Abstract
Objectives. We examined whether periodontal treatment or other dental care is associated with adverse birth outcomes within a medical and dental insurance database.
Methods. In a retrospective cohort study, we examined the records of 23 441 women enrolled in a national insurance plan who delivered live births from singleton pregnancies in the United States between January 1, 2003, and September 30, 2006, for adverse birth outcomes on the basis of dental treatment received. We compared rates of low birthweight and preterm birth among 5 groups, specifying the relative timing and type of dental treatment received. We used logistic regression analysis to compare outcome rates across treatment groups while adjusting for duration of continuous dental coverage, maternal age, pregnancy complications, neighborhood-level income, and race/ethnicity.
Results. Analyses showed that women who received preventive dental care had better birth outcomes than did those who received no treatment (P < .001). We observed no evidence of increased odds of adverse birth outcomes from dental or periodontal treatment.
Conclusions. For women with medical and dental insurance, preventive care is associated with a lower incidence of adverse birth outcomes.
Preterm birth and low birthweight in the United States lead to significant infant morbidity and mortality. A preterm, or premature, birth has a gestational age of less than 37 weeks at delivery. Low birthweight is defined as birthweight less than 2500 grams. Approximately 12.5% of women in the United States deliver their babies prematurely, and those who deliver before reaching a gestation period of 32 weeks comprise 1% to 2% of all births.1 During the neonatal period, low birthweight babies are less likely to survive compared to normal birthweight babies, and those who do survive are at an increased risk of developing respiratory, behavioral, and neurodevelopmental problems.2 The Institute of Medicine of the National Academies estimates that premature births cost society at least $26 billion annually in the US.3
Several studies have examined the effect of periodontal treatment on preterm birth and low birthweight outcomes.4 In 2 randomized controlled trials, Lopez et al. determined that periodontal therapy provided during pregnancy to women with periodontitis or gingivitis reduced the incidence of preterm low birthweight.5,6 A study conducted in India reported that pregnant women who received plaque control instructions and scaling and root planing experienced significantly reduced rates of preterm births and low birthweight infants.7 In addition, case control, cross-sectional, and longitudinal studies relating periodontal disease and preterm low birthweight have shown that there is an association between the 2 conditions.4,8–10 A 2007 meta-analysis confirmed an association between periodontal disease and preterm low birthweight but cautioned that additional studies must be conducted in order to more accurately identify the mechanisms for the association.8
Conversely, several studies have failed to detect an association between periodontal disease and adverse birth outcomes.11–17 Jeffcoat et al. reported a reduced, albeit not statistically significant, risk of premature birth in women with periodontal disease who received scaling and root planing or dental prophylaxis treatment.11 Mitchell-Lewis et al. reported a nonsignificant reduction in preterm low birthweight outcomes in women who received basic periodontal therapy during pregnancy.12 Michalowicz et al. conducted a multicenter trial of 823 women randomized to receive scaling and root planing either before 21 weeks of gestation or after delivery.16 Periodontitis treatment during pregnancy did not significantly affect rates of preterm birth or low birthweight. Offenbacher et al. conducted a multicenter randomized trial of 1806 women randomized to receive scaling and root planing early in the second trimester or after delivery.17 In their study, periodontal treatment did not reduce the incidence of preterm delivery.
A retrospective examination of health insurance data for women with concomitant medical and dental coverage can contribute to the study of the association between oral conditions and outcomes; however, comprehensive examinations of dental insurance data have rarely included combined medical and dental databases.18 Certain specific features of health insurance claims data, such as representativeness and generalizability, make the data an important source of information for health services research.19 Insurance claims data provide information on dental treatment, medical treatment procedures, and medical diagnoses and have been reported to be more closely associated with actual medical record documentation than has self-reported health information garnered from patient surveys.20–22
We examined dental and medical claims data from the Aetna Data Warehouse to determine the association between periodontal treatment, dental prophylaxis, and other dental treatment and 2 adverse birth outcomes: preterm birth and low birthweight. We hypothesized that (1) women receiving preventive care (prophylaxis treatment) during the period of observation would experience improved birth outcomes compared with those receiving no dental treatment and (2) periodontal treatment provided before delivery would be associated with a lower incidence of adverse pregnancy outcomes.
