Abstract
Personal health records (PHRs) are information repositories; however, PHRs may be less available to persons in the safety net setting. We deployed a free, secure, internet-based PHR for persons receiving care at the AIDS/HIV clinic at San Francisco General Hospital. In our initial rollout, 221 persons registered for the PHR. Compared to the entire clinic, these initial users were more likely to be Caucasian, male, non-Hispanic, on antiretroviral medications, and have better control of their HIV infection. The median number of online sessions was 7 and the median session length was 4 min. Laboratory results were the most commonly accessed feature. Patients were satisfied with the PHR and more than 80% of users agreed that the PHR helped them manage their medical problems; however, some users were concerned that their health information was not accurate or secure. Patients in a safety net setting will access and use an online PHR.
Case description
Personal health records (PHRs) are used to share health information, increase health understanding, enhance engagement between patients and their providers and health organizations, and ultimately may contribute to improved personal health.1 2 The high degree of interest in PHRs is in part due to the importance of sharing health information among organizations and providers.3 4 Accurate PHRs eventually may impact health outcomes.5 Recently, consumer-oriented software companies have begun developing PHR applications, generating significant interest among health organizations and their patients.6 7
PHRs are a component of health information technology and are a tool for consumers seeking to organize their health information.8–11 An idealized PHR should retrieve comprehensive information from multiple sources and should enable patients to share their health information.12 The information in a PHR must be secure, portable, and understandable, and allow patients to obtain the best possible advice and services. One concern is that patients in the safety net setting with poor internet access and limited health literacy will not have access to PHRs and thus may not benefit from their use.13–16 We developed a PHR for HIV/AIDS patients at San Francisco General Hospital (SFGH), a public hospital, to understand the extent that this technology would be used and to investigate the patterns of use.
Example and observations
myHERO is a secure online PHR (https://myhero.sfdph.org) established for persons with HIV/AIDS at UCSF AIDS Clinic at SFGH (screens available in supplementary material at http://jamia.bmj.com). Data in the personal health record are automatically populated from HERO (Healthcare Electronic Record Organizer), the electronic medical record (EMR) system used in the HIV/AIDS clinic. Developed by members of the SFGH AIDS Program, HERO is a secure web-based application that allows clinicians to document and verify demographics, diagnoses, medications, and laboratory data and uses Health Level-7 to exchange information with outside information systems. All information entered into HERO is submitted through a local intranet for storage in a relational database. Data in myHERO are populated automatically from HERO and include lists of active diagnoses, medications, laboratory values (following a 10-day delay to allow clinician review prior to patient access), drug allergies, scheduled clinic visits, and tools to promote healthcare maintenance. Explanations of laboratory data and normal ranges are provided alongside the laboratory values listed by clinic visit date. In an effort to provide the most valuable laboratory values to patients and after patient and clinician interviews regarding the laboratory studies of greatest importance to patients, we decided to display CD4-T lymphocytes, HIV plasma viral load, hemoglobin, total cholesterol, high density lipoprotein, low density lipoprotein, triglycerides, serum creatinine, serum alanine aminotransferase, and aspartate aminotransferase. Problem lists and medications are linked to the National Library of Medicine's MedlinePlus (http://medlineplus.gov) and, when available, images of the medications (jpeg) are included. Patients may enter their blood pressure, serum glucose, and weight or record private notes in myHERO. The application provides online help, a weekday help desk accessible by phone, and links to the clinic and to community support and information. myHERO was built using the .NET Framework (version 2.0, Microsoft) a software development technology that enables developers to create dynamic web applications. Data from myHERO users are retrieved from the websites' log records and are merged with HERO SQL server information and extracted for analysis.
A session tracking tool was launched after myHERO was initiated. This tool measured online PHR usage via computer log files. The tracking tool recorded session start and end times and the viewed myHERO pages for each session. In September 2008, a 25-item evaluation survey was added to myHERO. The survey appeared when users viewed their PHR. In addition, we sent users three email requests asking them to complete the survey. No inducement to complete the survey was offered. The survey was patterned after commonly used Likert-response satisfaction questionnaires.17 18 It asked users to rate the helpfulness of 13 site features with response scale of 1=did not use, 2=not helpful at all, 3=a little helpful, 4=somewhat helpful, and 5=very helpful. Five additional questions asked patients to agree or disagree about the completeness and accuracy of myHERO information with a response scale of 1=do not know, 2=strongly disagree, 3=disagree, 4=agree, and 5=strongly agree. Patients were also asked to agree or disagree with statements that myHERO was easy to access, easy to navigate, supported participation in their own care by improving management of medical problems, prepared them for their clinic visit, helped them take charge of their healthcare, maintained confidentiality, and allowed for information sharing. Free text comments were also elicited.
