Abstract
Objectives. We examined demographic, clinical, and treatment outcome characteristics of Filipinos with tuberculosis (TB) in the United States.
Methods. We calculated TB case rates from US Census Bureau population estimates and National Tuberculosis Surveillance System data for US-born non-Hispanic Whites and for US residents born in the Philippines, India, China, Cambodia, Vietnam, Pakistan, and Korea––countries that are major contributors to the TB burden in the United States. We compared Filipinos with the other groups through univariate and multivariate analyses.
Results. Of 45 504 TB patients, 15.5% were Filipinos; 43.0% were other Asian/Pacific Islander groups; and 41.6% were Whites. Per 100 000 persons in 2007, the TB rate was 73.5 among Cambodians, 54.0 among Vietnamese, 52.1 among Filipinos, and 0.9 among Whites. Filipinos were more likely than other groups to be employed as health care workers and to have used private health care providers but less likely to be HIV positive and to be offered HIV testing.
Conclusions. The relatively high TB rate among Filipinos indicates that TB control strategies should target this population. Providers should be encouraged to offer HIV testing to all TB patients.
Tuberculosis (TB), an infectious disease caused by Mycobacterium tuberculosis, is transmitted through the air by droplet nuclei, most often infecting the lungs and resulting in pulmonary disease.1 The people of the Philippines have many risk factors for latent TB infection and TB disease, including poverty and lack of access to quality health care.2–5 In 2005, the Philippines ranked ninth among countries with high TB burdens, with an incidence rate of 291 per 100 000 persons and a prevalence of 450 per 100 000 persons.6 In recent years, implementation of effective public health practices in the Philippines has achieved high rates of treatment success and a decrease in unfavorable treatment outcomes. Nonetheless, in 2002 TB was the fourth leading cause of death in the Philippines,7and it continues to be a major cause of mortality.8
In 2007, the United States reported 13 299 new TB cases and a case rate of 4.4 per 100 000 persons.9 The TB case rate was more than 10 times as high among foreign-born as among US-born residents. Foreign-born persons accounted for 58.6% (n = 7799) of the total 13 299 TB cases in the United States in 2007. Countries of origin accounting for the majority of cases were Mexico (24%), the Philippines (12%), India (8%), Vietnam (7%), and China (5%). In 2007, 861 foreign-born TB patients reported the Philippines as their country of origin, second in number only to persons born in Mexico.10
We found no published national studies about TB among Filipinos in the United States. We performed an epidemiological analysis of US-residing Filipinos with TB disease reported to the National Tuberculosis Surveillance System (NTSS) of the Centers for Disease Control and Prevention (CDC) from 2000 to 2007. We compared TB case rates among US residents born in Asian/Pacific Islander (API) countries (the Philippines, India, China, Cambodia, Vietnam, Pakistan, and Korea) as well as rates for non-Hispanic Whites born in the United States. People born in these 7 API countries accounted for the majority of API TB cases in the United States.
To determine the extent to which country of birth is a risk factor for TB, we compared characteristics and treatment outcomes among Filipinos born in the Philippines but now residing in the US with those of TB patients born in 43 other API countries and non-Hispanic Whites born in the United States. We chose the 43 API countries of origin because data on characteristics and outcomes were available. We chose US-born non-Hispanic Whites as a comparison group because they have the lowest TB case rate in the United States. We hypothesized that we would find significant differences in factors underlying TB case rates among persons born in the Philippines and other API countries and non-Hispanic Whites born in the United States.
METHODS
We analyzed 45 504 reports of verified cases of TB submitted to the NTSS by the 50 states and the District of Columbia through a standardized data collection form.11 The NTSS monitors the frequency of occurrence and distribution of TB cases in the US population, information that guides policy decisions regarding TB control programs.
The study population consisted of US patients whose diagnosed TB was reported to NTSS between January 1, 2000, and December 31, 2007, and who were born in API countries or were US-born non-Hispanic Whites. We defined Filipino TB cases as occurring in TB patients in the study population who were born in the Philippines and API TB cases as occurring in TB patients who were born in the East Asian and Pacific region (except the Philippines) and the South and Central Asian region, as defined by the US Department of State.12,13 The East Asian and the Pacific region comprises 31 countries, and the South and Central Asian region, 13 countries. We defined US-born non-Hispanic White TB patients as those who were born in the United States or a US jurisdiction or were born in another country but had at least 1 US-born parent9 and self-identified as being of non-Hispanic ethnicity and White race.
Case Rates, HIV Status, and Culture-Positive Tuberculosis
We derived the TB case rates for patients born in 7 API countries (Philippines, India, China, Cambodia, Vietnam, Pakistan, and Korea) who accounted for the majority of the US TB burden from the national population estimates by country of birth determined by the US Census Bureau's American Community Surveys.14 We accessed survey data through the American Fact Finder and used Table PCT027, which shows place-of-birth data for the foreign-born population for 2002 to 2003, and Table B05006, which provides the same information for 2004 to 2007.
We calculated TB case rates for US-born non-Hispanic Whites for 2004 to 2007 from the American Fact Finder's Table B06004H, which shows place of birth by race (White, not Hispanic or Latino). For 2002 to 2003 TB case rates, American Community Survey population estimates for non-Hispanic Whites were not available. Therefore, we used the Federated Electronic Research, Review, Extract, and Tabulation Tool version 1.3.3 (US Census Bureau DataFerrett free software)15 to access the Census Bureau's population estimates from the Current Population Survey for non-Hispanic Whites born in the United States. Population estimates of other API countries were not available for 2000 to 2001, so we were unable to calculate TB case rates for these years. We also calculated TB rates among US health care workers in 2007 by using DataFerrett to access American Community Survey population estimates by occupation.
We also determined the drug-resistance patterns among culture-positive TB patients who were tested for susceptibility. Organisms belonging to a group of closely related mycobacteria that can cause TB disease, M. tuberculosis complex, were identified from an isolate grown in a media containing a patient's clinical specimen.11
All reporting sites (except in California since 2004 and Vermont since 2007) recorded HIV test results for TB cases (positive; negative; indeterminate; test not done, refused, or not offered; or unknown). We excluded California and Vermont from our analysis of HIV status.
Analyses
We compared the demographic, clinical, and treatment outcome characteristics of Filipino TB patients with those of TB patients from 43 other API countries and of US-born, non-Hispanic White TB patients by calculating unadjusted odds ratios (ORs) and 95% confidence intervals (CIs). In addition, we analyzed several variables from subsets of the total study population, such as unemployment in the past 24 months among patients aged 16 to 65 years, in accordance with current federal working-age restrictions.16 For all analyses, we used SAS version 9.1 (SAS Institute Inc, Cary, NC).
