Abstract
Objective
To study the effects of using a population-based informatics system for osteoporosis screening and treatment in women aged 65 years or older.
Design
A population-based informatics system (PRECARES: PREventive CAre REminder System) was implemented to meet the needs of the workflow of a primary care practice. Patients treated in either of two sections of a primary care internal medicine department were selected for the intervention, and patients of a comparable third section served as the control group. PRECARES identified women in the intervention group who were due for osteoporosis screening on the basis of age and who had no record of previous screening in our clinical system. If these eligible patients did not have an upcoming outpatient appointment, appointment secretaries sent a letter requesting that they call to make an appointment for a dual-energy x-ray absorptiometry scan.
Measurements
At baseline and 3 months after the letters were sent, a database was used to determine the rate of osteoporosis screening in the intervention and control groups.
Results
A total of 689 patients in the intervention group were sent the letter. Three months after the letters were sent, the rate of osteoporosis screening was 76.4% (2409/3152) in the intervention group vs 69% (928/1344) in the control group (p<0.001). In the intervention group, 25% of the 689 patients responded to the letter and completed osteoporosis screening. Patients who had osteoporosis screening received appropriate treatment.
Conclusion
A population-based informatics system for primary care practice significantly improved the rate of osteoporosis screening.
Keywords: Information technology, osteoporosis, population management, prevention, screening
Keywords: DEXA, dual-energy x-ray absorptiometry, PCIM, primary care internal medicine, PRECARES, PREventive CAre REminder System
Introduction
Osteoporosis is a common medical condition with substantial health and societal effects. It is estimated that 35% of postmenopausal white women have osteoporosis.1 For white women aged 50 years and older, the lifetime risk of hip fracture is 17%.1 After hip fracture, one in five patients require nursing home care and only 30% are able to return to their former level of functioning.1 The mortality rate for an older patient during the first year after a hip fracture is estimated at 20%.1 Unless appropriate changes are made in osteoporosis screening and treatment, the direct medical costs from incident fractures are expected to increase from $16.9 billion in 2005 to $25.3 billion in 2025.2
On the basis of these data, the US Preventive Services Task Force and the National Osteoporosis Foundation recommend screening for osteoporosis for all women aged 65 years and older and for younger postmenopausal women with risk factors.3 4 Despite these recommendations, the screening rate for osteoporosis remains low. One study in 2002 found that only 12% of women aged 65 years and older in a managed care network reported being screened for osteoporosis.5
Screening for osteoporosis by measuring bone mineral density with dual-energy x-ray absorptiometry (DEXA) is minimally invasive, readily available, low cost, and predictive of fragility fracture.4 After screening, safe and effective treatments are available for osteoporosis.4 Recently, the WHO6 developed a fracture risk calculator, and the National Osteoporosis Foundation4 released specific guidelines for treatment that are based on the risk of fracture.
As medicine in the US moves toward pay for performance, primary care physicians increasingly are being evaluated by the preventive services that they deliver. The limiting factor for primary care physicians is time.7 Therefore, information systems must be developed to identify and screen patients who are due for preventive services independent of direct physician contact.
In a prior study at Mayo Clinic in Rochester, Minnesota, a population-based information system was effective in improving the rate of mammography screening.8 In that study we sent women two reminder letters, the second one sent 30 days after the first if the patient had not responded. The primary purpose of our current study was to evaluate whether expanding the use of this information system in an intervention group resulted in an improved osteoporosis screening rate compared with that in a control group if only one reminder letter was sent. A secondary aim of our study was to determine if the patients who underwent screening as a result of the population-based system (which did not require a primary care provider visit for screening) received appropriate treatment for osteopenia or osteoporosis.
Methods
Study population
Mayo Clinic in Rochester, Minnesota, is a large multispecialty group practice. The Division of Primary Care Internal Medicine (PCIM) includes 45 general internists who provide primary care for 24 000 adult patients living in Olmsted County, Minnesota. Currently, 5259 women older than 64 years are primary care patients of PCIM. PCIM is divided into six different sections by geographic location, and each of the 45 internists' patient panels is assigned to one of these sections. In this study, two sections of the division were selected for the intervention group and one section was selected for the control group.
