Scholar]
- National Research Council . In: Biosocial Surveys. Weinstein M, Vaupel JW, Wachter KW, Committee on Advances in Collecting and Utilizing Biological Indicators and Genetic Information in Social Science Surveys, Committee on Population, Division of Behavioral and Social Sciences and Education, editors. Washington, DC: National Academies Press; 2008. [Google Scholar]
- Nowlin PR, Colder CR. “The Role of Ethnicity and Neighborhood Poverty on the Relationship Between Parenting and Adolescent Cigarette Use”. Nicotine & Tobacco Research. 2007;9:545–56. doi: 10.1080/14622200701239613. [DOI] [PubMed] [Google Scholar]
- Palloni A. “Childhood Health and the Reproduction of Inequalities”. Demography. 2006;43:587–615. doi: 10.1353/dem.2006.0036. [DOI] [PubMed] [Google Scholar]
- Pamuk E, Makuc D, Heck K, Reuben C, Lochner K. Health, United States. Socio economic Status and Health Chartbook. Hyattsville, MD: National Center for Health Statistics; 1998. [Google Scholar]
- Pinhas-Hamiel O, Dolan LM, Daniels SR, Standiford D, Khoury PR, Zeitler P. “Increased Incidence of Non-Insulin-Dependent Diabetes Mellitus Among Adolescents”. Journal of Pediatrics. 1996;128:608–15. doi: 10.1016/s0022-3476(96)80124-7. [DOI] [PubMed] [Google Scholar]
- Plomin R, DeFries JC, McClearn GE, McGuffin P. Behavioral Genetics. 4th ed. New York: Worth Publishers; 2001. [Google Scholar]
- Richmond TK, Subramanian SV. “School Level Contextual Factors Are Associated With the Weight Status of Adolescent Males and Females”. Obesity. 2008;16:1324–30. doi: 10.1038/oby.2008.48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rindfuss RR. “The Young Adult Years: Diversity, Structural Change, and Fertility”. Demography. 1991;29:493–512. [PubMed] [Google Scholar]
- Rogers RG. “Living and Dying in the USA: Sociodemographic Determinants of Death Among Blacks and Whites”. Demography. 1992;2:287–303. [PubMed] [Google Scholar]
- Sampson RJ. “The Neighborhood Context of Well-being”. Perspectives in Biology and Medicine. 2003;46:S53–S64. [PubMed] [Google Scholar]
- Satcher D, Higginbotham EJ. “The Public Health Approach to Eliminating Disparities in Health”. American Journal of Public Health. 2008;98:400–403. doi: 10.2105/AJPH.2007.123919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schulenberg J, Maggs JL, Hurrelmann K, editors. Health Risks and Developmental Transitions During Adolescence. Cambridge: Cambridge University Press; 1997. [Google Scholar]
- Settersten RA Jr, Furstenberg FF Jr, Rumbaut RG, editors. On the Frontiers of Adulthood: Theory, Research, and Public Policy. Chicago: University of Chicago Press; 2005. [Google Scholar]
- Smith KP, Christakis NA. “Social Networks and Health”. Annual Review of Sociology. 2008;34:405–29. [Google Scholar]
- Trogdon JG, Nonnemaker J, Pais J. “Peer Effects in Adolescent Overweight”. Journal of Health Economics. 2008;27:1388–99. doi: 10.1016/j.jhealeco.2008.05.003. [DOI] [PubMed] [Google Scholar]
- Uhlenberg P, editor. International Handbook of Population Aging. Dordrecht: Springer; 2009. [Google Scholar]
- U.S. Department of Health and Human Services . Healthy People 2010: Understanding and Improving Health. Washington, DC: U.S. Government Printing Office; 2000. [Google Scholar]
- U.S. Department of Health and Human Services . National Institutes of Health Strategic Research Plan and Budget to Reduce and Ultimately Eliminate Health Disparities, Volume I, Fiscal Years 2002–2006. Washington, DC: U.S. Government Printing Office; 2002. [Google Scholar]
- Waite LJ. “Does Marriage Matter?”. Demography. 1995;32:483–508. [PubMed] [Google Scholar]
- Waller MR, Swisher R. “Fathers’ Risk Factors in Fragile Families: Implications for ‘Healthy’ Relationships and Father Involvement”. Social Problems. 2006;53:392–420. [Google Scholar]
- Williams DR, Collins C. “US Socioeconomic and Racial Differences in Health: Patterns and Explanations”. Annual Review of Sociology. 1995;21:349–86. [Google Scholar]
- Williams DR, Collins C. “Racial Residential Segregation: A Fundamental Cause of Racial Disparities in Health”. Public Health Reports. 2001;116:404–16. doi: 10.1093/phr/116.5.404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams DR, Jackson P. “Social Sources of Racial Disparities in Health”. Health Affairs. 2005;24:325–34. doi: 10.1377/hlthaff.24.2.325. [DOI] [PubMed] [Google Scholar]
- Williams DR, Neighbors HW, Jackson JS. “Racial/Ethnic Discrimination and Health: Findings From Community Studies”. American Journal of Public Health. 2003;93:200–208. doi: 10.2105/ajph.93.2.200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization (WHO) 1948Preamble to the Constitution of the World Health Organization as adopted by the International Health ConferenceNew York19–22 June, 1946; signed on 22 July 1946 by the representatives of 61 States (Official Records of the World Health Organization, No. 2, p. 100) and entered into force on 7 April 1948. [Google Scholar]
- Young T, Shahar E, Nieto FJ, Redline S, Newman AB, Gottlieb DJ, Walsleben JA, Finn L, Enright P, Samet JM. “Predictors of Sleep-Disordered Breathing in Community-Dwelling Adults: The Sleep Heart Health Study”. Archives of Internal Medicine. 2002;162:893–900. doi: 10.1001/archinte.162.8.893. [DOI] [PubMed] [Google Scholar]