Abstract
Objective
An important question in pediatric bipolar research is whether marked nonepisodic irritability is a manifestation of bipolar disorder in youth. This study tests the hypothesis that youth with severe mood dysregulation (SMD), a category created for the purpose of studying children presenting with severe nonepisodic irritability, will be significantly less likely to develop (hypo-)manic or mixed episodes over time than will youth with bipolar disorder (BD).
Method
Patients with SMD (N = 84) and narrowly defined BD (N = 93) at baseline were followed up in 6-monthly intervals using the relevant K-SADS modules to ascertain (hypo-)manic or mixed episodes.
Results
Only one of 84 SMD subjects (1/84 [1.2%]; 95% confidence interval CI = 0.0003 to 0.064) experienced a (hypo-)manic or mixed episode during the study (median follow-up = 28.7 months). The frequency of such episodes was more than 50 times higher in those with narrowly defined BD (58/93 [62.4%]; 95% CI 0.52 to 0.72).
Conclusions
These data suggest that, over an approximately 2-year follow-up period, youth with SMD are unlikely to develop (hypo-)manic or mixed episodes.
Keywords: bipolar disorder, pediatric, severe mood dysregulation, irritability, ADHD
In American psychiatric clinics and inpatient settings, dramatic increases in the rates of diagnosis of pediatric bipolar disorder (BD) have been documented over the past decade,1,2 with a concomitant increase in prescription rates for antipsychotic medication.3 This rapid increase in the diagnosis of pediatric BD has coincided with the contention that the clinical presentation of BD differs between children and adults.4,5
The debate regarding the pediatric presentation of BD is complex. One important aspect of it has been the suggestion that marked irritability, even when it does not constitute an episodic change from baseline, is a manifestation of BD in youth.4,6,7 To provide a framework for research on whether irritable children without distinct manic episodes have a developmental presentation of BD, we operationalized8 a clinical syndrome, severe mood dysregulation (SMD), designed to capture chronically irritable children whose diagnostic status is in doubt. This paper uses a longitudinal sample to investigate the extent to which subjects with SMD develop episodes of (hypo-)mania, compared to youth with narrowly defined BD.
The criteria for SMD require a persistent, nonepisodic clinical presentation of negatively valenced mood with frequent and impairing anger outbursts, combined with at least three of the “B” criteria of mania (pressured speech, agitation, insomnia, and flight of ideas/racing thoughts) and one (distractibility) that is also common to ADHD.8 A community-based follow-up study suggests that SMD is common, with a lifetime prevalence of 3.3% in youth 9 to 19 years of age.9 Furthermore, in that sample SMD predicted depressive disorder at 7-year follow-up in youths who were 9 to 19 years old at baseline.9 Consistent with this finding, another community-based study of nonepisodic irritability in youth showed that it predicted depressive disorders and generalized anxiety disorder, but not phobias, Axis II disorders, or BD at 20-year follow-up.10 However, these studies were conducted in community samples in which BD was a relatively rare outcome. Moreover, because the intervals between assessments were long and depressive episodes are more frequent in adult BD than are manic episodes,11 only depressive episodes may have been captured. For these reasons, these studies allow only very limited inferences to be drawn about the relationship between SMD or nonepisodic irritability and BD.
The present study includes higher numbers of children with SMD and BD than commonly afforded by epidemiologic samples, as well as data gathered at 6-month intervals over a median follow-up of 28.4 months. The purpose of the study is to establish whether the absence of (hypo-)manic episodes is an enduring characteristic of SMD, or whether children commonly evolve from SMD to a more classic presentation of BD by developing episodes of (hypo-)mania. If children with SMD differ markedly from BD in the frequency of manic episodes, this would support the clinical importance of distinguishing children with severe chronic irritability from those with classically defined BD. Accordingly, our hypothesis is that, over time, children with SMD will be significantly less likely to experience a (hypo-)manic or mixed episode than will those with BD.
Method
Participants
Participants with BD and SMD were enrolled in an Institutional Review Board-approved study at the Intramural Research Program of the National Institute of Mental Health. Parents and children provided written informed consent/assent.
