Abstract
Objective
To evaluate the impact of generic substitution decision support on electronic (e-) prescribing of generic medications.
Design
The authors analyzed retrospective outpatient e-prescribing data from an academic medical center and affiliated network for July 1, 2005–September 30, 2008 using an interrupted time-series design to assess the rate of generic prescribing before and after implementing generic substitution decision support. To assess background secular trends, e-prescribing was compared with a concurrent random sample of hand-generated prescriptions.
Measurements
Proportion of generic medications prescribed before and after the intervention, evaluated over time, and compared with a sample of prescriptions generated without e-prescribing.
Results
The proportion of generic medication prescriptions increased from 32.1% to 54.2% after the intervention (22.1% increase, 95% CI 21.9% to 22.3%), with no diminution in magnitude of improvement post-intervention. In the concurrent control group, increases in proportion of generic prescriptions (29.3% to 31.4% to 37.4% in the pre-intervention, post-intervention, and end-of-study periods, respectively) were not commensurate with the intervention. There was a larger change in generic prescribing rates among authorized prescribers (24.6%) than nurses (18.5%; adjusted OR 1.38, 95% CI 1.17 to 1.63). Two years after the intervention, the proportion of generic prescribing remained significantly higher for e-prescriptions (58.1%; 95% CI 57.5% to 58.7%) than for hand-generated prescriptions ordered at the same time (37.4%; 95% CI 34.9% to 39.9%) (p<0.0001). Generic prescribing increased significantly in every specialty.
Conclusion
Implementation of generic substitution decision support was associated with dramatic and sustained improvements in the rate of outpatient generic e-prescribing across all specialties.
Introduction
Despite decades of policies directed toward reducing healthcare costs through increased prescribing of generic medications, US physicians continue to over-prescribe brand name medications. Electronic prescribing is an application of health information technology with potential to improve generic prescribing practices. Furthermore, user interface design techniques are considered a critical component of healthcare decision-support technology. Despite this opportunity, there are no published studies describing the effect of e-prescribing interventions on generic prescribing rates. This report describes an approach to integrate generic substitution knowledge into the workflow of providers using e-prescribing systems.
Background
Currently, US providers write 1.5 billion prescriptions each year at an annual cost of US$286.5 billion,1 an expense expected to double over the next 10 years.2 Overall, only 58–67% of medications dispensed in 2007 were generic; this rate varies among states.3 4 While the US fill rate of generic medications is higher than many other countries (eg, 48% in Canada, 30% in Australia, 17% in Japan), experts estimate the maximum achievable rate of US generic prescriptions to be 80% and possibly higher as more brand name medications come off patent.1 5 Increased outpatient generic medication prescribing could save over US$9 billion, or roughly 11% of annual medication expenditures.6 These savings would be realized by both insurers and patients. Americans spend significantly more out of pocket for medications than patients from other countries. Over 66% of US patients who regularly take medications spend more than US$500 per year on them, and 30% spend more than US$1000 per year.7 In addition, a statistically significant increase in medication adherence has been demonstrated in patients prescribed generic medications.8 With a few limited exceptions, there is no evidence that generic medication usage has adversely affected patient outcomes.9 Unfortunately, prescribers routinely fail to consider patient out-of-pocket costs or issues of adherence when choosing prescription drugs.10 Worse still, older patients and economically disadvantaged patients receive proportionally fewer generic medication prescriptions than others.11 12 When faced with increased medication costs, older patients often skip doses or reduce them and do not refill prescriptions, leading to poorer clinical outcomes and increased system-wide healthcare costs.13 14
A recent American Association of Retired Persons Public Policy Institute publication described the following strategies to increase use of generic medications: generic substitution policies; tiered-design medication plans; consumer and prescriber education; narrower institutional medication formularies; pharmacist and prescriber incentives; and electronic prescribing.15 Insurers and policy makers developed many of these strategies in an attempt to control medication costs.16 In addition, researchers have identified the following barriers that public policy alone may not be able to circumvent.
Patient knowledge gaps. In one study, almost 40% of patients said they had little knowledge about generic medications.17 Another study showed that patients associate higher price with increased value.18 Information related to prescription medications currently available in the USA is of limited quality, exacerbating challenges posed by low health literacy. In addition, prescription medication labels,19 20 warning labels,21 and other materials, such as medication information leaflets22 23 and FDA medication guides,24 all suffer from poor design and poor readability, thus limiting their utility.
Physician knowledge gaps. In one study, only 40% of physicians surveyed believed that generic medications were usually therapeutically equivalent to brand name medications, while 36% agreed with the statement that ‘therapeutic failures are a serious problem with generic products.’25 Complicating this problem is the fact that the pharmaceutical industry spends over US$7 billion per year marketing brand name products directly to physicians.26
Generic substitution policies vary by state; in Tennessee, pharmacists can substitute generic medications unless a brand name is explicitly prescribed. However, generic substitution is not required and may be impacted by pharmacist workload. An intervention to encourage prescribing by the generic name is an effective way to ensure use of generic medications.
Although provider education may improve generic medication prescribing rates, simply providing data to prescribers may not be enough. For example, showing prescribers data about costs has marginal benefit—only up to 10% in some studies.27 28 A retrospective study in 2005 showed no differences between e-prescribers and traditional prescribers in formulary compliance or generic medication prescribing.29 A 2008 study suggested that physicians with handheld electronic formulary access have a lower rate of increase in brand name, non-formulary medication prescribing.30 More recently, Fischer et al16 demonstrated savings through increased generic prescribing after integrating formulary decision support into an e-prescribing system. However, formulary decision support will not be available for all patients, and will be out of date if e-prescribing systems do not use real-time interfaces to pharmacy benefit managers and eligibility databases.
