Abstract
Background
Although limited health literacy is a barrier to disease management and has been associated with poor glycemic control, the mechanisms underlying the relationships between health literacy and diabetes outcomes are unknown. We examined the relationships between health literacy, determinants of diabetes self-care, and glycemic control in adults with type 2 diabetes.
Methods
Patients with diabetes were recruited from an outpatient primary care clinic. We collected information on demographics, health literacy, diabetes knowledge, diabetes fatalism, social support, and diabetes self-care, and hemoglobin A1c values were extracted from the medical record. Structural equation models tested the predicted pathways linking health literacy to diabetes self-care and glycemic control.
Results
No direct relationship was observed between health literacy and diabetes self-care or glycemic control. Health literacy had a direct effect on social support (r = −0.20, P < 0.05) and through social support had an indirect effect on diabetes self-care (r = −0.07) and on glycemic control (r = −0.01). More diabetes knowledge (r = 0.22, P < 0.05), less fatalism (r = −0.22, P < 0.05), and more social support (r = 0.27, P < 0.01) were independent, direct predictors of diabetes self-care and through self-care were related to glycemic control (r = −0.20, P < 0.05).
Conclusions
Our findings suggest health literacy has an indirect effect on diabetes self-care and glycemic control through its association with social support. This suggests that for patients with limited health literacy, enhancing social support would facilitate diabetes self-care and improved glycemic control.
Introduction
It is estimated that 90 million Americans may have basic or below basic health literacy skills, defined as “the degree to which individuals have the capacity to obtain, process, and understand basic health information and services needed to make appropriate health decisions.”1 Compared to patients with adequate health literacy, patients with limited health literacy have been shown to have difficulty understanding their medical condition and its management,2–5 are less likely to engage in self-care behaviors,6 have poorer clinical outcomes,7 and a higher risk of mortality.8,9 While limited health literacy is common among patients with diabetes,10–14 the evidence of its impact on glycemic control has been mixed.10,11 Some studies report limited health literacy is associated with poor glycemic control,10,11,13 whereas others report limited health literacy is associated with poor disease knowledge and less adherence to diabetes self-care, but is not associated with glycemic control.12,14
The mechanisms linking health literacy to diabetes self-care and clinical outcomes are poorly understood.15,16 A recent study examined potential mechanisms through which health literacy impacts hypertension disease management and self-rated health.17 Findings revealed significant paths from health literacy to hypertension knowledge, from hypertension knowledge to disease management self-efficacy, from disease management self-efficacy to physical activity, and from physical activity to self-rated health.17 To our knowledge, there have been no published studies to date exploring the mechanisms linking health literacy to diabetes self-care and glycemic control. Identification of the factors linking health literacy to behavior and clinical outcomes in diabetes could have far-reaching utility, namely in the form of targeted interventions to address health literacy limitations. This study examines whether limited health literacy was directly or indirectly related to diabetes self-care and glycemic control via relations with disease-specific knowledge and with personal and social motivation as measured by diabetes fatalism and social support, respectively.
We used the self-care domain of the conceptual framework proposed by Paasche-Orlow and Wolf16 to examine the relationships between health literacy, determinants of diabetes self-care, and glycemic control in an adult population with type 2 diabetes mellitus (T2DM). The self-care domain posits that the impact of health literacy on health outcomes is mediated by disease-related knowledge, motivation, problem solving skills, self-efficacy, and, in turn, self-care behaviors.16,17 Based on the conceptual underpinnings of this framework, we hypothesized that, among adults with T2DM, health literacy would be related to diabetes self-care via relations with disease-specific knowledge and with personal and social motivation and that health literacy would be indirectly related to glycemic control via relations with these determinants of behavior, which would be linked to diabetes self-care and, in turn, glycemic control.
Subjects and Methods
Sample
We recruited consecutive patients diagnosed with T2DM who had scheduled appointments at the University Internal Medicine Clinic of the Medical University of South Carolina, Charleston, SC. The Institutional Review Board at Medical University of South Carolina approved all procedures prior to study enrollment. Eligible participants were clinic patients, age 18 years or older with a diagnosis of T2DM in the medical record, and a clinic appointment between June and August 2008. Patients were ineligible if they did not speak English or if the research assistant determined (by interaction or chart documentation) they were too ill or cognitively impaired to participate.