BD subjects met DSM-IV criteria for BDI/II, with a history of at least one clearly demarcated hypomanic or manic episode (lasting ≥4 days for hypomania or ≥7 days for mania). During these episodes, abnormally elevated or expansive mood, and at least three DSM-IV criterion “B” mania symptoms were present.8
Participants with SMD fulfilled the following criteria: abnormal mood (specifically anger or sadness), present at least half of the day on most days, and of sufficient severity to be noticeable by people in the child's environment (e.g., parents, teachers, peers). In addition, compared with his/her peers, the child exhibits hyperreactivity to negative emotional stimuli (e.g., temper tantrums inappropriate for age or precipitating event) at least three times weekly. In addition, SMD youth had hyperarousal symptoms (i.e., at least three of the following: insomnia, intrusiveness, pressured speech, flight of ideas/racing thoughts, distractibility, psychomotor agitation). Symptom onset had to be before age 12 years, and symptoms were required to be present for at least 1 year, with no remission period ≥2 months. These symptoms were required to cause severe impairment in at least one setting (i.e., home, school, peers), and at least mild impairment in another. Euphoric mood or distinct hypomanic or manic episodes lasting ≥1 day were exclusionary.8 Exclusion criteria for both patient groups included IQ <70, pervasive developmental disorder, unstable medical illness, or substance abuse within the past 2 months.
Initial Assessment
The Kiddie Schedule for Affective Disorders—Present and Lifetime Version (KSADS-PL12), a semi-structured diagnostic interview was administered at the NIMH to parents and children separately by graduate level clinicians with established reliability (κ = 0.9, including the differentiation between SMD and BD). Clinicians administering the KSADS were licensed practitioners (M.D., M.S.W., Ph.D., or M.S.N.) with 5 to 25 years of postlicensure clinical experience. Training in KSADS consisted of 20 to 30 hours of observation, monitored administration of the instrument, and establishing reliability with experienced child research clinicians. Diagnoses were based on best-estimate procedures13 generated in a consensus conference led by a least one psychiatrist with extensive experience evaluating children with bipolar-spectrum illness. SMD was assessed using a specifically developed KSADS supplementary module.8,14
The Wechsler Abbreviated Scale of Intelligence was used to measure intelligence15 at initial assessment. WASI data were absent for five patients with SMD and one patient with BD. For the WASI data, no imputation was used; the means and standard deviations presented were calculated on those with data available, and group differences were estimated using listwise deletion.
Longitudinal Data
After the initial in-person assessment, subjects were followed up, on average, at 6-month intervals. Experienced clinicians with at least Master's-level qualifications and with documented reliability on the KSADS administered the KSADS mania and depression modules by telephone to the patient's parent. These KSADS modules were used to define the onset, offset, and symptom content of manic, hypo-manic, mixed, or depressive episodes.
The initial telephone assessment is designated as “baseline” in this paper. The patients were followed up subsequently in intervals of approximately 6 months; the means and standard deviations (in parentheses) for the follow-up intervals are as follows: first follow-up: 6.02 (1.49) and 5.97 (2.35) months for SMD and BD, respectively; second follow-up: 6.06 (1.74) and 5.51 (2.30) months for SMD and BD, respectively; third follow-up: 5.74 (1.83) and 5.54 (2.41) months for SMD and BD, respectively; and fourth follow-up: 6.06 (1.62) and 6.12 (1.99) months for SMD and BD, respectively.
Figure 1 shows the data available at each time point and the attrition rates. Two things should be noted when interpreting Figure 1. First, the denominator of the rates presented in Figure 1 varies. This is because the study is ongoing and, therefore, not all patients enrolled in the study at the same time point—by the time of data analysis, the range of possible follow-up duration for a given patient varied from 6 to 30 months. Second, the numerator of the rates provided in Figure 1 varies as a result of study attrition. Hence, the follow-up rates are a quotient of the number of patients in the study at each follow-up point to the number of patients who could have been followed up at that time point.
FIGURE 1.
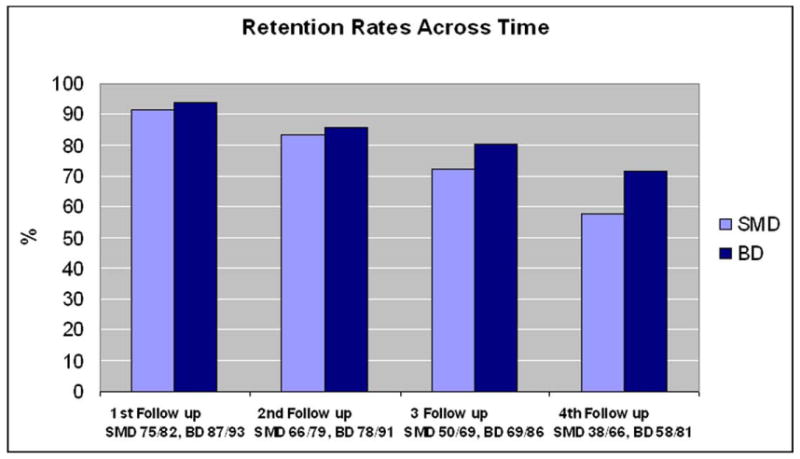
Percentage of patients with severe mood dysregulation (SMD) and bipolar disorder (BD) at each follow-up point is shown in the bars. Note: Underneath each pair of bars are the raw number proportions for each category.