METHODS
We used a retrospective cohort study design on the medical and dental claims database of a large national health insurer. We examined claims of fully insured women participating in medical and dental insurance plans who delivered live births from singleton pregnancies between January 1, 2003, and September 30, 2006. The only demographic information available in the database provided was maternal age. Therefore, we generated proxy demographic information to use in the analyses by matching the enrollee zip code of primary residence listed in the database to 2000 US Census data to obtain neighborhood characteristics on income and race/ethnicity.
The outcome variables for this study were preterm delivery and low birthweight delivery. We determined these outcomes by the use of the World Health Organization's International Classification of Diseases, Ninth Revision (ICD-9)23 codes, available through claims records. (Low birthweight and preterm delivery classification and associated ICD-9 codes are available in Supplemental Table 1, available as a supplement to the online version of this article at http://www.ajph.org).
TABLE 1.
Study Distributions of Key Analytic Variables in an Insured US Population: January 1, 2003–September 30, 2006
| Variable | No. (%) |
| Birth outcomes | |
| Low birth weight (< 2500 g) | 994 (4.2) |
| Preterm delivery (< 37 wk) | 2125 (9.1) |
| Periodontal and other dental treatment groups | |
| Received periodontal treatment before delivery | 464 (2.0) |
| Received periodontal treatment after delivery | 622 (2.6) |
| Received prophylactic treatment at least once during follow-up | 8010 (34.2) |
| Received other dental treatment at least once during follow-up | 2024 (8.6) |
| No dental treatment of any kind during the period of observation | 12 321 (52.6) |
| Complications of pregnancy | 6552 (28.0) |
| Distribution of African American population within enrollee zip code, % | |
| 0 | 1111 (4.7) |
| 1–10 | 14 192 (60.5) |
| 11–35 | 4659 (19.9) |
| 36–50 | 649 (2.8) |
| 51–100 | 1779 (7.6) |
| Missing | 1051 (4.5) |
| Distribution of income within enrollee zip code | |
| Between 1st and 20th percentile nationally | 1179 (5.0) |
| Between 20th and 40th percentile nationally | 1457 (6.3) |
| Between 40th and 60th percentile nationally | 2399 (10.3) |
| Between 60th and 80th percentile nationally | 4376 (18.7) |
| Between 80th percentile and maximum nationally | 13 217 (56.4) |
| Missing | 813 (3.5) |
| Enrollment span for dental coveragea | |
| Enrolled ≥ 36 mo | 6602 (28.2) |
| Enrolled ≥ 30 mo | 9127 (38.9) |
| Enrolled ≥ 24 mo | 12 462 (53.2) |
Note. The sample size was n = 23 441. Table gives no. (% of overall sample) unless otherwise indicated. Average age of mother at time of delivery was 30.9 ±5.6 years.
Average length of enrollment for dental coverage was 25.4 ±13.5 months.
The primary exposure variables in our analyses were periodontal and other dental treatment provided during the observation period. We generated treatment groups using the American Dental Association's Current Dental Terminology, version 3 (CDT-3) codes on treatment types. The CDT-3 dental coding system includes treatment codes but does not include disease classifications. The codes we used to define periodontal treatment included scaling and root planing and periodontal surgery. Periodontal and prophylaxis treatment classification and associated CDT-3 codes are available in Supplemental Table 1. In addition, we used CDT-3 code D1110 (dental prophylaxis) because this particular code, in addition to its preventive care purpose, is used in conjunction with scaling procedures.