Data and procedure
Research assistants reviewed the electronic clinic roster to identify eligible patients. Eligible patients were approached in the clinic waiting room and provided a description of the study. Those interested and eligible were consented and taken to a private area in the clinic to complete the study instruments. The entire assessment took approximately 30–45 min to complete. Participants completed the assessment before or after their scheduled clinic appointments, depending on clinic flow. One hundred thirty subjects were consented and completed all study measures.
We collected data on self-reported age, sex, race/ethnicity, education, household income, and marital status. Additional measures included validated surveys of health literacy, diabetes knowledge, motivation (i.e., diabetes fatalism and social support), and diabetes self-care. Hemoglobin A1c values were extracted from the electronic medical record.
Health literacy
We assessed health literacy by using the Rapid Estimate of Adult Literacy in Medicine, Revised (REALM-R), an eight-item instrument designed to rapidly screen patients for potential health literacy problems. The REALM-R has been previously correlated with the Wide Range Achievment Test Revised (WRAT-R) (r = 0.64) and demonstrated a Cronbach's alpha of 0.91.18 The REALM-R is scored on a scale from 0 to 8 and asks patients to read a series of eight medical words and a correct response is given for each correct pronunciation. Scores of six or less correspond to a 6th grade or less reading level and identify patients at risk for poor health literacy.18
Diabetes knowledge
Diabetes knowledge was assessed with the Diabetes Knowledge Questionnaire (DKQ),19 a 23-item instrument that elicits information about a respondent's understanding of the cause of diabetes, types of diabetes, self-management skills, and complications of diabetes. Responses are graded as “yes,” “no,” or “don't know.” The final score is based on the percentage of correct scores, with a maximum possible score of 100.19
Diabetes fatalism
Diabetes fatalism served as our measure of personal motivation and was assessed with the 18-item Diabetes Fatalism Scale (DFS-18).20 Diabetes fatalism is operationally defined as “a complex psychological cycle characterized by perceptions of despair, hopelessness, and powerlesseness.” Items are scored on a 6-point Likert scale with scores ranging from 1 = strongly disagree to 6 = strongly disagree. Higher scores represent more fatalistic attitudes (i.e., less personal motivation). A summary score consisting of the sum of individual items is created, such that higher scores represent greater fatalistic attitudes. The DFS-18 has good internal consistency (Cronbach's alpha = 0.73) and response variability (range, 30–90; mean, 58.2; SD, 6.8).20
Social support
Social support served as our measure of social motivation and was assessed with the 19-item Medical Outcomes Study (MOS) Social Support Survey.21 The MOS measures perceived general functional support in four domains—emotional/informational, tangible, positive social interaction, and affection—and yields an overall support index, which was used in our analysis.
Diabetes self-care
Diabetes self-care was assessed with the 11-item Summary of Diabetes Self-Care Activities (SDSCA) scale.22 The SDSCA scale measures frequency of diabetes self-care in the past 7 days for five aspects of the diabetes regimen: two items for general diet (followed healthful diet), two items for specific diet (ate fruits/low fat diet), two items for foot care, two items for blood-glucose testing, two items for exercise, and one item for cigarette smoking. Response options range from 0 to 7 to correspond to the number of days in a week. The average score across items for each subscale or, in the instance of cigarette smoking, score for one item represents the frequency of performing the self-care behavior in the past 7 days.
Glycemic control
Patients' most recent hemoglobin A1c value was extracted from the medical record and served as our measure of glycemic control.
Statistical analysis
Descriptive statistics were performed using SPSS version 17.0 (SPSS Inc., Chicago, IL). In our previous work,23 a confirmatory factor analytic model (CFA) was estimated using AMOS version 17.0, a structural equation modeling program. The CFA model tested the measurement model (i.e., the latent variable diabetes self-care was predicted to load onto six measured variables: general diet, specific diet, foot care, blood glucose testing, exercise, and cigarette smoking), and was tested for data fit. Variables with nonsignificant factor loadings were omitted from the measurement model nested in the structural equation model.