To determine the adjusted effects of TB risk factors for birth in the Philippines compared with birth in other API countries, we fitted a logistic regression model with variables that had significant unadjusted ORs. From this, we calculated adjusted odds ratios (AORs), with control for all other variables in the analysis. We determined the final model through manual backward elimination. We used Wald statistics to test for significance and included a variable in the final model if it was significantly associated with the outcome (P < .01). We investigated plausible pairwise interaction terms to test for effect modification.
For each of the significant variables (isoniazid and rifampin resistance, type of TB therapy, treatment outcome, provider type, and HIV status) that could not be fitted into the final model owing to specific population subset criteria, we used separate multivariate models. We calculated the ORs of these variables by adjusting them for age at diagnosis and gender.
RESULTS
Of 45 504 total TB patients in the study population, 15.5% (7038) were Filipinos, 43.0% (19 559) were from other API groups, and 41.6% (18 907) were US-born non-Hispanic Whites (Table 1). Of 18 152 female TB patients, 17.9% were Filipinos, 48.0% were from other API countries, and 34.0% were US-born non-Hispanic Whites.
TABLE 1.
Demographic, Clinical, and Risk Factor Characteristics of Tuberculosis (TB) Patients, by Birth Country and Ethnicity: United States, 2000–2007
| Foreign-Born Filipinos (n = 7 038), No. (%) | Other Foreign-Born APIs (n = 19 559), No. (%) | US-Born Non-Hispanic Whites (n = 18 907), No. (%) | |
| Age at diagnosis, y | |||
| > 44 | 4 306 (61.2) | 9 323 (47.7) | 14 042 (74.3) |
| ≤ 44 | 2 731 (38.8) | 10 233 (52.3) | 4 862 (25.7) |
| Age at entry into the United States, ya | |||
| > 44 | 2 379 (33.8) | 14 641 (74.9) | NA |
| ≤ 44 | 4 659 (66.2) | 4 918 (25.1) | NA |
| Residence in the United States, y | |||
| < 2 | 3 107 (44.1) | 8 099 (41.4) | NA |
| 2–5 | 648 (9.2) | 2 376 (12.1) | NA |
| > 5 | 3 283 (46.6) | 9 084 (46.4) | NA |
| Gender | |||
| Female | 3 250 (46.2) | 8 728 (45.6) | 6 174 (32.7) |
| Male | 3 787 (53.8) | 10 829 (55.4) | 12 729 (67.3) |
| Mortality at diagnosis | |||
| Deceased | 68 (1.0) | 244 (1.2) | 763 (4.0) |
| Living | 6 969 (99.0) | 19 305 (98.7) | 18 136 (95.9) |
| Type of TB disease | |||
| Extrapulmonary | 1 380 (19.6) | 5 441 (27.8) | 2 655 (14.0) |
| Extrapulmonary and pulmonary | 415 (5.9) | 1 511 (7.7) | 1 140 (6.0) |
| Pulmonary | 5 241 (74.5) | 12 601 (64.4) | 15 101 (79.9) |
| Chest radiograph result | |||
| Abnormal | 5 946 (84.5) | 15 521 (79.4) | 16 919 (89.5) |
| Normal | 964 (13.7) | 3 604 (18.4) | 1 468 (7.8) |
| Cavitation on chest radiographb | |||
| Cavitary | 1 214 (20.8) | 3 010 (19.9) | 4 811 (29.0) |
| Noncavitary, consistent with TB | 4 312 (73.7) | 11 090 (73.3) | 10 138 (61.2) |
| Noncavitary, not consistent with TB | 254 (4.3) | 795 (5.3) | 1 302 (7.9) |
| Drug resistancec | |||
| INH monoresistance | 718 (13.0) | 1 670 (10.7) | 511 (3.5) |
| RIF monoresistance | 10 (0.2) | 43 (0.3) | 52 (0.4) |
| INH and RIF resistance (multidrug resistance) | 92 (1.7) | 315 (2.0) | 59 (0.4) |
| Susceptible to INH and RIF | 4 700 (85.1) | 13 563 (87.0) | 13 826 (95.7) |
| Sputum smear test | |||
| Positive | 2 009 (28.6) | 6 066 (31.0) | 7 188 (38.0) |
| Not done | 1 196 (17.0) | 4 286 (21.9) | 4 354 (23.0) |
| Negative | 3 809 (54.1) | 9 133 (46.7) | 7 282 (38.5) |
| Therapyd | |||
| Any DOT | 4 848 (70.2) | 13 035 (68.2) | 13 876 (77.1) |
| Self-therapy style | 1 493 (21.6) | 4 292 (22.4) | 2 976 (16.6) |
| Completed therapyd | |||
| Yes | 3 947 (82.4) | 10 872 (81.8) | 10 436 (83.5) |
| No | 841 (17.6) | 2 423 (18.2) | 2 060 (16.5) |
| Outcomed | |||
| Died | 306 (4.4) | 888 (4.6) | 2 081 (11.6) |
| Lost to follow-up | 73 (1.1) | 351 (1.8) | 214 (1.2) |
| Moved | 270 (3.9) | 644 (3.4) | 161 (0.9) |
| Completed | 5 563 (80.5) | 14 961 (78.2) | 13 796 (76.7) |
| Provider typee | |||
| Private | 1 848 (26.5) | 4 559 (23.6) | 3 971 (21.9) |
| Public | 4 544 (65.3) | 12 923 (66.9) | 12 993 (71.6) |
| HIV statusf | |||
| Positive | 27 (0.8) | 191 (1.6) | 796 (4.8) |
| Refused | 295 (9.0) | 1 783 (15.2) | 1 783 (10.7) |
| Not offered | 751 (23.0) | 2 210 (18.9) | 3 665 (22.0) |
| Negative | 1 906 (58.4) | 6 585 (56.3) | 9 288 (55.7) |
| Homeless in past 12 mo | |||
| Yes | 48 (0.7) | 174 (0.9) | 1 864 (9.9) |
| No | 6 938 (98.6) | 19 121 (97.8) | 16 882 (89.3) |
| Resident of correctional facility | |||
| Yes | 18 (0.3) | 109 (0.6) | 606 (3.2) |
| No | 7 010 (99.6) | 19 427 (99.3) | 18 280 (96.7) |
| Resident of long-term health care facility | |||
| Yes | 82 (1.2) | 217 (1.1) | 1 116 (5.9) |
| No | 6 944 (98.7) | 19 314 (98.7) | 17 763 (93.9) |
| Occupation in past 24 mog | |||
| Health care worker | 647 (9.2) | 481 (2.5) | 460 (2.4) |
| Migrant worker | 14 (0.2) | 15 (0.1) | 14 (0.1) |
| Unemployed | 1 748 (24.8) | 5 780 (29.6) | 5 055 (26.7) |
| Other employment | 2 589 (36.8) | 8169 (41.8) | 5 485 (29.0) |
| Excessive alcohol use | |||
| Yes | 273 (3.9) | 571 (2.9) | 3 907 (20.7) |
| No | 6 531 (92.8) | 18 597 (95.1) | 14 450 (76.4) |
| Injection drug use | |||
| Yes | 8 (0.1) | 38 (0.2) | 573 (3.0) |
| No | 6 777 (96.3) | 19 148 (97.9) | 17 753 (93.9) |
| Noninjection drug use | |||
| Yes | 56 (0.8) | 141 (0.7) | 1 587 (8.4) |
| No | 6 708 (95.3) | 19 012 (97.2) | 16 686 (88.3) |
| Previous TB diagnosis | |||
| Yes | 473 (6.7) | 1 233 (6.3) | 1 010 (5.3) |
| No | 6 499 (92.3) | 18 133 (92.7) | 17 751 (93.9) |
Note. API = Asian/Pacific Islander; DOT = directly observed therapy; INH = isoniazid; NA = not applicable; RIF = rifampin.