As e-prescribing programs gain attention and acceptance at the national level,31 32 the challenge is to learn from early adopters about how to improve generic prescribing. Experience with decision support tools suggests that sophisticated probabilistic or rule-based models are unnecessarily complicated and can be replaced with people- and process-focused implementations.33
In 2004, Vanderbilt Medical Center began a rollout of a locally developed outpatient e-prescribing system called RxStar. We observed a suboptimal rate of generic medication prescribing and consequently completed a series of focus groups in 2005 to help us understand local prescribing processes.34 As a result of our findings, we instituted minimally obtrusive changes in RxStar on September 25, 2006. Starting on that date, available generic formulations were displayed in a larger, bolder font, and generic medications were listed above brand name medications. Anecdotal evidence suggested that these changes affected e-prescribing practices. We performed this study to determine the effectiveness of generic substitution decision support in increasing e-prescribing of generic medications.
Methods
The study was conducted at Vanderbilt University Medical Center (VUMC). During the study period (July 1, 2005–September 30, 2008) prescribers wrote over 1.3 million electronic medication prescriptions for over 800 000 patients. They represented approximately half of all prescriptions written during the period, based on manual counts of prescriptions sent to VUMC on-site pharmacies (data not shown). The study examined prescribing habits of attending physicians, house staff, nurses, and advanced practice nurses at Vanderbilt who use e-prescribing. Authorized prescribers (physicians and advanced practice nurses) entered 51% of the total prescriptions directly; nurses entered the remainder. Of note, nurses acting as an agent of the prescriber can renew prescriptions using the e-prescribing system. This approach is modeled after the workflow used in our clinics before the implementation of e-prescribing as described by Johnson and Fitzhenry.34 In brief, a nurse can create a renewal for an expired prescription based on a prescriber's order. The nurse can use e-prescribing after the ordering provider provides the nurse with access as the provider's agent. Prescriptions contain the digital signatures of the ordering provider and the nurse.
The RxStar system was developed at VUMC in collaboration with the doctors and nurses of the Vanderbilt Medical Group's outpatient clinics. These clinics are located in urban and suburban locations. They include sites on the university campus itself and as far as 40 miles from the city. The program was launched in early 2004 and is used by over 3000 prescribers who generate over 80 000 electronic prescriptions per month. The RxStar system supports many of the commonly recommended tools for clinical decision support, including formulary and benefit checking, therapeutic substitution when a proposed medication is not covered by a patient's insurance, weight-based dosing for pediatrics, dose-limit checking, drug allergy warnings, potential drug–drug interaction warnings, geriatric precaution warnings, and other warnings. Medication knowledge is provided by First Databank (FDB).
The RxStar system is fully integrated into Vanderbilt's electronic health record system. Prescriptions are printed or electronically submitted to a pharmacy according to patient preferences. In addition, all prescriptions are automatically entered into a patient's medication list.
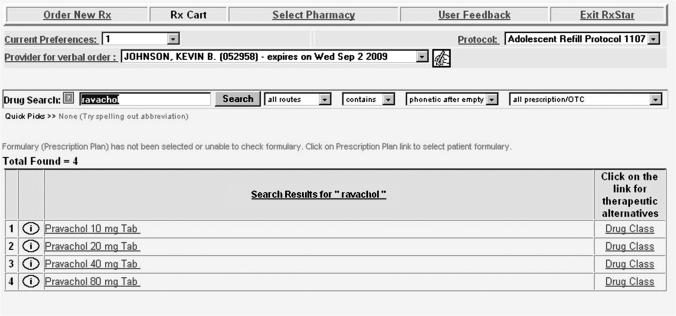
Like many e-prescribing systems, RxStar initially provided a free-text data entry field that allowed the user to search for a medication name. The system returned best matches for the search term, without attention to whether the result set included generic names in addition to brand names (figure 1). After a medication name was selected the user would modify the dose, route, schedule, amount, refills, and special instructions. Once finalized, the prescription could be printed, or, more commonly, electronically faxed to a pharmacy selected from an online database.
Figure 1.
Ordering a medication using RxStar prior to implementation of e-prescribing decision support with generic medication suggestions. A user enters a name of a branded medication or part of a brand name as a search string and clicks the ‘search’ button. Only the brand name formulations that match the search string are displayed.
In 2005, VUMC began investigating ways to improve the rate of generic medication prescribing in an effort to curb unnecessary prescription costs and meet pay-for-performance generic prescribing challenges. In response, the RxStar team conducted user-centered design sessions to create a new user interface that would recommend generic alternatives to brand name medications.
