Abstract
Millions of people in the United States do not have health insurance, and wide racial and ethnic disparities exist in coverage. Current research provides a limited description of this problem, focusing on the number or proportion of individuals without insurance at a single time point or for a short period. Moreover, the literature provides no sense of the joint risk of being uninsured and in need of medical care. In this article, we use a life table approach to calculate health- and insurance-specific life expectancies for whites and blacks, thereby providing estimates of the duration of exposure to different insurance and health states over a typical lifetime. We find that, on average, Americans can expect to spend well over a decade without health insurance during a typical lifetime and that 40% of these years are spent in less-healthy categories. Findings also reveal a significant racial gap: despite their shorter overall life expectancy, blacks have a longer uninsured life expectancy than whites, and this racial gap consists entirely of less-healthy years. Racial disparities in insurance coverage are thus likely more severe than indicated by previous research.
Forty-six million individuals in the United States did not have health insurance coverage in 2008 (DeNavas-Walt, Proctor, and Smith 2009), and wide racial and ethnic disparities exist in the proportion uninsured (Institute of Medicine 2001b:98; U.S. Department of Health and Human Services 2000). The consequences of being uninsured are well documented; compared with those who have health insurance, the uninsured more frequently go without needed medical care; receive lower quality care; and as a result, have worse health (Ayanian et al. 2000; Ayanian et al. 1993; Hadley 2003; Institute of Medicine 2001a, 2002a; Osteen et al. 1994; Roetzheim et al. 1999). Being uninsured also poses serious financial threats to Americans, with millions carrying a large burden of debt from medical expenses (Himmelstein et al. 2005). Although public programs—such as Medicaid and the State Children’s Health Insurance Program (SCHIP)—provide health insurance to many who would otherwise not be able to afford coverage, millions are without health insurance.
In this article, we argue that current research offers a limited description of health insurance coverage in the United States, especially with respect to racial disparities. More specifically, the literature to date does not give a sense of the duration of exposure to being uninsured over a typical lifetime, nor does it address the joint risk of being uninsured and being unhealthy. Yet, having an estimate of the duration of time that individuals typically live with these risks is essential in assessing the magnitude of the insurance-related challenges facing the United States. Moreover, having durational measures of the joint risk of being uninsured and in different health states is particularly important when examining disparities between whites and blacks because blacks are not only more likely to be uninsured but also more likely to experience adverse health events.
In this study, we use a life table approach to examine racial differences in health insurance coverage in the United States by calculating health- and insurance-specific life expectancies for whites and blacks. These measures capture the duration of exposure to different insurance and health states during a typical lifetime. In the absence of individual data on lifetime insurance coverage, life table analysis is a valuable tool that enables us to simulate life course experiences with health insurance coverage and health. By creating measures with a focus on the lifetime exposure to the joint risks of being uninsured and less healthy, we hope not only to provide a better understanding of issues related to health insurance coverage in the United States but also to elucidate racial disparities in the current U.S. health care system. Specifically, we address three important questions. First, how does the proportion of time spent in different health and insurance states over the course of one year differ by age and race? Second, given current age-specific mortality, subjective health, and health insurance rates in the United States, how many years can individuals expect to live with different types of insurance coverage and in different health states over a typical lifetime? Third, how large are the differences between blacks and whites in the expected number of years lived in different health-specific insurance states?
BACKGROUND
Health Insurance Coverage in the United States
Health insurance coverage in the United States is provided by a complex mix of public and private sources. Most Americans (62% in 2006) are covered by private health insurance obtained through their employers (Fronstin 2007). The proportion of individuals covered by employer-sponsored plans has, however, been declining since the early 1990s because of the rising cost of health insurance premiums (Fronstin 2007). Individuals who do not have access to employer-sponsored insurance may be able to purchase coverage in the private, “nongroup” market. In 2006, about 7% of individuals in the United States were insured this way (Fronstin 2000, 2007). However, individually purchased coverage is generally much more expensive than employer-sponsored coverage and, regardless of cost, is more difficult to obtain (Gabel, Hunt, and Kim 1998; Pauly and Percy 2000). Individuals who have certain chronic conditions, for example, will pay high premiums or may be denied coverage (Institute of Medicine 2001a:42).
For individuals unable to obtain private coverage either through an employer or in the private, nongroup market, a patchwork of public programs is available. These programs are generally aimed at covering the elderly, the disabled, and poor and low-income individuals with dependent children. In the 1960s, Medicare and Medicaid were created to provide health insurance for many who had been left uncovered by the expansion of employer-sponsored coverage in the preceding decades (Starr 1982). Medicare is a federal program that provides nearly universal hospital inpatient and outpatient coverage for those aged 65 and older as well as the disabled. Medicaid is a joint federal-state program that provides health insurance coverage for many poor and low-income people. In 2004, 15.6% of the U.S. noninstitutionalized population younger than age 65 was covered by Medicaid for at least part of the year.1 Finally, the State Children’s Health Insurance Program (SCHIP) is a federal program started in 1997 and designed to cover uninsured children in families with incomes that are low yet too high to qualify for Medicaid (Dubay et al. 2007). Although these public programs help mitigate some of the health and financial risks associated with not being able to obtain private insurance coverage (Currie and Thomas 1995), some studies find that those younger than age 65 with public health insurance are still disadvantaged compared with those with private health insurance coverage. For example, individuals with Medicaid are more frequently diagnosed late with certain types of cancer than those with private health insurance (Roetzheim et al. 1999).
Because the sources of health insurance coverage in the United States are so varied, complex, and generally uncoordinated, any one of a number of common life course events can easily result in an individual “falling through the cracks” of the system. For example, a loss of or change in jobs, change in income, change in marital status, change in health status, graduating from school, or simply reaching a certain age can result in losing coverage. As a result, millions of Americans are left uninsured, and the number has increased nearly every year for several decades (DeNavas-Walt et al. 2009).
The Consequences of Being Uninsured
The negative consequences of being uninsured, particularly those related to health and financial well-being, are well documented (for a review, see Institute of Medicine 2002a). Previous research has established that individuals without health insurance have poor access to medical care across a number of important indicators, including having a usual source of medical care, having at least one physician visit during a given year, and having confidence that they can obtain care when needed (Haley and Zuckerman 2000; Hoffman et al. 2001; Kasper, Giovannini, and Hoffman 2000; Nelson et al. 1999; Newacheck et al. 1998; Newacheck et al. 1999; Shi 2000; Zuvekas and Weinick 1999). Individuals without health insurance are also more likely to forgo preventive and routine care for chronic conditions (Ayanian et al. 2000). Perhaps most alarming, the uninsured are less likely to receive care for conditions that are judged by physicians to be serious and to require medical attention (Baker, Shapiro, and Schur 2000). Consequently, the uninsured are more frequently hospitalized for conditions that are potentially avoidable (Kozak, Hall, and Owings 2001; Weissman, Gatsonis, and Epstein 1992).