Median age of entry into the United States was age 37 years for Filippinos, and age 31 years for other APIs.
Analysis limited to TB patients with abnormal X-ray results: Filipinos (n = 5 780); other APIs (n = 14 895); US-born non-Hispanic Whites (n = 16 251); patients with these data unknown or missing were not included.
Analysis limited to culture-positive TB patients with isolates that had susceptibility testing performed: Filipinos (n = 5 520); other APIs (n = 15 591); US-born non-Hispanic Whites (n = 14 448); patients with these data unknown or missing were not included.
Analysis limited to patients registered in the National Tuberculosis Surveillance System from 2000 to 2005 who were alive at diagnosis and started drug therapy: Filipinos (n = 6 341); other APIs (n = 17 327); US-born non-Hispanic Whites (n = 16 852); patients with these data unknown or missing were not included.
Analysis limited to patients who were alive at diagnosis: Filipinos (n = 6 392); other APIs (n = 17 482); US-born non-Hispanic Whites (n = 16 964); patients with these data unknown or missing were not included.
Analysis limited to patients registered in the National Tuberculosis Surveillance System from all states excluding California and Vermont: Filipinos (n = 2 979); other APIs (n = 10 769); US-born non-Hispanic Whites (n = 15 532); patients with these data unknown or missing were not included.
Patients aged younger than 16 years or older than 65 years included in analysis as a separate group, not eligible for employment (results not shown).
Tuberculosis Case Rates
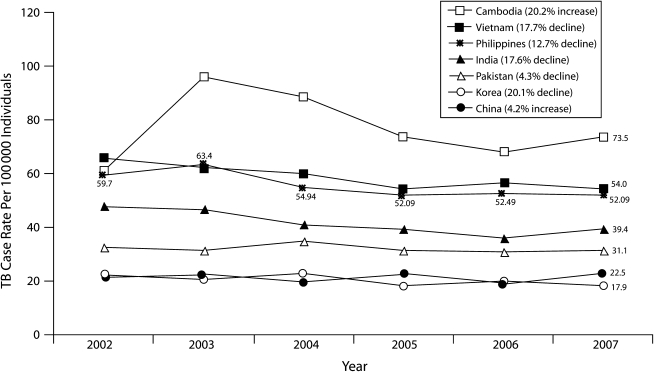
From 2002 to 2007, 85.7% of TB patients in the United States who were born in API countries were from the Philippines, India, China, Cambodia, Vietnam, Pakistan, or Korea (Figure 1). In 2007, the TB case rate in the United States for persons born in the Philippines was 52.1 per 100 000 persons; only Cambodians (73.5 per 100 000 persons) and Vietnamese (54.0 per 100 000 persons) had higher rates. During this period, the Filipino case rate declined by 12.7%. Declines were also recorded for Koreans (20.1% decline), Vietnamese (17.7% decline), Indians (17.6% decline), and Pakistanis (4.3% decline), but increases occurred among Chinese (4.2% increase) and Cambodians (20.2% increase; Figure 1). The case rate for US-born non-Hispanic Whites declined by 35.7%, from 1.4 per 100 000 persons in 2002 to 0.9 per 100 000 in 2007.
FIGURE 1.
Trends in tuberculosis (TB) cases rates among persons born in Asian/Pacific Islander countries and residing in the United States, by year: 2002–2007.
Note. Percent decline was calculated by dividing the difference of the 2002 and 2007 TB case rate by the 2002 TB case rate.
In 2007, the TB case rate among health care workers from the Philippines was 39.5 per 100 000 persons; from India, 34.8; from Vietnam, 9.6; and from China, 6.5. Among US natives, the rate was 0.6 per 100 000.
Comparisons of Filipino and Other Patients
Compared with US-born non-Hispanic White TB patients in our univariate analysis, Filipino TB patients were more likely to be female (OR = 1.8; 95% CI = 1.7, 1.9), to be employed as health care workers (OR = 3.0; 95% CI = 2.6, 3.4), to have had a previous diagnosis of TB (OR = 1.3; 95% CI = 1.1, 1.4), to have multidrug-resistant TB (OR = 4.6; 95% CI = 3.3, 6.5), and to have sought medical care from a private provider (OR = 1.3; 95% CI = 1.3, 1.4; Table 2). Filipino TB patients were less likely to be HIV positive (OR = 0.2; 95% CI = 0.1, 0.3), homeless (OR = 0.1; 95% CI = 0.1, 0.1), residents of a correctional or long-term care facility (OR = 0.1; 95% CI = 0.1, 0.1), excessive alcohol users (OR = 0.2; 95% CI = 0.1, 0.2), or injection drug users (OR = 0.1; 95% CI = 0.0, 0.1).
TABLE 2.