Statistical Analyses
Gender and comorbidity comparisons between SMD and BD were performed with χ2 tests. To compare SMD and BD on age and IQ scores, t tests were used.
To address the paper's main hypothesis comparing the rates of (hypo-)manic or mixed episodes at follow-up between SMD and BD, we created a dichotomous variable that was coded zero (0) if no manic, hypo-manic, or mixed episode had occurred, or one (1) if at least one manic, hypo-manic, or mixed episode had occurred over the time of follow-up. The respective proportions were estimated and binomial confidence intervals constructed around those estimates. We conducted a z test of the null hypothesis that the proportion of SMD and BD subjects experiencing at least one manic, hypo-manic, or mixed episode during the follow-up period did not differ between groups. Of note, this analysis assumes that the length of follow-up was equal between SMD and BD.
We also compared SMD and BD groups in the propensity to experience at least one depressive episode during the follow-up period. The analytic strategy was similar to the one for manic, hypo-manic, or mixed episodes. Finally, we used a t test to compare SMD and BD on the mean number of depressive episodes over follow-up.
Only data from those available at the each study point were analyzed, and no imputation procedure was used.
Results
Sample Characteristics
For the follow-up study, 93 patients with BD and 84 patients with SMD had a baseline assessment.
The follow-up rates are shown in Figure 1, and the sample characteristics are described in Table 1. At baseline, compared with youth with BD, participants with SMD were significantly younger and more often male, although this did not reach statistical significance. In addition, given the inclusion criteria for SMD, it is not surprising that children with SMD showed higher rates of ODD and ADHD than did those with BD. BD and SMD youth did not differ in the prevalence of CD or GAD. BD Type-I was present in 76% of the BD patients (71 of 93), the rest being BD Type-II. Retention rates over the follow-up period of approximately 2 years were significantly higher for the BD than for the SMD group. The median follow-up was 25.1 months overall (minimum = 0.7, maximum = 89.8), with a median of 23.0 months (minimum = 0.7, maximum = 75) for SMD and a median of 32.3 months (minimum = 0.69, maximum = 89.8) for BD. The difference between the two groups was significant (Mann–Whitney U = 2720, z = −3.48, p < .001). An attrition analysis showed that not taking part in the study at the last follow-up was not predicted by age, gender, IQ, or any of the following diagnoses: ODD, CD, ADHD, MDD, or GAD (data available upon request).
TABLE 1. Sample Characteristics at Baseline.
| SMD | BD | t | χ2 | |
|---|---|---|---|---|
| N | 84 | 93 | – | – |
| Mean age (SD) | 11.6 (2.3) | 12.9 (2.8) | −3.2** | – |
| Gender (male) | 56 (66.7%) | 49 (52.7%) | 3.6§ | |
| Mean IQ (SD) | 101.9 (13.3) | 107.8 (15.2) | −2.6** | – |
| ADHD (%) | 69 (82.1%) | 42 (45.2%) | – | 25.8*** |
| ODD (%) | 66 (78.6%) | 24 (25.8%) | – | 49.2*** |
| CD (%) | 4 (4.8%) | 2 (2.22%) | – | 0.9 |
| GAD (%) | 25 (29.8%) | 30 (32.3%) | – | 0.128 |
| MDD (%) | 19 (22.6%) | – | – | – |
Note: ADHD = attention-deficit/hyperactivity disorder; BD = bipolar disorder; CD = conduct disorder; GAD = generalized anxiety disorder; MDD = major depressive disorder; ODD = oppositional defiant disorder; SMD = severe mood dysregulation.
p < .01;
p < .001;
p = .058.
Conversion from SMD to BD
The main hypothesis of this paper was that youth with SMD would be significantly less likely to experience (hypo-)manic or mixed episodes over time, compared with BD. Of the 84 subjects with SMD at baseline who were followed up over time, only one experienced an episode of mania or hypomania and thus was reclassified as BD. This subject, who had first- and second-degree relatives with BD, developed a brief hypomanic episode within 1 year of enrollment in the study. Of the 93 subjects with BD followed up, 58 developed at least one episode of mania, hypomania, or mixed state over the follow-up period. Therefore, the probability of developing at least one manic, hypomanic, or mixed episode was approximately 50 times lower among subjects with SMD (1/84 [1.2%]; 95% confidence interval [CI] 0.0003 to 0.064) compared with subjects with BD (58/93 [62.4%]; 95% CI 0.52 to 0.72), and the difference was significant (z = −8.61; p < .00001). These results are summarized in Figure 2. Given that the median follow-up differed significantly between groups, we wanted to ensure that we did not unduly bias our results in favor of our hypothesis by having longer follow-up periods for BD than for SMD subjects. For this reason, we conducted a supplementary analysis restricting the analysis to a maximum follow-up of 75 months (the longest follow-up for SMD subjects) instead of 89.8 months (the longest follow-up time BD subjects). This analysis showed that only one of 84 subjects with SMD developed a (hypo-)manic or mixed episode during follow-up, whereas 50 of 85 subjects with BD (58.8%, 95% CI = 0.48 to 0.69) developed such an episode during follow-up (z = −8.16; p < .0001).