Next, we performed a series of structural equation models. Advantages of this procedure include the generality and flexibility of model specification and the ability to assess fit of the hypothesized model to the observed data. The likelihood ratio χ2 tests are reported, but model fit was primarily evaluated with the comparative fit index and root mean square of approximation (RMSEA).24,25 A comparative fit index value can range from 0 to 1, where 1 indicates perfect data fit, 0.9 indicates adequate fit, and 0.8 is considered marginal fit.25 An RMSEA value can range from 0 to 1, with smaller values indicating closer fit; specifically, values at 0.06 or lower indicate close fit,26 values at 0.08 or lower indicate reasonable fit, and values greater than or equal to 0.10 indicate poor fit.24,25
Hypotheses regarding the specific structural relations of the constructs in the model were also evaluated through inspection of the direction and magnitude of the path coefficients. A path coefficient is a standardized regression coefficient (beta) showing the direct effect of one variable on another variable. When there are two or more variables, the path coefficient reflects the effect of one variable controlling for all other variables. Path coefficients may be decomposed into direct and indirect effects, corresponding to direct and indirect arrows in a path model. A direct effect occurs when variable A is significantly related to variable B, whereas an indirect effect occurs when variable C is related to variable A and a part of this relationship is transmitted to variable B (i.e., part of that “direct effect” is due to relations between A and C).
Two structural equation models were estimated with a correlation matrix generated by 130 cases, a sample size that providers adequate power to detect medium effects.27 Model 1 tested whether health literacy had a direct effect on diabetes knowledge, diabetes fatalism (personal motivation), and social support (social motivation); whether health literacy had a direct or indirect effect on diabetes self-care; and whether health literacy had a direct or indirect effect on glycemic control. To identify the most parsimonious model, Model 2 tested a trimmed version of the aforementioned model, which included all significant paths to diabetes self-care and glycemic control, omitting all nonsignificant paths.
Results
Sample characteristics
A total of 130 men and women with T2DM completed all measures noted above. Participants were, on average, 63 years old. As shown in Table 1, the majority of the sample was female (72.5%), African American (71.4%), and not working (78.3%) and had health insurance (96.4%). Approximately one-third (29.7%) of the sample had limited health literacy skills according to the REALM-R.
Table 1.
Sample Demographics
| Demographics | Mean ± SD or % |
|---|---|
| Mean age (years) | 62.7 ± 11.8 |
| Age categories | |
| 18–49 years | 14.5 |
| 50–64 years | 36.2 |
| 65+ years | 49.3 |
| Females | 72.5 |
| Race/ethnicity | |
| Non-Hispanic white | 28.6 |
| Non-Hispanic black | 71.4 |
| Mean education (years) | 12.4 ± 5.2 |
| Education categories | |
| <High school graduate | 34.1 |
| High school graduate | 34.1 |
| >High school graduate | 31.8 |
| Married | 41.2 |
| Unemployed | 78.3 |
| Income categories | |
| <$10,000 | 19.6 |
| $10,000–<$15,000 | 26.1 |
| $15,000+ | 54.3 |
| Insurance status | |
| Individual plan | 15.2 |
| Group plan | 13.8 |
| Medicaid | 31.2 |
| Medicare | 36.2 |
| None/uninsured | 3.6 |
| Health status | |
| Better than last year | 19.6 |
| Worse than last year | 26.1 |
| Same as last year | 54.3 |
| Health literacy | |
| REALM-R scores ≤6 | 29.7 |
| REALM-R scores 6+ | 70.3 |
REALM-R, Rapid Estimate of Adult Literacy in Medicine, Revised.