Comparison of Demographic, Clinical, and Risk Factor Characteristics of Tuberculosis (TB) Patients, by Birth Country and Ethnicity: United States, 2000–2007
| Foreign-Born Filipinos (n = 7 038), No. (%) | US-Born Non-Hispanic Whites (n = 18 907), No. (%) | OR (95% CI) | |
| Age at diagnosis, y | |||
| > 44 | 4306 (61.2) | 14 042 (74.3) | 0.55 (0.51, 0.58) |
| ≤ 44 (Ref) | 2731 (38.8) | 4 862 (25.7) | 1.00 |
| Gender | |||
| Female | 3250 (46.2) | 6 174 (32.7) | 1.77 (1.67, 1.87) |
| Male (Ref) | 3787 (53.8) | 12 729 (67.3) | 1.00 |
| Mortality at diagnosis | |||
| Deceased | 68 (1.0) | 763 (4.0) | 0.23 (0.18, 0.30) |
| Living (Ref) | 6969 (99.0) | 18 136 (95.9) | 1.00 |
| Type of TB disease | |||
| Extrapulmonary | 1380 (19.6) | 2 655 (14.0) | 1.50 (1.39, 1.61) |
| Extrapulmonary and pulmonary | 415 (5.9) | 1 140 (6.0) | 1.05 (0.93, 1.18) |
| Pulmonary (Ref) | 5241 (74.5) | 15 101 (79.9) | 1.00 |
| Chest radiograph result | |||
| Abnormal | 5946 (84.5) | 16 919 (89.5) | 0.54 (0.49, 0.58) |
| Normal (Ref) | 964 (13.7) | 1 468 (7.8) | 1.00 |
| Cavitation on chest radiographa | |||
| Cavitary | 1214 (20.8) | 4 811 (29.0) | 0.63 (0.59, 0.68) |
| Noncavitary, consistent with TB (Ref) | 4312 (73.7) | 10 138 (61.2) | 1.00b |
| Noncavitary, not consistent with TB (Ref) | 254 (4.3) | 1 302 (7.9) | 1.00b |
| Drug resistancec | |||
| INH monoresistance | 718 (13.0) | 511 (3.5) | 4.13 (3.67, 4.66) |
| RIF monoresistance | 10 (0.2) | 52 (0.4) | 0.57 (0.27, 1.15) |
| INH and RIF resistance (multidrug resistance) | 92 (1.7) | 59 (0.4) | 4.59 (3.26, 6.46) |
| Susceptible to INH and RIF (Ref) | 4700 (85.1) | 13 826 (95.7) | 1.00 |
| Sputum smear test | |||
| Positive | 2009 (28.6) | 7 188 (38.0) | 0.53 (0.50, 0.57) |
| Not done | 1196 (17.0) | 4 354 (23.0) | 0.65 (0.60, 0.70) |
| Negative (Ref) | 3809 (54.1) | 7 282 (38.5) | 1.00 |
| Therapyd | |||
| Any DOT | 4848 (70.2) | 13 876 (77.1) | 0.70 (0.65, 0.75) |
| Self-therapy style (Ref) | 1493 (21.6) | 2 976 (16.6) | 1.00 |
| Outcomed | |||
| Died | 306 (4.4) | 2 081 (11.6) | 0.36 (0.32, 0.41) |
| Lost | 73 (1.1) | 214 (1.2) | 0.85 (0.64, 1.11) |
| Moved | 270 (3.9) | 161 (0.9) | 4.16 (3.40, 5.09) |
| Completed (Ref) | 5563 (80.5) | 13 796 (76.7) | 1.00 |
| Provider typee | |||
| Private | 1848 (26.5) | 3 971 (21.9) | 1.33 (1.25, 1.42) |
| Public (Ref) | 4544 (65.3) | 12 993 (71.6) | 1.00 |
| HIV statusf | |||
| Positive | 27 (0.8) | 796 (4.8) | 0.17 (0.11, 0.25) |
| Refused | 295 (9.0) | 1 783 (10.7) | 0.81 (0.70, 0.92) |
| Not offered | 751 (23.0) | 3 665 (22.0) | 1.00 (0.91, 1.10) |
| Negative (Ref) | 1906 (58.4) | 9 288 (55.7) | 1.00 |
| Homeless in past 12 mo | |||
| Yes | 48 (0.7) | 1 864 (9.9) | 0.06 (0.05, 0.08) |
| No (Ref) | 6938 (98.6) | 16 882 (89.3) | 1.00 |
| Resident of correctional facility | |||
| Yes | 18 (0.3) | 606 (3.2) | 0.08 (0.05, 0.13) |
| No (Ref) | 7010 (99.6) | 18 280 (96.7) | 1.00 |
| Resident of long-term health care facility | |||
| Yes | 82 (1.2) | 1 116 (5.9) | 0.19 (0.15, 0.24) |
| No (Ref) | 6944 (98.7) | 17 763 (93.9) | 1.00 |
| Occupation in past 24 mog | |||
| Health care worker | 647 (9.2) | 460 (2.4) | 2.98 (2.62, 3.39) |
| Migrant worker | 14 (0.2) | 14 (0.1) | 2.12 (0.95, 4.71) |
| Unemployed | 1748 (24.8) | 5 055 (26.7) | 0.84 (0.81, 0.88) |
| Other employment (Ref) | 2589 (36.8) | 5 485 (29.0) | 1.00 |
| Excessive alcohol use | |||
| Yes | 273 (3.9) | 3 907 (20.7) | 0.15 (0.14, 0.18) |
| No (Ref) | 6531 (92.8) | 14 450 (76.4) | 1.00 |
| Injection drug use | |||
| Yes | 8 (0.1) | 573 (3.0) | 0.04 (0.02, 0.08) |
| No (Ref) | 6777 (96.3) | 17 753 (93.9) | 1.00 |
| Noninjection drug use | |||
| Yes | 56 (0.8) | 1 587 (8.4) | 0.09 (0.07, 0.12) |
| No (Ref) | 6708 (95.3) | 16 686 (88.3) | 1.00 |
| Previous TB diagnosis | |||
| Yes | 473 (6.7) | 1 010 (5.3) | 1.28 (1.14, 1.43) |
| No (Ref) | 6499 (92.3) | 1 7751 (93.9) | 1.00 |
Note. CI = confidence interval; DOT = directly observed therapy; INH = isoniazid; OR = odds ratio; RIF = rifampin. Unknown and missing data categories were included in analyses if they composed more than 3% of the total (results not shown).
Analysis limited to TB patients with abnormal X-ray results: Filipinos (n = 5 780); US-born non-Hispanic Whites (n = 16 251); patients with these data unknown or missing were not included.
We pooled noncavitary, consistent with TB and noncavitary, not consistent with TB to compose the referent group.
Analysis limited to culture-positive TB patients with isolates that had susceptibility testing performed: Filipinos (n = 5 520); US-born non-Hispanic Whites (n = 14 448); patients with these data unknown or missing data not included.
Analysis limited to patients registered in the National Tuberculosis Surveillance System from 2000 to 2005 who were alive at diagnosis and started drug therapy: Filipinos (n = 6 341); US-born non-Hispanic Whites (n = 16 852); patients with these data unknown or missing data not included.
Analysis limited to patients who were alive at diagnosis: Filipinos (n = 6 392); US-born non-Hispanic Whites (n = 16 964); patients with these data unknown or missing data not included.
Analysis limited to patients registered in the National Tuberculosis Surveillance System from all states excluding California and Vermont: Filipinos (n = 2 979); US-born non-Hispanic Whites (n = 15 532); patients with these data unknown or missing data not included.
Patients aged younger than 16 years or older than 65 years included in analysis as a separate group, not eligible for employment (results not shown).
