Abstract
Objectives. We assessed the determinants of health care funding allocations among South Africa's provinces and their effects on health care from 1996 through 2007.
Methods. We performed multivariate regression of funding allocation data against measures of disease burden and health system infrastructure by province.
Results. Disease burden was increasingly negatively correlated with funding allocations and explained less than one quarter of the variation in allocations among provinces. Nearly three quarters of the variation in allocations was explained by preexisting hospital infrastructure and health care workers. The density of private hospitals in the preceding year was associated with greater government allocations (bprivate = 0.12; 95% confidence interval [CI] = 0.08, 0.15), but public hospital density in the preceding year was not (bpublic = 0.05; 95% CI = −0.02, 0.11). Greater allocations were associated with a higher number of doctors (b = 0.54; 95% CI = 0.34, 0.75) but fewer nurses (b = −0.37; 95% CI = −0.72,−0.25) in the same year.
Conclusions. Regions with a greater capacity to spend funds received more funding and created more infrastructure than those with greater health needs. Historical infrastructure inequalities may have created an infrastructure–inequality trap, in which the distribution of funds to those with greater “absorptive capacity” exacerbates inequalities.
“Freedom for South Africa has brought the opportunity at last to address the basic needs of our people. It allows us not only to attend to immediate health needs, but also to begin to eradicate the legacy of poverty and inequity that is the greatest threat to our public health.”
—Nelson Mandela1a(p375)
When apartheid ended in South Africa in 1994, many saw it as an opportunity to redress inequalities that underpinned the country's health care system. As a middle-income country, South Africa had provided world-class care for White elites, including the world's first heart transplant, while denying many in the majority populations access to appropriate health care services.1b Spatial segregation between populations was a prominent method to sustain inequality, with racially biased policies leading to the creation of “Black homelands” that detached the poorest areas from regions with better health care infrastructure (Figure 1).
FIGURE 1.
South Africa's provinces.
Source. http://en.wikipedia.org/wiki/File:Map_of_South_Africa_with_English_labels.svg.
In the late 1980s, South African health care researchers called for a needs-based formula to redistribute health resources more equitably.2 But it was not until Nelson Mandela and the African National Congress came to power in 1994 that the national government explicitly addressed health equity and access for the majority population. Health care was enshrined as a constitutional right, and over the next few years the government constructed new health care facilities, provided free maternal and child care, and created new programs for water, nutrition, and welfare.3
However, South Africa's economic growth slowed toward the end of Mandela's presidency, turning negative by 1998. Hard economic times reduced the resources available for redistribution just as health services faced increasing demands from patients with HIV/AIDS. The government introduced programs to improve efficiency and reduce budget deficits.4
Despite the government's commitment to health equity, some analysts expressed concerns that poorer provinces were unable to manage the funds allocated to them.5 In response to this criticism, 2 significant reforms in the late 1990s changed how health care funds were distributed. First, instead of the Minister of Health allocating earmarked health resources to disadvantaged regions, the Department of Finance disbursed block grants for general social spending to each province on the basis of the Treasury's “Equitable Shares” formula. Provincial ministers then allocated the majority of funds for health care spending within each province out of this block grant,6 although conditional grants for specific diseases (e.g., HIV/AIDS) were also made available for disadvantaged provinces. Critics of this reform held that poor provinces had less spending autonomy because the Equitable Shares formula rewarded provinces according to economic output, rather than exclusively basing allocations on need; thus, poor provinces relied more heavily on conditional health grants to address their high burden of disease.7
Second, the government introduced a growth, employment, and redistribution (GEAR) strategy that emphasized privatization and fiscal austerity. Comprehensive implementation of GEAR reforms began after Thabo Mbeki assumed the presidency in 1999.8 The change in administration coincided with declines in public health spending and a substantial increase in private-sector investment in health care, particularly in the wealthiest provinces.9
When health policy aims to maximize efficiency, as intended by GEAR, it may be logical in the short run to distribute more resources to rich provinces with better health infrastructure10 because the regions can use the available funds more rapidly to meet health needs. In the long run, however, resource-deprived settings would benefit more from the additional funds required to develop new capacity. If health spending was distributed to those areas with the most capacity, this would create a self-perpetuating cycle of inequality, or what we call an infrastructure–inequality trap. According to this logic, the inequitable distribution of health infrastructure during apartheid would continue to affect distribution of health funding today.