Beginning in March 2007, patients with primary care appointments at the SFGH HIV/AIDS clinic were invited by their clinicians (physicians and nurse practitioners) to establish access to myHERO via an online account. As needed, patients were helped to acquire an email address, taught how to access the internet, and provided addresses of locations offering free web access (eg, public libraries). Many patients were unfamiliar with email. We offered an email account with Yahoo, Gmail, MSN, and other service providers. We found that patients selected Yahoo as the preferred email service due to easier to understand questions for forgotten identification or password. Remembering passwords and identification for new email users became a significant issue for some PHR users.
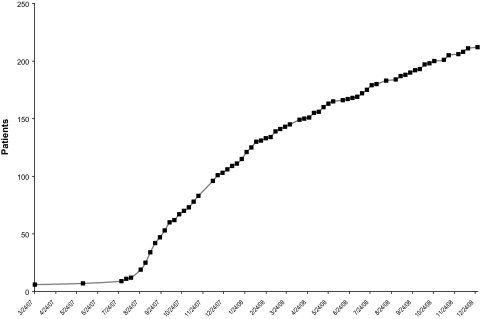
From March 2007 through December 2008, 3760 patients had a primary care appointment at San Francisco General Hospital's AIDS clinic, of whom 221 registered for online access to their personal health record and 211 activated their account (figure 1). There was no inducement, other than the availability of the online information, to influence a person to register, activate, or view their online personal health record. We considered that patients with increasing internet involvement would be more likely to use the system and so we categorized patients in the clinic into categories with higher levels of recorded technical proficiency: (1) patients who did not have or did not provide an email address; (2) patients who provided an email address but did not register for myHERO; and (3) patients who registered for myHERO. We contrast the three groups with respect to demographic characteristics and HIV-related disease characteristics, and we test for trends across groups using 1-degree-of-freedom χ2 tests (Mantel–Haenszel test for discrete characteristics; Wald test for continuous characteristics). For each tracked PHR user, we define “session count” as the number of distinct PHR sessions; “months of PHR use” is defined as the difference between the user's first and most recent month of access (plus 1); and “usage rate” as the user's session count divided by months of PHR use. We use a Poisson model and Pearson goodness-of-fit statistic (reported as χ2 divided by degrees of freedom) to evaluate variation in the usage rate by months of PHR use and we summarize the monthly usage rates via medians and interquartile ranges. Similarly, we summarize the median session duration per patient via a Poisson model and via medians and interquartile ranges, overall and by months of PHR use. In addition, we report the frequency of individually viewed PHR pages. This project was granted an exemption certification (#0833272) by the University of California Committee for Human Research (the Investigational Review Board at UCSF) and was approved by the Privacy Board of the San Francisco Department of Public Health.
Figure 1.
Total number of activated personal health record users.
Patients in the clinic were categorized by increasing level of online access to health information (a surrogate for technical proficiency) as follows: 3061 clinic patients without or have not provided an email address, 478 patients with an email address but did not register for myHERO, and 221 persons registered users of myHERO (see supplementary material). As online access increased, patients were younger (less than 40 years old: 29%, 43%, 37%, respectively), more often male (81%, 95%, 95%, respectively), more often Caucasian (51%, 66%, 78%, respectively), and less often Hispanic (26%, 26%, 15%, respectively). Although an AIDS diagnosis was equally common among all subgroups, myHERO users were most likely to be receiving antiretroviral agents and had better health status in terms of lower HIV plasma RNA values (undetectable: 51%, 53%, 65%, respectively) and CD4 cell counts (below 250 cells/ml: 27%, 20%, 17%, respectively).