Individuals who do not have health insurance also incur risks to their finances. The uninsured go without the benefits of risk-pooling against expenses associated with rare or unexpected medical events. If they do require care, they are charged more by health care providers than are insured patients whose insurance carriers negotiate prices on their behalf. This greatly amplifies the financial disadvantage of being uninsured. The financial risk associated with being uninsured is substantial; 29 million Americans currently have some medical debt (Seifert and Rukavina 2006), and some estimates put the proportion of bankruptcies owing to medical debt as high as 50% (Himmelstein et al. 2005).
The negative consequences of being without health insurance extend well beyond individuals; their families and the communities in which they live are also affected. A single adverse health event of one family member can quickly drain the resources of an entire family (Institute of Medicine 2002b). Communities also pay a price for gaps in health insurance coverage of their residents. As much as 85% of uncompensated care is estimated to be paid for with public funds (Hadley and Holahan 2003). Safety-net providers, such as hospital emergency rooms and community clinics, can become overburdened in communities with large pools of uninsured and publicly insured individuals, and this can adversely affect the quality of care for all community residents (Derlet, Richards, and Kravitz 2001; Lewin Group 2002; Richards, Navarro, and Derlet 2000).
Disparities in Insurance Coverage by Race and Age
Wide differences exist across racial and ethnic groups regarding insurance coverage. Compared with non-Hispanic whites, non-Hispanic blacks are twice as likely to be uninsured, and Hispanics are three times as likely to be uninsured (Institute of Medicine 2001a:83), in part because Hispanics and blacks have experienced a disproportionate decline in employer-sponsored health insurance coverage since the 1970s (Gabel et al. 1998). Racial and ethnic minorities are also more likely to rely on public programs for their insurance coverage (Roberts 2006).
African Americans are a particularly vulnerable group when it comes to the many disadvantages of being uninsured. Not only are they more likely to be uninsured (Roberts 2006); they also have a higher risk of serious illness at any age compared with whites. Blacks have a shorter life expectancy and, on average, spend more years in ill health than whites (Hayward and Heron 1999; Kington and Smith 1997). Blacks are consequently over-represented among those who are simultaneously in poor health and uninsured or publicly insured (Wherry and Feingold 2004). This double jeopardy constitutes a vicious cycle. Blacks are less likely to have health insurance as a result of their socioeconomic position; they are more likely to have poor-paying jobs that frequently offer no health benefits and are thus less likely to be able to afford private coverage (Catanzarite 2003; McCall 2001). This socioeconomic disadvantage is, in turn, associated with higher morbidity rates, and higher morbidity coupled with higher likelihood of being uninsured make it more likely that an adverse health event will result in financial problems. Thus, socioeconomic disadvantage gives rise to poor health and inadequate health insurance coverage, which together contribute to further socioeconomic disadvantage. Some individuals caught in this negative cycle may eventually qualify for public health insurance, but not before they spend virtually all their financial resources.
Insurance coverage differs not only by race but also by age. Among the non-elderly (younger than 65), the proportion of individuals who are uninsured is the lowest in children, increases sharply until age 25, then declines thereafter (Fronstin 2007; Rhoades and Chu 2000; Rhoades and Cohen 2007). However, a substantial number of near-elderly (55–64) are without health insurance. In 1996, more than 30% of near-elderly making less than $10,000 yearly were uninsured, and the proportion without coverage dropped below 10% only for those with incomes more than $40,000 per year (Institute of Medicine 2001a:74). This reflects that transitions from full-time work to contingent work or retirement are common among this age group, and that securing private coverage in the nongroup market at older ages is difficult and expensive because of age-adjusted premiums and restrictions based on preexisting conditions. The uninsured near-elderly are of great concern because they are more likely to need medical care than other age groups not covered by Medicare. For example, average per capita medical expenditures are 30% greater for those aged 55–64 than for those aged 45–54 (Holahan 2004). Furthermore, the proximity of the near elderly to retirement makes recovery from any financial shock caused by unexpected health events more difficult than for the younger age groups.
In this article, we use a population perspective to provide a better understanding of race and age disparities. Rather than describing insurance coverage in terms of the number or proportion of individuals uncovered at any point in time or some short interval of time (as previous research has), our analysis provides estimates of health- and insurance-specific life expectancies. These estimates make it possible to contrast the duration of exposure to different health and insurance states over a typical lifetime across racial groups.
DATA AND METHODS
Sources of Data
We use two sources of data for this study. Mortality data come from published period life tables from the National Center for Health Statistics (NCHS) based on vital records for 2003 (Hoyert et al. 2006). Data on health and insurance status come from the Medical Expenditure Panel Survey (MEPS). The MEPS is a series of longitudinal surveys based on clustered and stratified samples of households that provide nationally representative estimates of health care use, insurance coverage, and sociodemographic characteristics for the U.S. civilian noninstitutionalized population (Cohen 1996, 1997). We use data covering 2004 collected in three interviews (N = 34,403). Note that the mortality data from NCHS pertain to the entire U.S. population, but MEPS data pertain only to the U.S. civilian non-institutionalized population, excluding those who are incarcerated or in institutional homes (e.g., nursing homes). Because morbidity is likely lower in the MEPS sample than in the total U.S. population, we suspect that the expected number of years lived in less-healthy states is underestimated in our life tables.
Insurance Status
We measure insurance status based on coverage information available for each month of 2004 in the MEPS. For each month, we categorize individuals as having one of the following four types of insurance as their primary source of coverage: (1) private coverage, (2) Medicaid or other non-Medicare public insurance, (3) Medicare, or (4) no coverage. Except those with Medicare, most individuals had only one type of insurance in any given month (96%). Many individuals on Medicare, however, also had private supplemental insurance. We include these individuals in the Medicare group because Medicare is generally their primary source of coverage. To create insurance- and health-specific life expectancies, we also calculate the prevalence of different health and insurance states at midyear. For these, we use the insurance status as of June. Our results are not sensitive to this choice.
Health Status
We measure health status with an indicator of subjective health. Respondents are asked to rate their health based on the question, “In general, compared to other people of your age, would you say that your health is excellent, very good, good, fair, or poor?” Previous studies demonstrate that similar subjective health measures are strongly associated with morbidity, mortality, and other more-objective health indicators across a wide variety of settings (Idler and Angel 1990; Idler and Benyami 1997; Jytha et al. 1998; Zimmer et al. 2000). More-objective indicators of health status, however, typically require health exams or assessment by medical professionals, which uninsured individuals are much less likely to obtain. Subjective health status is therefore more suitable for the purpose of this article.
Using this subjective health indicator, then, we distinguish between individuals who reported being in the healthiest two categories (excellent or very good health) and those who reported being in the three least-healthy categories (poor, fair, or good health). About 64% of the sample reported being in excellent or very good health, and 36% reported being in poor, fair, or good health. For simplicity, we refer to these groups as “healthy” and “less-healthy,” respectively. This dichotomous measure performs well as a leading indicator of medical need; individuals categorized as less-healthy in the first interview round of 2003 were 1.4 times more likely to have an emergency room visit; were three times more likely to be hospitalized; and spent, on average, $3,334 more on health care in 2004 than individuals categorized as healthy. The subjective health indicator together with the insurance status indicators enables us to identify individuals in a particularly risky category: those who are simultaneously uninsured and at a high risk of needing medical care in the near future.