To determine how South Africa's historical inequalities in health care resources may have been affected by these economic and administrative changes, we used multivariate regression to examine how health spending patterns among South Africa's provinces have related to system capacity and disease burden since the end of apartheid.
METHODS
Data on health care funding allocations, capacity, and disease burden were taken from the South African Health Systems Trust Database (number of doctors and nurses, allocations per capita)9 and the Hospital and Nursing Yearbook series11–13 (number of hospitals in total and per 100 000 population). We measured health care funding allocations as spending per capita adjusted for inflation, using the consumer price index as described in the annual reports of the South African Council for Medical Schemes.14,15 The burden of disease was measured as antenatal HIV prevalence, infant mortality, and crude death rates.9 We smoothed the data over a 3-year span to isolate general trends, reduce measurement errors, and maximize the sample size. We also ran our regressions without this step and found that none of the effect sizes in our regressions were affected by use of this technique.
Differences in health care spending were principally determined by 3 factors: (1) the National Treasury's allocations to the provinces for social spending, (2) provinces' allocations to health system spending, and (3) conditional disease grants made by the Treasury to the Health Ministry, which then provided the funds to the provinces.
The National Treasury's Equitable Shares formula has varied over time. The formula comprises measures of need for education (public school enrollments), health (dependents on government-funded medical aid), poverty, and economic activity (based on the province's gross geographic product).16 Between 1999 and 2005, a backlog component was introduced to account for historical disparities in physical infrastructure.17 The relative weight assigned to each component remained a political decision made by the national and provincial finance ministers. The weight assigned to the backlog component was never greater than 3% of the total formula. Treasury officials wanted to ensure that funds flowed to provinces able to absorb them (Di McIntyre, PhD, personal communication, 2009); they also wanted to encourage urban migration, which was seen as a way of tackling inequalities over the long term.18
A province's burden of disease and its health infrastructure, or “absorptive capacity,”19 are not explicitly included in the formula. Hence, although the explicit inclusions in the allocation formula are known, the political decisions concerning how to weight the formula's components and how to allocate funds to health after block grants are distributed are poorly understood. We sought to assess determinants of the variation in health care funding allocations per capita across provinces by examining how funding allocations related to disease burden and health care infrastructure in the preceding year. Thus, our model is
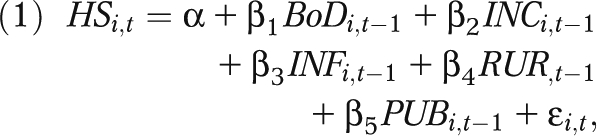 |
where i is the province, t is the year, HS denotes total per capita public health spending in province i in fiscal year t, BoD refers to the province's burden of disease as measured by the health indicators we listed, INC is income as measured by the log of the province's gross domestic product per capita20 (reflecting the economic activity component of the Treasury formula), INF is the province's health care infrastructure and resources (measuring the province's capacity to absorb funds), RUR is a dummy for the 4 provinces with the largest rural and impoverished populations (i.e., the backlog component), and PUB is the log of the province's public sector–dependent population, as the social service component.
In a second step, to identify whether changes in public health care allocations translated into inequalities in health infrastructure, we estimated
where X is a set of control variables—including disease burden, income levels, and other factors from equation 1—that may affect the current year's infrastructure or alter the relationship between health spending and health capacity development.
Because regression models estimate β = ∂Y/∂X, or the change in one variable with respect to the change in another variable, we can ascertain the effect of an increase in infrastructure capacity on the rate of capacity development by combining equations 1 and 2 as follows:
This permitted us to assess how inequalities in preexisting infrastructure affected health allocations and how these allocations further related to health capacity development. We ran regression models in Stata version 9.2 (StataCorp LP, College Station, TX).