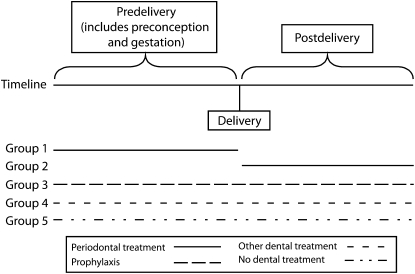
To evaluate the potential relationship between periodontal and other dental treatment and birth outcomes, we grouped all fully insured medical and dental members according to the type of dental services received and the timing of care relative to delivery. Thus, study participants were divided into 5 dental treatment groups, as shown in Figure 1: (1) women whose first instance of periodontal treatment occurred before delivery; (2) women whose first instance of periodontal treatment occurred postdelivery; (3) women who received only prophylactic treatment at least once during the period of observation, without any additional periodontal treatment; (4) women who received other dental treatment (e.g., restorative and emergency treatment, but no periodontal treatment or prophylaxis) at least once during the period of observation; and (5) women who received no dental treatment of any kind during the period of observation. Because periodontal disease is a chronic disease, we assume that the postdelivery periodontal treatment group (group 2) had clinical periodontal disease during pregnancy. The prophylaxis group (group 3) represented women who received preventive treatment. We assumed women who received preventive treatment to be more health conscious; we therefore included all women with either pre- or postprophylaxis treatment in this category.
FIGURE 1.
Dental treatment group classification and pregnancy outcomes in an insured US population: January 1, 2003–September 30, 2006.
Other variables controlled for in the analysis included the maternal age at delivery, neighborhood-level race/ethnicity and income, the presence of pregnancy complications, and the duration of continuous dental coverage. We calculated maternal age at delivery using the mother's birth date and the delivery date as recorded in the data set. Race/ethnicity and income were not available for individual cohort members, so we determined proxies by the use of the zip code of first residence recorded in the database referenced against census tract information. Thus, a surrogate for race/ethnicity was defined as percentage of African American residents within a woman's home zip code.24 A surrogate for household income was defined according to distribution of household income within the residence zip code.24 Complications of pregnancy were determined by identifying ICD-9 codes related to conditions known to be independent predictors of preterm birth or low birthweight or confounders. (Complications related to pregnancy and the puerperium, disease comorbidities, and associated ICD-9 codes are available in Supplemental Table 2, available as a supplement to the online version of this article at http://www.ajph.org).25,26
TABLE 2.
Relationship Between Dental Treatment Groups and Low Birthweight and Preterm Delivery in an Insured US Population: January 1, 2003–September 30, 2006
| Treatment Group Variable | No. | Observed Probability of Low Birth Weight,* No. (%) | Observed Probability of Preterm Delivery,* No. (%) |
| Received periodontal treatment before delivery | 464 | 17 (3.7) | 46 (9.9) |
| Received periodontal treatment after delivery | 622 | 11 (1.8) | 39 (6.3) |
| Received prophylactic treatment at least once during follow-up | 8010 | 260 (3.3) | 609 (7.6) |
| Received other dental treatment at least once during follow-upa | 2024 | 94 (4.6) | 190 (9.4) |
| No dental treatment of any kind during the period of observation | 12 321 | 612 (5.0) | 1241 (10.1) |
Note. By the χ2 test across all 5 categories of periodontal or dental treatment.
*P < .001.
Other dental treatment included nonperiodontal or nonprophylaxis procedures at any time during the period of observation.
For analytic purposes, we defined a single dichotomous complications of pregnancy variable, with a value of “1” indicating the occurrence of at least 1 complication or the presence of 1 or several factors associated with preterm delivery or low birthweight (Supplemental Table 2). We defined a variable representing the number of months of dental insurance coverage using monthly dental enrollment data. We used this variable to adjust for the evidence that, all other factors being equal, the likelihood of dental treatment would vary in proportion to the total span of continuous coverage for each member. Values for this particular variable ranged from 1 to 45 months. To reduce the potential for bias because of unequal duration of follow-up, we conducted confirmatory analyses in a subsample of women who had continuous medical and dental coverage for at least 12 months before delivery, throughout pregnancy, and 90 days after delivery.