We chose not to group those reporting good health into the healthy category because this would divide the sample into the healthiest 90% and the least healthy 10%. This is inappropriate for our study because the healthiest 90% of the population is likely to be extremely heterogeneous with respect to health status, containing many individuals who are not healthy and are likely to need medical care in the near future. It is the insurance status of these individuals with which we are most concerned. Therefore, dividing the sample into the healthiest 64% and the least healthy 36% makes more sense substantively. On a more practical level, dividing the sample between the healthiest 90% and the least-healthy 10%, or subdividing into smaller groups, leads to very small cell sizes when calculating insurance- and health-specific prevalence rates for each group defined by age and race. To test the sensitivity of our findings to the coding of subjective health, we reestimated all life tables by using a measure of subjective health that groups those reporting good health with those reporting very good or excellent health (available upon request). Although the expected number of years spent in the less-healthy category is much smaller for both racial groups in absolute terms when using this coding scheme, racial differences are slightly larger in relative terms. Moreover, the results from this supplemental analysis are consistent with our substantive conclusions.
Analytic Approach
Our analysis begins with a description of the proportion of time spent in different health and insurance states during one year by age and race. For each age group, we calculate the proportion of person-months spent in each insurance and health state during 2004 for blacks and whites. In the second part of our analysis, we calculate expected years remaining in life in various health and insurance states for different age groups by race using a life table approach based on the Sullivan method (Sullivan 1971). This method rests on the usual stationarity assumptions of a period life table, plus the assumption that the age-specific insurance and health prevalence rates are also stationary (Imai and Soneji 2007).
The starting point for calculating health- and insurance-specific life expectancies is abridged, race-specific period life tables constructed by using vital statistics published by NCHS. Using MEPS data, we then calculate the prevalence of different health-specific insurance states for each age interval in the life table. These prevalences are then applied to the number of person-years lived between two ages (nLx), thereby partitioning the person-years lived into different health-specific insurance states. We then complete a new life table based on the health- and insurance-specific nLx functions. To calculate age-specific prevalence rates, we use appropriate sample weights, which ensures that the health- and insurance-specific life expectancies are representative of the U.S. noninstitutionalized population. We also calculate standard errors for the different life expectancies by using the balanced repeated replications (BRR) approach, which accounts for clustering in the sample (Rust and Rao 1996; Wolter 1985).
With two health states (healthy and less-healthy) and four insurance states (private, Medicaid, Medicare, and uninsured), we define eight possible health-specific insurance states for each person in the 2004 sample. Our main outcomes of interest are the life expectancies in each of these eight health-specific insurance states.
RESULTS
Time Spent in Different Insurance and Health States
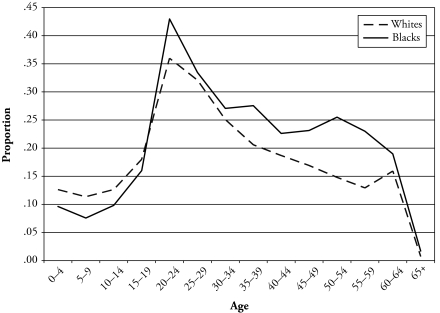
Figure 1 displays the proportion of person-months lived without health insurance by age for blacks and whites. For both races, the proportion of person-months with no insurance is lowest in childhood, increases rapidly to a peak at the 20–24 age group, and declines thereafter. This general pattern aside, there are important differences by race. Blacks younger than age 20 actually spend proportionately less time uninsured than their white counterparts. This is likely a result of the expansions in public health insurance for children in poverty during the late 1990s. Because black children are more likely to live in poor families than white children, more black children gained coverage under these expansions. After childhood, blacks spend a higher proportion of time without health insurance than whites, as shown in Figure 1. For example, blacks in the 20–24 age group spend 43% of their time, on average, without health insurance, while their white counterparts spend about 36% not covered. The racial gap generally increases with age until the 60–64 age group, after which virtually everyone becomes eligible for Medicare.
Figure 1.
Proportion of Person-Months Lived Without Health Insurance, by Age and Race
The largest difference by race occurs between the ages of 50 and 60, when the proportion of time spent uninsured diverges sharply between blacks and whites. This is important because rates of disability and ill health begin rising rapidly at these ages, but as discussed earlier, most individuals are not yet eligible for health insurance coverage through Medicare. The racial divergence in the time spent uninsured among the near-elderly is not peculiar to 2004. In fact, our preliminary analysis of data prior to 2004 showed an even more pronounced pattern (graphs for other years are available upon request).
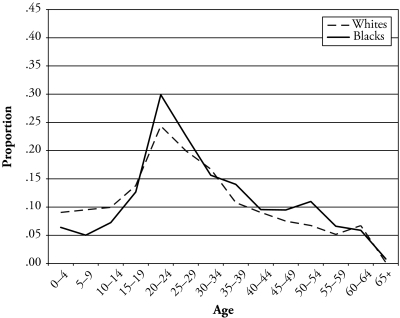
Figures 2 and 3 are analogous to Figure 1 but distinguish between time spent in the healthy state (Figure 2) and the less-healthy state (Figure 3). The overall pattern in Figure 2 showing the proportion of time spent without health insurance and in the healthy state is similar to that displayed in Figure 1. For both blacks and whites, the proportion of time spent without health insurance peaks at ages 20–24 and declines thereafter. Unlike the pattern in Figure 1, however, the racial gap in Figure 2 is concentrated between the ages of 20 and 29 and is small at subsequent ages.
Figure 2.
Proportion of Person-Months Lived Without Health Insurance and Healthy, by Age and Race
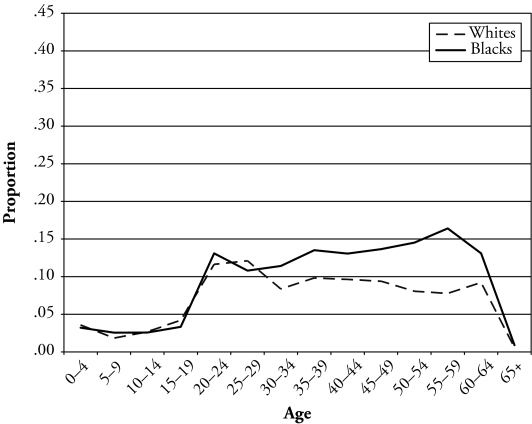
Figure 3.
Proportion of Person-Months Lived Without Health Insurance and Less Healthy, by Age and Race
The age and race patterns in Figure 3 showing the proportion of time spent uninsured and in the less-healthy state differ from those in Figure 2. Although the proportion of time spent without insurance increases rapidly with age for both races as in the other figures, it declines little or not at all after age 25. For whites, the proportion of time spent uninsured declines only a little in subsequent age groups; for blacks, the proportion of time spent uninsured actually continues to increase with age, peaking at the age group 55–59. Figure 3 thus shows that unlike the proportion of time spent uninsured and in the healthy state, the proportion of time spent uninsured and in the less-healthy state remains high into the near-elderly years, especially among blacks.