RESULTS
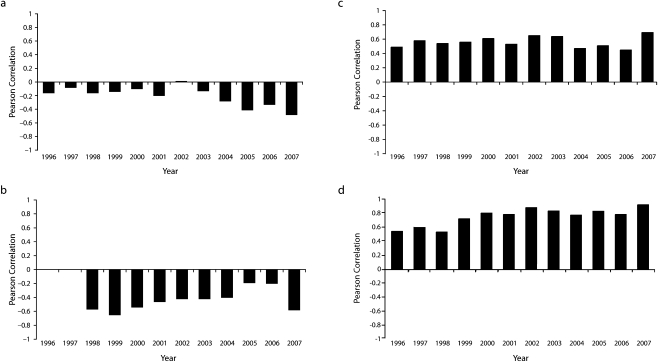
Figure 2 presents the trends in correlations between health care allocations and measures of disease burden, income, and race in South African provinces from 1996 through 2007. We observed an inverse relationship between allocations and measures of disease burden, which increased over time. In the case of HIV, health allocations became slightly more in line with the disease burden up through 2002, but then the scale of the inverse association substantially increased afterward as HIV prevalence rose and allocations did not respond to the growing burden (Figure 2a). Throughout the period, provinces with greater existing infrastructure and a greater proportion of persons of White race among the population gained more resources at the expense of those provinces with greater health burdens and fewer resources (Figure 2c and 2d). By 2007, the provinces of South Africa with the greatest health burdens (Figure 2a and 2b), least economic resources (Figure 2c), and largest Black populations (Figure 2d) received the smallest shares of national public health care funds.
FIGURE 2.
Relationship between health spending and antenatal HIV prevalence (a), infant mortality rates (b), income per capita (c), and White population (d): South Africa's provinces, 1996–2007.
Note. Bars above the x-axis indicate a positive correlation; bars below indicate a negative correlation. Pearson coefficients are presented for 46 correlations across South Africa's 9 provinces for each year from 1996 to 2007. Higher public spending was associated with higher levels of antenatal HIV prevalence, income per capita, White population, and infant mortality (r > 0). Infant mortality and income per capita are used in log form to adjust for positive skew. Similar results were observed using Spearman correlations and relative health spending data (data not shown).
Source. Data on income per capita and White population ranking were obtained from the Statistics South Africa database. Data on antenatal HIV prevalence and infant mortality rates were obtained from the South Africa Health Systems Trust database and were available for 1996–2007 and 1998–2007, respectively.
Determinants of Inequalities in Health Care Spending
Table 1 shows that 3 general measures of burden of disease—HIV prevalence, infant mortality rates, and crude total death rates—explain roughly one fifth of the variation in health spending among the provinces from 2001 to 2007, the period of GEAR implementation. However, only infant mortality rates showed a statistically significant association with spending, and the association was in the opposite direction from an equitable distribution: greater infant mortality rates corresponded to lower health spending in the next fiscal year, which is consistent with the correlations we noted earlier (bimr = −0.31; P < .001).
TABLE 1.
Determinants of Provincial Health Care Funding Allocations: South Africa Health System Trust Database, 2007
| Covariates (year prior to funding allocations) | Unadjusted Bivariate Regression,a b (P) | Adjusted Multivariate Regression |
|
| Separate Models,b b (P) | Full Model, b (P) | ||
| Disease burden | |||
| Antenatal HIV prevalence | –0.31% (.358) | −0.07% (.863) | 0.07% (.8) |
| Infant mortality rates | −0.31% (< .001) | −0.37% (< .001) | −0.14% (.059) |
| Crude death rates | 0.02% (.897) | 0.28% (.121) | 0.013% (.913) |
| Model R2 | R2 = 0.21 | ||
| Treasury formula for economic activity | |||
| Income level | 0.26% (< .001) | −0.0002% (.998) | −0.37% (< .001) |
| Rural dummy | −23.41% (< .001) | −28.58% (< .001) | −4.34% (.504) |
| Public-sector dependents | −0.05% (.196) | −0.11% (.004) | −0.13% (.186) |
| Model R2 | R2 = 0.48 | ||
| Health system capacity | |||
| Hospitals | 0.26% (< .001) | 0.24% (< .001) | 0.24% (< .001) |
| Doctors | 0.08% (.069) | 0.27% (< .001) | 0.49% (< .001) |
| Nurses | −0.04% (.174) | −0.12% (.001) | −0.20% (< .001) |
| Model R2 | R2 = 0.73 | R2 = 0.85 | |
Note. The log of real public health spending per capita is the dependent variable. Parameter estimates are the percentage increase in the dependent variable given a 1% increase in the covariate (elasticity). Results were similar when evaluating the relative proportion of resources allocated to each province, rather than differences in the absolute levels of resources. The number of provinces is n = 9; the number of province-years is n = 54.