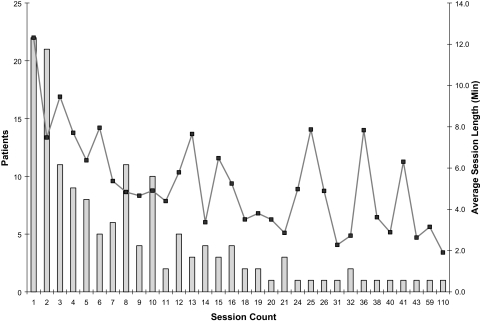
Among the 136 patients who used myHERO during the tracking period, the median months of myHERO use was 6 ((25%, 75%)=(3, 8)), and the median session count was 7 ((25%, 75%)=(2, 13); (min, max)=(1, 109)). myHERO usage rate did not vary with the number of months of PHR use (Poisson mean, 2.0; 95% CI 1.8 to 2.3) sessions/month). The median session length was 4 min ((25%, 75%)=(2, 6.5)), and was longer for inexperienced users than for experienced users (figure 2).
Figure 2.
Total number of sessions per user and time for each session.
In our experience, laboratory results were the most commonly viewed PHR feature, with 2044 separate visits to the summary page by 136 users (table 1). The single most commonly viewed laboratory value was CD4 cell results (891 visits by 110 persons) and then HIV RNA plasma value results (542 visits by 104 persons). The laboratory values were a source of frustration because of our policy to publish laboratory values 10 days after they appear in the EMR. Initially the time frame was 30 days and moved to 10 days. In our experience and observation, patients would like the values to be simultaneously populated in the PHR and the EMR. Office visit lists were viewed 719 times by 117 persons, medical conditions 441 by 107 persons, and medications 366 times by 107 patients. Features for recording weight, blood pressure, and blood glucose were also utilized. The feature that allowed patients to enter comments was accessed the least. Provider profiles were the most accessed clinic information page.
Table 1.
Number of times specific personal health record (PHR) pages were accessed (N=136 patients)*
| Page description | % (no.) of patients accessing PHR page | No. of times PHR page accessed | No. of times accessed per patient |
| Personal medical information | |||
| Laboratory results | |||
| Summary page | 96% (131) | 2044 | 15.6 |
| CD4/T-cell count | 81% (110) | 891 | 8.1 |
| Viral load | 76% (104) | 542 | 5.2 |
| Total cholesterol | 65% (88) | 274 | 3.1 |
| LDL cholesterol | 54% (73) | 209 | 2.9 |
| HDL cholesterol | 51% (69) | 202 | 2.9 |
| Triglycerides | 55% (75) | 199 | 2.7 |
| Creatinine | 55% (75) | 241 | 3.2 |
| Hemoglobin | 55% (75) | 236 | 3.1 |
| AST | 51% (70) | 224 | 3.2 |
| ALT | 46% (62) | 170 | 2.7 |
| Other personal information | |||
| Scheduled visits | 86% (117) | 719 | 6.1 |
| Medical conditions | 79% (107) | 441 | 4.1 |
| Current medications | 74% (107) | 366 | 3.6 |
| Allergies | 58% (79) | 180 | 2.3 |
| Medication refill | 18% (25) | 153 | 6.1 |
| Pages for patient to record information | |||
| Blood pressure record | 74% (100) | 237 | 2.4 |
| Weight record | 68% (93) | 227 | 2.4 |
| Glucose record | 62% (84) | 177 | 2.1 |
| Personal notes record | 51% (69) | 164 | 2.4 |
| General information | |||
| Clinic information | |||
| Provider profiles | 34% (46) | 462 | 10.0 |
| Clinic services | 22% (30) | 62 | 2.1 |
| General information | 16% (22) | 30 | 1.4 |
| Help links | |||
| Local resources | 13% (17) | 52 | 3.1 |
| HIV resources | 8% (11) | 17 | 1.5 |
| Addiction resource | 5% (7) | 16 | 2.3 |
April 21, 2008 through December 31, 2008.