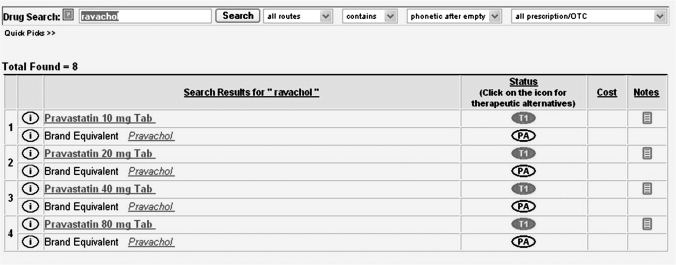
Figure 2 shows the system after the interface had been redesigned to emphasize generic prescribing. A clinician wishing to prescribe ‘Pravachol 40 mg’ searches for it in RxStar (figure 2). First, RxStar finds all medications—generic or branded—that match the search criteria. Then, using tools available through FDB, RxStar creates a list of generic formulations associated with Pravachol. They are displayed as bolded results in the medication selection screen. Brand name medications also are displayed, but are listed below the generic medication in a slightly smaller, unbolded font (figure 2). First DataBank knowledge about the availability of a packaged form is used to determine if a generic formulation is displayed; if a generic formulation is not available, it is not seen. If the clinician searches for ‘pravastatin 40 mg’, RxStar returns the same results, displaying the generic formulation first, with the brand name below (figure 2). The rationale behind this design was that providers could use the language they were accustomed to using to search for medications (ie, brand names), but would be presented with a generic equivalent in a prominent way that would remind them of its availability. Therapeutic (within medication class) generic substitution recommendations are not provided by RxStar.
Figure 2.
Ordering a medication using RxStar following implementation of e-prescribing decision support with generic medication suggestions. A user searches for a brand name medication. RxStar displays the names of all generic formulations with brand equivalents below each generic formulation. To the right of each result, RxStar displays the formulary status (approved, prior authorization required, etc).
To assess the impact of this modification on the rate of generic medication prescribing, we queried our prescribing database to retrieve all prescriptions generated beginning in July, 2005 (14 months before implementation of the new interface) and continuing through September, 2008 (2 years after the intervention). These data were combined with data from the credentialing office to identify the department and clinical role of the person creating the prescription (attending physician, house staff, nurse, or advance practice nurse). Prescriptions were labeled as ‘brand’ or ‘generic’ by an additional query of the FDB database. A preliminary analysis of this process found that the database labeled medications with 100% accuracy. In addition, we retrieved data about the prescriber's medical specialty, and a date and time stamp for each prescription. All patient and physician identifiers were removed and replaced with unique codes that could not be used to re-link data to their original source. The analysis began with all prescribing data from July 1, 2005 through September 30, 2008. We excluded 110 184 (8.5%) prescriptions because of missing values for prescriber, department, or type of prescription. We excluded an additional 5650 (0.4%) prescriptions ordered by two departments (Department of Cardiac and Thoracic Surgery and Department of Nuclear Medicine) that only used the system after the implementation date. Our final dataset contained over 1.1 million electronic prescriptions.
To determine the rate of generic prescribing without the aid of the e-prescribing system, we randomly sampled and manually reviewed 4456 handwritten prescriptions that were filled at a single VUMC outpatient pharmacy during three 1-week periods (pre-implementation, immediate post-implementation, and end-of-study); a manual review of all prescriptions during the study period would have been time prohibitive. We selected the largest and busiest of three VUMC outpatient pharmacies as the control pharmacy for a representative sample and for ease of access to non-RxStar prescriptions. We compared the proportion of generic prescribing for RxStar prescriptions with non-RxStar prescriptions. All prescriptions from non-VUMC prescribers were excluded.
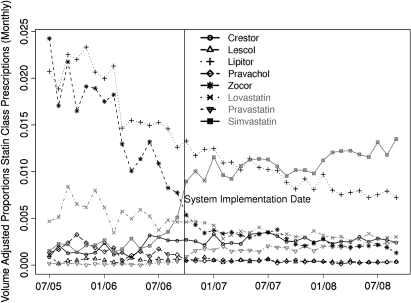
To determine if recommendations for generic prescriptions affected within-class substitutions, we assessed the proportion of statins (prescriptions to treat hypercholesterolemia). We included each of the six statins available during the study period: atorvastatin (Lipitor, available as brand only), fluvastatin (Lescol, available as brand only), lovastatin (Mevacor), pravastatin (Pravachol), rosuvastatin (Crestor, available as brand only), and simvastatin (Zocor). For each medication we summarized the volume-adjusted proportion of statin prescriptions over time. We determined the within-class effect for the highest volume brand name statin, Lipitor, using a generalized estimating equations (GEEs) intra-class correlation coefficient model.
We tested system stability 1 month prior to the ‘system implementation date’ by piloting the generic substitution decision support changes in a single internal medicine clinic. During the analysis, we included the pilot month prescribing data from this clinic in the pre-implementation group.
Statistical analysis
We described the effect of our system change on generic prescribing with frequencies, percentages and 95% CIs. χ2 Tests were used to compare the control group with the RxStar sample prescribed at the same time. Owing to the large size of our dataset, we reported 95% CIs instead of p values of conducted hypothesis tests. To study the generic prescribing behavior of nurses and prescribers during pre- and post-intervention periods and to control for prescribers' cluster effect, we used GEEs with logit link and binomial distribution. The model included the main effects of the system (before/after), days from study commence (linear), role, department, and two-way interactions of the system by role and the system by department. Covariance weighting generally permits efficiency gains over independence weighting but, owing to our large sample size, covariance weighting was not computationally feasible and efficiency was not a concern in the analysis. Therefore, we adjusted for clustering by physician using GEEs with a working independence covariance matrix followed by robust or sandwich SE adjustment to quantify uncertainty. The 95% CIs were constructed by Wald statistics.