Results are presented from 9 bivariate regression models.
Results are presented from 3 multivariate regression models using variables for disease burden, Treasury formula for economic activity, and absorptive capacity.
Given the limited explanatory power of the burden of disease data, we next turned to other factors that may have driven the observed trends in health care funding allocation. We first included the major factors used in the economic activity and backlog components of the Treasury's redistribution formula, including the size of the public-sector-dependent population, average provincial income, and a measure of the percentage of the population living in rural settings. These 3 factors explained roughly half of the variance in health fund allocations across provinces (R2 = 0.48). Regions that were more rural received 28.6% less government funding on average than regions that were more urban (95% confidence interval [CI] = 8.9%, 46.8%), and having a larger population dependent on the public sector also corresponded to lower health spending (b = −0.11%; P = .004). We found that greater economic activity corresponded to higher allocations, but this association was not statistically significant; hence, variations in provincial income alone are unlikely to account for overall trends in spending.
Next, we tested whether greater absorptive capacity was associated with differences in health care spending. Measures of health system capacity included hospitals, doctors, and nurses per capita. These 3 factors explained roughly three quarters of the variation in health funding among provinces (R2 = 0.73).
In models including components for burden of disease, economic activity, and absorptive capacity, greater existing infrastructure remained a strong determinant of higher health expenditure during the 2002–2007 period, corresponding to the period of the Mbeki administration (Table 1). In the fully adjusted model, each percentage point increase in the number of doctors was associated with a 0.49% increase in health spending (P < .01). More nurses, on the other hand, were negatively associated with health spending in the fully adjusted model (b = −0.20; P < .01), which is consistent with the interpretation that nurses substitute for doctors in poorer provinces, where the latter are scarce.
Private Versus Public Infrastructure
When evaluating changes in South Africa's health care infrastructure, it is important to differentiate between the public and private sectors. Beginning in the late 1980s, when there were concerns among the White population about the possibility of desegregation, South Africa experienced substantial growth in private hospital development. The new private hospitals, at least initially, catered primarily to the White population.1b The increase in private hospitals accelerated during the 1990s, reflecting pressure to reduce the budget deficit and an international climate favoring private-sector provision of health care. For example, in Gauteng Province, 20 new private hospitals opened from 1998 through 2004, so that 128 of the province's 157 hospitals were private. When public and private hospitals were differentiated in our analysis, we found that only private hospitals were more strongly associated with greater spending (bprivate = 0.12; P < .001 vs bpublic = 0.05; P = .15). Although hospitals per capita were moderately correlated with health spending across provinces in 2001 (r = 0.37), the strength of the relationship grew substantially by 2007 (r = 0.83), such that the more health infrastructure a region had, the more health funding it was receiving.
Robustness Checks
We performed a series of robustness checks to test the initial findings. First, we used the Treasury provincial budget documents, which had fewer years of data availability (1998–2007) but had the benefit of having been audited; we found that our main results did not qualtitatively change (see Appendix 1, available as a supplement to the online version of this article at http://www.ajph.org). Second, we used each province's relative health spending—i.e., the province's health expenditures as a percentage of South Africa's total public health spending—as the dependent variable instead of overall health spending per capita. This procedure replicated the findings. We replicated the models by using health spending scaled to the size of the population dependent on public-sector health care as the dependent variable.
We also tested whether the patterns observed could be explained better by Treasury allocations or provincial allocations. Although poorer provinces allocated less of their Treasury allocations to health because they received offsetting conditional grants for specific diseases (e.g., HIV/AIDS), the fraction of resources allocated to health by each province remained relatively constant during the study period, although the size of the conditional grants did not experience real growth.9 Thus, any changes in overall spending over the past decade were primarily being driven by modifications to how the central government distributes resources. When we included provincial allocations to health as a fraction of Treasury allocations in the fully adjusted models, we found that this was not a significant determinant of health financing variation among provinces (see Appendix 2, available as a supplement to the online version of this article at http://www.ajph.org), and our other results were consistent, which reinforced our observation that the disparities observed are being driven by Treasury-to-province allocations rather than province-to-health allocations.
