Abstract
Acupuncture has been widely used in alternative medicine for pain relief but may have many complications due to lack of appropriate cares. Pharmacopuncture is a sort of acupuncture that injects a herbal ingredient through a thin tube for the purpose of combining the effects of the herb and acupuncture and it has many pitfalls. The agents used in pharmacopuncture are not refined for a desired effect and not produced by sterile standard processes under strict medical surveillance. We report a case of a 44-yr-old male patient who had multiple abscesses in the psoas region with fever, right low back and hip pain that began after the pharmacopuncture treatment. This case shows that although pharmacopuncture has been practiced widely, it is important that the appropriate aseptic technique should be used to prevent severe infections and other complications.
Keywords: pharmacopuncture, psoas abscess
As the patients with low back pain increasing, new treatments in alternative medicine have been also increasing [1]. Pharmacopuncture is one of the representative treatments in alternative medicine, which is widely used in recent. Pharmacopuncture is included in acupuncture, which injects ingredients extracted from medicinal herbs or bee venom through thin tube to meridian points and tries to achieve effects both from acupuncture and medicine. However, pharmacopuncture might cause a lot of complications regarding the treatment, and in particular, it is vulnerable to infection.
As well as the risks of infection from acupuncture itself, it is a serious problem that medicinal herbs used for pharmacopuncture treatment are made and applied by each different method of the operator at discretion, which has higher risks of infection than other treatments, even if they are produced, distributed by standardization or sterilization [2]. In particular, as for the patients with low back pain, acupuncture tends to be applied to deep muscles around the spine, and in case intramuscular abscess occurred, the pain patterns are greatly similar to the general low back pain, which can cause the dangerous condition such as septicemia. The authors witnessed pyogenic, multiple intramuscular abscess which occurred after pharmacopuncture treatment, so this case was prepared with literature reviews.
CASE REPORT
A 44-year-old male patient visited the hospital. He claimed low back pain at right, buttock pain, and thigh pain at upper front with fever that occurred 6 days ago. He had got physical therapy and medicinal herbs treatment for a long time in the oriental medical clinic because of low back pain. In recent, he got additional pharmacopuncture treatment several times until 6 days before visiting this hospital. Right after the pharmacopuncture treatment, the symptom was improved, but he got a fever and the degree of pain got worse for 6 days before visiting this hospital. At first in this hospital, the patient claimed that he felt stiff in the lumbar at right side, buttocks, and thigh at upper front and he said they were numb. The degree of pain was 6/10 on visual analogue scale (VAS). The pain was sustained all day without being relieved even though taking a rest. It got worse when bending over or straightening his back, and it was greatly serious at night, so he claimed sleep disorders. The specific medical history of the patient, which can cause infection disease was not identified.
In the physical examination, tenderness was detected in spinous process of lumbar spine at level 2, 3, 4, and the right paraspinal area. There was no particular opinion in other neurologic examination or physical examination. High fever of 39.7 degrees was shown but other vital signs such as blood pressure and pulse were normal. In blood test, white blood cell count was 7,300/µl, which is in normal range, and erythrocyte sedimentation rate and C-reactive protein were respectively 67 mm/hr, 97.44 mg/L. AST/ALT/γGT were 92/151/226 IU/L, and ALP increased to 152 IU/L.