Results
Table 1 shows the usage of the e-prescribing system by each specialty (department). Medicine generated the largest number of prescriptions (50%), followed by pediatrics (11%), family practice (7%), general surgery (7%), and psychiatry (6%). More than 1.1 million prescriptions were created during the evaluation period, with 170 751 prescriptions generated prior to the intervention and 1 015 649 prescriptions generated afterward. The total number of prescriptions generated using the e-prescribing system increased over time as the system was more widely adopted. Over 2000 unique prescribers were identified. All reported percentages are unadjusted.
Table 1.
Electronic prescriptions before and after implementation of decision support on generic availability
| Pre-implementation prescriptions (N=170751) | Post-implementation prescriptions (N=1015649) | Increase in generic prescriptions (% (95% CI)) |
|||
| Total (%) | Generic (%) | Total (%) | Generic (%) | ||
| Prescriber | 65991 (38.6) | 22644 (34.3) | 522196 (51.4) | 307821 (58.9) | 24.6 (24.2 to 25.0) |
| Nurse | 104760 (61.4) | 32200 (30.7) | 493453 (48.6) | 242791 (49.2) | 18.5 (18.2 to 18.8) |
| Anesthesiology | 7797 (4.6) | 2737 (35.1) | 12438 (1.2) | 7041 (56.6) | 21.5 (20.1 to 22.9) |
| EM | 1813 (1.1) | 502 (27.7) | 6406 (0.6) | 3709 (57.9) | 30.2 (27.8 to 32.6) |
| Family practice | 10919 (6.4) | 3015 (27.6) | 68550 (6.7) | 35790 (52.2) | 24.6 (23.7 to 25.5) |
| General surgery | 14060 (8.2) | 3310 (23.5) | 64024 (6.3) | 38300 (59.8) | 36.3 (35.5 to 37.1) |
| Medicine | 50205 (29.4) | 18438 (36.7) | 536722 (52.8) | 297780 (55.5) | 18.8 (18.3 to 19.2) |
| Med/Peds | 922 (0.5) | 342 (37.1) | 14260 (1.4) | 9497 (66.6) | 29.5 (26.3 to 32.7) |
| Neurology | 6487 (3.8) | 1588 (24.5) | 38424 (3.8) | 15920 (41.4) | 17.0 (15.8 to 18.1) |
| Neurosurgery | 74 (0.0) | 11 (14.9) | 6289 (0.6) | 2829 (45.0) | 30.1 (21.9 to 38.3) |
| OB/GYN | 12008 (7.0) | 3539 (29.5) | 32350 (3.2) | 18998 (58.7) | 29.3 (28.3 to 30.2) |
| Ophthalmology | 1537 (0.9) | 568 (37.0) | 2395 (0.2) | 1272 (53.1) | 16.2 (13.0 to 19.3) |
| Oral surgery | 344 (0.2) | 92 (26.7) | 8452 (0.8) | 6215 (73.5) | 46.8 (42.0 to 51.6) |
| Orthopedics | 2876 (1.7) | 983 (34.2) | 31270 (3.1) | 16408 (52.5) | 18.3 (16.5 to 20.1) |
| Otolaryngology | 1116 (0.7) | 161 (14.4) | 12692 (1.2) | 5648 (44.5) | 30.1 (27.8 to 32.3) |
| Pathology | 1107 (0.6) | 76 (6.9) | 2269 (0.2) | 451 (19.9) | 13.0 (10.8 to 15.2) |
| Pediatrics | 22145 (13.0) | 7772 (35.1) | 109770 (10.8) | 56483 (51.5) | 16.4 (15.7 to 17.1) |
| Plastic surgery | 31 (0.0) | 2 (6.5) | 5910 (0.6) | 4077 (69.0) | 62.5 (53.8 to 71.3) |
| Psychiatry | 23388 (13.7) | 7563 (32.3) | 47907 (4.7) | 23311 (48.7) | 16.3 (15.6 to 17.1) |
| Rad Onc | 6579 (3.9) | 1658 (25.2) | 9760 (1.0) | 3611 (37.0) | 11.8 (10.4 to 13.2) |
| Radiology | 7343 (4.3) | 2487 (33.9) | 5761 (0.6) | 3272 (56.8) | 22.9 (21.3 to 24.6) |
EM, emergency medicine; Med/Peds, medicine/pediatrics; OB/GYN, obstetrics and gynecology; oral surgery, oral & maxillofacial surgery; Rad Onc, radiation oncology.
The departments of medicine, pediatrics, family practice, and general surgery generated 75% of the total 1 186 400 e-prescriptions. Overall, the proportion of generic prescribing increased 22.1%, with a greater increase for providers than nurses. Generic prescribing increased significantly in every specialty.
Figure 3 and table 1 report the effects of our intervention on prescribing behavior. Generic medications made up 32.1% of all electronic prescriptions prior to the intervention. This percentage increased to 54.2% afterward (22.1% increase, 95% CI 21.9% to 22.3%).
Figure 3.
Monthly proportion of generic prescriptions before and after implementation of generic substitution decision support. Use of the e-prescribing system and number of e-prescriptions (open circles) increased with time. Proportion of generic e-prescriptions increased 22.1% after the system implementation date (day 451). The proportion of non-e-prescribing generic prescriptions (crosses) remained consistently and significantly lower.
