Abstract
We conducted the first US study using graphic-output temperature data loggers in quantifying cold chain failure. Fifty-four vaccine refrigerators of a county outpatient health system were studied. Forty-eight percent maintained temperatures of 2°C to 8°C and 24% had protracted periods of temperatures less than 0°C. The correlation between the percentage of refrigerators with freezing temperatures and the pertussis rate for each health region was r = 0.76. The findings suggest that improper vaccine storage may have contributed to recent increases in pertussis rates.
From 2001 to 2005, the incidence of pertussis in Harris County, Texas, increased 196% to a rate of 5.6 cases per 100 000.1–3 This elevated rate paralleled a peak in the overall US incidence.2 Domestic studies attempted to explain the higher incidence by implicating a fall in immunity among vaccinated adults, unvaccinated children causing disease clusters, and seasonal variation.1 However, a Canadian outbreak during the 1990s was attributed to excessively cooled pertussis vaccine.4 Vaccine spoilage as a result of cooling has been studied outside of the United States,5–13although there have been few domestic studies.7
The purpose of our study was to evaluate the use of data loggers in quantifying the cold cain failure rate within the Harris County Hospital District community health center network.14,15 The health centers are the primary provider of indigent care services in Harris County; they support approximately 580 000 outpatient visits per year.
METHODS
We used Extech TH10 digital data loggers (Extech/Instrusmart, Burlington, VT), which sample the temperature inside refrigerators every minute and can store up to 32 000 data points. A built-in Universal Serial Bus port enabled periodic data downloads to a spreadsheet and printing a temperature–time graph. Users can set the data collection frequency and alarm values. The devices have a 0.1°C resolution with an accuracy of ±0.5°C.
We studied 54 refrigerators at 13 community health centers (an average of 4 refrigerators per center). Temperature data loggers were placed in each refrigerator compartment for a minimum of 6 days and the temperature was automatically recorded every minute. The data were then transferred to individual Excel spreadsheets (Excel 2000).
The percentage of vaccine refrigerator compartments with freezing temperatures was calculated for each health region within the City of Houston, a subset of Harris County. The results were correlated with the 2005 to 2009 annual average rate of pertussis per 100 000 persons in each area.
RESULTS
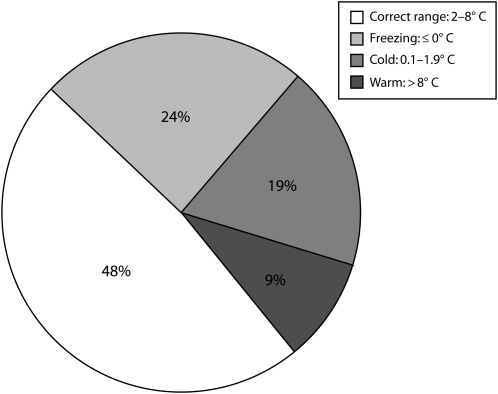
Twenty-six refrigerator compartments (48%) maintained a stable temperature within the 2°C to 8°C range recommended by the World Health Organization. Thirteen refrigerator compartments (24%) had freezing temperatures at some point during the data collection. Ten refrigerators (19%) registered temperatures from 0.1°C to 1.9°C with no freezing. Five refrigerators had temperatures greater than 8°C during the data collection. These data are summarized in Figure 1 (also see the table available as a supplement to the online version of this article at http://www.ajph.org).
FIGURE 1.
Percentage of Refrigerators Within and Outside of Correct Temperature Range Houston, Texas, 2005–2009
Refrigerators that registered freezing levels had temperatures less than 0°C for an average of 8.0% of the total time recorded (equivalent to 2 hours per day). Refrigerators that were excessively cold but not freezing maintained temperatures between 0.1°C and 1.9°C for an average of 25.3% of the total time recorded.
The Pearson correlation between the percentages of refrigerator compartments with freezing temperatures in each health region of Houston and the 2005 to 2009 annual average rate of pertussis per 100 000 persons in each area was r = 0.76 (P < 0.05). These data are summarized in Table 1.
TABLE 1.
Percentage of Vaccine Refrigerators with Freezing Temperatures and the Pertussis Rate: Houston, Texas, 2005–2009
| Health Region | % Refrigerator Compartments With Freezing Temperatures | Average Annual Pertussis Rate per 100 000 Personsa |
| North | 33 | 4.3 |
| North East | 80 | 6.3 |
| Central West | 56 | 3.5 |
| South | 43 | 2.9 |
| South East | 14 | 3.1 |
| South West | 45 | 3.0 |
Source. Pertussis data provided by the City of Houston Public Health Department.
r = 0.76; P < .05.