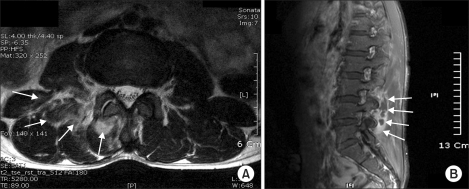
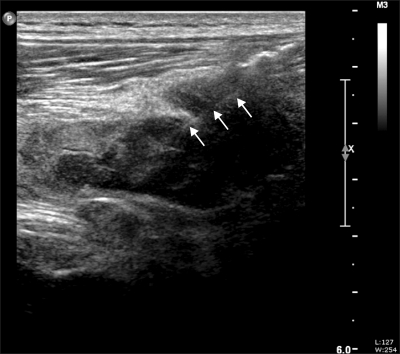
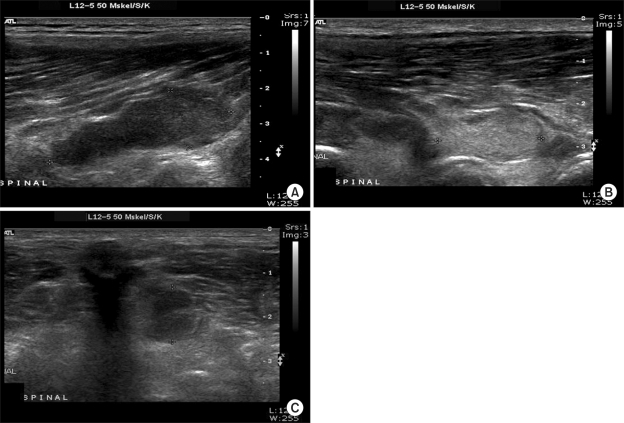
There was no particular opinion in simple radiography of lumbar spine, but in MRI for checking lesion, a wide range of myositis and multiple abscess in paraspinal muscles and psoas muscle between right lumbar spine at level 3-5, including multifidus muscle, longissimus muscle, iliocostal muscle, quadratus lumborum muscle, psoas muscle were detected (Fig. 1). With blood culture, about 3 cc thick pus was aspirated (Fig. 2) from three abscess sites (Fig. 3) under ultrasound needle guide and it was cultured. Except for it, there was no particular opinion in simple radiography of chest, ECG, echocardiography, and urine test.
Fig. 1.
Multifocal abscess formation and diffuse myositis of right paraspinal muscle at the level of L3, L4, L5 in magnetic resonance image. (A) axial view and (B) sagittal view at L3 level.
Fig. 2.
Sono-guided needle aspiration (arrows point to the needle within abscess cavity) was done targeting all three abscess cavities. About 3 ml of thick pus was aspirated at L4 level.
Fig. 3.
Multilobulated heterogeneous abscess formations in right lower paraspinal muscles. The largest one in L4 level with 4 × 1.7 cm (A), about 2 cm in L3 level (B), about 2.9 × 1.3 cm in L2 level (C).
Before obtaining the results from culture, 3rd generation antibiotic cefazolin and gentamicin were injected under being admission. As a result of incubation, staphylococcus aureus was identified, and cefazolin and gentamicin treatment which sensitivity checked were maintained. From the 4th day after admission, the fever came down significantly, the symptom was improved, and the patient's condition was stabilized. The patient discharged after replacing with levofloxacin which is the oral antibiotic 12 days after admission. Since then, the patient's condition was improved, but the treatment sustained for 1-month more with the oral antibiotic and it was closed.
DISCUSSION
There has been a lot of controversy over clinical usefulness of acupuncture [3], but traditional chinese medicine has a deep-rooted tradition, so acupuncture is widely used nationally. According to Witt et al. [4], it is known that the incidence of complications due to acupuncture amounts to about 7%, and 1.9% of them needed for treatment. Complications include pain, bleeding, infection related to procedure, and direct damages to nerves and organs due to acupuncture [4,5]. Moreover, infection of diseases such as AIDS [6] or hepatitis type B [7] are reported. In particular, infection is one of the complications regarding acupuncture, which is occurred not infrequently [8]. It is estimated the incidence will be increasing, considering the reality that complications regarding traditional chinese medicine treatment are not reported appropriately nationally.
It is not easy to find the reports on complications related to pharmacopuncture which is widely used in recent. As for pharmacopuncture, more complications might be triggered than simple acupuncture because there are complications not only related to acupuncture but related to used medicinal herbs. Even for infection, the incidence will be increasing because it might be caused not only by acupuncture itself but by used medicinal herbs.
The causes of acupuncture itself include inappropriate management of needles for treatment, inappropriate dressing of needle injection sites, and hand sanitation of the operator. Especially, there are reports that abscess is occurred even after using disposable needles [9], as well as reusing the needle after disinfection. It seems to be related to the fact that generally acupuncture tends to be applied to the injection sites with the bare hands without the specific disinfection, that's why it is required to derive the solutions for dressing of the injection sites and hand sanitation of the operator.
Medicinal herbs used for pharmacopuncture treatment are not medical supplies which are produced, distributed and controlled by thorough standardization or sterilization. Medicinal herbs for pharmacopuncture are not inspected on their aseptic property and safety, and are not controlled properly. And they are made by each different method of the operator at discretion. In this regard, regardless the effectiveness of medicinal herbs for pharmacopuncture, it is required to secure at least safety on medicinal herbs as soon as possible for public health.