After the decision support on generic availability was implemented, 59% of prescriber prescriptions were generic, versus 49% of nurse-generated prescriptions (adjusted OR=1.52, 95% CI 1.37 to 1.68). There was a higher increase in generic prescribing rates among authorized prescribers (24.6%) than nurses (18.5%; adjusted ratio of ORs=1.38, 95% CI 1.17 to 1.63).
There was a significant increase in generic medication ordering behavior among providers in all 19 departments studied, with the largest increase in the surgical specialties. Five of the 10 departments with the largest increases were surgical departments. The department of medicine was the highest user of e-prescribing, accounting for 50% of all prescriptions in the study. This figure was nearly five times more than that of the next department (pediatrics, 11%). These two departments accounted for 61% of all prescriptions. Both departments had a high overall initial generic prescribing rate (36.7% and 35.1%, respectively) and a lower increase in the proportion of generic medication prescribing using the updated interface. Medicine increased by 18.8%, and pediatrics increased by 16.4%. However, the combined proportion of generic prescribing in both departments using the updated interface exceeded the proportion in all other departments (54.8% vs 53.2%; adjusted OR=1.07, 95% CI 0.97 to 1.17). Pathology, radiation oncology, and neurology had the lowest final rates of generic prescribing, and the lowest percentage changes (13.0%, 11.8%, and 17.0%, respectively). Across all departments, the increase in the proportions of generic prescribing varied from 11.8% to 62.5%. The associated precisions (half length of the 95% CI) ranged from 0.45% to 8.75%.
The proportion of generic e-prescribing rose 6% in the month immediately prior to the decision support implementation (figure 3). This period was consistent with the time that the updated interface was piloted in an internal medicine clinic to assess system stability. The pilot clinic data were included in the pre-implementation period analysis because identification of prescribers' clinic was not available in the dataset.
The proportion of generic prescriptions was similar for hand-generated and electronic prescriptions before generic substation decision support was implemented. The proportion of generic prescriptions was significantly higher in the electronic prescription group after the system changes. The ‘pre-implementation period’ was November 1, 2005–November 7, 2005, the ‘immediate post-implementation period’ was November 1, 2006–November 7, 2006, and the ‘end-of-study post-implementation period’ was September 1, 2008–September 30, 2008.
As shown in table 2, there was no significant difference between RxStar and non-RxStar prescriptions in the pre-implementation period (32.4% vs 29.3%; p=0.07). The difference became significant in the immediate post-implementation period (50.3% vs 31.4%; p<0.0001) and continued to increase in the end-of-study post-implementation period (58.1% vs 37.4%; p<0.0001). The proportion of non-RxStar generic prescribing was not significantly different between the pre-implementation and immediate post-implementation periods (29.3% vs 31.4%; p=0.224). The proportion of non-RxStar generic prescribing rose from the pre-implementation period to the end of the study (29.3% vs 37.4%; p<0.0001); however, the increase in RxStar generic prescribing was significantly greater in the immediate post-implementation (15.7%, 95% CI 11.6% to 19.9%) as well as end-of-study post-implementation periods (17.4%, 95% CI 13.2% to 21.5%).
Table 2.
Electronic and hand-generated prescriptions before and after implementation of generic substitution decision support
| Total | Generic | Percent generic (95% CI) | |
| Electronic | |||
| Pre-implementation period | 1707 | 553 | 32.4 (30.2% to 34.7%) |
| Immediate post-implementation period | 6505 | 3269 | 50.3 (49.0% to 51.5%) |
| End-of-study post-implementation period | 24894 | 14470 | 58.1 (57.5% to 58.7%) |
| Hand-generated | |||
| Pre-implementation period | 1490 | 437 | 29.3 (27.0% to 31.6%) |
| Immediate post-implementation period | 1527 | 480 | 31.4 (29.1% to 33.8%) |
| End-of-study post-implementation period | 1439 | 538 | 37.4 (34.9% to 39.9%) |
We examined statin prescriptions to assess any learning effect that might have resulted in within-class substitutions following our intervention, as shown in figure 4. The proportion of Zocor prescriptions fell dramatically after system implementation and was associated with a concomitant rise in the proportion of simvastatin prescriptions; we saw a similar trend with Pravachol/pravastatin, and essentially an unchanged rate of lovastatin prescriptions (with virtually no prescriptions for its branded form). The proportion of Lipitor prescriptions began to decrease steadily when simvastatin became commercially available and continued to decline after system implementation (p=0.00007) although without the dramatic change seen with other statins.
Figure 4.
Monthly volume-adjusted proportion of statin prescriptions before and after implementation of generic substitution decision support. The proportion of commercially available generic statin equivalents increased dramatically after the system implementation date. A slight within-class effect was observed for the brand-only statin, Lipitor, without any intervention to directly recommend a within-class generic alternative.