Considered together, the three figures reveal two important characteristics of insurance coverage in the United States. First, although young adults spend a disproportionate amount of time with no insurance, much of this time is spent in the healthy state. In contrast, although the near-elderly spend proportionately less time uninsured, the majority of this time is spent in the less-healthy state. Second, the largest gap between blacks and whites in the proportion of time spent uninsured occurs among the near-elderly. Thus, examining insurance coverage, age, and health status simultaneously reveals important life course patterns and racial disparities that are often overlooked. Yet, these figures do not give a sense of the duration of exposure during a typical lifetime. This is accomplished by using a life table approach, discussed in the following section.
Insurance- and Health-Specific Life Expectancies by Race
Table 1 presents health- and insurance-specific life expectancies for both blacks and whites by age. Columns 2–6 show insurance-specific life expectancies for both the healthy and less-healthy states combined. These represent the number of years that individuals can expect to live with private insurance, Medicaid, Medicare, and no insurance, if they experience the prevailing age-specific insurance rates and mortality rates during their entire lives. The results indicate that of the 77.5 years of total life expectancy at birth, one can expect to live, on average, 41.1 years with private insurance coverage, 8.1 years with Medicaid, 16.3 years with Medicare, and 12.0 years with no insurance. In relative terms, these figures imply that individuals can expect to spend 53% of their lifetimes with private insurance, 10% with Medicaid, 21% with Medicare, and 15% without health insurance.
Table 1.
Health-and Insurance-Specific Life Expectancies by Age: Total Population (years)
| Age | Total |
Healthy (excellent or very good) |
Less Healthy (poor, fair, or good) |
||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Total (ex) | Private Insurance | Medicaid | Medicare | No Insurance | Total (ex) | Private Insurance | Medicaid | Medicare | No Insurance | Total (ex) | Private Insurance | Medicaid | Medicare | No Insurance | |
| 0–4 | 77.5 | 41.1 | 8.1 | 16.3 | 12.0 | 48.5 | 29.7 | 4.9 | 6.6 | 7.3 | 29.0 | 11.4 | 3.2 | 9.7 | 4.8 |
| 5–9 | 73.1 | 39.0 | 6.4 | 16.1 | 11.6 | 44.8 | 27.7 | 3.6 | 6.5 | 6.9 | 28.3 | 11.2 | 2.8 | 9.6 | 4.7 |
| 10–14 | 68.2 | 36.1 | 4.8 | 16.1 | 11.1 | 40.7 | 25.3 | 2.5 | 6.5 | 6.4 | 27.5 | 10.9 | 2.4 | 9.6 | 4.6 |
| 15–19 | 63.2 | 33.1 | 3.6 | 16.1 | 10.5 | 36.6 | 22.6 | 1.6 | 6.5 | 6.0 | 26.6 | 10.5 | 2.0 | 9.6 | 4.5 |
| 20–24 | 58.4 | 30.1 | 2.6 | 16.1 | 9.6 | 32.9 | 20.1 | 0.9 | 6.5 | 5.3 | 25.6 | 10.0 | 1.7 | 9.6 | 4.3 |
| 25–29 | 53.7 | 27.5 | 2.1 | 16.2 | 7.9 | 29.4 | 18.0 | 0.7 | 6.6 | 4.1 | 24.3 | 9.5 | 1.4 | 9.6 | 3.8 |
| 30–34 | 48.9 | 24.6 | 1.8 | 16.2 | 6.3 | 26.1 | 15.9 | 0.5 | 6.6 | 3.1 | 22.9 | 8.8 | 1.2 | 9.6 | 3.2 |
| 35–39 | 44.2 | 21.4 | 1.4 | 16.3 | 5.1 | 22.7 | 13.5 | 0.4 | 6.6 | 2.3 | 21.5 | 7.9 | 1.0 | 9.7 | 2.8 |
| 40–44 | 39.5 | 18.0 | 1.1 | 16.3 | 4.1 | 19.8 | 11.1 | 0.3 | 6.6 | 1.7 | 19.8 | 6.9 | 0.8 | 9.7 | 2.3 |
| 45–49 | 35.0 | 14.5 | 0.9 | 16.4 | 3.2 | 16.9 | 8.7 | 0.2 | 6.7 | 1.3 | 18.1 | 5.8 | 0.7 | 9.7 | 1.9 |
| 50–54 | 30.6 | 11.0 | 0.6 | 16.5 | 2.4 | 14.4 | 6.5 | 0.1 | 6.8 | 1.0 | 16.2 | 4.6 | 0.5 | 9.7 | 1.4 |
| 55–59 | 26.3 | 7.5 | 0.4 | 16.8 | 1.6 | 12.1 | 4.4 | 0.1 | 7.0 | 0.6 | 14.3 | 3.1 | 0.4 | 9.8 | 1.0 |
| 60–64 | 22.2 | 3.9 | 0.2 | 17.2 | 1.0 | 9.9 | 2.3 | 0.0 | 7.2 | 0.4 | 12.3 | 1.5 | 0.2 | 10.0 | 0.6 |
| 65+ | 18.4 | 0.4 | 0.0 | 17.9 | 0.2 | 7.9 | 0.2 | 0.0 | 7.6 | 0.0 | 10.5 | 0.1 | 0.0 | 10.3 | 0.1 |
The 10 columns that follow show insurance-specific life expectancies separately for the two subjective health states. These results indicate that of the 77.5 years of total life expectancy, individuals can expect to spend 48.5 years in the healthy state and 29.0 years in the less-healthy state. Although they will spend the majority of the healthy years with private insurance (61%, or 29.7 of the 48.5 healthy years), only 39% of the less-healthy years will be spent with private insurance (11.4 of the 29.0 less-healthy years). Individuals can also expect to spend 4.8 years uninsured and in the less healthy state, and 3.2 years on Medicaid and in the less-healthy state.
Tables 2 and 3 present health- and insurance-specific life expectancies separately for whites and blacks, respectively. The racial differences that are statistically significant at the p < .05 level are indicated by asterisks in Table 3. All the standard errors are presented in supplemental tables that are available online (http://www.populationassociation.org/publications/demography). Tables 2 and 3 reveal significant racial differences in total life expectancy, healthy life expectancy, and health- and insurance-specific life expectancies for most age groups.
Table 2.