Health literacy, diabetes self-care, and glycemic control
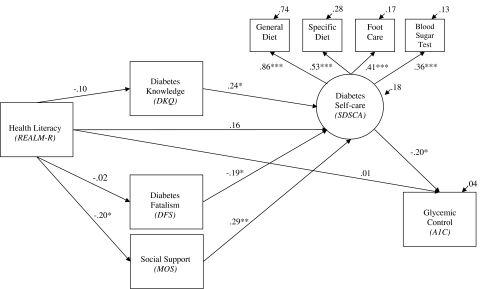
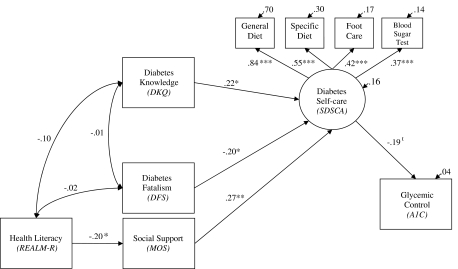
As shown in Figure 1, health literacy did not have a direct effect on diabetes knowledge, diabetes fatalism, diabetes self-care, or glycemic control. Diabetes knowledge (r = 0.22, P < 0.05), diabetes fatalism (r = −0.22, P < 0.05), and social support (r = 0.27, P < 0.01) each had a direct effect on diabetes self-care. Diabetes self-care, in turn, had a direct effect on glycemic control (r = −0.020, P < 0.05). Health literacy had a direct effect on social support (r = −0.20, P < 0.05) and, through social support, had an indirect effect on diabetes self-care (r = −0.07) and indirect effect on glycemic control (r = −0.01). Figure 2 presents the trimmed version of this model with all significant paths to diabetes self-care and glycemic control, omitting all nonsignificant paths to these outcomes.
FIG. 1.
Relationships between health literacy, diabetes knowledge, diabetes fatalism, social support, diabetes self-care, self-care, and glycemic control (full model). Note that coefficients are standardized path coefficients. Overall model fit, χ2 (23, n = 130) = 21.27, P = 0.56, comparative fit index = 1.00, root mean square of approximation = 0.00 (90% confidence interval, 0.00–0.06). For tests of significance of individual paths, *P < 0.05, **P < 0.01, and ***P < 0.001. A1C, hemoglobin A1c; DFS, Diabetes Fatalism Scale; DKQ, Diabetes Knowledge Questionnaire; MOS, Medical Outcomes Study; REALM-R, Rapid Estimate of Adult Literacy in Medicine, Revised; SDSCA, Summary of Diabetes Self-Care Activities.
FIG. 2.
Relationships between health literacy, diabetes knowledge, diabetes fatalism, social support, diabetes self-care, self-care, and glycemic control (trimmed model). Note that coefficients are standardized path coefficients. Overall model fit, χ2 (24, n = 130) = 23.91, P = 0.47, comparative fit index = 1.00, root mean square of approximation = 0.00 (90% confidence interval, 0.00–0.07). For tests of significance of individual paths, *P < 0.05, **P < 0.01, and ***P < 0.001. A1C, hemoglobin A1c; DFS, Diabetes Fatalism Scale; DKQ, Diabetes Knowledge Questionnaire; MOS, Medical Outcomes Study; REALM-R, Rapid Estimate of Adult Literacy in Medicine, Revised; SDSCA, Summary of Diabetes Self-Care Activities.
Discussion
We performed cross-sectional structural equation modeling on data collected from adult patients with T2DM receiving care at an academic medical center. Consistent with the conceptual framework of Paasche-Orlow and Wolf16 and our study hypotheses, health literacy did not have a direct effect on diabetes self-care or glycemic control. We included our diabetes knowledge, diabetes fatalism, and social support, in the predicted pathways linking health literacy to diabetes self-care. Our findings suggest health literacy has an indirect effect on diabetes self-care and glycemic control through social support.
The research linking health literacy to glycemic control has been mixed.10,11 For studies with null findings, our results provide an alternative explanation, namely, that patients with diabetes and limited health literacy may be eliciting support from significant others (e.g., providers, family, friends, and caregivers) to perform diabetes self-care needed for glycemic control. When this occurs, health literacy does not have a direct effect on glycemic control. Instead, it has an indirect effect through determinants of diabetes self-care, and, in turn, diabetes self-care in and of itself. Intervening with patients with diabetes and limited health literacy who do not have social support and identifying other determinants of diabetes self-care that can be targeted to address health literacy limitations is an area of research that needs greater attention and may inform clinical practice.28
There are limitations to this study that should be acknowledged. First, although our findings propose causal relationships between variables, the cross-sectional nature of the data precludes causal conclusions and can most appropriately speak to associations between constructs observed at a single point in time. Consequently, we have relied on theory and the research literature to direct our conclusions. Future prospective research is needed to investigate the longitudinal effects of these constructs on changes in health behaviors and health outcomes.