Discussion
Adding reminders about the availability of generic medications to the user interface of an e-prescribing system resulted in a dramatic and sustained improvement in the proportion of generic formulations written using the system. This change improved the generic medication prescribing rate in every department. Although increases were seen in all 19 departments, they were less dramatic in three. This result caused increased variance across departments before and after the e-prescribing intervention. In two of these departments, radiation oncology and neurology, it is likely that providers were appropriately prescribing brand name medications, even when generic medications were suggested, given recent data about the potential risks of substituting generic medications in some settings.35–37
Novelty, as well as learning and adaptation by providers, likely contributed to the rise in proportion of generic prescriptions immediately after the intervention. After a dramatic increase to >65%, the proportion of generic prescriptions decreased to 50–60%, where it remained (figure 3). Since the intervention provided a new way of displaying medications, a novelty effect would increase the rate of users selecting generic formulations. Additionally, providers who desired to prescribe brand name medications may have unintentionally selected the generic formulation after searching for a brand name medication. Displaying generic medication names along with corresponding brand name medication equivalents might have an educational effect. The system implies that generic medications are preferable to brand name drugs by listing generic medications first. This subtle change may ultimately encourage prescribers to think of and use medications in generic, rather than brand name, form. We observed a slight within-class effect for Lipitor, a brand-only statin, without any intervention to directly recommend a within-class generic alternative. An educational effect may also enhance prescribers' substitution behavior even without explicit substitution recommendations. While it is not the major focus of our study, this observation is intriguing and should be the topic of future research. Other educational efforts have improved generic medication prescribing by about 10%.27 28 38 39 However, none have had as large an impact on prescribing behavior as the intervention in this study.
It has been demonstrated that changes in human/computer interfaces may improve clinician performance. For example, seminal research by McDonald40 noted that computer-provided suggestions altered behavior. McDonald's study also noted the importance of sustaining these behavior changes by automating decision support. More recently, a study by Miller and colleagues41 proposed a framework for determining how to implement a decision-support feature into an order-entry system. The study evaluated the type of intervention to create, its optimal location in the workflow, and the level of disruption appropriate for the feature. Our intervention followed Miller's framework closely, and may provide support for others who wish to implement decision support into the prescribing workflow.
Despite the improvements, our results should be interpreted with respect to some methodological limitations. First, the e-prescribing system contains two features that help to encourage the continuation of previous prescribing behavior, potentially underestimating the impact of the intervention. All prescribers have a ‘favorites’ menu that allows them to quickly prescribe medications they prescribe frequently. All patient medications are saved explicitly so that future prescriptions can be refilled with a few clicks. If a prescriber had stored a brand name medication in a favorites list or if patients had previously been prescribed brand name medications, the intervention would not be as likely to have an immediate impact on prescribing behavior. From the standpoint of methodological limitations, the study is observational and used a limited concurrent control. The intervention was driven by a real-world directive to increase generic prescribing and the effect was analyzed post hoc. Although there was no centralized quality improvement effort to improve e-prescribing, clinic-level or department-wide efforts may have been underway. It is therefore reassuring that the analysis showed a prescriber-wide impact associated with the user interface changes. While we cannot rule out the possibility that other factors influenced prescribing behavior during the time that prescribing patterns were observed, we would expect that these factors would have had a continuous effect on the proportion of generic prescriptions. The abrupt and large change in this proportion that occurred immediately after the intervention was implemented is difficult to attribute to factors other than the intervention. Furthermore, a review of non-RxStar prescriptions written during three periods of the study revealed a significantly higher proportion of generic prescribing in prescriptions written using the e-prescribing system compared with non-RxStar-generated prescriptions after implementation of generic substitution decision support. While non-RxStar generic prescribing increased slightly during the study, RxStar generic prescribing increased a significantly greater amount. The increase in non-RxStar generic prescribing may have been due to an educational effect of the system on users who sometimes hand-write prescriptions, or related to documentation left by RxStar in the electronic problem list after patients were switched to generic formulations because of the intervention. If other factors beyond the intervention influenced the change in generic prescribing behavior, these changes should have been equally observed in both RxStar and non-RxStar prescriptions.
A second limitation of the study is that it does not control for the emergence of new generic medications during the time of the study. This limitation likely did not affect the study outcome, since new generic formulations became available in both the pre- and post-intervention periods, but generic prescribing increased only after the day 419 intervention. Frequently prescribed medications that became available as generic formulations during the pre-intervention period (days 0–419) included azithromycin, simvastatin, ondansetron, and itraconazole.42 Generic medications that became available during the post-intervention period (days 419–1187) include zolpidem, paroxetine, cetirazine HCl, and amlodipine besylate.42 In addition, the effect we saw might be specific to Vanderbilt, to RxStar, or to other factors such as a higher starting rate of brand name medication prescribing.
Despite the above limitations, our results reveal that generic substitution decision support can significantly increase the generic e-prescribing rate. Generic medications cost US$45 less than brand name medications, on average, and patients typically save about US$10 per generic prescription because of lower copayments.43 The potential savings for patients and payers as a result of the increased generic prescribing demonstrated in this study could be significant. Additionally, e-prescribing decision support could help providers realize significant pay-for-performance incentives by meeting generic prescribing benchmarks. A formal evaluation of the economic impact of decision support in e-prescribing systems, accounting for actual fill rates, variations in generic and brand name medication costs, and differences in patient copayments, pay-for-performance incentives, and downstream effects, should be included in future studies. Furthermore, our findings support ongoing research by the Agency for Healthcare Research and Quality and the Office of the National Coordinator for Health Information. While further study is needed, we believe that e-prescribing decision support will be a valuable method for improving providers' adherence to prescribing guidelines across multiple settings and should be considered by institutions and practices trying to meet ‘meaningful use' and pay-for-performance goals.
Conclusion
This study demonstrates a positive impact of e-prescribing decision support for generic prescribing and supports the use of electronic tools to improve prescribing safety and quality. Additional studies are needed to demonstrate the impact of e-prescribing decision support in multiple institutions, using multiple electronic systems, and including physicians in a variety of practice settings.