Compared with other API TB patients in our multivariate analysis, Filipino TB patients were more likely to be employed as health care workers (OR = 4.6; 95% CI = 4.0, 5.2) or as migrant workers (OR = 3.3; 95% CI = 1.5, 7.0) and less likely to be unemployed (OR = 0.8; 95% CI = 0.7, 0.9) in the 12 months preceding their TB diagnosis.
Filipino TB patients were more likely to have less than 2 years of US residence before diagnosis (OR = 1.4; 95% CI = 1.3, 1.6; Table 3). We also found an association between Filipino TB patients and US residence of more than 5 years that varied by age of entry into the United States. This association was negative among persons who were aged older than 44 years when they entered the United States (OR = 0.8; 95% CI = 0.6, 1.0) but positive among immigrants who arrived when they were aged 44 years or younger (OR = 1.4; 95% CI = 1.2, 1.6). The median age of entry into the United States was 37 years for Filipino TB patients and 31 years for other API TB patients. Filipino patients were also more likely than other API TB patients to be female (OR = 1.2; 95% CI = 1.1, 1.2; Table 3).
TABLE 3.
Univariate and Multivariate Comparisons of Demographic, Clinical, and Risk Factor Characteristics of Tuberculosis (TB) Patients, by Birth Country and Ethnicity: United States, 2000–2007
| Foreign-Born Filipinos |
Other Foreign-Born APIs |
|||
| (n = 7 038), No. (%) | OR (95% CI) | (n = 19 559), No. (%) | AOR (95% CI) | |
| Age at diagnosis, y | ||||
| > 44 | 4306 (61.2) | 1.73 (1.64, 1.83) | 9 323 (47.7) | 1.62 (1.50, 1.76) |
| ≤ 44 (Ref) | 2731 (38.8) | 1.00 | 10 233 (52.3) | 1.00 |
| Age at entry into the United States, y | ||||
| > 44 | 2379 (33.8) | 0.17 (0.16, 0.18) | 14 641 (74.9) | NA |
| ≤ 44 (Ref) | 4659 (66.2) | 1.00 | 4 918 (25.1) | NA |
| Median | 37 | NA | 31 | NA |
| Residence in the United States, y | ||||
| < 2 | 3107 (44.1) | 1.41 (1.28, 1.55) | 8 099 (41.4) | NA |
| 2–5 (Ref) | 648 (9.2) | 1.00 | 2 376 (12.1) | NA |
| > 5 | 3283 (46.6) | 1.33 (1.20, 1.46) | 9 084 (46.4) | NA |
| Residence in the United States among persons aged > 44 y at arrival, y | ||||
| < 2 | 1163 (48.9) | 1.68 (1.40, 2.00) | 1 530 (31.1) | 1.58 (1.25, 2.00) |
| 2–5 (Ref) | 230 (9.7) | 1.00 | 507 (10.3) | 1.00 |
| > 5 | 986 (41.4) | 0.75 (0.63, 0.90) | 2 881 (58.6) | 0.78 (0.61, 0.98) |
| Residence in the United States among persons aged ≤ 44 y at arrival, y | ||||
| < 2 | 1944 (41.7) | 1.32 (1.17, 1.49) | 6 569 (44.9) | 1.25 (1.10, 1.42) |
| 2–5 (Ref) | 418 (9.0) | 1.00 | 1 869 (12.8) | 1.00 |
| > 5 | 2297 (49.3) | 1.66 (1.47, 1.86) | 6 203 (42.4) | 1.38 (1.21, 1.57) |
| Gender | ||||
| Female | 3250 (46.2) | 1.23 (1.16, 1.30) | 8 728 (45.6) | 1.17 (1.10, 1.24) |
| Male (Ref) | 3787 (53.8) | 1.00 | 10 829 (55.4) | 1.00 |
| Type of TB disease | ||||
| Extrapulmonary | 1380 (19.6) | 0.61 (0.57, 0.65) | 5441 (27.8) | 0.57 (0.52, 0.62) |
| Extrapulmonary and pulmonary | 415 (5.9) | 0.66 (0.59, 0.74) | 1 511 (7.7) | 0.65 (0.58, 0.73) |
| Pulmonary (Ref) | 5241 (74.5) | 1.00 | 12 601 (64.4) | 1.00 |
| Chest radiograph result | ||||
| Abnormala | 5946 (84.5) | 1.43 (1.32, 1.55) | 15 521 (79.4) | NS |
| Normal (Ref) | 964 (13.7) | 1.00 | 3 604 (18.4) | 1.00 |
| Sputum smear test | ||||
| Positive | 2009 (28.6) | 0.79 (0.75, 0.85) | 6 066 (31.0) | 0.72 (0.67, 0.77) |
| Not done | 1196 (17.0) | 0.67 (0.62, 0.72) | 4 286 (21.9) | 0.86 (0.79, 0.94) |
| Negative (Ref) | 3809 (54.1) | 1.00 | 9 133 (46.7) | 1.00 |
| Resident of correctional facility | ||||
| Yes | 18 (0.3) | 0.46 (0.27, 0.77) | 109 (0.6) | 0.53 (0.31, 0.90) |
| No (Ref) | 7010 (99.6) | 1.00 | 19 427 (99.3) | 1.00 |
| Excessive alcohol use | ||||
| Yes | 273 (3.9) | 1.36 (1.17, 1.58) | 571 (2.9) | 1.36 (1.16, 1.60) |
| No (Ref) | 6531 (92.8) | 1.00 | 18 597 (95.1) | 1.00 |
| Drug resistancebc | ||||
| INH monoresistance | 718 (13.0) | 1.24 (1.13, 1.36) | 1670 (10.7) | 1.29 (1.17, 1.42) |
| RIF monoresistance | 10 (0.2) | 0.67 (0.32, 1.39) | 43 (0.3) | 0.68 (0.33, 1.40) |
| INH and RIF resistance (multidrug resistance) | 92 (1.7) | 0.84 (0.66, 1.07) | 315 (2.0) | 0.90 (0.70, 1.14) |
| Susceptible to INH and RIF (Ref) | 4700 (85.1) | 1.00 | 13 563 (87.0) | 1.00 |
| Therapycd | ||||
| Any DOT | 4848 (70.2) | 1.07 (1.00, 1.14) | 13 035 (68.2) | 1.05 (0.98, 1.14) |
| Self-therapy (Ref) | 1493 (21.6) | 1.00 | 4 292 (22.4) | 1.00 |
| Outcomecd | ||||
| Died | 306 (4.4) | 0.93 (0.81, 1.06) | 888 (4.6) | 0.80 (0.69, 0.94) |
| Lost | 73 (1.1) | 0.56 (0.43, 0.78) | 351 (1.8) | 0.65 (0.49, 0.86) |
| Moved | 270 (3.9) | 1.13 (0.97, 1.31) | 644 (3.4) | 1.16 (0.97, 1.36) |
| Completed (Ref) | 5563 (80.5) | 1.00 | 14 961 (78.2) | 1.00 |
| Provider typece | ||||
| Private | 1848 (26.5) | 1.15 (1.08, 1.23) | 4 559 (23.6) | 1.12 (1.04, 1.20) |
| Public (Ref) | 4544 (65.3) | 1.00 | 12 923 (66.9) | 1.00 |
| HIV statuscf | ||||
| Positive | 27 (0.8) | 0.49 (0.32, 0.74) | 191 (1.6) | 0.64 (0.42, 0.96) |
| Refused | 295 (9.0) | 0.57 (0.50, 0.65) | 1 783 (15.2) | 0.60 (0.52, 0.69) |
| Not offered | 751 (23.0) | 1.17 (1.06, 1.30) | 2 210 (18.9) | 1.23 (1.11, 1.36) |
| Negative (Ref) | 1906 (58.4) | 1.00 | 6 585 (56.3) | 1.00 |
| Occupation in past 24 mog | ||||
| Health care worker | 647 (9.2) | 4.24 (3.73, 4.82) | 481 (2.5) | 4.57 (4.00, 5.21) |
| Migrant worker | 14 (0.2) | 2.94 (1.34, 6.45) | 15 (0.1) | 3.27 (1.52, 7.02) |
| Unemployed | 1748 (24.8) | 0.95 (0.89, 1.02) | 5 780 (29.6) | 0.79 (0.73, 0.85) |
| Other employment (Ref) | 2589 (36.8) | 1.00 | 8 169 (41.8) | 1.00 |
Note. AOR = adjusted odds ratio; API = Asian/Pacific Islander; CI = confidence interval; DOT = directly observed therapy; INH = isoniazid; NA = not applicable; NS = not significant; OR = odds ratio; RIF = rifampin. Unknown and missing data categories were included in analyses if they composed more than 3% of the total (results not shown).