Health- and Insurance-Specific Life Expectancies by Age: Whites (years)
| Age | Total |
Healthy (excellent or very good) |
Less Healthy (poor, fair, or good) |
||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Total (ex) | Private Insurance | Medicaid | Medicare | No Insurance | Total (ex) | Private Insurance | Medicaid | Medicare Insurance | No | Total (ex) | Private Insurance | Medicaid | Medicare | No Insurance | |
| 0–4 | 78.0 | 42.8 | 7.0 | 16.4 | 11.8 | 49.6 | 31.3 | 4.2 | 6.8 | 7.2 | 28.4 | 11.5 | 2.7 | 9.6 | 4.6 |
| 5–9 | 73.5 | 40.5 | 5.4 | 16.2 | 11.3 | 45.8 | 29.2 | 3.1 | 6.7 | 6.8 | 27.7 | 11.3 | 2.4 | 9.5 | 4.5 |
| 10–14 | 68.5 | 37.5 | 4.0 | 16.2 | 10.8 | 41.6 | 26.6 | 2.0 | 6.7 | 6.3 | 26.9 | 11.0 | 2.0 | 9.5 | 4.5 |
| 15–19 | 63.6 | 34.2 | 3.0 | 16.2 | 10.2 | 37.5 | 23.7 | 1.3 | 6.7 | 5.8 | 26.1 | 10.6 | 1.7 | 9.5 | 4.3 |
| 20–24 | 58.8 | 31.1 | 2.2 | 16.2 | 9.3 | 33.7 | 21.1 | 0.8 | 6.7 | 5.2 | 25.1 | 10.0 | 1.4 | 9.5 | 4.1 |
| 25–29 | 54.1 | 28.4 | 1.8 | 16.3 | 7.6 | 30.2 | 18.8 | 0.6 | 6.7 | 4.0 | 23.9 | 9.5 | 1.2 | 9.5 | 3.6 |
| 30–34 | 49.3 | 25.4 | 1.5 | 16.3 | 6.1 | 26.8 | 16.6 | 0.5 | 6.8 | 3.0 | 22.4 | 8.8 | 1.0 | 9.6 | 3.0 |
| 35–39 | 44.5 | 22.0 | 1.2 | 16.4 | 4.9 | 23.4 | 14.1 | 0.3 | 6.8 | 2.2 | 21.1 | 7.9 | 0.9 | 9.6 | 2.7 |
| 40–44 | 39.8 | 18.5 | 0.9 | 16.4 | 3.9 | 20.4 | 11.6 | 0.2 | 6.8 | 1.7 | 19.4 | 6.9 | 0.7 | 9.6 | 2.2 |
| 45–49 | 35.2 | 15.0 | 0.7 | 16.5 | 3.0 | 17.5 | 9.2 | 0.1 | 6.9 | 1.3 | 17.8 | 5.8 | 0.6 | 9.6 | 1.7 |
| 50–54 | 30.8 | 11.4 | 0.6 | 16.6 | 2.2 | 14.9 | 6.8 | 0.1 | 7.0 | 0.9 | 15.9 | 4.6 | 0.4 | 9.6 | 1.3 |
| 55–59 | 26.5 | 7.7 | 0.4 | 16.9 | 1.5 | 12.4 | 4.6 | 0.1 | 7.2 | 0.6 | 14.0 | 3.1 | 0.3 | 9.7 | 0.9 |
| 60–64 | 22.3 | 4.0 | 0.2 | 17.3 | 0.9 | 10.2 | 2.5 | 0.0 | 7.4 | 0.4 | 12.1 | 1.5 | 0.1 | 9.9 | 0.6 |
| 65+ | 18.5 | 0.4 | 0.0 | 17.9 | 0.1 | 8.1 | 0.2 | 0.0 | 7.8 | 0.0 | 10.4 | 0.1 | 0.0 | 10.2 | 0.1 |
Table 3.
Health- and Insurance-Specific Life Expectancies by Age: Blacks (years)
| Age | Total |
Healthy (excellent or very good) |
Less Healthy (poor, fair, or good) |
||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Totala (ex) | Private Insurance | Medicaid | Medicare | No Insurance | Total (ex) | Private Insurance | Medicaid | Medicare | No Insurance | Total (ex) | Private Insurance | Medicaid | Medicare | No Insurance | |
| 0–4 | 72.7 | 30.3* | 14.5* | 14.3* | 13.6* | 40.6* | 19.8* | 8.6* | 4.5* | 7.7 | 32.1* | 10.5 | 5.9* | 9.8 | 6.0* |
| 5–9 | 68.9 | 29.2* | 12.0* | 14.3* | 13.4* | 37.3* | 18.7* | 6.7* | 4.5* | 7.4 | 31.6* | 10.6 | 5.2* | 9.8 | 6.0* |
| 10–14 | 63.9 | 27.4* | 9.3* | 14.3* | 13.0* | 33.4* | 17.1* | 4.7* | 4.5* | 7.1 | 30.5* | 10.3 | 4.6* | 9.8 | 5.9* |
| 15–19 | 59.0 | 25.3* | 6.9* | 14.3* | 12.5* | 29.6* | 15.4* | 3.0* | 4.5* | 6.8* | 29.4* | 10.0 | 3.9* | 9.8 | 5.7* |
| 20–24 | 54.2 | 23.1* | 5.1* | 14.2* | 11.8* | 26.1* | 13.6* | 1.8* | 4.4* | 6.2* | 28.2* | 9.5 | 3.3* | 9.8 | 5.6* |
| 25–29 | 49.6 | 21.2* | 4.2* | 14.3* | 9.8* | 22.9* | 12.3* | 1.4* | 4.5* | 4.8* | 26.7* | 8.9 | 2.8* | 9.9 | 5.0* |
| 30–34 | 45.0 | 19.1* | 3.6* | 14.2* | 8.2* | 19.9* | 10.8* | 1.1* | 4.5* | 3.6 | 25.1* | 8.3 | 2.5* | 9.7 | 4.6* |
| 35–39 | 40.4 | 16.4* | 3.0* | 14.3* | 6.8* | 17.0* | 9.0* | 0.8* | 4.5* | 2.8 | 23.4* | 7.5 | 2.1* | 9.8 | 4.0* |
| 40–44 | 36.0 | 13.7* | 2.4* | 14.3* | 5.5* | 14.3* | 7.0* | 0.6* | 4.5* | 2.1 | 21.7* | 6.7 | 1.8* | 9.8 | 3.4* |
| 45–49 | 31.6 | 11.0* | 1.8* | 14.5* | 4.4* | 11.9* | 5.3* | 0.4* | 4.6* | 1.6 | 19.8* | 5.8 | 1.4* | 9.8 | 2.8* |
| 50–54 | 27.6 | 8.1* | 1.3* | 14.7* | 3.5* | 9.8* | 3.6* | 0.2 | 4.7* | 1.3 | 17.8* | 4.5 | 1.1* | 10.0 | 2.2* |
| 55–59 | 23.8 | 5.5* | 0.9* | 15.0* | 2.3* | 8.3* | 2.6* | 0.1 | 4.9* | 0.8 | 15.5* | 3.0 | 0.8* | 10.1 | 1.6* |
| 60–64 | 20.2 | 2.9* | 0.5* | 15.6* | 1.2 | 6.8* | 1.3* | 0.0 | 5.1* | 0.4 | 13.4* | 1.6 | 0.5* | 10.4 | 0.8 |
| 65+ | 17.0 | 0.2 | 0.1 | 16.3* | 0.3 | 5.8* | 0.1 | 0.0 | 5.5* | 0.1 | 11.2 | 0.1 | 0.1* | 10.8 | 0.2 |
Total life expectancy is based on population data, and therefore statistical significance is not indicated.