To further examine the utility of the models presented here, we applied the model regression results to 2 very different provinces: South Africa's richest province, Western Cape, and its poorest, Limpopo. In 2007, Western Cape had substantially greater health infrastructure than did Limpopo: 60 private hospitals, 55 public hospitals, and 1246 doctors for a population of 4.8 million, compared with only 6 private hospitals, 44 public hospitals, and 882 doctors for a population of 5.7 million in Limpopo. However, Limpopo had about 50% more nurses per capita than did Western Cape (2756 vs 1866). On the basis of these differences in health capacity, our models estimated a 20% difference in spending resulting from gaps in doctors, a 10% additional difference from nurses, and another 31% from differences in hospitals. This estimate is similar to the magnitude of the observed difference: in 2007, Limpopo spent US $101 per person on health, or 53% less than the amount spent by Western Cape, which spent US $155 per person.
During the study period, funding appears to have been associated more closely with capacity than with disease burden. We then sought to determine whether this was a self-perpetuating situation wherein additional public health funding expanded infrastructure such that regions with greater absorptive capacity continued to receive more funding.
We performed 2 multivariate regressions evaluating the relationship between health care funding and infrastructure development from 2001 through 2007. A 10% increase in health allocations to a given province was associated with a 5.44% increase (95% CI = 3.36%, 7.52%; P < .05) in the number of doctors (b = 0.54; 95% CI = 0.34, 0.75). In contrast, a 10% increase in health allocations to a given province was related to a 3.72% decrease (95% CI = –7.19%, –2.52%; P < .05) in the number of nurses (b = −0.37; 95% CI = −0.72, −0.25).
Infrastructure–Inequality Trap
By combining the findings in Table 1 (linking greater existing infrastructure to higher health allocations) with those from the multivariate regression models evaluating the relationship between health care funding and infrastructure development (linking higher health allocations to health capacity development), it is possible to estimate the effects of inequalities in health capacity on subsequent health spending and infrastructure development.
Table 2 lists South Africa's provinces in descending order from most hospitals (Northern Cape) to fewest hospitals (Limpopo) in 2001. According to our models, a province that had twice as many hospitals per capita as a peer province that was equivalent in other ways would have obtained, on average, 24.2% more health funding, 13.2% more doctors, and 27.3% more hospitals than its peer from 2002 through 2007. Because post-1998 allocations were not substantially adjusted for historical inequalities in health infrastructure, the gap between resource-rich and resource-deprived areas was sustained in health spending (about 110%); as a result, the gaps in doctors (about 60%) and hospitals per capita (about 125%) were also sustained. For example, Northern Cape's health spending rose by US $76 per capita from 2002 through 2007, whereas in Limpopo the rise was US $23 per capita over this period, so that by 2007 Northern Cape was spending US $168 per capita compared with Limpopo's US $101. In addition, by 2007 Northern Cape had roughly twice as many doctors per capita and more than 4 times as many hospitals per capita as Limpopo. Overall, these results were consistent with the scenario of an infrastructure–inequality trap and accounted for the observed perpetuation in inequalities in health care spending and capacity among South Africa's provinces.
TABLE 2.
Estimated Changes in Health Resources Attributable to Presence of Hospitals in 2001, by Province: South Africa, 2002–2007
| Province | Hospitals per 100 000 Population in 2001 | Estimated Attributable Percentage Difference in Health Resources, 2002–2007 |
|
| Health Spending, b | No. of Doctors, b | ||
| Northern Cape | 4.6 | 109.8 | 59.7 |
| Western Cape | 2.8 | 56.6 | 30.8 |
| Free State | 1.9 | 31.5 | 17.1 |
| Eastern Cape | 1.9 | 30.8 | 16.7 |
| Gauteng | 1.6 | 22.1 | 12.0 |
| Kwazulu-Natal | 1.2 | 9.6 | 5.2 |
| Mpumalanga | 1.2 | 9.2 | 5.0 |
| North West | 1.0 | 5.0 | 2.7 |
| Limpopo (Ref) | 0.8 | NA | NA |
Note. Provinces are ordered from greatest (Northern Cape) to least (Limpopo) health care infrastructure per capita in 2001. Parameter estimates are from multivariate models and multivariate regressions evaluating the relationship between health care funding and infrastructure development.