Second, participants were recruited from a single outpatient clinic at a single academic medical center. It is unclear if our findings would generalize to other types of clinics (e.g., inpatient) and care facilities (e.g., federally qualified health centers). Future work across settings would provide a more comprehensive conceptualization of the core constructs believed to implicate health literacy as a barrier to performing diabetes self-care and thus receiving the hemoglobin A1c benefits of doing so.
Third, diabetes studies have used different assessments of health literacy. Although we measured health literacy with the REALM-R, which has demonstrated strong reliability and construct validity,18 there have been no published studies to date reporting its predictive validity. The REALM-R was not predictive of diabetes knowledge, diabetes self-care, or glycemic control in our study. While our findings suggest health literacy as measured by the REALM-R does have an indirect effect on diabetes self-care and glycemic control through a direct effect on social support, finding no direct effect on these outcomes with or without social support in the predictive pathway may be indicative of a measurement limitation. Future studies should examine the REALM-R's predictive validity with diabetes outcomes18 and provide additional support for our findings with other measures of health literacy.29–31
Fourth, we did not control for when participants completed the survey in our analyses. While bias might have been introduced by when participants completed the survey (i.e., participants felt more support after meeting with their provider and inflated their estimates of social support), this is an unlikely possibility because only a small proportion (<20%) of participants completed the survey after their provider visit. This should be verified and accounted for in future research.
Finally, we did not collect information on other factors believed to explain the relationship between health literacy and health outcomes in the conceptual framework of Paasche-Orlow and Wolf.16 This framework assumes health literacy indirectly impacts health outcomes through a direct effect on system-level factors (access and utilization of health care), provider-level factors (provider–patient interaction), and individual-level factors (determinants of self-care). Our study only tested two factors in the individual level factors domain, specifically, disease-specific knowledge and motivation as measured by diabetes fatalism and social support. Future models should include system-level factors (e.g., patient navigation skills and system complexity), provider-level factors (e.g., patient participation in decision-making and provider communication skills), and additional individual-level factors (e.g., disease management self-efficacy and problem solving skills), which may explain more of the variability in the sequence of intervening variables linking health literacy to diabetes self-care and glycemic control.
Despite these limitations, this study is the first to our knowledge to show the indirect effect of health literacy on diabetes self-care via widely recognized determinants of diabetes self-care (i.e., diabetes knowledge and personal and social motivation), an indirect effect on glycemic control via the aforementioned indirect effect, and the direct effect of diabetes self-care on glycemic control. Our findings are just one step in what should be an iterative process of model specification and clarification. Future studies that can both validate our findings and extend them would provide the most useful explanation of the relationship between health literacy and health outcomes in diabetes and inform professional responses to the problem in many diverse contexts of health care.32 In the meantime, health literacy-sensitive interventions should aim to provide social support and teach patients how to elicit support from significant others to facilitate the performance of diabetes self-care necessary for glycemic control. Future qualitative and quantitative research to determine the most effective techniques to promote social support among patients with limited health literacy is needed.
Our findings suggest the role social support links health literacy to health outcomes for adult patients with T2DM, highlighting the potential impact of peer navigators, providing instrumental and practical support to patients, and teaching patients how to cultivate a supportive environment to manage their diabetes as a means of improving glycemic control. Healthcare providers can also function as liaisons between patients and their social support networks (e.g., caregivers, relatives), communicating the types of support that would be most beneficial for a patient.33 In these discussions, providers can encourage patients to effectively communicate their request of the type of social support, the amount, and timing of support they need from a caregiver. Providers can also serve as a source of support for a patient and help patients identify other sources of support. Social support is a complex and multifaceted construct, understanding the problematic aspects in addition to the supportive aspects is important to effectively tailor interventions that utilize social support to improve the health of patients with limited health literacy.
Acknowledgments
C.Y.O. is supported by a Diversity Supplement Award (NIDDK P60 DK020593).
Author Disclosure Statement
No competing financial interests exist.