Significantly different from whites at p < .05.
Comparing total and healthy life expectancies at birth by race shows that even though overall life expectancy is 5.3 years shorter for blacks than for whites (72.7 vs. 78.0), blacks live four more years in the less-healthy state (32.1 vs. 28.4). Racial differences in health-specific life expectancies are statistically significant for all age groups. Significant racial differences also exist in the insurance-specific life expectancies. The expected number of years on Medicaid at birth is substantially larger for blacks than whites (14.5 vs. 7.0), as is the number of years with no insurance (13.6 vs. 11.8), but the number of years spent with private insurance is considerably smaller for blacks than for whites (30.3 vs. 42.8). Differences are statistically significant for all but the final one or two age groups. For example, even at ages 50–54, the remaining years of life expected to be spent uninsured is 3.5 years for blacks compared with 2.2 years for whites.
Tables 2 and 3 thus show blacks to be at a significant disadvantage compared with whites with respect to both subjective health and health insurance coverage. To fully understand this disadvantage, however, we must consider health and insurance status simultaneously. The last 10 columns in Tables 2 and 3 enable this. No significant difference exists between blacks and whites in the expected number of years at birth spent uninsured and healthy (7.7 vs. 7.2, respectively), but the expected number of years spent uninsured and in the less-healthy state is significantly higher for blacks (6.0 vs. 4.6). Moreover, racial differences in the years spent uninsured and in the less-healthy state remain statistically significant for all but the last two age groups. For example, even in the 55–59 age group, blacks can expect to live 1.6 years without health insurance while in the less-healthy state, twice as much time as their white counterparts. These findings reveal an important characteristic of the racial difference in uninsured life expectancy; the difference between blacks and whites in the expected number of years spent without insurance during a typical lifetime is made up almost entirely of less-healthy years. As discussed earlier, these years represent a disproportionate amount of health and financial risk to individuals as well as a large burden on family and community resources.
DISCUSSION
The large and growing number of Americans without health insurance is a social problem that has been documented in numerous studies, government reports, and news articles. The statistics most often cited, however, provide only a limited picture of this critical problem. Lapses in health coverage are often long-term and can occur across the life course, but conventional statistics typically give no sense of the duration of exposure to being uninsured. Furthermore, although being uninsured carries high health and financial risks to everyone, the risks are particularly high for those who are not healthy and who are thus likely to need medical care. Using a life table approach, we address these issues by providing estimates of the number of years that blacks and whites spend during a typical lifetime with different types of health insurance coverage and in different health states, given prevailing age-specific rates of mortality, subjective health, and insurance coverage.
Our analyses reveal several important patterns in health insurance coverage. First, we find that Americans, on average, can expect to spend well over a decade (12.0 years) without health insurance during their lives, which amounts to more than 15% of the typical lifetime. Furthermore, 4.8 of these years (40%) are spent in the less-healthy state (as we defined it: the three lowest subjective health categories). Individuals in these lower subjective health categories are much more likely to require medical care in the following year than those reporting higher subjective health (according to our supplemental analyses). Thus, lack of insurance coverage poses especially serious risks to them.
Second, our analysis on the health- and insurance-specific life expectancies sheds light on the nature of racial disparities in insurance coverage. Despite their shorter overall life expectancy, blacks have a longer uninsured life expectancy than whites. Moreover, the racial gap in uninsured years consists almost entirely of less-healthy years. The health insurance gap between whites and blacks is therefore potentially more severe than indicated by previous research.
Finally, the life table results, together with the age-specific insurance and health proportions, suggest that the near-elderly are a key subgroup to target both for reducing the exposure to the joint risk of being uninsured and less healthy as well as for reducing disparities between whites and blacks. Although young adults spend a great deal of time uninsured and contribute disproportionately to the total uninsured life expectancy, this time is mostly spent in the healthy state. In contrast, the near-elderly spend proportionately less time uninsured, but the majority of this time is spent in the less-healthy state. Furthermore, the largest gap between blacks and whites in the time spent uninsured occurs among the near-elderly, and this gap consists primarily of time spent in the less-healthy state.
Although this study provides a useful description of health insurance coverage in the United States, our results must be interpreted with several limitations in mind. First, our approach depends on the stationarity assumptions common to all period life tables and the assumption that age-specific insurance proportions are also stationary. In supplemental analysis using data for the four preceding years (1999–2003), we found little variance in age-specific insurance proportions across years, lending tentative support to the stationarity of insurance proportions. Nevertheless, insurance proportions are sensitive to economic and policy changes to a much greater degree than morbidity and mortality rates; therefore, the assumptions made in this study are particularly strong. One alternative approach that does not require the stationarity assumptions is to calculate multistate life tables. This approach, however, rests on other strong and untestable assumptions pertaining to the underlying transition probabilities (Imai and Soneji 2007). Another approach is to use a true cohort life table method as described in Imai and Soneji (2007). Findings from such an analysis, however, would pertain to specific cohorts rather than a hypothetical cohort representing current age-specific mortality, morbidity, and insurance rates. Still, these alternative methods may provide distinct insight into the challenges facing the United States regarding insurance coverage and are worth exploring in future research.
A second limitation is that like most life table analyses, our results are descriptive and should not be viewed as causal. We cannot say, for example, whether or to what extent being uninsured for many years reduces one’s life expectancy nor how having private insurance throughout one’s life affects life expectancy. A growing literature suggests that insurance coverage does have an influence on morbidity and mortality (Institute of Medicine 2002a), but quantifying this causal effect is not the aim of our study.
Another important limitation is that the only published race-specific period life tables currently available in the United States are for whites and blacks (Arias 2002), and therefore our analysis focuses on disparities between these two groups regardless of Hispanic ethnicity. Hispanics, however, are more disadvantaged than either non-Hispanic blacks or non-Hispanic whites with respect to health insurance coverage. Because most Hispanics identify themselves as white, differences between whites and blacks in the expected number of years spent without health insurance reported here are probably smaller than if we were to conduct an analysis with Hispanics as a separate group. As better vital statistics become available for Hispanics, a more inclusive and thorough description of racial and ethnic gaps in the expected number of years spent with different insurance types and in different health states will be possible and should be undertaken.
These limitations notwithstanding, by focusing on the joint risk of being uninsured and less healthy, and by developing measures for the duration of exposure to different subjective health and health insurance states over a typical lifetime, our analysis deepens current understanding of the health insurance coverage problem in the United States. Our results also point to several important questions for future research. What are the costs associated with the 12 years that Americans are expected to live without health insurance to individuals, their families, the communities in which they live, and society at large? What does one year of life without health insurance cost individuals in terms of financial loss, poor health, and emotional distress? Answers to these questions are important when evaluating the costs and benefits of particular health care reforms, especially those aimed at achieving universal coverage. Another important direction for future research is to examine the timing and sequence of spells without health insurance. For example, does being uninsured during young adulthood have financial or health consequences later in life? Does being uninsured and in a less-healthy state in later adulthood have consequences for health and finances in old age? As the debate over health care reform intensifies, these questions will become increasingly important, and the tools and perspectives of demography can provide valuable insights.