FIGURE 2.
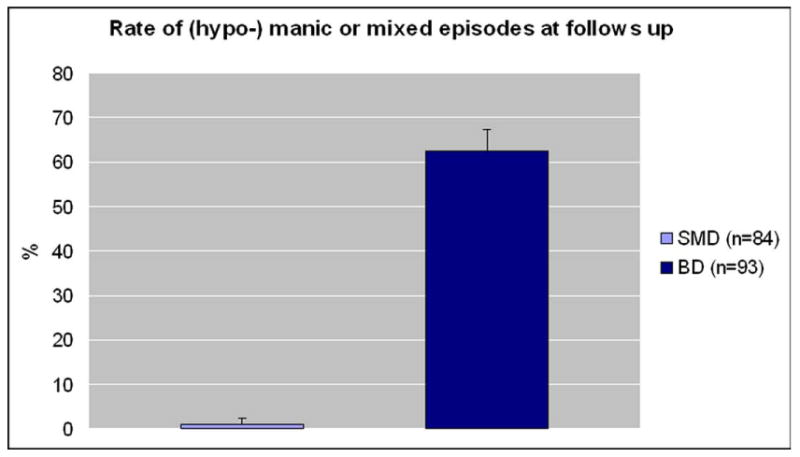
Bars with standard errors show the percentage of patients with either severe mood dysregulation (SMD) or bipolar disorder (BD) who developed a (hypo-)manic or mixed episode during the follow-up period.
Episode Characteristics for SMD and BD
Table 2 displays the episode characteristics of the two groups. In BD, depressive episodes were most common, followed by hypomanic episodes, as shown in Table 2. In addition, the mean number of depressive episodes was significantly higher in BD than in SMD (Table 2).
TABLE 2. Episode Characteristics for Severe Mood Dysregulation (SMD) and Bipolar Disorder (BD).
| Characteristic | BD (N = 93) | SMD (N = 84) | |||
|---|---|---|---|---|---|
| Number of episodes | Range | Mean (SD) | Range | Mean (SD) | t Test |
| Hypomanic | 0–12 | 1.34 (1.96) | – | – | |
| Hypomanic per months in study | 0–0.28 | 0.036 (0.05) | – | – | |
| Manic | 0–6 | 0.59 (1.23) | – | – | |
| Manic per months in study | 0–0.23 | 0.016 (0.04) | – | – | |
| Depressive | 0–14 | 2.18 (2.71) | 0–4 | 0.36 (0.83) | |
| Depressive per months in study | 0–0.21 | 0.05 (0.056) | 0–0.34 | 0.015 (0.046) | −5.2*** |
| Mixed | 0–2 | 0.18 (.49) | – | – | |
| Mixed per months in study | 0–0.09 | 0.005 (0.015) | – | – | |
p < .001.
Discussion
We conducted a longitudinal follow-up study of a clinic sample of youth with SMD and narrowly defined BD to answer an important question related to the pediatric BD debate—namely, whether children commonly evolve from a phenotype characterized by severe, nonepisodic irritability to a more classic presentation of BD by developing distinct episodes of (hypo-)mania. We found that (hypo-)manic or mixed episodes were significantly less likely to occur in youth with SMD compared with BD.
It is important to note that SMD was created for the purpose of studying children presenting with severe nonepidsodic irritability.8 SMD overlaps with ODD in that both ascertain temper outbursts, irritability, and anger. Crucially, however, SMD does not include the symptoms of defiance and annoyance that are also included in ODD—this distinction between headstrong and irritable dimensions in ODD has been shown to have important differential predictions.16,17 In addition, the criteria for SMD define irritability much more specifically than do those for ODD, requiring a high frequency of outbursts, and the SMD criteria require that impairing irritability be present in at least two settings, although a child can meet criteria for ODD with impairment in only one setting. Thus, whereas most children with SMD meet criteria for ODD, most with ODD do not meet criteria for SMD, and SMD, but not ODD, ascertains a population that is as impaired as are youth with BD. For these reasons, we undertook this line of research using the SMD criteria, rather than those for ODD. Finally, it should be noted that SMD, as originally proposed,8 contains sadness as an alternative to anger for the criterion of negatively valenced mood. Nonetheless, all SMD youth meet the criteria of at least three outbursts per week, so that irritability is one of its prominent features, regardless of whether the negatively valenced mood is anger or sadness.