Acknowledgments
We thank Randolph A Miller, MD and William D Dupont, PhD, for their critical reading and suggestions for this article. We thank Ron Eatherly, DPh, and the outpatient pharmacy staff for their help obtaining written prescriptions for review. We also thank Christopher Ryland for his assistance with the background literature search and Anna Rezunenko, MS, for her help obtaining data and images from RxStar. None of the above received compensation for their contributions.
Footnotes
Funding: SPS was funded by grant #5 T15 LM007450-07 from the National Library of Medicine.
Competing interests: None.
Contributors: Conception and design: SPS, KBJ. Analysis and interpretation of the data: SPS, QC, KBJ. Drafting of the article: SPS, QC, KBJ. Critical revision of the article for important intellectual content: SPS, KBJ. Final approval of the article: SPS, KBJ. Provision of study materials or patients: KBJ. Statistical expertise: QC, KBJ. Administrative, technical, or logistic support: KBJ. Collection and assembly of data: SPS, KBJ.
Provenance and peer review: Not commissioned; externally peer reviewed. Dr Randolph A Miller did not participate in the peer review of this manuscript.
References
- 1.IMS Health IMS Health Reports U.S. Prescription Sales Grew 3.8 Percent in 2007, to $286.5 Billion. Press Release 2008. March 12 [Google Scholar]
- 2.Keehan S, Sisko A, Truffer C, et al. Health spending projections through 2017: the baby-boom generation is coming to Medicare. Health Aff (Millwood) 2008;27:145–55 [DOI] [PubMed] [Google Scholar]
- 3.National Association of Chain Drug Stores Table 151. Retail Prescription Drug Sales. NACDS Foundation Chain Pharmacy Industry Profile, 2007. http://www.census.gov/compendia/statab/tables/09s0151.xls (accessed 16 Jun 2009).
- 4.IMS Health The United States is also the world's largest consumer of prescription drugs, accounting for almost half of global pharmaceutical sales in 2007. Global Pharmaceutical Sales by Region 2007, 2008 [Google Scholar]
- 5.Weisbart E. Taming pharmacy: driving out waste one consumer at a time. Express scripts, 2008. http://personnel.ky.gov/NR/rdonlyres/36B1DA8B-7F0B-4A48-BA1E-73D7BDC436B7/0/ExpressScriptsPresentation0508.pdf (accessed 16 Jun 2009).
- 6.Haas JS, Phillips KA, Gerstenberger EP, et al. Potential savings from substituting generic drugs for brand-name drugs: medical expenditure panel survey, 1997–2000. Ann Intern Med 2005;142:891–7 [DOI] [PubMed] [Google Scholar]
- 7.Schoen C, Osborn R, Doty MM, et al. Toward higher-performance health systems: adults' health care experiences in seven countries, 2007. Health Aff (Millwood) 2007;26:w717–34 [DOI] [PubMed] [Google Scholar]
- 8.Shrank WH, Hoang T, Ettner SL, et al. The implications of choice: prescribing generic or preferred pharmaceuticals improves medication adherence for chronic conditions. Arch Intern Med 2006;166:332–7 [DOI] [PubMed] [Google Scholar]
- 9.American Medical Association Report 2 of the Council on Science and Public Health (A-07). 2007. http://www.ama-assn.org/ama/no-index/about-ama/17730.shtml (accessed 16 Jun 2009).
- 10.Pham HH, Alexander GC, O'Malley AS. Physician consideration of patients' out-of-pocket costs in making common clinical decisions. Arch Intern Med 2007;167:663–8 [DOI] [PubMed] [Google Scholar]
- 11.Federman AD, Halm EA, Siu AL. Use of generic cardiovascular medications by elderly Medicare beneficiaries receiving generalist or cardiologist care. Med Care 2007;45:109–15 [DOI] [PubMed] [Google Scholar]
- 12.Shrank WH, Stedman M, Ettner SL, et al. Patient, physician, pharmacy, and pharmacy benefit design factors related to generic medication use. J Gen Intern Med 2007;22:1298–304 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kohl H, Shrank WH. Increasing generic drug use in Medicare Part D: the role of government. J Am Geriatr Soc 2007;55:1106–9 [DOI] [PubMed] [Google Scholar]
- 14.Madden JM, Graves AJ, Zhang F, et al. Cost-related medication nonadherence and spending on basic needs following implementation of Medicare Part D. JAMA 2008;299:1922–8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Purvis L. Insight on the Issues: Strategies to Increase Generic Drug Utilization and Associated Savings, Vol 16 Washington DC: AARP Public Policy Institute, 2008 [Google Scholar]
- 16.Fischer MA, Vogeli C, Stedman M, et al. Effect of electronic prescribing with formulary decision support on medication use and cost. Arch Intern Med 2008;168:2433–9 [DOI] [PubMed] [Google Scholar]
- 17.Medco Growing confidence in generic drugs may help you reduce prescription drug costs. Medco Monitor 2005;1:1–2 [Google Scholar]
- 18.Waber RL, Shiv B, Carmon Z, et al. Commercial features of placebo and therapeutic efficacy. JAMA 2008;299:1016–17 [DOI] [PubMed] [Google Scholar]
- 19.Shrank WH, Agnew-Blais J, Choudhry NK, et al. The variability and quality of medication container labels. Arch Intern Med [Research Support, Non-U.S. Gov't] 2007;167:1760–5 [DOI] [PubMed] [Google Scholar]
- 20.Wolf MS, Davis TC, Shrank W, et al. To err is human: patient misinterpretations of prescription drug label instructions. Patient Educ Couns 2007;67:293–300 [DOI] [PubMed] [Google Scholar]
- 21.Wolf MS, Davis TC, Tilson HH, et al. Misunderstanding of prescription drug warning labels among patients with low literacy. Am J Health-Syst Pharm 2006;63:1048–55 [DOI] [PubMed] [Google Scholar]
- 22.Kimberlin CL, Winterstein AG. Expert and Consumer Evaluation of Consumer Medication Information-2008. Final Report to the U.S. Department of Health and Human Services and the Food and Drug Administration. http://www.fda.gov/AboutFDA/CentersOffices/CDER/ReportsBudgets/ucm163777.htm (accessed 28 Sep 2010).