We used initial descriptive statistics (percentages, means, and standard deviations) to characterize the study cohort. We used the Pearson χ2 test to compare the rates of low birthweight and preterm birth among the treatment groups. We also compared the treatment groups with respect to all the adjustment variables (complications of pregnancy, maternal age, distribution of African American residents by zip code, distribution of income by zip code, and duration of continuous enrollment) using the χ2 test, one-way analysis of variance, and the Kruskal-Wallis test. We used logistic regression analysis to compare outcome rates across treatment exposure groups while adjusting for additional covariates (duration of continuous dental coverage, maternal age, pregnancy complications, neighborhood-level income, and neighborhood-level race/ethnicity). Logistic regression modeling yielded estimated odds ratios (ORs) relating each treatment variable to the outcome, with ORs greater than 1 indicating increased probability for the outcome (i.e., suggesting a putative risk factor) and ORs less than 1 indicating decreased probability (i.e., a possible protective effect). We began regression analyses with the unadjusted model having the treatment group variable as the sole predictor. We then added the adjustment variables simultaneously to obtain adjusted estimates of the ORs relating treatment group to each outcome. We used SPSS, version 15.0 (SPSS, Inc, Chicago, IL) and Stata, version 10 (StataCorp LP, College Station, TX) for all analyses.
RESULTS
The number of women with deliveries during the specified timeframe was 29 068, representing women from 47 states, the District of Columbia, and Guam. Hawaii, North Dakota, and Wyoming were unrepresented in the data set, and 51.7% of the women were from California, Maryland, New Jersey, New York, or Texas. The deliveries included 28 961 live births and 107 stillborn events. Among the 29 068 total deliveries, 5285 women had ICD-9 codes indicating the presence of medical exclusion factors (ICD-9 codes for exclusion conditions are listed in Supplemental Table 3, available as a supplement to the online version of this article at http://www.ajph.org). Thirty-eight women had a reported maternal age of younger than 13 years or older than 50 years. There were 756 women who had multiple births. A total of 5627 women had 1 or more of the exclusion factors and were removed from the research sample. This selection resulted in a final analytic sample of 23 441 participants. Among the mothers in the final sample, mean age at the time of birth was 30.9 years, with a standard deviation of 5.6 years.
TABLE 3.
Logistic Regression Analysis Results of Low Birthweight and Preterm Birth in an Insured US Population: January 1, 2003 Through September 30, 2006
| Unadjusted OR (95% CI) | Adjusteda OR (95% CI) | |
| Low birthweight* | ||
| Treatment groups | ||
| Received periodontal treatment before delivery | 0.73 (0.45, 1.19) | 0.76 (0.46, 1.24) |
| Received periodontal treatment after delivery | 0.34 (0.19, 0.63) | 0.36 (0.20, 0.66) |
| Received prophylactic treatment at least once during follow-up | 0.64 (0.55, 0.74) | 0.71 (0.61, 0.83) |
| Received other dental treatment at least once during follow-upb | 0.93 (0.75, 1.16) | 0.96 (0.77, 1.21) |
| No dental treatment of any kind during the period of observation (Ref) | 1.00 | 1.00 |
| Preterm birth* | ||
| Treatment groups | ||
| Received periodontal treatment before delivery | 0.98 (0.72, 1.34) | 1.04 (0.76, 1.42) |
| Received periodontal treatment after delivery | 0.60 (0.43, 0.83) | 0.63 (0.45, 0.88) |
| Received prophylactic treatment at least once during follow-up | 0.73 (0.66, 0.81) | 0.80 (0.72, 0.89) |
| Received other dental treatment at least once during follow-up | 0.92 (0.79, 1.09) | 0.95 (0.81, 1.12) |
| No dental treatment of any kind during the period of observation (Ref) | 1.00 | 1.00 |
Note. OR = odds ratio; CI = confidence interval. Preterm was defined as a gestation of 37 weeks or less.
Adjusted for complications, percentage of African Americans in zip code area, income distribution in zip code area, duration of continuous dental coverage in months, and maternal age in years.
Other dental treatment included nonperiodontal or nonprophylaxis procedures at any time during the period of observation.
*P < .001 across all categories of the exposure variable.