Having an abnormal X-ray result was not significant in main effects and was therefore eliminated from subsequent models.
Analysis limited to culture-positive TB patients with isolates that had susceptibility testing performed: Filipinos (n = 5 520); other APIs (n = 15 591); patients with these data unknown or missing were not included.
Odds ratios adjusted for age of diagnosis and gender.
Analysis limited to patients registered in the National Tuberculosis Surveillance System from 2000 to 2005 who were alive at diagnosis and started drug therapy: Filipinos (n = 6 341); other APIs (n = 17 327); patients with these data unknown or missing data not included.
Analysis limited to patients who were alive at diagnosis: Filipinos (n = 6 392); other APIs (n = 17 482); patients with these data unknown or missing data not included.
Analysis limited to patients registered in the National Tuberculosis Surveillance System from all states excluding California and Vermont: Filipinos (n = 2 979); other APIs (n = 10 769); patients with these data unknown or missing data not included.
Patients aged younger than 16 years or older than 65 years included in analysis as a separate group, not eligible for employment (results not shown).
Among culture-positive TB patients, being Filipino was significantly associated with having an M. tuberculosis isolate that was isoniazid resistant (OR = 1.3; 95% CI = 1.2, 1.4) but not associated with resistance to rifampin or to both isoniazid and rifampin (multidrug-resistant TB). In the subset of the study population who were alive at diagnosis and started drug therapy between 2000 and 2005, Filipino TB patients were less likely to be lost to follow-up during treatment (OR = 0.7; 95% CI = 0.5, 0.9) or to die during treatment (OR = 0.8; 95% CI = 0.7, 0.9; Table 3).
Filipino TB patients were more likely to report that they were not offered HIV testing (OR = 1.2; 95% CI = 1.1, 1.4), and were less likely to test positive for HIV (OR = 0.6; 95% CI = 0.4, 1.0) and to refuse HIV testing (OR = 0.6; 95% CI = 0.5, 0.7; Table 3). Patients diagnosed with TB while residing in a correctional facility were less likely to be Filipinos (OR = 0.5; 95% CI = 0.3, 0.9). The only behavioral risk factor for which we observed a significant association among Filipino patients was excess alcohol use (OR = 1.4; 95% CI = 1.2, 1.6; Table 3).
DISCUSSION
Ours is the first study to examine current trends in TB rates and to compare characteristics of TB patients born in the Philippines and living in the United States with those born in other API countries. Ours is also the first study to compare Philippines-born TB patients with US-born non-Hispanic White TB patients.
Tuberculosis Case Rates and Age
In 2007, the Filipino TB case rate in the United States was 57.9 times as high as the rate for US-born non-Hispanic Whites and 11.8 times as high as the national US case rate of 4.4 per 100 000 population.9 Persons born in the Philippines had the third-highest TB case rate among API immigrants in 2007, surpassed only by Cambodians and Vietnamese. From 2002 to 2007, however, the TB case rate declined faster among Filipinos than among persons born in Pakistan, China, and Cambodia. The decline of Filipino TB case rates from 2002 to 2007 parallels the decline of TB case rates in the Philippines, which has been attributed to that country's TB prevention, control, and treatment campaigns.6 In the future, US TB rates in this population may fall further as a consequence of the enhanced TB screening and treatment program for Filipino applicants for US permanent residency implemented in 2007.17
The 1997 Nationwide TB Prevalence Survey in the Philippines revealed a positive correlation between age and the prevalence of abnormal chest radiographs suggestive of pulmonary TB.18 In our study, Filipino TB patients were significantly older than were other API patients when diagnosed with TB, possibly because they were older when they arrived in the United States. Our comparison of median ages showed that Filipino TB patients had 6 additional years of exposure in their home country, which has a high TB burden. Also, Filipinos were more likely to have resided in the United States for less than 2 years before diagnosis. These data suggest that Filipinos have a high infection rate when they arrive in the United States.
Risk Factors
The greater association of excessive alcohol use with TB among Filipinos than among other API groups in our study is consistent with a report of alcohol abuse among Filipinos in the United States.19 However, US-born non-Hispanic Whites had the highest proportion of excess alcohol use in our study.
In our sample, Filipinos were significantly less likely than were any other group to be HIV positive. HIV is currently not a major public health problem in the Philippines. In 2007, the Philippines had an HIV prevalence rate of less than 0.1 per 100 000 persons, or an estimated 8300 persons living with HIV.20 The proportion of patients with HIV among Filipino TB patients in the United States was less than 1% in our study. In addition, Filipino TB patients were more likely than were other API TB patients to report not being offered HIV testing and were less likely to refuse testing.