DISCUSSION
Postapartheid South Africa inherited a health system that was profoundly and explicitly inequitable. The multiracial government that came to power in 1994 began a process of addressing many of the existing inequalities. A combination of policy changes that began in 1996 but took effect mainly after 1999 appears to have maintained vast inequalities among wealthy and poor provinces in spite of government mandates and statements favoring redistribution. Our analyses begin to explain how this happened.
We found that South Africa's distribution of health spending was consistent with the inverse care law observed in other poor countries,21 according to which regions with greater health needs receive fewer health resources. We also observed that greater existing capacity was associated with a rise in health care spending and the subsequent rise in spending was associated with expansion of new infrastructure. This cycle appears to have created an infrastructure-inequality trap in which capacity determined new funds, thus widening existing inequalities in health care infrastructure. Despite ostensible efforts to redress historical inequalities by means of the Treasury's Equitable Shares formula, we find that its provincial allocations do not weigh redistribution strongly enough to counteract inequalities or their ongoing inequitable influence on health resource allocations.
As with any statistical study, there were several limitations to our analysis. First, we used the most recent data, which are already a few years old. Second, we were only able to look at the level of provincial spending, although there were persisting inequalities in access to care at an individual level.22 However, we note that of the possible sources of inequality, the Treasury–province allocations appear to be more powerful than the provincial-health allocations. Third, as South Africa contains only 9 provinces, the available observations were relatively few compared with those of countries with a large number of territorial divisions. However, because the effect sizes were so large, the low numbers of observations did not impede our ability to investigate the trends in inequality and their possible causes at the provincial level or to obtain statistically significant results.
Finally, our measures of disease burden were crude, incorporating antenatal HIV prevalence, crude death rates, and infant mortality. This constraint reflected the limited availability of health-sector data in South Africa. Despite great achievements in a few sentinel surveillance sites, especially those within the INDEPTH (International Network for the Demographic Evaluation of Populations and Their Health in Developing Countries) network,23 vital registration remains far from perfect24; nevertheless, the situation in South Africa is considerably better than that in the rest of Africa.25 Although such data were not available for our study, they were not available to those deciding how to allocate health funds either; hence, our assessment did not use any information to which policymakers did not have access.
We also identified and overcame a number of problems with the data. We found that several items reported in the Health Statistics Trust data set, such as data on hospitals and financing, had structural breaks (e.g., the inclusion of mining hospitals) and needed to be transformed before being used for comparative analysis. We ultimately gathered hospital data from the Hospital and Nursing Yearbook series to ensure consistently reported data. Financing data had been presented in a variety of formats, and these were rescaled to the total population and converted to constant US dollars. Future research should attempt to investigate the inequalities in financial allocations occurring at the health district and medical district level once comprehensive data of this nature become available.
Finally, although economic transformations since 2001 (during the Mbeki administration and the GEAR program) were clearly linked to significant transformations in resource allocation and prospects for health equity, it was beyond the scope of our study to isolate the specific policy processes—some of which appear to be unavailable to the public—that led to rising inequalities in health spending and infrastructure. As others have noted, the health policy process in South Africa is complex, involving multiple actors and specific contexts26; in the past, disagreements among actors have been obstacles to the development of health care financing reforms that might have been more equitable.27
We found that health system capacity, measured by numbers of doctors and hospitals, emerged as a significant driver of inequalities in health spending. Human resources have been attracting increasing attention as an important factor when seeking to scale up health care investment and can be considered a measure of absorptive capacity.19 Although the postapartheid government recognized early on that the scarcity of human resources was a barrier to scaling up basic health services, the measures put in place to address this problem do not seem to have been effective.28 Other research in 3 South African provinces and interviews with Treasury civil servants suggest that implementation capacity, a function of availability of managerial staff, is at least as important as a shortage in the number of health care workers.16 There is also evidence of uneven distribution of the limited number of staff available, a situation exacerbated by better conditions in the private sector and HIV programs.29
After correcting for the association of rich regions with lower numbers of public hospitals and higher numbers of private hospitals, we found that existing private hospital capacity was also an important determinant of health care funding allocations and infrastructure development. (The same was not true for existing public hospital capacity.) Although an explanation of this phenomenon was beyond the scope of this analysis, we speculate that private hospitals would lobby aggressively for greater public resources because they would benefit from the resulting contracts. There is evidence for this in South Africa, where government funders and private medical care suppliers were found to be linked in a manner that facilitated public–private contracts.9 This finding is also consistent with sociological evidence from other countries showing that elites in private health institutions may be able to use political networks to capture resources from the national health pool for their own region's benefit, fundamentally shaping the allocation of public health resources.30 The possible existence and functioning of such a mechanism deserves further study.