One of the main questions about SMD relates to the extent to which it is a developmental presentation of BD. If it were, one would expect that, over time, youth with SMD would manifest manic or hypomanic episodes meeting DSM-IV criteria. However, only one of 84 SMD subjects manifested an episode of (hypo-)mania at follow-up. The difference between SMD and BD is of an order of magnitude: the probability for a (hypo-)manic episode occurring in BD subjects was more than 50 times higher than in those with SMD. Moreover, the lower confidence limit of the probability of a (hypo-)manic episode in BD was more than six times higher than the upper confidence limit for manic episodes in SMD.
Our finding that only one youth with SMD experienced an episode of (hypo)mania over the follow-up period contrasts with the high conversion rate for short-episode bipolar disorder–not otherwise specified (BD-NOS) noted in the Course and Outcome of Bipolar Illness in Youth (COBY) study.18 The diagnosis of BD-NOS is poorly specified in DSM-IV; in child psychiatry, it is frequently assigned to two distinct clinical presentations: youth with severe, nonepisodic irritability (a presentation that we operationalized as SMD), and those with distinct (hypo-)manic episodes that are shorter than 4 days in duration. This distinction between these different presentations is important, given its potential implications for pathophysiology treatment, and nosologic classification. Youth with the short-duration episodes were followed longitudinally in the COBY study, in which approximately 25% of the BD-NOS subjects experienced a full-duration hypomanic or manic episode over the course of a 3-year follow-up18 In contrast, in the present study, 1.2% of SMD subjects converted from SMD to BD-I or BD-II within an approximate 2-year follow-up. Of note, the AACAP guidelines for BD recommend considering both the “short episode” and the “nonepisodic” phenotypes to be BD-NOS presentations.19 In contrast, our data, in concert with those from the COBY study, suggest that, whereas the “short-episode” phenotype may be a manifestation of BD and thus may warrant the diagnosis of BD-NOS, such a conclusion is considerably less clearly justified in the case of the nonepisodic presentation that is characteristic of SMD. Importantly, our study did not include youth with brief (hypo-)manic episodes, like those in the COBY study. Because we included only the SMD phenotype (i.e., severe, nonepisodic irritability), our data do not speak to the longitudinal course of any of the other possible bipolar spectrum phenotypes.
Our finding here is consistent with previous results using SMD-proxy phenotypes in community samples9,10 as well as with a preliminary family history study.20 These studies indicate that irritable youth are at risk for developing depressive and anxiety disorders in adulthood, and that youth with SMD are less likely than those with BD to have a parent with BD.20 Moreover, our findings are in keeping with those of a recent clinic study showing that, for children with severe persistent irritability, a diagnosis of BD is rarely justified upon careful clinical assessment.21 However, it should be noted that the current study was not designed to test the hypothesis that the occurrence of (hypo-)manic or mixed episodes in SMD was no more than would occur by chance; this would require a much larger sample. Moreover, our findings do not exclude the possibility that BD and SMD have common pathophysiologic features. Indeed, previous studies suggest that the two share behavioral deficits in emotion labeling processing14,22 and cognitive flexibility,23 although the neural mechanisms mediating these deficits may differ between the two patient groups.24
In sum, to the extent that the question, “Is SMD a developmental presentation of BD?” is framed categorically, the conclusion from this and previous studies9,20,24 is “no.” Because treatment decisions are categorical, there is value to framing the question categorically. That is, if a clinician views SMD as a BD phenotype, that clinician might prescribe atypical antipsychotic and/or mood-stabilizing medication for youth with this clinical presentation. Alternatively, if the clinician views SMD as a phenotype of anxiety and/or unipolar depression, coupled with ADHD, that individual might consider prescribing antidepressant medication coupled with a stimulant (these are medications that are relatively contraindicated in BD). Unfortunately, no published data currently exist on the safety or effectiveness of anti-depressant or stimulant medication in the SMD phenotype, and that is an important question for future study. So far, the only clinical trial in SMD is a pilot study of lithium, which was not effective.25 Additional treatment trials in youth with severe, nonepisodic irritability are a pressing public health need, given that an SMD proxy phenotype occurred with a prevalence of 3.3% in an epidemiologic sample in the United States9 and mood lability occurred in more than 5% of the population of children and adolescents in a sample in the United Kingdom.26
Although it is important to frame the question, “Is SMD a developmental presentation of BD?” categorically, it is equally important to ask the question dimensionally. Recent data demonstrate convincingly that DSM-IV diagnoses may not necessarily be pathophysiologically distinct: there is considerable genetic overlap between BD and schizophrenia27 and between BD and MDD.28 As noted, BD and SMD appear to share pathophysiological mechanisms, making it possible that the SMD phenotype will ultimately be placed on a pathophysiological spectrum between BD and MDD and/or other depressive syndromes. Accordingly, we found that depressive episodes were significantly more common in the BD group; a possible post hoc explanation for this finding is that, consistent with previous data,10 SMD may be linked with depressive phenotypes not characterized by episodicity, such as dysthymia. The findings of this study are relevant to researchers who study the early development of BD and inform their choices for the phenotypes to use, for example in genetic studies of early onset BD.