- 23.Shrank WH, Avorn J. Educating patients about their medications: the potential and limitations of written drug information. Health Aff [Research Support, Non-U.S. Gov't] 2007;26:731–40 [DOI] [PubMed] [Google Scholar]
- 24.Wolf MS, Davis TC, Shrank WH, et al. A critical review of FDA-approved Medication Guides. Patient Educ Couns 2006;62:316–22 [DOI] [PubMed] [Google Scholar]
- 25.Barrett L. Physicians' Attitudes and Practices Regarding Generic Drugs. AARP Knowledge Management, Mar 2005. http://assets.aarp.org/rgcenter/health/phys_generic.pdf (accessed 16 Jun 2009).
- 26.Raffaele M. States combat drug reps to cut costs. Washington Post 2008. March 2 [Google Scholar]
- 27.Bielby J, Silagy E. Trials of providing costing information to general practitioners: a systematic review. Med J Aust 1997;167:89–92 [DOI] [PubMed] [Google Scholar]
- 28.Wadland WC, Farquhar L, Priester F, et al. Increasing generic prescribing: a resident educational intervention. Fam Med 2005;37:259–64 [PubMed] [Google Scholar]
- 29.Ross SM, Papshev D, Murphy EL, et al. Effects of electronic prescribing on formulary compliance and generic drug utilization in the ambulatory care setting: a retrospective analysis of administrative claims data. J Manag Care Pharm 2005;11:410–15 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Lyman JA, Conaway M, Lowenhar S. Formulary access using a PDA-based drug reference tool: does it affect prescribing behavior? AMIA Annu Symp Proc 2008:1034. [PubMed] [Google Scholar]
- 31.U.S. House of Representatives Ways and Means Committee Congress 111, Session 1. A Bill to Provide for a Portion of the Economic Recovery Package Relating to Revenue Measures, Unemployment, and Health, 2009:138–328 http://waysandmeans.house.gov/media/pdf/110/sbill.pdf (accessed 16 Jun 2009).
- 32.Langston Consider e-Prescribing as One Step in Climb to Health IT. American Medical News 2008. April 7 [Google Scholar]
- 33.Johnson KB, Feldman MJ. Medical informatics and pediatrics. Decision-support systems. Arch Pediatr Adolesc Med 1995;149:1371–80 [DOI] [PubMed] [Google Scholar]
- 34.Johnson KB, Fitzhenry F. Case report: activity diagrams for integrating electronic prescribing tools into clinical workflow. J Am Med Inform Assoc 2006;13:391–5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Rodriguez MJ, Diaz S, Vera-Llonch M, et al. Cost-effectiveness analysis of pregabalin versus gabapentin in the management of neuropathic pain due to diabetic polyneuropathy or post-herpetic neuralgia. Curr Med Res Opin 2007;23:2585–96 [DOI] [PubMed] [Google Scholar]
- 36.Duh MS, Andermann F, Paradis PE, et al. The economic consequences of generic substitution for antiepileptic drugs in a public payer setting: the case of lamotrigine. Dis Manag 2007;10:216–25 [DOI] [PubMed] [Google Scholar]
- 37.Heaney DC, Sander JW. Antiepileptic drugs: generic versus branded treatments. Lancet Neurol 2007;6:465–8 [DOI] [PubMed] [Google Scholar]
- 38.Kim CS, Kristopaitis RJ, Stone E, et al. Physician education and report cards: do they make the grade? Results from a randomized controlled trial. Am J Med 1999;107:556–60 [DOI] [PubMed] [Google Scholar]
- 39.O'Brien M A, Rogers S, Jamtvedt G, et al. Educational outreach visits: effects on professional practice and health care outcomes. Cochrane Database Syst Rev 2007;4:CD000409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.McDonald CJ. Protocol-based computer reminders, the quality of care and the non-perfectability of man. N Engl J Med 1976;295:1351–5 [DOI] [PubMed] [Google Scholar]
- 41.Miller RA, Waitman LR, Chen S, et al. The anatomy of decision support during inpatient care provider order entry (CPOE): empirical observations from a decade of CPOE experience at Vanderbilt. J Biomed Inform 2005;38:469–85 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.International Association of Generic & Innovative Drug Manufacturers Drugs off-patent reports 2000, 2001. http://www.locumusa.com/pdf/members/100m+00.pdf (accessed 16 Jun 2009).
- 43.Express Scripts I. Express Scripts, Inc Geographic variation in generic fill rate. http://www.express-scripts.com/research/studies/healthservicesresearch/pharmacoepidemiology/docs/regionalgenericvariation.pdf (accessed 1 Jul 2010).