Others have proposed that the gaps in the provinces' health spending arise from the Treasury's bias toward richer provinces, based on income,7 but we have found that historical inequalities in public health capacity appear to be more important determinants of inequalities in health care allocations. A key finding from our analyses was that this situation has become self-perpetuating: the provinces with the most needs have fallen into an infrastructure–inequality trap in which the inequitable pre-1994 distribution of health infrastructure has had an enduring effect on both the distribution of health resources and continued changes in that distribution. In other words, inequalities in health care are not merely historical; they also appear to influence ongoing allocations. Our study further indicates that the backlog component in the National Treasury's Equitable Shares formula, designed to correct for inequalities in health capacity among provinces, is insufficient to counteract historical inequalities or to prevent them from worsening further as a result of the infrastructure–inequality trap.
Our findings have implications for public health research and policy. There is a need for much better information on health needs in South Africa; such research should build on earlier work to develop indices of deprivation and equity7 and should be informed by data on financial flows and the changing burden of illness at district levels that are more detailed than the data being gained from existing sentinel surveillance sites.31 There is also a clear need to develop an explicit goal not simply to modify but to reverse the current inequitable trends in allocations of health funds, so as to escape the infrastructure–inequality trap.
Acknowledgments
The authors would like to thank Lucy Gilson, Diane McIntyre, and Matthew McKeever for their comments on various drafts of this article.
Human Participant Protection
No protocol approval was needed because all data were obtained from publicly available secondary sources.
References
- 1a.Mandela N. In His Own Words. New York, NY: Little, Brown and Company; 2004 [Google Scholar]
- 1b.Price M. Explaining trends in the privatization of health services in South Africa. Health Policy Plan. 1989;4(2):121–130 [Google Scholar]
- 2.Bourne DE, Pick WM, Taylor SP, McIntyre DE, Klopper JM. A methodology for resource allocation in health care for South Africa. Part III. A South African health resource allocation formula. S Afr Med J. 1990;77(9):456–459 [PubMed] [Google Scholar]
- 3.Sanders D, Chopra M. Key challenges to achieving health for all in an inequitable society: the case of South Africa. Am J Public Health. 2006;96(1):73–78 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Coovadia H, Jewkes R, Barron P, Sanders D, McIntyre D. The health and health system of South Africa: historical roots of current public health challenges. Lancet. 2009;374(9692):817–834 [DOI] [PubMed] [Google Scholar]
- 5.Gilson L, Doherty J, McIntyre D, et al. The Dynamics of Policy Change: Health Care Financing in South Africa 1994–1999. Johannesburg, South Africa: Centre for Health Policy; 2000 [Google Scholar]
- 6.Thomas S, Muirhead D, Doherty J, Muheki C, Khosa S. South Africa Health Review 2000. Durban, South Africa: Health Systems Trust; 2000 [Google Scholar]
- 7.McIntyre D, Muirhead D, Gilson L. Geographic patterns of deprivation in South Africa: informing health equity analyses and public resource allocation strategies. Health Policy Plan. 2002;17(suppl):30–39 [DOI] [PubMed] [Google Scholar]
- 8.Jerome A. Privatisation and regulation in South Africa: an evaluation. Paper presented at: Third International Conference on Pro-Poor Regulation and Competition; September 7–9, 2004; Cape Town, South Africa [Google Scholar]
- 9.Shevel A. Competition body to probe “clubby” healthcare industry. Health Systems Trust Web site. Available at: http://www.hst.org.za/news/20020518. Published May 16, 2002. AccessedDecember23, 2008