This study has a number of strengths. It is the first to report a follow-up of subjects with well-characterized SMD. Moreover, in comparison with previous community-based studies on SMD9 and mood lability,20 in which BD and SMD are relatively rare, the present clinic sample is enriched with cases of both SMD and BD and thus in reducing the likelihood of recall bias.
However, there are a number of important limitations. First, there is considerable attrition. Therefore, we cannot exclude the possibility that the conversion rate from SMD to BD has been underestimated. Secondly, from a psychometric point of view, it is conceivable that the prominence of nonepisodic irritability in those with SMD has generated “background noise” affecting on our instrument's ability to detect episodes. Although we cannot exclude this possibility, the effect size of the difference between SMD and BD is very large and therefore unlikely to be the result of a reduced signal-to-noise ratio. Third, it was not feasible to have the follow-up assessments be conducted blindly, so assessment bias cannot be excluded. However, follow-up was performed by experienced clinicians, who were 1) particularly attuned to the clinical importance of establishing (hypo-)manic and mixed episodes and 2) instructed to have a low threshold for their ascertainment. Importantly, parents were aware that, should an SMD child develop manic or hypomanic symptoms, the child and his/her family could continue to participate in the study, so that there should be no concern that reporting such an episode would result in exclusion. Fourth, follow-up interviews were only conducted only with the patient's parents and not with the children themselves. Given the generally low parent–child agreement in reporting symptoms of mania and depression, this may conceivably underestimate symptoms.29,30 However, we consider it unlikely that full-blown (hypo-)manic or mixed episodes would have gone unnoticed by parents. Fifth, it is important to reiterate that this study focuses on the comparison between narrowly defined BD and only one phenotype of several that have been described as BD–NOS. That is, although SMD captures children with nonepisodic irritability, this study did not include children with episodes of manic symptoms that are too short to meet DSM-IV criteria for hypomania. Thus, clinicians and researchers should not extrapolate from these results to other BD-NOS presentations, in particular to children with episode durations of less than 4 days. Finally, we used a narrow phenotype to ascertain cases of BD at baseline, in that we required abnormally elevated or expansive mood during an episode; the presence of irritability on its own30,31 was not a sufficient Criterion A for (hypo-)mania in this study. It is therefore possible that the BD cases in this study might not be representative of all cases of pediatric BD. However, two findings argue against this. First, the patterns of our results regarding the course of BD are in keeping with those of a recent large longitudinal study,32 i.e., episodes of depression were most common. Second, a recent study comparing patients with BD and abnormally elevated or expansive mood and/or grandiosity as the only Criterion A to those with either episodic irritability-only or with episodes characterized by both irritability and elevated or expansive mood suggests these groups are similar on important variables.33
In conclusion, our results suggest that research efforts should continue to focus on the pathophysiology of SMD and BD, as well as on the treatment of both conditions, given that both groups continued to exhibit significant psychopathology. In addition, studies should address the overlap and distinctions between SMD and ODD. Finally, studies using larger samples with longer follow-ups of SMD subjects, replicated in other centers, are required.
Acknowledgments
This work was supported by the National Institute of Mental Health, Intramural Program.
Footnotes
Disclosure: Drs. Stringaris, Baroni, Brotman, Rustgi, Towbin, and Leibenluft, and Ms. Haimm, Mr. Lowe, Ms. Myers, Ms. Wheeler, and Mr. Kayser report no biomedical financial interests or potential conflicts of interest.