Acknowledgments
The authors gratefully acknowledge Professor Kosuke Imai and Professor Scott Lynch for their helpful advice, as well as the anonymous reviewers who provided extremely constructive comments and suggestions. Dr. Kaneda would also like to acknowledge the support she received from the Population Reference Bureau. The views in this article are those of the authors, and no official endorsement by the Agency for Healthcare Research and Quality and the Department of Health and Human Services is intended or should be inferred.
Footnotes
This calculation is based on data from the 2004 full-year public use file from the Medical Expenditure Panel Survey. Analysis is available upon request.
Contributor Information
JAMES B. KIRBY, The Agency for Healthcare Research and Quality, Center for Financing, Access, and Cost Trends, 540 Gaither Road, Rockville, MD 20850; e-mail: jkirby@ahrq.gov
TOSHIKO KANEDA, Population Reference Bureau.
REFERENCES
- Arias E. National Vital Statistics Reports. 3. Vol. 51. National Center for Health Statistics; Hyattsville, MD: 2002. “United States Life Tables, 2000”. [PubMed] [Google Scholar]
- Ayanian JZ, Kohler BA, Abe T, Epstein AM. “The Relation Between Health Insurance Coverage and Clinical Outcomes Among Women With Breast Cancer”. New England Journal of Medicine. 1993;329:326–31. doi: 10.1056/NEJM199307293290507. [DOI] [PubMed] [Google Scholar]
- Ayanian JZ, Weissman JS, Schneider EC, Ginsburg JA, Zaslavsky AM. “Unmet Health Needs of Uninsured Adults in the United States”. Journal of the American Medical Association. 2000;284:2061–69. doi: 10.1001/jama.284.16.2061. [DOI] [PubMed] [Google Scholar]
- Baker DW, Shapiro MF, Schur CL. “Health Insurance and Access to Care for Symptomatic Conditions”. Archives of Internal Medicine. 2000;160:1269–74. doi: 10.1001/archinte.160.9.1269. [DOI] [PubMed] [Google Scholar]
- Catanzarite L. “Race-Gender Composition and Occupational Pay Degradation”. Social Problems. 2003;51:14–37. [Google Scholar]
- Cohen J. “The Medical Expenditure Panel Survey: A National Health Information Resource”. Inquiry. 1996;33:373–89. [PubMed] [Google Scholar]
- Cohen J. Agency for Health Care Policy and Research; Rockville, MD: 1997. “Design and Methods of the Medical Expenditures Panel Survey Household Component”. Methodology Report No. 1. [Google Scholar]
- Currie J, Thomas D. “Medical Care for Children: Public Insurance, Private Insurance, and Racial Differences in Utilization”. Journal of Human Resources. 1995;30:135–62. [Google Scholar]
- DeNavas-Walt C, Proctor BD, Smith J. Current Population Reports. U.S. Census Bureau; Washington, DC: 2009. “Income, Poverty, and Health Insurance Coverage in the United States: 2008”. P60-236(RV). [Google Scholar]
- Derlet RW, Richards JR, Kravitz RL. “Frequent Overcrowding in US Emergency Departments”. Academic Emergency Medicine. 2001;8:151–55. doi: 10.1111/j.1553-2712.2001.tb01280.x. [DOI] [PubMed] [Google Scholar]
- Dubay L, Guyer J, Mann C, Odeh M. “Medicaid at the Ten-Year Anniversary of SCHIP: Looking Back and Moving Forward”. Health Affairs. 2007;26:370–81. doi: 10.1377/hlthaff.26.2.370. [DOI] [PubMed] [Google Scholar]
- Fronstin P. Employee Benefit Research Institute; Washington, DC: 2000. “Sources of Health Insurance and Characteristics of the Uninsured: Analysis of the March 2000 Current Population Survey.”. Issue Brief No. 228. [PubMed] [Google Scholar]
- Fronstin P. Employee Benefit Research Institute; Washington, DC: 2007. “Sources of Health Insurance and Characteristics of the Uninsured: Analysis of the March 2007 Current Population Survey.”. Issue Brief No. 310. [PubMed] [Google Scholar]
- Gabel J, Hunt K, Kim J. The Financial Burden of Self-paid Health Insurance on the Poor and Near Poor. New York: The Commonwealth Fund; 1998. [Google Scholar]
- Hadley J. “Sicker and Poorer—The Consequences of Being Uninsured: A Review of the Research on the Relationship Between Health Insurance, Medical Care Use, Health, Work, and Income”. Medical Care Research and Review. 2003;60(Suppl. 2):3S–75S. doi: 10.1177/1077558703254101. [DOI] [PubMed] [Google Scholar]
- Hadley J, Holahan J. “How Much Medical Care Do the Uninsured Use and Who Pays for It?”. Health Affairs Web Exclusive. 2003;1:W66–W81. doi: 10.1377/hlthaff.w3.66. [DOI] [PubMed] [Google Scholar]
- Haley JM, Zuckerman S. Washington, DC: Urban Institute; 2000. “Health Insurance, Access, and Use: United States Tabulations From the 1997 National Survey of America’s Families”. [Google Scholar]
- Hayward MD, Heron M. “Racial Inequality in Active Life Among Adult Americans”. Demography. 1999;36:77–91. [PubMed] [Google Scholar]
- Himmelstein DU, Warren E, Thorne D, Woolhandler S. “Illness and Injury as Contributors to Bankruptcy”. Health Affairs. 2005;24:63–74. doi: 10.1377/hlthaff.w5.63. [DOI] [PubMed] [Google Scholar]
- Hoffman C, Schoen C, Rowland D, Davis K. “Gaps in Health Coverage and Among Working-Age Americans and the Consequences”. Journal of Health Care for the Poor and Underserved. 2001;12:273–89. doi: 10.1353/hpu.2010.0739. [DOI] [PubMed] [Google Scholar]
- Holahan J. The Henry J. Kaiser Family Foundation; Washington, DC: 2004. “Health Insurance Coverage of the Near Elderly”. Publication No. 7114. The Kaiser Commission on Medicaid and the Uninsured. [Google Scholar]
- Hoyert DL, Heron MP, Murphy SL, Kung H. National Vital Statistics Reports. 13. Vol. 54. National Center for Health Statistics; Hyattsville, MD: 2006. “Deaths: Final Data for 2003”. [PubMed] [Google Scholar]
- Idler EL, Angel R. “Self-rated Health and Mortality in the NHANES-1 Epidemiologic Follow-up Study”. American Journal of Public Health. 1990;80:446–52. doi: 10.2105/ajph.80.4.446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Idler EL, Benyami Y. “Self-rated Health and Mortality: A Review of Twenty-seven Community Studies”. Journal of Health and Social Behavior. 1997;38:21–37. [PubMed] [Google Scholar]
- Imai K, Soneji S. “On the Estimation of Disability-Free Life Expectancy: Sullivan’s Method and Its Extension”. Journal of the American Statistical Association. 2007;102:1199–211. doi: 10.1198/016214507000000040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Institute of Medicine . Coverage Matters: Insurance and Health Care. Washington, DC: National Academies Press; 2001a. [PubMed] [Google Scholar]