Filipino patients in our sample were more likely than other API TB patients to have isoniazid-monoresistant TB, but we found no significant association with resistance to rifampin alone or to both isoniazid and rifampin (multidrug-resistant TB). Our finding of a higher proportion of multidrug-resistant TB among Filipinos than among Whites suggests that clinicians need to be vigilant in monitoring drug resistance among this population. Because Filipinos are more likely to seek care from private providers, strategies to inform these providers about this issue should be developed.
Tuberculosis Among Health Care Workers
Our study documents for the first time that Filipino TB patients living in the United States are more likely than are other API immigrants and US-born non-Hispanic Whites to be employed as health care workers. This reflects the high percentage of health care workers from the Philippines in the US health care system; in 2004, more than half of foreign-educated registered nurses were from the Philippines.21 A study in New York state found that 12% of foreign-born TB patients employed as health care workers were from the Philippines.22 Moreover, in our study, the TB case rate among health care workers from the Philippines surpassed that of health care workers from India, Vietnam, China, and the United States in 2007.
NTSS data do not distinguish between TB that occurs as a consequence of nosocomial transmission and disease that arises from reactivation of untreated latent TB infection acquired in the country of origin. Such reactivation of latent infection has been reported, however, among health care workers.22 In 2003, a health care worker from the Philippines was diagnosed with pulmonary TB.23 When hired 11 years earlier, the worker had a positive tuberculin skin test result but no other test indicating TB infection or disease. Citing a history of Bacillus Calmette-Guerin vaccination, the worker had declined treatment for latent TB infection. This is an example of the limited efficacy of Bacillus Calmette-Guerin vaccination, which is not routinely recommended in the United States.24,25
Overall, these findings highlight the public health problem of TB among foreign-born health care workers, particularly among those born in countries with a high TB burden, such as the Philippines. CDC recommendations for TB screening and treatment should be followed vigilantly for this population, especially in employment settings with a high risk for TB exposure.26,27
Tuberculosis Screening of Permanent Residency Applicants
In our study, Filipino TB patients (including health care workers and students who did not undergo medical screening before departing the Philippines) were more likely than were other API TB patients to have resided in the United States for less than 2 years before diagnosis. This finding could in some cases reflect unrecognized TB at the time of screening in the Philippines. It also highlights the importance of an effective TB screening process for US visa applicants.
Prior to 2007, permanent residency visa applicants aged 15 years or older were screened for TB with a chest radiograph and sputum smear examinations.28 Applicants were classified according to the presence and infectiousness of TB. With the exception of those with active infectious TB, applicants could immigrate to the United States without completion of TB treatment but were instructed to report to the local health department for further medical evaluation within 30 days of arrival.
Although this TB screening process detected active TB cases, studies have cited gaps in the process.29,30 A major deficiency was reliance on a sputum smear test for diagnosis of TB disease. The nationwide Philippine survey observed a low prevalence of smear-positive TB, which was attributed to a low bacillary load.17 TB with low bacillary load may be undetectable by the acid-fast bacilli test. This flaw in TB screening may have contributed to unrecognized TB disease among recent Filipino immigrants, but it has been addressed by the addition of culture to the laboratory screening tests starting in 2007.17
Limitations and Conclusions
NTSS data do not include migration information, such as TB classification at time of immigration, time between migration medical examinations and departure to the United States, and complete socioeconomic data in the Philippines and the United States. Further study on how these factors influence the development of TB disease could elucidate the epidemiology of immigrants with the disease, particularly among people from countries with a high burden of disease, such as Filipinos.
Our results on low HIV prevalence among Filipino TB patients should be interpreted with caution because California data on HIV status were limited to the classifications positive and unknown. Nevertheless, all health care providers (private or public) should be informed about the importance of offering HIV testing to all TB patients.
Despite a declining trend in case rates, TB among Filipinos living in the United States is an important public health issue. Although improvements in TB screening for visa applications can better detect TB or prevent importation of the disease from the Philippines, additional public health efforts are needed.
The Filipino community has a relatively high socioeconomic status in comparison with non-Hispanic Whites and the Asian community in general.31 This community has a high percentage of professionals, a low poverty rate (5.2 per 100 000 persons versus 8.8 per 100 000 for non-Hispanic Whites), and a high median income ($65 700 versus $48 784 for non-Hispanic Whites). However, a study of the attitudes and beliefs regarding TB among Filipinos indicated poor knowledge of TB disease and fear of social stigma.3 Therefore, culturally appropriate public health efforts such as education and case management are important in addressing TB among Filipinos. Additional international efforts to decrease the endemic TB problem in the Philippines would contribute to the prevention of imported Filipino TB cases. Comparing the TB case rate among health care workers in the Philippines with the rates among workers in the United States and other countries is also important for future research.
Our findings indicate that the TB case rate in the United States for 2007 among persons born in the Philippines was among the highest of immigrants from API countries. Compared with other API TB patients and non-Hispanic White TB patients, Filipino TB patients were more likely to be female, to be employed as health care workers, to use private health care providers, and to have lived in the United States for less than 2 years. Filipinos were significantly older at time of TB diagnosis and on first arriving in the United States than were TB patients from other API countries. Innovative TB control strategies tailored to the needs of this immigrant population should be developed.
Acknowledgments
We thank the staff of the state and local health departments throughout the United States who collected and reported the data used in this article. We also thank Tom Navin, MD, for his valuable insights and Ann Lanner, BS, for her helpful editorial comments.
Human Participant Protection
Protocol approval was not required because data were obtained from secondary sources.