Among the 136 persons for whom we tracked session usage, 51 (38%) completed the survey (table 2). There were no significant demographic or HIV-related differences between persons completing or not completing the survey (data not shown). The number of missing individual items ranged from 0 to 4. The most commonly used page contained laboratory values (50; 98% of respondents), lists of medical conditions (45; 94% of respondents), medication list (42; 88% of respondents), and links to information about their health conditions (41; 80% of respondents). Links to health conditions, links to community and other resources, and the laboratory results were reported to be useful by 80–90% of patients. Over two-thirds of patients agreed that the information provided was complete and accurate, though a substantial number reported that they believed there were inaccuracies in current medications (25%) and in medical conditions (32%). Over 90% of patients agreed that navigation of myHERO was easy, though somewhat fewer (84%) agreed that the same was true with regard to accessing the myHERO website. More than 80% of users agreed that myHERO helped them manage their medical problems, prepared them better for their visits, and helped them take charge of their healthcare. Thirty-one percent did not agree that the information was confidential. The reasons for the lack of confidentiality were not captured. Overall, 71% of patients reported being satisfied or very satisfied with myHERO. Thirty-one comments were provided by 19 users. The most common critical comment was that the laboratory results were not up to date and the lists of medical conditions and medications were incomplete or inaccurate.
Table 2.
Results from personal health record (PHR) user survey (N=51)
| PHR feature | % (no.) reporting having accessed feature | % (no.) reporting feature to be helpful* | PHR function | % (no.) reporting agreement† |
| Helpfulness of information | Complete and accurate | |||
| List of laboratory results | 98% (49) | 88% (43) | List of allergies | 87% (34) |
| List of medical conditions | 94% (45) | 69% (31) | Laboratory results | 81% (39) |
| List of current medications | 88% (42) | 74% (31) | List of medications | 75% (33) |
| Links to information about conditions | 80% (41) | 81% (33) | List of medical conditions | 68% (30) |
| Information on positive health program | 69% (35) | 71% (25) | Easy to use | |
| Links to community resources | 59% (30) | 90% (27) | Easy to navigate | 92% (45) |
| Self-monitor weight | 56% (28) | 68% (19) | Easy to access | 84% (42) |
| Self-monitor glucose | 53% (27) | 67% (18) | Supports self-management | |
| List of allergies | 51% (26) | 73% (19) | Allows sharing information | 92% (34) |
| Refill requests | 49% (25) | 72% (18) | Helps managing medical problems | 87% (41) |
| Self-monitor blood pressure | 49% (24) | 42% (10) | Makes me better prepared for visits | 83% (40) |
| View appointment schedule | 48% (23) | 74% (17) | Helps me take charge | 83% (38) |
| Private notes | 38% (18) | 72% (13) | Information is confidential | 95% (35) |
Helpful includes “very helpful” and “somewhat helpful”; it excludes “a little helpful” and “not at all helpful”.
Agreement includes “strongly agree” and “agree”; it excludes “I don't know”, “disagree”, and “strongly disagree”.
Discussion
A secure, portable, and internet-based personal health record was initiated and used by HIV/AIDS patients receiving care at San Francisco General Hospital. This is the first reported use of a PHR in the safety net setting to detail the extent of patient access to the information in a PHR, including the number of sessions per user, the duration of the sessions, and patient satisfaction with their online PHR. We observed a steady increase in the number of patients with a PHR account although we offered no inducements for establishing the online PHR. Patients who used myHERO were more likely to be male, Caucasian, and non-Hispanic, and to be receiving antiretroviral medications, to have higher CD4 cells, and lower HIV viral load; however, the incidence of AIDS was not different among PHR users, non-PHR users, or persons without an email address. We observed that our patients were capable and desired a PHR to be a convenient tool of information exchange. Providing patients with an email address provided a barrier for some patients and Yahoo! tended to be the preferred service provider for new email users. Forgotten passwords for access to the PHR and email service were the most common sources of patient frustration and the most common reason for patients to access our help desk.