References
- 1.Institute of Medicine. Health Literacy: A Prescription to End Confusion. Washington, DC: National Academies Press; 2004. [PubMed] [Google Scholar]
- 2.Davis TC. Wolf MS. Health literacy: implications for family medicine. Fam Med. 2004;36:595–598. [PubMed] [Google Scholar]
- 3.Torres RY. Marks R. Relationships among health literacy, knowledge about hormone therapy, self-efficacy, and decision-making among postmenopausal health. J Health Commun. 2009;14:43–55. doi: 10.1080/10810730802592247. [DOI] [PubMed] [Google Scholar]
- 4.Wolf MS. Davis TC. Cross JT. Marin E. Green K. Bennett CL. Health literacy and patient knowledge in a Southern US HIV clinic. Int J STD AIDS. 2004;15:747–752. doi: 10.1258/0956462042395131. [DOI] [PubMed] [Google Scholar]
- 5.Gazmararian JA. Williams MV. Peel J. Baker DW. Health literacy and knowledge of chronic disease. Patient Educ Couns. 2003;51:267–275. doi: 10.1016/s0738-3991(02)00239-2. [DOI] [PubMed] [Google Scholar]
- 6.Osborn CY. Paasche-Orlow MK. Davis TC. Wolf MS. Health literacy: an overlooked factor in understanding HIV health disparities. Am J Prev Med. 2007;33:374–378. doi: 10.1016/j.amepre.2007.07.022. [DOI] [PubMed] [Google Scholar]
- 7.Bautista RE. Glen ET. Shetty NK. Wludyka P. The association between health literacy and outcomes of care among epilepsy patients. Seizure. 2009;18:400–404. doi: 10.1016/j.seizure.2009.02.004. [DOI] [PubMed] [Google Scholar]
- 8.Baker DW. Wolf MS. Feinglass J. Thompson JA. Health literacy, cognitive abilities, and mortality among elderly persons. J Gen Intern Med. 2008;23:723–726. doi: 10.1007/s11606-008-0566-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Baker DW. Wolf MS. Feinglass J. Thompson JA. Gazmararian JA. Huang J. Health literacy and mortality among elderly persons. Arch Intern Med. 2007;167:1503–1509. doi: 10.1001/archinte.167.14.1503. [DOI] [PubMed] [Google Scholar]
- 10.Schillinger D. Grumbach K. Piette J. Wang F. Osmond D. Daher C. Palacios J. Sullivan GD. Bindman AB. Association of health literacy with diabetes outcomes. JAMA. 2002;288:475–482. doi: 10.1001/jama.288.4.475. [DOI] [PubMed] [Google Scholar]
- 11.Schillinger D. Barton LR. Karter AJ. Wang F. Adler N. Does literacy mediate the relationship between education and health outcomes? A study of a low-income population with diabetes. Public Health Rep. 2006;121:245–254. doi: 10.1177/003335490612100305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Morris NS. MacLean CD. Littenberg B. Literacy and health outcomes: a cross-sectional study in 1002 adults with diabetes. BMC Fam Pract. 2006;7:49. doi: 10.1186/1471-2296-7-49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Powell CK. Hill EG. Clancy DE. The relationship between health literacy and diabetes knowledge and readiness to take health actions. Diabetes Educ. 2007;33:144–151. doi: 10.1177/0145721706297452. [DOI] [PubMed] [Google Scholar]
- 14.Mancuso JM. The impact of health literacy and patient trust on glycemic control. West J Nurs Res. 2009;31:1086–1087. doi: 10.1177/0193945909342548. [DOI] [PubMed] [Google Scholar]
- 15.von Wagner C. Steptoe A. Wolf MS. Wardle J. Health literacy and health actions: a review and a framework from health psychology. Health Educ Behav. 2009;36:860–877. doi: 10.1177/1090198108322819. [DOI] [PubMed] [Google Scholar]
- 16.Paasche-Orlow MK. Wolf MS. The causal pathways linking health literacy to health outcomes. Am J Health Behav. 2007;31(Suppl 1):S19–S26. doi: 10.5555/ajhb.2007.31.supp.S19. [DOI] [PubMed] [Google Scholar]