References
- 1.Blader JC, Carlson GA. Increased rates of bipolar disorder diagnoses among U.S. child, adolescent, and adult inpatients, 1996–2004. Biol Psychiatry. 2007;62:107–114. doi: 10.1016/j.biopsych.2006.11.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Moreno C, Laje G, Blanco C, et al. National trends in the outpatient diagnosis and treatment of bipolar disorder in youth. Arch Gen Psychiatry. 2007;64:1032–1039. doi: 10.1001/archpsyc.64.9.1032. [DOI] [PubMed] [Google Scholar]
- 3.Olfson M, Blanco C, Liu L, Moreno C, Laje G. National trends in the outpatient treatment of children and adolescents with antipsychotic drugs. Arch Gen Psychiatry. 2006;63:679–685. doi: 10.1001/archpsyc.63.6.679. [DOI] [PubMed] [Google Scholar]
- 4.Biederman J, Klein RG, Pine DS, Klein DF. Resolved: mania is mistaken for ADHD in prepubertal children. J Am Acad Child Adolesc Psychiatry. 1998;37:1091–1096. doi: 10.1097/00004583-199810000-00020. [DOI] [PubMed] [Google Scholar]
- 5.Carlson GA, Meyer SE. Phenomenology and diagnosis of bipolar disorder in children, adolescents, and adults: complexities and developmental issues. Dev Psychopathol. 2006;18:939–969. doi: 10.1017/S0954579406060470. [DOI] [PubMed] [Google Scholar]
- 6.Biederman J. The evolving face of pediatric mania. Biol Psychiatry. 2006;60:901–902. doi: 10.1016/j.biopsych.2006.09.016. [DOI] [PubMed] [Google Scholar]
- 7.Mick E, Spencer T, Wozniak J, Biederman J. Heterogeneity of irritability in attention-deficit/hyperactivity disorder subjects with and without mood disorders. Biol Psychiatry. 2005;58:576–582. doi: 10.1016/j.biopsych.2005.05.037. [DOI] [PubMed] [Google Scholar]
- 8.Leibenluft E, Charney DS, Towbin KE, Bhangoo RK, Pine DS. Defining clinical phenotypes of juvenile mania. Am J Psychiatry. 2003;160:430–437. doi: 10.1176/appi.ajp.160.3.430. [DOI] [PubMed] [Google Scholar]
- 9.Brotman MA, Schmajuk M, Rich BA, et al. Prevalence, clinical correlates, and longitudinal course of severe mood dysregulation in children. Biol Psychiatry. 2006;60:991–997. doi: 10.1016/j.biopsych.2006.08.042. [DOI] [PubMed] [Google Scholar]
- 10.Stringaris A, Cohen P, Pine DS, Leibenluft E. Adult outcomes of youth irritability: a 20-year prospective community-based study. Am J Psychiatry. 2009;166:1048–1054. doi: 10.1176/appi.ajp.2009.08121849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Judd LL, Akiskal HS, Schettler PJ, et al. The long-term natural history of the weekly symptomatic status of bipolar I disorder. Arch Gen Psychiatry. 2002;59:530–537. doi: 10.1001/archpsyc.59.6.530. [DOI] [PubMed] [Google Scholar]
- 12.Kaufman J, Birmaher B, Brent D, et al. Schedule for Affective Disorders and Schizophrenia for School-Age Children-Present and Lifetime Version (K-SADS-PL): initial reliability and validity data. J Am Acad Child Adolesc Psychiatry. 1997;36:980–988. doi: 10.1097/00004583-199707000-00021. [DOI] [PubMed] [Google Scholar]
- 13.Leckman JF, Sholomskas D, Thompson WD, Belanger A, Weissman MM. Best estimate of lifetime psychiatric diagnosis: a methodological study. Arch Gen Psychiatry. 1982;39:879–883. doi: 10.1001/archpsyc.1982.04290080001001. [DOI] [PubMed] [Google Scholar]
- 14.Rich BA, Grimley ME, Schmajuk M, Blair KS, Leibenluft E. Face emotion labeling deficits in children with bipolar disorder and severe mood dysregulation. Develop Psychopathol. 2008;20:529–546. doi: 10.1017/S0954579408000266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wechsler D. Wechsler Abbreviated Scale of Intelligence. San Antonio, TX: Psychological Corporation; 1999. [Google Scholar]
- 16.Stringaris A, Goodman R. Longitudinal outcome of youth oppositionality: irritable, headstrong, and hurtful behaviors have distinctive predictions. J Am Acad Child Adolesc Psychiatry. 2009;48:404–412. doi: 10.1097/CHI.0b013e3181984f30. [DOI] [PubMed] [Google Scholar]
- 17.Stringaris A, Goodman R. Three dimensions of oppositionality in youth. J Child Psychol Psychiatry. 2009;50:216–223. doi: 10.1111/j.1469-7610.2008.01989.x. [DOI] [PubMed] [Google Scholar]