Overall, patients found myHERO useful, particularly for laboratory results, medication lists, medical conditions lists, and links to resources of information. Reported usefulness was somewhat limited by delays of laboratory results populating myHERO and a surprising number of inaccuracies in medications and medical conditions. Providing up to date laboratory results would seem to be especially important, given the popularity of checking lab results. Improving this feature has the advantage of providing patients with timely information, and may trigger clinicians to review patients' laboratory values and discuss the implications of the laboratory values with their patients once the values are available. We are now attempting to change the policy so that laboratory studies that populate the EMR will simultaneously populate the PHR. Patients complained that their medications and problem lists in myHERO were inaccurate. MyHERO information is populated from the EMR, suggesting that in our case, the data in the EMR were inaccurate. Although the exact nature of the inaccuracies is unclear, our own chart review would suggest that clinicians fail to update problem lists and acute problems remain active despite their clinical resolution. A similar thread applies to inaccurate medications. Clinicians often fail to discontinue medications that were administered and were subsequently changed or when the medication ended such as short course antibiotics. “Medication reconciliation” is an increasingly recognized element for high-quality outpatient care.19–21 Allowing the patient to review and verify their information in a PHR and alert their clinician of discrepancies in their list of conditions and their medication may help improve the accuracy of their records. Thus we would recommend more feedback from patients to clinicians to maintain accurate information in all electronic systems of healthcare. Knowing that patients are reviewing their diagnoses and medications may act as an important stimulus for the clinicians to maintain accurate information.
Limitations of this study
We were not able to determine the reasons for persons who registered an account but did not subsequently activate their account, although this number was low. We were also not able to determine why persons with early access did not continue to log onto their PHR for more sessions. Possible reasons that these early users did not continue to use their online PHR include access to the internet, and problems with how to use a computer or a PHR. There was considerable variation in the number of sessions and the number of months of PHR use across individuals. Some users with few months of use were new users, while others may have had poorer access to the internet, or did not derive sufficient value from myHERO. Providing better access to the internet might improve the continuity of use of a PHR, and a more comprehensive educational service to the end-users might improve their computer use or increase the value of the information in myHERO.
A limitation of the satisfaction data is that it is derived from 25% of the initial PHR users and therefore may not be representative of all PHR users nor would it represent the larger clinic population. The small sample size is a limitation of the preliminary study but still suggests that our patients would use a PHR. It is possible that number of sessions, pages accessed, and satisfaction would be different with a more diverse population with access to a PHR. It is also possible that internet access may limit PHR use and further work is needed to determine the relationship between PHR use and internet access.
The main goal of a PHR is to improve patient self-management of their health, and it is gratifying that over 80% of users responded that myHERO helped them better manage their health related problems. The finding that nearly a third of patients did not agree that the information is confidential is surprising given the consistent communications between staff and patients regarding the website, and it is not clear whether this concern with confidentiality impacted patients' PHR use. It is important in the future to clarify the issues of confidentiality and PHR use. Fundamentally, a PHR must provide value to the patient or it will not be used.22 For many patients, myHERO information was useful; however more applications, more timely information, or more accurate information will provide patients with greater utility and will probably lead to greater use of a PHR.8 23–25
In conclusion, this project demonstrated that HIV/AIDS patients receiving care in a safety net setting will choose to create, activate, and use a PHR. In the future PHRs will be flexible to changes and improvements, share data, retrieve comprehensive information from multiple sources, and allow patients or their advocates to use data to deliver the best possible advice and services. Patients who adopt PHRs will require that the information is protected and private, however data security was not as dominant a concern. Access to the internet will likely be a key factor for patients to access their health information on an online PHR. Patients receiving care from safety net institutions, and vulnerable patient populations, will utilize these new information technology tools and should have access to online PHRs.
Footnotes
Funding: Dr Kahn acknowledges support from the Commonwealth Fund 20070269; AHRQ R18 HS017784-01; and the NIH K24RR024369.
Competing interest: None.