- 17.Osborn CY. Paasche-Orlow MK. Bailey SC. Wolf MS. The mechanisms linking health literacy to behavior, health status. Am J Health Behav. 2011;35:118–128. doi: 10.5993/ajhb.35.1.11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Bass PF., 3rd Wilson JF. Griffith CH. A shortened instrument for literacy screening. J Gen Intern Med. 2003;18:1036–1038. doi: 10.1111/j.1525-1497.2003.10651.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Garcia AA. Villagomez ET. Brown SA. Kouzekanani K. Hanis CL. The Starr County Diabetes Education Study: development of the Spanish-language diabetes knowledge questionnaire. Diabetes Care. 2001;24:16–21. doi: 10.2337/diacare.24.1.16. [DOI] [PubMed] [Google Scholar]
- 20.Egede LE. Ellis C. Diabetes fatalism, health-related quality of life and glycemic control in adults with type 2 diabetes [abstract] Diabetes. 2008;57(Suppl 1):A244. [Google Scholar]
- 21.Sherbourne CD. Stewart AL. The MOS social support survey. Soc Sci Med. 1991;32:705–714. doi: 10.1016/0277-9536(91)90150-b. [DOI] [PubMed] [Google Scholar]
- 22.Toobert DJ. Hampson SE. Glasgow RE. The summary of diabetes self-care activities measure: results from 7 studies and a revised scale. Diabetes Care. 2000;23:943–950. doi: 10.2337/diacare.23.7.943. [DOI] [PubMed] [Google Scholar]
- 23.Osborn CY. Egede LE. Validation of an Information-Motivation-Behavioral Skills model of diabetes self-care (IMB-DSC) Patient Educ Couns. 2010;79:49–54. doi: 10.1016/j.pec.2009.07.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Bentler PM. Comparative fit indexes in structural models. Psychol Bull. 1990;107:238–246. doi: 10.1037/0033-2909.107.2.238. [DOI] [PubMed] [Google Scholar]
- 25.Ridgon E. CFI versus RMSEA: comparison of two fit indexes for structural equation modeling. Struct Equ Modeling. 1996;3:369–379. [Google Scholar]
- 26.Hu L. Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: conventional criteria versus new alternatives. Struct Equ Modeling. 1999;6:1–55. [Google Scholar]
- 27.MacCallum RC. Browne MW. Sugawara HM. Power analysis and determination of sample size for covariance structure modeling. Psychol Methods. 1996;1:130–149. [Google Scholar]
- 28.Lee SY. Arozullah AM. Cho YI. Health literacy, social support, and health: a research agenda. Soc Sci Med. 2004;58:1309–1321. doi: 10.1016/S0277-9536(03)00329-0. [DOI] [PubMed] [Google Scholar]
- 29.Baker DW. Williams MV. Parker RM. Gazmararian JA. Nurss J. Development of a brief test to measure functional health literacy. Patient Educ Couns. 1999;38:33–42. doi: 10.1016/s0738-3991(98)00116-5. [DOI] [PubMed] [Google Scholar]
- 30.Davis TC. Long SW. Jackson RH. Mayeaux EJ. George RB. Murphy PW. Crouch MA. Rapid estimate of adult literacy in medicine: a shortened screening instrument. Fam Med. 1993;25:391–395. [PubMed] [Google Scholar]
- 31.Davis TC. Crouch MA. Long SW. Jackson RH. Bates P. George RB. Bairnsfather LE. Rapid assessment of literacy levels of adult primary care patients. Fam Med. 1991;23:433–435. [PubMed] [Google Scholar]
- 32.Jukkala A. Deupree JP. Graham S. Knowledge of limited health literacy at an academic health center. J Contin Educ Nurs. 2009;40:298–302. doi: 10.3928/00220124-20090623-01. quiz 303–304, 336. [DOI] [PubMed] [Google Scholar]
- 33.Boutin-Foster C. Getting to the heart of social support: a qualitative analysis of the types of instrumental support that are most helpful in motivating cardiac risk factor modification. Heart Lung. 2005;34:22–29. doi: 10.1016/j.hrtlng.2004.09.002. [DOI] [PubMed] [Google Scholar]