Six of the 28 refrigerators could not maintain a stable temperature regardless of the thermostat setting and were not suitable for storing vaccines (figure available as a supplement to the online version of this article at http://www.ajph.org). Only 1 was recognized as defective using the Vaccines for Children recommended standard of recording temperatures from digital thermometers twice every workday.15
DISCUSSION
Manufacturer recommendations for the storage of acellular pertussis vaccine advise discarding any vaccine exposed to temperatures less than 0°C since the vaccine is inactivated upon freezing.15,16 Approximately 24% of the refrigerators studied exposed vaccines to considerable durations of subzero temperatures. The periods of freezing temperatures typically occurred on weekends and nights.
The Harris County Hospital District adhered to the current vaccine storage guidelines recommended by Vaccines for Children and internal audits have complied with a Joint Commission survey conducted during the study. The inadequate storage would not have been detected or quantified without the use of the digital temperature data loggers. The graphic output provided by the loggers has allowed us to interpret temperature data in a manner not possible with the traditional twice-daily temperature records.
Our findings raise the possibility that the recent increase in cases of pertussis may be partially the result of improper storage of acellular pertussis vaccine. The current standard of twice-daily readings from thermometers is not adequate to maintain proper vaccine storage. Given the low cost of these devices ($35–45), adoption of digital data loggers for maintaining the cold chain should be considered.
Acknowledgments
We acknowledge the Department of Family and Community Medicine at Baylor College of Medicine for providing the funds used to purchase the data loggers.
Note. The authors have no financial interests or ownership in any companies related to the study.
Human Participant Protection
The institutional review board at Baylor College of Medicine granted approval for the study.
References
- 1.Harris County Public Health and Environmental Services. 2007 Annual Report. Available at: http://www.hcphes.org/2007Annual.pdf. Accessed February 7, 2010.
- 2.Jajosky RA, Hall PA, Adams DA, et al. Summary of notifiable diseases – United States, 2004. MMWR Morb Mortal Wkly Rep. 2006;53(53):1–79 [PubMed] [Google Scholar]
- 3.O'Brien JA, Caro JJ. Hospitalization for pertussis: profiles and case costs by age. BMC Infect Dis. 2005;5:57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Milhomme P. Cold chain study: danger of freezing vaccines. Can Commun Dis Rep. 1993;19:33–38 [PubMed] [Google Scholar]
- 5.Ortega Molina P, Astasio AP, Albaladejo VR, et al. Vaccine storage cold chain at primary care centers in one area of Madrid: keeping the chain intact and degree of knowledge. Rev Esp Salud Publica. 2002;76(4):333–346 [PubMed] [Google Scholar]
- 6.Boros CA, Hanlon M, Gold MS, Roberton DM. Storage at -3 degrees C for 24 h alters the immunogenicity of pertussis vaccines. Vaccine. 2001;19(25-26):3537–3542 [DOI] [PubMed] [Google Scholar]
- 7.Matthias DM, Robertson J, Garrison MM, Newland S, Nelson C. Freezing temperatures in the vaccine cold chain: a systematic literature review. Vaccine. 2007;25(20):3980–3986 [DOI] [PubMed] [Google Scholar]
- 8.Miller NC, Harris MF. Are childhood immunization programmes in Australia at risk? Investigation of the cold chain in the Northern Territory. Bull World Health Organ. 1994;72(3):401–408 [PMC free article] [PubMed] [Google Scholar]
- 9.Gzyl A, Augustynowicz E, Rabczenko D. Potency of pertussis component in the DTP vaccine–an overview of a three decade study in Poland. Biologicals. 2004;32(3):129–137 [DOI] [PubMed] [Google Scholar]
- 10.Andreescu V, Marion M, Ivan I, et al. Influence of temperature on the stability of pertussis vaccine. Arch Roum Pathol Exp Microbiol. 1985;44(4):283–292 [PubMed] [Google Scholar]
- 11.Haworth EA, Booy R, Stirzaker L, Wilkes S, Battersby A. Is the cold chain for vaccines maintained in general practice? BMJ. 1993;307(6898):242–4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Thakker Y, Woods S. Storage of vaccines in the community: weak link in the cold chain? BMJ. 1992;304(6829):756–758 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Page SL, Earnest A, Birden H, et al. Improving vaccination cold chain in the general practice setting. Aust Fam Physician. 2008;37(10):892–896 [PubMed] [Google Scholar]
- 14.Gold MS, Martin L, Nayda CL, Kempe AE. Electronic temperature monitoring and feedback to correct adverse vaccine storage in general practice. Med J Aust. 1999;171(2):83–84 [DOI] [PubMed] [Google Scholar]
- 15.Vaccine Storage and Handling Toolkit. Atlanta, GA: Centers for Disease Control and Prevention; 2008 [Google Scholar]
- 16.Jacquet JM, Bégué P, Grimprel E, et al. Safety and immunogenicity of a combined DTPa-IPV vaccine administered as a booster from 4 years of age: a review. Vaccine. 2006;24(13):2440–2448 [DOI] [PubMed] [Google Scholar]