Ethics approval: This project was granted an exemption certification (#0833272) by the University of California Committee for Human Research (the Investigational Review Board at UCSF) and was approved by the Privacy Board of the San Francisco Department of Public Health.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Kimmel Z, Greenes RA, Liederman E. Personal health records. J Med Pract Manage 2005;21:147–52 [PubMed] [Google Scholar]
- 2.Ball MJ, Costin MY, Lehmann C. The personal health record: consumers banking on their health. Stud Health Technol Inform 2008;134:35–46 [PubMed] [Google Scholar]
- 3.Haux R. Health information systems—past, present, future. Int J Med Inf 2006;75:268–81 [DOI] [PubMed] [Google Scholar]
- 4.Ball MJ, Gold J. Banking on health: personal records and information exchange. J Healthc Inf Manag 2006;20:71–83 [PubMed] [Google Scholar]
- 5.Wuerdeman L, Volk L, Pizziferri L, et al. How accurate is information that patients contribute to their electronic health record? AMIA Annu Symp Proc 2005:834–8 [PMC free article] [PubMed] [Google Scholar]
- 6.Lohr S. Kaiser backs Microsoft patient-data plan. NY Times June 10, 2008 [Google Scholar]
- 7.Steinbrook R. Personally controlled online health data—the next big thing in medical care? N Engl J Med 2008;358:1653–6 [DOI] [PubMed] [Google Scholar]
- 8.Detmer DE, Bloomrosen M, Raymond B, et al. Integrated personal health records: transformative tools for consumer-centric care. BMC Med Inform Decis Mak 2008;8:45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kupchunas WR. Personal health record: new opportunity for patient education. Orthop Nurs 2007;26:185–91; [quiz 92–3]. [DOI] [PubMed] [Google Scholar]
- 10.Tang PC, Ash JS, Bates DW, et al. Personal health records: definitions, benefits, and strategies for overcoming barriers to adoption. J Am Med Inform Assoc 2006;13:121–6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Tang PC, Lansky D. The missing link: bridging the patient-provider health information gap. Health Aff 2005;24:1290–5 [DOI] [PubMed] [Google Scholar]
- 12.Kahn JS, Aulakh V, Bosworth A. What it takes: characteristics of the ideal personal health record. Health Aff (Millwood) 2009;28:369–76 [DOI] [PubMed] [Google Scholar]
- 13.West DM, Miller EA. The digital divide in public e-health: barriers to accessibility and privacy in state health department websites. J Health Care Poor Underserved 2006;17:652–67 [DOI] [PubMed] [Google Scholar]
- 14.Graschew G, Roelofs TA, Rakowsky S, et al. Interactive telemedicine as a tool to avoid a digital divide in the world. Stud Health Technol Inform 2004;103:150–6 [PubMed] [Google Scholar]
- 15.Chang BL, Bakken S, Brown SS, et al. Bridging the digital divide: reaching vulnerable populations. J Am Med Inform Assoc 2004;11:448–57 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lorence D, Park H. Web-based consumer health information: public access, digital division, and remainders. MedGenMed 2006;8:4. [PMC free article] [PubMed] [Google Scholar]
- 17.Safran DG, Kosinski M, Tarlov AR, et al. The primary care assessment survey: tests of data quality and measurement performance. Med Care 1998;36:728–39 [DOI] [PubMed] [Google Scholar]
- 18.Rubin HR, Gandek B, Rogers WH, et al. Patients' ratings of outpatient visits in different practice settings. Results from the medical outcomes study. JAMA 1993;270:835–40 [PubMed] [Google Scholar]
- 19.Bernstein L, Frampton J, Minkoff NB, et al. Medication reconciliation: Harvard Pilgrim Health Care's approach to improving outpatient medication safety. J Healthc Qual 2007;29:40–5, 55. [DOI] [PubMed] [Google Scholar]
- 20.Dunham DP, Makoul G. Improving medication reconciliation in the 21st century. Curr Drug Saf 2008;3:227–9 [DOI] [PubMed] [Google Scholar]
- 21.Orrico KB. Sources and types of discrepancies between electronic medical records and actual outpatient medication use. J Manag Care Pharm 2008;14:626–31 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Sprague L. Personal health records: the people's choice? NHPF Issue Brief 2006:1–1317146910 [Google Scholar]
- 23.Ball MJ, Smith C, Bakalar RS. Personal health records: empowering consumers. J Healthc Inf Manag 2007;21:76–86 [PubMed] [Google Scholar]
- 24.Raisinghani MS, Young E. Personal health records: key adoption issues and implications for management. Int J Electron Healthc 2008;4:67–77 [DOI] [PubMed] [Google Scholar]
- 25.Fanjiang G, von Glahn T, Chang H, et al. Providing patients web-based data to inform physician choice: if you build it, will they come? J Gen Intern Med 2007;22:1463–6 [DOI] [PMC free article] [PubMed] [Google Scholar]