References
- 1.Questions and answers about TB Atlanta, GA: Centers for Disease Control and Prevention; 2009. Available at: http://www.cdc.gov/tb/publications/faqs/default.htm. Accessed February 1, 2010 [Google Scholar]
- 2.Bates I, Fenton C, Gruber J, et al. Vulnerability to malaria, tuberculosis, and HIV/AIDS infection and disease. Part 1: determinants operating at individual and household level. Lancet Infect Dis. 2004;4(5):267–277 [DOI] [PubMed] [Google Scholar]
- 3.Yamada S, Caballero J, Matsunaga DS, Agustin G, Magana M. Attitudes regarding tuberculosis in immigrants from the Philippines to the United States. Fam Med. 1999;31(7):477–482 [PubMed] [Google Scholar]
- 4.Wallerstein C. Tuberculosis ravages Philippine slums. BMJ. 1999;319(7207):402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Tupasi TE, Radhakrishna S, Quelapio MI, et al. Tuberculosis in the urban poor settlements in the Philippines. Int J Tuberc Lung Dis. 2000;4(1):4–11 [PubMed] [Google Scholar]
- 6.Global tuberculosis control: surveillance, planning, financing. Geneva, Switzerland: World Health Organization; 2007:73–160 Available at: http://www.who.int/tb/publications/global_report/2007/pdf/full.pdf. Accessed February 1, 2010 [Google Scholar]
- 7.Top 10 causes of death, all ages—Philippines. Geneva, Switzerland: World Health Organization; 2002. Available at: http://www.who.int/entity/healthinfo/statistics/bodgbddeathdalyestimates.xls. Accessed February 1, 2010 [Google Scholar]
- 8.World Health Statistics 2009: Cause-specific mortality and morbidity-Philippines. Geneva, Switzerland: World Health Organization; 2009. Available at: http://www.who.int/whosis/whostat/EN_WHS09_Table2.pdf. Accessed February 1, 2010 [Google Scholar]
- 9.Centers for Disease Control and Prevention Trends in tuberculosis—United States, 2007. MMWR Morb Mortal Wkly Rep. 2008;57(11):281–285 Available at: http://www.cdc.gov/mmwr/preview/mmwrhtml/mm5711a2.htm. Accessed February 1, 2010 [PubMed] [Google Scholar]
- 10.Reported tuberculosis in the United States, 2007. Atlanta, GA: Centers for Disease Control and Prevention; 2008. Available at: http://www.cdc.gov/tb/statistics/reports/2007/default.htm. Accessed February 1, 2010 [Google Scholar]
- 11.Division of Tuberculosis Elimination, National Center for HIV/STD/TB Prevention Tuberculosis information management system user's guide, version 1.2. Atlanta, GA: Centers for Disease Control and Prevention; 2003. Available at: ftp://ftp.cdc.gov/pub/Software/TIMS/Documentation. Accessed February 1, 2010 [Google Scholar]
- 12.US Department of State List of South and Central Asian countries. Available at: http://www.state.gov/p/sca/ci. Accessed November 1, 2009
- 13.US Department of State List of East Asian and Pacific countries. Available at: http://www.state.gov/p/eap/ci. Accessed November 1, 2009
- 14.US Census Bureau American Community Survey, 2000–2007. Available at: http://www.census.gov/acs. Accessed November 1, 2009
- 15.US Census Bureau Current Population Survey, March supplements (2002–2003). DataFerrett. Available at: http://www.thedataweb.org/faq.html. Accessed February 1, 2010
- 16.Child Labor Coalition Fair Labor Standards Act: an overview of federal child labor laws. 2008. Available at: http://www.stopchildlabor.org/USchildlabor/fact1.htm. Accessed February 1, 2010
- 17.Technical instructions for tuberculosis screening and treatment for panel physicians. Atlanta, GA: Centers for Disease Control and Prevention; 2007. Available at: www.cdc.gov/ncidod/dq/panel_2007.htm. Accessed February 1, 2010 [Google Scholar]
- 18.Tupasi TE, Radhakrishna S, Rivera AB, et al. The 1997 nationwide tuberculosis prevalence survey in the Philippines. Int J Tuberc Lung Dis. 1999;3(6):471–477 [PubMed] [Google Scholar]
- 19.Caetano R, Clark CL, Tam T. Alcohol consumption among racial/ethnic minorities: theory and research. Alcohol Health Res World. 1998;22(4):233–241 [PMC free article] [PubMed] [Google Scholar]
- 20.2008 report on the global AIDS epidemic—annex I: country profiles. Geneva, Switzerland: UNAIDS; 2008:222 Available at: http://data.unaids.org/pub/GlobalReport/2006/2006_GR_ANN1M-Z_en.pdf. Accessed November 1, 2009 [Google Scholar]
- 21.The registered nurse population: findings from the 2004 national sample survey of registered nurses. Washington, DC: US Department of Health and Human Services; 2006. Available at: ftp://ftp.hrsa.gov/bhpr/workforce/0306rnss.pdf. Accessed November 1, 2009 [Google Scholar]
- 22.Driver CR, Stricof RL, Granville K, et al. Tuberculosis in health care workers during declining tuberculosis incidence in New York State. Am J Infect Control. 2005;33(9):519–526 [DOI] [PubMed] [Google Scholar]
- 23.Centers for Disease Control and Prevention Mycobacterium tuberculosis transmission in a newborn nursery and maternity ward—New York City, 2003. MMWR Morb Mortal Wkly Rep. 2005;54(50):1280–1283Available at: http://www.cdc.gov/mmwr/preview/mmwrhtml/mm5450a2.htm. Accessed November 1, 2009 [PubMed] [Google Scholar]
- 24.The role of BCG vaccine in the prevention and control of tuberculosis in the United States: a joint statement by the Advisory Council for the Elimination of Tuberculosis and the Advisory Committee on Immunization Practices. MMWR Recomm Rep. 1996;45(RR4):1–18 Available at: http://www.cdc.gov/mmwr/preview/mmwrhtml/00041047.htm. Accessed February 1, 2010 [PubMed] [Google Scholar]
- 25.Centers for Disease Control and Prevention Immunization of health-care workers: recommendations of the Advisory Committee on Immunization Practices (ACIP) and the Hospital Infection Control Practices Advisory Committee (HICPAC). MMWR Morb Mortal Wkly Rep. 1997;46(RR18):1–42 Available at: ftp://ftp.cdc.gov/pub/Publications/mmwr/rr/rr4618.pdf. Accessed February 1, 20109011775 [Google Scholar]
- 26.Centers for Disease Control and Prevention Targeted tuberculin testing and treatment of latent tuberculosis infection. MMWR Recomm Rep. 2000;46(RR-6):1–54 Available at: http://www.cdc.gov/mmwr/preview/mmwrhtml/rr4906a1.htm. Accessed February 1, 2010 [PubMed] [Google Scholar]
- 27.Centers for Disease Control and Prevention Guidelines for preventing the transmission of Mycobacterium tuberculosis in health-care settings, 2005. MMWR Recomm Rep. 2005;54(RR-17):1–141 Available at: http://www.cdc.gov/mmwr/preview/mmwrhtml/rr5417a1.htm. Accessed February 1, 2010 [PubMed] [Google Scholar]
- 28.Technical instructions for tuberculosis screening and treatment for panel physicians. Atlanta, GA: Centers for Disease Control and Prevention; 1991. Available at: http://www.cdc.gov/ncidod/dq/panel_1991.htm. Accessed February 1, 2010 [Google Scholar]
- 29.Maloney SA, Fielding KL, Laserson KF, et al. Assessing the performance of overseas tuberculosis screening programs: a study among US-bound immigrants in Vietnam. Arch Intern Med. 2006;166(2):234–240 [DOI] [PubMed] [Google Scholar]
- 30.DeRiemer K, Chin DP, Schecter GF, Reingold AL. Tuberculosis among immigrants and refugees. Arch Intern Med. 1998;158(7):753–760 [DOI] [PubMed] [Google Scholar]
- 31.US Census Bureau The American community—Asians: 2004. 2007. Available at: http://www.census.gov/prod/2007pubs/acs-05.pdf. Accessed November 1, 2009