Since its description by Child1 in 1953, portacaval transposition has proved to be a versatile tool for studying various aspects of hepatic and gastrointestinal physiology. With this preparation, the effects of diverting the splanchnic drainage away from the liver can be assessed without the complicating factor of deterioration of hepatic function.4
Two factors have reduced the experimental value of portacaval transposition. The first of these involves the ligation of tributary vessels to the portal vein or vena cava1 in order to obtain greater mobilization for the anastomoses. The resultant alteration of the adrenal, pancreatic or duodenal venous drainage could influence various parameters to be measured. The second factor involves technical difficulties5 which are related to the need for portal obstruction during transposition of the vessels.
In the present study, a simple technique is outlined with which acute portal or caval hypertension is prevented during operation, and with which none of the portal or vena caval branches are ligated. A high rate of success has been attained, without transfusions, intravenous fluid therapy or other care.
TECHNIQUE
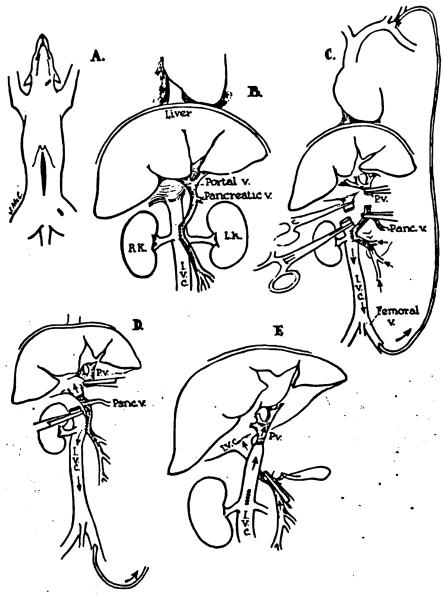
Twenty-two mongrel dogs, from 13 to 25 kg., were anesthetized with pentobarbital sodium. An upper midline incision was made (Fig. 1, A). The vena cava above the adrenal veins was mobilized. The portal vein was cleaned and mobilized above the entrance of the pancreatic vein (the highest tributary of the portal vein) to the bifurcation in the liver hilus. The proximal 1 cm, of the pancreatic vein was also mobilized.
Fig. 1.
Steps in the technique of portacaval transposition.
An 8 to 10 mm, portacaval anastomosis was performed as far below the pancreatic vein as possible (Fig. 1, B) without excision of tissue from either vessel wall. The femoral-jugular external polyethylene bypass described by Kaupp3 was then inserted and the portal vein and inferior vena cava occluded with Potts clamps above and below the proposed site of transposition (Fig. 1, C).
The anastomosis of the distal portal vein to the proximal vena cava was performed first with 6-0 continuous arterial silk (Fig. 1, D). The distal vena cava was then connected to the proximal portal vein (Fig. 1, E). The posterior row was placed from within the vessels. At first, these anastomoses were difficult because of the short segments of vessels and the confined space of the operative field. After a few trials, these difficulties were eliminated.
After completion of transposition, the external polyethylene bypass was removed and the external jugular and femoral veins ligated. The preliminary side-to-side portacaval shunt was drawn into the jaws of a partially occluding Potts clamp, divided, and closed with continuous 6-0 silk (Fig. 1, E).
RESULTS
The external bypass which decompressed both the portal vein and vena cava afforded excellent protection to the gastrointestinal tract. The bowel remained pink during transposition of the vessels. Transfusions or fluids were not given during or after surgery. The dogs were allowed to eat the day after operation, and no subsequent care was required.
In the developmental stages of this technique, difficulties were encountered with the anastomoses, which had to be performed with short venous cuffs. In three of the first five experiments, portal anastomotic thrombosis occurred. Subsequently, 17 consecutive transpositions were performed with long-term survival.
The studies for which the portacaval transposition was performed were carried out from one and a half to eight weeks after operation, and the dogs were sacrificed. Weight loss was consistent for two or three weeks after operation, but all the dogs followed for one month or longer gained weight up to or toward the preoperative level.
At autopsy, the anastomoses were examined. In three of the first five animals, clots had formed at the anastomosis between the distal portal vein and the proximal vena cava. In the last 17 dogs, no anastomotic thrombosis was present. Thrombosis of the iliac vein was present above the site of femoral vein ligation, sometimes extending into the lower vena cava, but edema of the involved leg was not seen. In the chronic animals, no gross abnormalities of the gastrointestinal tract were found.
DISCUSSION
Apparently, most of the difficulties during and after portacaval transposition have been due to shock. Transfusions have generally been necessary.1,5 Summers5 has reported that irreversible shock with hemorrhagic gastroenteritis was commonly seen even when the technique of operation had reached a high degree of perfection. He suggested that exposure of the diverted adrenal venous flow to the detoxifying influence of the liver caused a state of adrenal insufficiency. In support of this contention was the fact that pre- and postoperative steroid therapy resulted in a striking reduction in operative mortality.5
The uniform success with the method described in the present study and further experience in Eiseman's laboratory1 provide evidence that acute adrenal insufficiency does not occur as a result of the transposition per se. Rather, it suggests that the problems of fluid therapy and hypotension are the result of depletion of the circulating blood volume by sequestration in the acutely obstructed portal and caval venous beds, and by continued fluid loss in these areas even after the obstruction is relieved. When such obstruction is avoided during the operation, as has been described, no shock problems are encountered, and the operative mortality approaches zero.
SUMMARY
A technique is described for portacaval transposition in which portal or inferior vena caval hypertension is prevented by a decompressing external bypass during the period of vascular anastomoses. Successful preparations were uniformly attained without transfusions or fluid therapy, and with a minimum of postoperative care. The method allows transposition without ligation of tributary branches of either the vena cava or portal vein.
ADDENDUM
Recently, an alternative technique for transposition has been used, based on the observation by Medins and Laufman6 of the protective action of hypothermia during mesenteric vein occlusion. The animals are cooled to 30°C, and the transposition performed as described above with omission of the portacaval shunt and external bypass. In experiments in which it is desirable to leave intact femoral veins for subsequent testing, this modification is the method of choice.
Acknowledgments
This work was aided by a grant from the American Heart Association and Grant A-3176 from the U.S. Public Health Service, National Institutes of Health, Bethesda, Maryland, Dr. Starzl is a Markle Scholar.
REFERENCES
- 1.Child CG, III, Barr DB, Holswade GR, Harrison CS. Liver regeneration following porta-caval transposition in dogs. Ann. Surg. 1952;138:600. doi: 10.1097/00000658-195310000-00013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Eiseman B. Personal communication [Google Scholar]
- 3.Kaupp HA, Jr., Starzl TE. The use of an external by-pass in experimental total hepatectomy. Surgery. 1960;48:330. [PMC free article] [PubMed] [Google Scholar]
- 4.Silen W, Mawdsley DL, Weirich WL, Harper HA, McCorkle HJ. A comparison of liver function following Eck fistula and porta-caval transposition. Surg. Forum. 1956;7:425. [PubMed] [Google Scholar]
- 5.Summers WB, Malette WG, Eiseman B. Metabolic effects of transposition of the portal vein and inferior vena cava. Surg. Forum. 1956;7:429. [PubMed] [Google Scholar]
- 6.Medins G, Laufman H. Hypothermia in mesenteric arterial and venous occlusions. Experimental study. Ann. Surg. 1958;148:747. doi: 10.1097/00000658-195811000-00004. [DOI] [PMC free article] [PubMed] [Google Scholar]