- 18.Birmaher B, Axelson D, Strober M, et al. Clinical course of children and adolescents with bipolar spectrum disorders. Arch Gen Psychiatry. 2006;63:175–183. doi: 10.1001/archpsyc.63.2.175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.McClellan J, Kowatch R, Findling RL. Practice parameter for the assessment and treatment of children and adolescents with bipolar disorder. J Am Acad Child Adolesc Psychiatry. 2007;46:107–125. doi: 10.1097/01.chi.0000242240.69678.c4. [DOI] [PubMed] [Google Scholar]
- 20.Brotman MA, Kassem L, Reising MM, et al. Parental diagnoses in youth with narrow phenotype bipolar disorder or severe mood dysregulation. Am J Psychiatry. 2007;164:1238–1284. doi: 10.1176/appi.ajp.2007.06101619. [DOI] [PubMed] [Google Scholar]
- 21.Carlson GA, Potegal M, Margulies D, Gutkovich Z, Basile J. Rages—what are they and who has them? J Child Adolesc Psychopharmacol. 2009;19:281–288. doi: 10.1089/cap.2008.0108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Guyer AE, McClure EB, Adler AD, et al. Specificity of facial expression labeling deficits in childhood psychopathology. J Child Psychol Psychiatry. 2007;48:863–871. doi: 10.1111/j.1469-7610.2007.01758.x. [DOI] [PubMed] [Google Scholar]
- 23.Dickstein DP, Nelson EE, McClure EB, et al. Cognitive flexibility in phenotypes of pediatric bipolar disorder. J Am Acad Child Adolesc Psychiatry. 2007;46:341–355. doi: 10.1097/chi.0b013e31802d0b3d. [DOI] [PubMed] [Google Scholar]
- 24.Rich BA, Schmajuk M, Perez-Edgar KE, et al. Different psychophysiological and behavioral responses elicited by frustration in pediatric bipolar disorder and severe mood dysregulation. Am J Psychiatry. 2007;164:309–317. doi: 10.1176/ajp.2007.164.2.309. [DOI] [PubMed] [Google Scholar]
- 25.Dickstein DP, Towbin KE, Van Der Veen JW, et al. Randomized double-blind placebo-controlled trial of lithium in youths with severe mood dysregulation. J Child Adolesc Psychopharmacol. 2009;19:61–73. doi: 10.1089/cap.2008.044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Stringaris A, Goodman R. Mood lability and psychopathology in youth. Psychol Med. 2009:1–9. doi: 10.1017/S0033291708004662. [DOI] [PubMed] [Google Scholar]
- 27.Craddock N, O'Donovan MC, Owen MJ. Genes for schizophrenia and bipolar disorder? Implications for psychiatric nosology. Schizophrenia Bulletin. 2006;32:9–16. doi: 10.1093/schbul/sbj033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Benazzi F. Is there a continuity between bipolar and depressive disorders? Psychother Psychosom. 2007;76:70–76. doi: 10.1159/000097965. [DOI] [PubMed] [Google Scholar]
- 29.Tillman R, Geller B, Craney JL, et al. Relationship of parent and child informants to prevalence of mania symptoms in children with a prepubertal and early adolescent bipolar disorder phenotype. Am J Psychiatry. 2004;161:1278. doi: 10.1176/appi.ajp.161.7.1278. [DOI] [PubMed] [Google Scholar]
- 30.Geller B, Zimerman B, Williams M, et al. DSM-IV mania symptoms in a prepubertal and early adolescent bipolar disorder phenotype compared to attention-deficit hyperactive and normal controls. J Child Adolesc Psychopharmacol. 2002;12:11–25. doi: 10.1089/10445460252943533. [DOI] [PubMed] [Google Scholar]
- 31.Stringaris A, Santosh P, Leibenluft E, Goodman R. Youth meeting symptom and impairment criteria for mania-like episodes lasting less than four days: an epidemiological enquiry. J Child Psychol Psychiatry. 2010;51:31–38. doi: 10.1111/j.1469-7610.2009.02129.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Birmaher B. Longitudinal course of pediatric bipolar disorder. Am J Psychiatry. 2007;164:537–539. doi: 10.1176/ajp.2007.164.4.537. [DOI] [PubMed] [Google Scholar]
- 33.Hunt J, Birmaher B, Leonard H, et al. Irritability without elation in a large bipolar youth sample: frequency and clinical description. J Am Acad Child Adolesc Psychiatry. 2009;48:730–739. doi: 10.1097/CHI.0b013e3181a565db. [DOI] [PMC free article] [PubMed] [Google Scholar]