- Institute of Medicine . Crossing the Chasm: A New Health System for the Twenty-first Century. Washington, DC: National Academies Press; 2001b. [Google Scholar]
- Institute of Medicine . Care Without Coverage: Too Little, Too Late. Washington, DC: National Academies Press; 2002a. [Google Scholar]
- Institute of Medicine . Health Insurance is a Family Matter. Washington, DC: National Academies Press; 2002b. [PubMed] [Google Scholar]
- Jytha M, Guralnik JM, Ferrucci L, Jokels J, Heikkinen E. “Is Self-rated Health Comparable Across Cultures and Genders?”. Journal of Gerontology. 1998;53B:S144–S152. doi: 10.1093/geronb/53b.3.s144. [DOI] [PubMed] [Google Scholar]
- Kasper JD, Giovannini TA, Hoffman C. “Gaining and Losing Health Insurance: Strengthening the Evidence for Effects of Access to Care and Health Outcomes”. Medical Care Research and Review. 2000;57:298–318. doi: 10.1177/107755870005700302. [DOI] [PubMed] [Google Scholar]
- Kington RS, Smith JP. “Socioeconomic Status and Race and Ethnic Differences in Functional Status Associated With Chronic Disease”. American Journal of Public Health. 1997;87:805–10. doi: 10.2105/ajph.87.5.805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kozak LJ, Hall MJ, Owings MF. “Trends in Avoidable Hospitalizations, 1980–1998”. Health Affairs. 2001;20(2):225–32. doi: 10.1377/hlthaff.20.2.225. [DOI] [PubMed] [Google Scholar]
- Lewin Group . Emergency Department Overload: A Growing Crisis. Washington, DC: American Hospital Association, American College of Emergency Physicians; 2002. [Google Scholar]
- McCall L. “Sources of Racial Wage Inequality in Metropolitan Labor Markets: Racial, Ethnic, and Gender Differences”. American Sociological Review. 2001;66:520–41. [Google Scholar]
- Nelson DE, Thompson B, Bland SD, Rubinson R. “Trends in Perceived Cost as a Barrier to Medical Care, 1991–1996”. American Journal of Public Health. 1999;89:1410–12. doi: 10.2105/ajph.89.9.1410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Newacheck PW, Brindis CD, Cart CU, Marchi K, Irwin CE. “Adolescent Health Insurance Coverage: Recent Changes and Access to Care”. Pediatrics. 1999;104:195–202. doi: 10.1542/peds.104.2.195. [DOI] [PubMed] [Google Scholar]
- Newacheck PW, Stoddard JJ, Hughs DC, Pearl M. “Health Insurance and Access to Primary Care for Children”. New England Journal of Medicine. 1998;338:513–19. doi: 10.1056/NEJM199802193380806. [DOI] [PubMed] [Google Scholar]
- Osteen RT, Winchester DP, Hussey DH, Clive RE, Freidman MA, Cady B. “Insurance Coverage of Patients With Breast Cancer in the 1991 Commission on Cancer Patient Care Evaluation Study”. Annual Surgical Oncology. 1994;1:462–67. doi: 10.1007/BF02303610. [DOI] [PubMed] [Google Scholar]
- Pauly MV, Percy AM. “Cost and Performance: A Comparison of the Individual and Group Health Insurance Markets”. Journal of Health Politics, Policy, and Law. 2000;25:9–26. doi: 10.1215/03616878-25-1-9. [DOI] [PubMed] [Google Scholar]
- Rhoades JA, Chu M. MEPS Research Findings. Agency for Healthcare Research and Quality; Rockville, MD: 2000. “Health Insurance Status of Civilian Noninstitutionalized Population”. [Google Scholar]
- Rhoades JA, Cohen SB. Agency for Healthcare Research and Quality; Rockville, MD: 2007. “The Long-Term Uninsured in America, 2002–2005: Estimates for the US Population Under Age 65” Statistical Brief No. 183. [Google Scholar]
- Richards JR, Navarro ML, Derlet RW. “Survey of Directors of Emergency Departments in California on Overcrowding”. Western Journal of Medicine. 2000;172:385–88. doi: 10.1136/ewjm.172.6.385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roberts M. Agency for Healthcare Research and Quality; Rockville, MD: 2006. “Racial and Ethnic Differences in Health Insurance Coverage and Usual Source of Care, 2002.”. MEPS Chartbook AHRQ Publication No. 06-0004. [Google Scholar]
- Roetzheim RG, Pal N, Tennant C, Voti L, Ayanian JZ, Schwabe A, Krischer JP. “Effects of Health Insurance and Race on Early Detection of Cancer”. Journal of the National Cancer Institute. 1999;91:1409–15. doi: 10.1093/jnci/91.16.1409. [DOI] [PubMed] [Google Scholar]
- Rust KF, Rao JNK. “Variance Estimation for Complex Surveys Using Replication Techniques”. Statistical Methods in Medical Research. 1996;5:283–310. doi: 10.1177/096228029600500305. [DOI] [PubMed] [Google Scholar]
- Seifert RW, Rukavina M. “Bankruptcy Is the Tip of a Medical-Debt Iceberg”. Health Affairs. 2006;25:W89–W92. doi: 10.1377/hlthaff.25.w89. [DOI] [PubMed] [Google Scholar]
- Shi L. “Type of Health Insurance and Quality of Primary Care Experience”. American Journal of Public Health. 2000;90:1848–55. doi: 10.2105/ajph.90.12.1848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Starr P. The Social Transformation of American Medicine. New York: Basic Books; 1982. [Google Scholar]
- Sullivan DF. “A Single Index of Mortality and Morbidity”. HSMHA Health Reports. 1971;86:347–54. [PMC free article] [PubMed] [Google Scholar]
- U.S. Department of Health and Human Services . Healthy People 2010: Understanding and Improving Health. 2nd ed. Washington, DC: U.S. Government Printing Office; 2000. [Google Scholar]
- Weissman JS, Gatsonis C, Epstein AM. “Rates of Avoidable Hospitalization by Insurance Status in Massachusetts and Maryland”. Journal of the American Medical Association. 1992;268:2388–94. [PubMed] [Google Scholar]
- Wherry L, Feingold K. “Changes in Health Insurance Coverage and Health Status by Race and Ethnicity”. Journal of the National Medical Association. 2004;96:1577–82. [PMC free article] [PubMed] [Google Scholar]
- Wolter KM. Introduction to Variance Estimation. New York: Springer-Verlag Inc; 1985. [Google Scholar]
- Zimmer Z, Natividad JN, Lin H-S, Chayovan N. “A Cross-National Examination of the Determinants of Self-assessed Health”. Journal of Health and Social Behavior. 2000;41:465–81. [PubMed] [Google Scholar]
- Zuvekas SH, Weinick RM. “Changes in Access to Care, 1977–1996: The Role of Health Insurance”. Health Services Research. 1999;34:271–79. [PMC free article] [PubMed] [Google Scholar]