The distribution of key analytic variables is shown in Table 1. Overall, 4.2% of birth outcomes were low birthweight and 9.1% were preterm. Of the women in the final analytic sample, 4.6% received periodontal treatment, 2.0% received periodontal services for the first time before delivery, and 2.6% had their first instance of periodontal treatment postdelivery. Dental prophylaxis was the most common dental procedure this group received; 34.2% received dental prophylactic treatment (D1110) without any periodontal treatment at least once during the period of observation. Sixty-three percent resided in zip codes whose population was between 1% and 10% African American, and 56.4% resided in zip codes whose income exceeded the 80th percentile nationally.
Unadjusted analyses indicated that the rates of low birthweight and preterm birth outcomes were lowest for women who received periodontal treatment postdelivery. Conversely, those who did not receive any dental care at all during the study period had the highest rates of low birthweight and preterm birth outcomes (Table 2). The low birthweight rate was 5.0% for women not receiving dental treatment, 4.6% for those receiving other dental treatment (nonperiodontal, nonprophylactic), 3.3% for those receiving prophylactic treatment, 3.7% for those receiving periodontal treatment before delivery, and 1.8% for those receiving postdelivery periodontal treatment (P < .001). The preterm birth rate was 10.1% for women not receiving dental treatment, 9.4% for those receiving other dental treatment, 7.6% for those receiving prophylactic treatment, 9.9% for those receiving periodontal treatment before delivery, and 6.3% for those receiving periodontal treatment postdelivery (P < .001).
In our assessment of potential confounders, our analyses revealed that the 5 exposure groups differed somewhat with respect to all the potential confounders: complication rate, maternal age, neighborhood-level percentage African American, neighborhood-level income, and duration of continuous enrollment (see Supplemental Table 4, available as a supplement to the online version of this article at http://www.ajph.org), indicating that it may be important to perform the adjusted analyses via regression.
Table 3 presents the results of the logistic regression analyses for low birthweight and preterm birth outcomes. The exposure groups differed significantly from one another with respect to risk of each adverse birth outcome. We calculated estimated ORs and 95% confidence intervals to compare the odds of low birthweight and preterm birth in each exposure group to the referent group, defined as women receiving no dental treatment of any kind during the period of observation.
Adjustment for secondary covariates caused very little change to the estimated effects for the treatment variables. The unadjusted and adjusted models indicate that postdelivery periodontal treatment yielded the lowest likelihood of low birthweight and preterm birth compared with no dental treatment. In addition, women who received only prophylactic treatment during the observation period had lower odds of preterm birth and low birthweight in the adjusted logistic regression analyses compared with women who received no dental treatment of any kind. For both birth outcomes, receiving periodontal treatment before delivery and receiving other dental treatment regardless of type did not differ significantly compared with no treatment at all.
To ensure that findings were not unduly biased by an unequal duration of follow-up, we conducted confirmatory analyses in a subset of 8824 women who received continuous coverage for at least 12 months before delivery and at least 90 days after delivery. The findings from the subsample analysis were completely consistent with those from the analysis of the full sample (data not shown), so the results cannot be attributed to any bias from different lengths of follow-up. An evaluation of the goodness of fit of the adjusted models via the Hosmer–Lemeshow statistic27 indicated that both models fit the data adequately.
DISCUSSION
We used claims data from a large national insurance database to explore the association between dental care and adverse pregnancy outcomes. These data demonstrated that women who received periodontal treatment postdelivery or dental prophylaxis at any time during the observation period had lower odds of adverse pregnancy outcomes compared with women who did not receive any form of dental care.
Some specific features of the study design need to be addressed to correctly interpret the findings. First, the data available for analyses did not include oral health or periodontal disease diagnostic codes but rather treatment codes. Therefore, the oral and periodontal status of the involved women is largely unknown. Instead, we used dental and medical claims data derived from professional ICD-9 and CDT-3 coding, which may not accurately reflect true disease status. In the medical setting, some diagnoses may be missed, and dental claims do not provide concomitant diagnostic coding. Second, although treatment codes indicating the type of dental treatment provided were available and constituted the “exposure” variable in our analysis, the effectiveness of the provided treatment in improving the periodontal conditions is unknown.