It is quite difficult to detect pyogenic abscess of deep muscle at the initial stage [10], so patients tend to be suffered from the pain in various parts such as lumbar, flank, or buttocks commonly 5-6 days later on. The symptom is subacute by deep infection, which occurred rarely, and generally it is occurred in single part of muscle but it might be occurred in a wide range of parts for 11-43% [11]. As to the patients with low back pain, it is common that acupuncture is applied up to deep muscle near the spine, so it is possible to invade spine or the surrounding parts [12]. In case the appropriate management are not taken, fatal complications such as necrotizing fasciitis, septicemia, and death might be caused [9,11]. In this case, medicinal herbs which unclear ingredients are contained were injected through thin tube after applying acupuncture to the wide parts several times without thorough dressing, that's why multiple abscess in deep muscle was occurred.
In conclusion, it is definitely possible that serious infection is occurred by acupuncture without applying the inspected medicinal herbs or equipments or following thorough aseptic technique. Therefore, in case of symptoms such as fever and nonspecific low back pain, whether there is an invasive procedure like acupuncture including pharmacopuncture should be checked out and the possibility of infection at the initial stage should be prevented before triggering fatal complications. In addition, it is thought that health authorities should play a vital role in controlling infection of acupuncture and preparing the solutions.
References
- 1.Rubinstein SM, van Middelkoop M, Kuijpers T, Ostelo R, Verhagen AP, de Boer MR, et al. A systematic review on the effectiveness of complementary and alternative medicine for chronic non-specific low-back pain. Eur Spine J. 2010;19:1213–1228. doi: 10.1007/s00586-010-1356-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kang KS, Lee JS, Kwon GR. The clinical studies on the cases of side effect of CF herbal acupuncture. J Korean Pharmacopuncture Inst. 2001;4:65–71. [Google Scholar]
- 3.Park KH, Yoo TW. Evidence based acupuncture. Hanyang Med Rev. 2010;30:91–102. [Google Scholar]
- 4.Witt CM, Pach D, Reinhold T, Wruck K, Brinkhaus B, Mank S, et al. Treatment of the adverse effects from acupuncture and their economic impact: A prospective study in 73,406 patients with low back or neck pain. Eur J Pain. 2010 doi: 10.1016/j.ejpain.2010.06.008. [in press] [DOI] [PubMed] [Google Scholar]
- 5.Kim SY, Jang WI, Chung S, Choi DE, Na KR, Lee KW, et al. Perirenal hematoma induced by acupuncture and intramuscular stimulation. Korean J Nephrol. 2009;28:146–151. [Google Scholar]
- 6.Vittecoq D, Mettetal JF, Rouzioux C, Bach JF, Bouchon JP. Acute HIV infection after acupuncture treatments. N Engl J Med. 1989;320:250–251. doi: 10.1056/NEJM198901263200413. [DOI] [PubMed] [Google Scholar]
- 7.Walsh B. Control of infection in acupuncture. Acupunct Med. 2001;19:109–111. doi: 10.1136/aim.19.2.109. [DOI] [PubMed] [Google Scholar]
- 8.Woo PC, Lin AW, Lau SK, Yuen KY. Acupuncture transmitted infections. BMJ. 2010;340:c1268. doi: 10.1136/bmj.c1268. [DOI] [PubMed] [Google Scholar]
- 9.Seeley EJ, Chambers HF. Diabetic ketoacidosis precipitated by Staphylococcus aureus abscess and bacteremia due to acupuncture: case report and review of the literature. Clin Infect Dis. 2006;43:e6–e8. doi: 10.1086/504945. [DOI] [PubMed] [Google Scholar]
- 10.Park CB, Kim KS, Shin JH, Suh GJ, Youn YK. Clinical presentations, diagnosis, and treatments of a psoas abscess. J Korean Soc Emerg Med. 2005;16:346–351. [Google Scholar]
- 11.Bickels J, Ben-Sira L, Kessler A, Wientroub S. Primary pyomyositis. J Bone Joint Surg Am. 2002;84-A:2277–2286. doi: 10.2106/00004623-200212000-00024. [DOI] [PubMed] [Google Scholar]
- 12.Cho YP, Jang HJ, Kim JS, Kim YH, Han MS, Lee SG. Retroperitoneal abscess complicated by acupuncture: case report. J Korean Med Sci. 2003;18:756–757. doi: 10.3346/jkms.2003.18.5.756. [DOI] [PMC free article] [PubMed] [Google Scholar]