- 10.Rice N, Smith PC. Capitation and risk adjustment in health care financing: an international progress report. Milbank Q. 2001;79(1):81–113 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hospital and Nursing Yearbook. Pretoria, South Africa: Pharmaceutical Publishers; 2007 [Google Scholar]
- 12.Hospital and Nursing Yearbook. Pretoria, South Africa: Pharmaceutical Publishers; 2008 [Google Scholar]
- 13.Hospital and Nursing Yearbook. Pretoria, South Africa: Pharmaceutical Publishers; 2009 [Google Scholar]
- 14.South Africa Council for Medical Schemes Annual Report 2004–5. Hatfield, South Africa: South Africa Council for Medical Schemes; 2005 [Google Scholar]
- 15.South Africa Council for Medical Schemes Annual Report 2006–7. Hatfield, South Africa: South Africa Council for Medical Schemes; 2007 [Google Scholar]
- 16.National Treasury, South Africa Ministry of Finance Explanatory Memorandum to the Division of Revenue. Pretoria, South Africa: National Treasury, South Africa Ministry of Finance; 2003 [Google Scholar]
- 17.National Treasury, South Africa Ministry of Finance Explanatory Memorandum to the Division of Revenue. Pretoria, South Africa: National Treasury, South Africa Ministry of Finance; 2005 [Google Scholar]
- 18.McIntyre D, Klugman B. The human face of decentralisation and integration of health services: experience from South Africa. Reprod Health Matters. 2003;11(21):108–119 [DOI] [PubMed] [Google Scholar]
- 19.De Renzio P. Scaling up versus absorptive capacity: challenges and opportunities for reaching the MDGS in Africa. Overseas Development Institute briefing paper. Available at: http://www.odi.org.uk/resources/download/1369.pdf. Published May 2005. Accessed October 5, 2010
- 20.Statistics South Africa Web site. Available at: http://www.statssa.gov.za. Accessed December 23, 2008.
- 21.Hart JT. The inverse care law. Lancet. 1971;1(7696):405–412 [DOI] [PubMed] [Google Scholar]
- 22.Gilson L, McIntyre D. Post-apartheid challenges: household access and use of health care in South Africa. Int J Health Serv. 2007;37(4):673–691 [DOI] [PubMed] [Google Scholar]
- 23.Tollman SM, Kahn K, Sartorius B, Collinson MA, Clark SJ, Garenne ML. Implications of mortality transition for primary health care in rural South Africa: a population-based surveillance study. Lancet. 2008;372(9642):893–901 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Udjo EO. Estimation of mortality from vital registrations in South Africa. Curr HIV Res. 2006;4(4):469–474 [DOI] [PubMed] [Google Scholar]
- 25.Setel PW, Macfarlane SB, Szreter S, et al. A scandal of invisibility: making everyone count by counting everyone. Lancet. 2007;370(9598):1569–1577 [DOI] [PubMed] [Google Scholar]
- 26.Gilson L, McIntyre D. The interface between research and policy: experience from South Africa. Soc Sci Med. 2008;67(5):748–759 [DOI] [PubMed] [Google Scholar]
- 27.Thomas S, Gilson L. Actor management in the development of health financing reform: health insurance in South Africa, 1994–1999. Health Policy Plan. 2004;19(5):279–291 [DOI] [PubMed] [Google Scholar]
- 28.Benatar SR. Health care reform and the crisis of HIV and AIDS in South Africa. N Engl J Med. 2004;351(1):81–92 [DOI] [PubMed] [Google Scholar]
- 29.Chopra M, Lawn JE, Sanders D, et al. ; Lancet South Africa Team Achieving the health Millenniumm Development Goals for South Africa: challenges and priorities. Lancet. 2009;374(9694):1023–1031 [DOI] [PubMed] [Google Scholar]
- 30.Whiteis DG. Unhealthy cities: corporate medicine, community economic underdevelopment, and public health. Int J Health Serv. 1997;27(2):227–242 [DOI] [PubMed] [Google Scholar]
- 31.Thorogood M, Connor M, Tollman S, Lewando Hundt G, Fowkes G, Marsh J. A cross-sectional study of vascular risk factors in a rural South African population: data from the Southern African Stroke Prevention Initiative (SASPI). BMC Public Health. 2007;7:326. [DOI] [PMC free article] [PubMed] [Google Scholar]