Third, our ability to adjust for relevant covariates was limited because individual-level demographic characteristics such as race/ethnicity, socioeconomic status, and cigarette smoking were unavailable. Instead, our adjusted analyses had to involve neighborhood-level surrogates for race/ethnicity and socioeconomic variables, and a certain degree of classification bias cannot be ruled out, although it is unlikely that it has systematically affected our findings.
Fourth, this sample of fully insured individuals may not be representative of insured women nationwide. Approximately 45% of the insurance market was fully insured in 2006. In addition, we used the group of women receiving periodontal treatment postdelivery as a risk group to be a proxy for women who likely had periodontal disease during gestation and possibly also during preconception that remained untreated at the time of delivery. This may indicate that they had prior knowledge of the need for treatment and, as such, were taking care to maintain oral health.
In our analyses, we combined the provision of periodontal treatment during preconception and during gestation into a single predelivery periodontal treatment group for 2 reasons: first, we could not determine the exact conception date from the available databases, and second, there were virtually no women receiving periodontal treatment in the 9 months before delivery (i.e., during the presumed gestational period). Instead, the most common procedure received by these women was dental prophylaxis.
Women who received dental prophylaxis and who received no treatment at any time for periodontal disease had a lower risk of preterm birth and low birthweight than did those receiving no dental treatment. We believe the women represented in the dental prophylaxis group (group 3) included women who attend dental offices for routine examinations and preventive treatment and, as such, are probably health-conscious dental care seekers with good periodontal status. It is likely that these women received more preventive treatment and advice and earlier and more regular medical care during gestation. Therefore, the evidence that these women experienced the best birth outcomes among all analyzed treatment groups may be a consequence of their good oral and general health status and their health-promoting behaviors rather than of the provision of oral prophylaxis per se.
Nevertheless, it is noteworthy that the incidence of adverse birth outcomes was lower among women who received some dental care and more so among those who received postdelivery periodontal care or those who received prophylactic treatment compared with the nonconsumers of dental care. The observation that women who received postpartum periodontal therapy experienced fewer adverse outcomes compared with those who received antepartum periodontal therapy may suggest that women with untreated periodontitis throughout their gestation fared better than did those who had their condition treated before delivery.
We emphasize again that the exact periodontal status of the women in the 2 groups is unknown and not necessarily comparable, as are the type, quality, and efficacy of the provided therapy. For example, mucogingival flap procedures that are also encompassed under the periodontal treatment codes used are largely considered to be elective and likely fall under the treatment service category that most dentists would traditionally postpone until after delivery.28 A recent study of an insured population showed that dental service utilization during gestation declines, but postdelivery and predelivery dental service utilization is generally similar.29 It should also be remembered that the current American Dental Association guidelines for treatment during pregnancy recommend a limited protocol including oral prophylaxis or preventive homecare instructions rather than comprehensive periodontal treatment.28
In a recent multicenter randomized controlled trial, Michalowicz et al. concluded that both essential dental care and nonsurgical treatment provided during the second trimester are safe.16,30 The findings of the current study support and extend these observations, as dental treatment did not increase the odds of adverse birth outcomes.
Contrary to most studies that have examined the effects of periodontitis and its treatment on adverse pregnancy outcomes in uninsured, low socioeconomic groups, our study involved insured women in middle or upper income groups, with approximately 60% of the cohort residing in zip codes with incomes exceeding the 80th percentile nationally. The only other published report that examined the effect of periodontitis on birth outcomes in an insured cohort concluded that periodontitis was an independent risk factor for adverse pregnancy outcomes in middle-income women.31
This 3-year retrospective examination of a large insurance company database suggests that receiving preventive dental treatment is associated with a lower incidence of adverse birth outcomes compared with instances when no dental services are delivered. Provision of postdelivery periodontal treatment and dental prophylaxis at any time was significantly associated with lower odds of adverse pregnancy outcomes compared with no dental treatment in adjusted analyses. It is unclear whether these findings reflect a truly beneficial effect of dental care or merely reflect the increased utilization of prophylactic and other dental care services by health-conscious, care-seeking women with access to medical and dental care services.
Acknowledgments
This study was supported in part by the New York State Foundation for Science, Technology, and Innovation (grant C040123), Aetna, and a Clinical and Translational Science Award from the National Institutes of Health (grant RR-025158).
The authors wish to thank Claire M. Spettell, PhD, of Aetna Integrated Informatics for her review of the article.
Human Participation Protection
The Columbia University institutional review board categorized this study as exempt from review because of its use of de-identified data.
References
- 1.Martin JA, Hamilton BE, Sutton PD, et al. Births: final data for 2004. National Vital Statistics Reports. 2006;55(1). Hyattsville, MD: National Center for Health Statistics; Available at: http://www.cdc.gov/nchs/data/nvsr/nvsr55/nvsr55_01.pdf. Accessed May 3, 2007 [PubMed] [Google Scholar]
- 2.Lorenz JM, Wooliever DE, Jetton JR, et al. A quantitative review of mortality and developmental disability in extremely premature newborns. Arch Pediatr Adolesc Med. 1998;152(5):425–435 [DOI] [PubMed] [Google Scholar]
- 3.Institute of Medicine Preterm birth: causes, consequences, and prevention. July 2006. Available at: http://www.iom.edu/Reports/2006/Preterm-Birth-Causes-Consequences-and-Prevention.aspx. Accessed March 5, 2009
- 4.Scannapieco FA, Bush RB, Paju S. Periodontal disease as a risk factor for adverse pregnancy outcomes. A systematic review. Ann Periodontol. 2003;8(1):70–78 [DOI] [PubMed] [Google Scholar]
- 5.Lopez NJ, Da Silva I, Ipinza J, et al. Periodontal therapy reduces the rate of preterm low birthweight in women with pregnancy-associated gingivitis. J Periodontol. 2005;76(suppl 11):2144–2153 [DOI] [PubMed] [Google Scholar]
- 6.Lopez NJ, Smith PC, Gutierrez J. Periodontal therapy may reduce the risk of preterm low birthweight in women with periodontal disease: a randomized controlled trial. J Periodontol. 2002;73(8):911–924 [DOI] [PubMed] [Google Scholar]
- 7.Tarannum F, Faizuddin M. Effect of periodontal therapy on pregnancy outcome in women affected by periodontitis. J Periodontol. 2007;78(11):2095–2103 [DOI] [PubMed] [Google Scholar]
- 8.Vergnes J-N, Sixou M. Preterm low birthweight and maternal periodontal status: a meta analysis. Am J Obstet Gynecol. 2007;196(2):135.e1–135.e7 [DOI] [PubMed] [Google Scholar]
- 9.Offenbacher S, Boggess KA, Murtha AP, et al. Progressive periodontal disease and risk of very preterm delivery. Obstet Gynecol. 2006;107(1):29–36 [DOI] [PubMed] [Google Scholar]
- 10.Khader YS, Ta'ani Q. Periodontal diseases and the risk of preterm birth and low birthweight: a meta analysis. J Periodontol. 2005;76(2):161–165 [DOI] [PubMed] [Google Scholar]
- 11.Jeffcoat MK, Hauth JC, Geurs NC, et al. Periodontal disease and preterm birth: results of a pilot intervention study. J Periodontol. 2003;74(8):1214–1218 [DOI] [PubMed] [Google Scholar]
- 12.Mitchell-Lewis D, Engebretson SP, Chen J, et al. Periodontal infections and pre-term birth: early findings from a cohort of young minority women in New York. Eur J Oral Sci. 2001;109(1):34–39 [DOI] [PubMed] [Google Scholar]
- 13.Moore S, Ide M, Coward PY, et al. A prospective study to investigate the relationship between periodontal disease and adverse pregnancy outcome. Br Dent J. 2004;197:251–258 [DOI] [PubMed] [Google Scholar]
- 14.Davenport ES, Williams CECS, Sterne JAC, et al. Maternal periodontal disease and preterm low birthweight: case-control study. J Dent Res. 2002;81(5):313–318 [DOI] [PubMed] [Google Scholar]
- 15.Vettore MV, Leal M, Leão AT, et al. The relationship between periodontitis and preterm low birthweight. J Dent Res. 2008;87(1):73–78 [DOI] [PubMed] [Google Scholar]
- 16.Michalowicz BS, Hodges JS, DiAngelis AJ, et al. Treatment of periodontal disease and the risk of preterm birth. N Engl J Med. 2006;355(18):1885–1894 [DOI] [PubMed] [Google Scholar]
- 17.Offenbacher S, Beck JD, Jared HL, et al. Effects of periodontal therapy on rate of preterm delivery. Obstet Gynecol. 2009;114(3):551–559 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Albert DA, Sadowsky D, Papapanou P, et al. An examination of periodontal treatment and per member per month (PMPM) medical costs in an insured population. BMC Health Serv Res. 2006;6:103–113 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Leake JL, Werneck RI. The use of administrative databases to assess oral health. J Public Health Dent. 2005;65(1):21–35 [DOI] [PubMed] [Google Scholar]
- 20.Tyree PT, Lind BK, Lafferty WE. Challenges of using medical claims data for utilization analysis. Am J Med Qual. 2006;21(4):269–275 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Fowles JB, Fowler EJ, Craft C. Validation of claims diagnoses and self-reported conditions compared with medical records for selected chronic diseases. J Ambul Care Manage. 1998;21(1):24–34 [DOI] [PubMed] [Google Scholar]
- 22.Fowles JB, Fowler E, Craft C, et al. Comparing claims data and self-reported data with the medical record for Pap smear rates. Eval Health Prof. 1997;20(3):324–342 [DOI] [PubMed] [Google Scholar]
- 23.International Classification of Diseases, Ninth Revision Geneva, Switzerland: World Health Organization; 1980 [Google Scholar]
- 24.Krieger N. Overcoming the absence of socioeconomic data in medical records: validation and application of a census-based methodology. Am J Public Health. 1992;82(5):703–710 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.McElrath TF, Hecht JL, Dammann O, et al. Pregnancy disorders that lead to delivery before the 28th week of gestation: an epidemiologic approach to classification. Am J Epidemiol. 2008;168(9):980–989 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Villar J, Carroli G, Wojdyla D, et al. ; World Health Organization Antenatal Care Trial Research Group. Preeclampsia, gestational hypertension and intrauterine growth restriction, related or independent conditions? Am J Obstet Gynecol. 2006;194(4):921–931 [DOI] [PubMed] [Google Scholar]
- 27.Hosmer DW, Lemeshow S. Applied Logistic Regression. New York, NY: John Wiley & Sons; 1989 [Google Scholar]
- 28.American Dental Association Council on Access, Prevention and Interprofessional Relations Women's oral health issues. Chicago: American Dental Association; 2006. Available at: http://www.ada.org/sections/professionalResources/pdfs/healthcare_womens.pdf. Accessed March 5, 2009 [Google Scholar]
- 29.Jiang P, Bargman EP, Garrett NA, et al. A comparison of dental service use among commercially insured women in Minnesota before, during and after pregnancy. J Am Dent Assoc. 2008;139(9):1173–1180 [DOI] [PubMed] [Google Scholar]
- 30.Michalowicz BS, DiAngelis AJ, Novak MJ, et al. Examining the safety of dental treatment in pregnant women. J Am Dent Assoc. 2008;139(6):685–695 [DOI] [PubMed] [Google Scholar]
- 31.Pitiphat W, Joshipura KJ, Gillman MW, et al. Maternal periodontitis and adverse pregnancy outcomes. Community Dent Oral Epidemiol. 2008;36(1):3–11 [DOI] [PubMed] [Google Scholar]