The two intervention sections were recruited because of their interest in trying this new model of care addressing osteoporosis screening at a population level. At the beginning of our initiative, the effectiveness of such a system was not known. Support staff were needed to manage the patient contacts, phone calls to schedule the screening, and non-visit care for patients with osteopenia and osteoporosis identified on DEXA. We did not have the resources to support all six sections because only our current staff was used. One section was chosen as the control group because it was in the same geographical location as the other two sections and was deemed comparable in organizational structure. In the remaining three sections, a separate pilot was initiated during the study period that identified patients due for osteoporosis screening at the time of a visit with a provider; thus, those sections were not eligible as controls for our study. Within the three study sections, women aged 65 years and older were eligible for the study.
Intervention
Description of PRECARES
Patients who were due for osteoporosis screening in the intervention group were identified by PREventive CAre REminder System (PRECARES). PRECARES is an information system that uses data from the medical record to determine the last date of a preventive service for a particular patient. Osteoporosis screening date is captured from our clinical system (electronic medical record) based on certain service codes. PRECARES updates every weekend to minimize the load to our clinical systems on weekdays; therefore, information is most current on Mondays, and our appointment secretaries are trained to use it to initiate the process of contacting patients on Mondays.
PRECARES was developed using MS SQL server database, J2EE, and DHTML technologies. On the back end, PRECARES has been designed to have an information base, knowledge base, rules engine, and inference engine. The information base contains pertinent information about the patients and providers. The knowledge base contains evidence-based guidelines. The rules engine is built on top of the knowledge base and is based on other policies pertinent to specific services. The inference engine provides a mechanism to integrate the information base, knowledge base, and rules engine to generate service-specific recommendations within certain parameters of interest. On the middle and front tiers, the application uses a J2EE Struts-based Model View Controller architecture and DHTML to provide development flexibility and rich client experience.
PRECARES is a secure role-based Web application. At a high level, it provides two functionalities: Patient List and Patient Record. Patient List allows users to get a list of patients based on selected criteria. The inference engine is responsible for generating the patient list based on the rules and data points available in the information base. For example, the inference engine will not list patients as needing the service if they have an upcoming primary care appointment in the next 30 days as part of a rule defined in the rules engine. Once the list is generated and after contacting the patients, users can stamp the patients as ‘contacted’ to ensure that the system does not display patients who already have been contacted in a future query. On the basis of the configurable rules, a patient may be contacted again if no responses are received within a certain time frame. Patient Record module allows users to add or modify information about the patients. For example, if a patient notifies PCIM that she cannot have a mammogram every year because of an insurance policy or other reasons, that information can be entered into the rules engine using Patient Record module. If a permanent or temporary hold must be placed on a patient for privacy or any other reason, Patient Record allows users to do that.
PRECARES thus develops a list of patients due for preventive services and allows appointment secretaries to proactively manage these services.8 The list generated by PRECARES excludes all patients with an upcoming appointment with a provider in PCIM. At the time of this study, PRECARES defined patients due for osteoporosis screening as women aged 65 years and older who had never had a DEXA scan or women aged 65 years or older who had had a DEXA scan before age 65 years if it had been more than 2 years since their last evaluation.
Workflow designed for osteoporosis screening and treatment management
Once a patient was identified by PRECARES, the patient's chart was reviewed by one of two appointment secretaries. Patients were excluded from receiving the intervention if a DEXA scan had already been ordered but not yet completed, if the patient had not been seen in PCIM in the previous 5 years and thus was not an active patient of the practice, if the patient was a nursing home resident, or if the patient had previously requested not to be sent reminder letters. About 2% of all our patients have requested not to be contacted with reminder letters for any preventive services; this is most likely related to patients' personal preferences toward preventive services.
For the patients in the intervention group who were not excluded and had been identified by PRECARES as due for screening, the appointment secretaries sent one letter asking the patient to call to set up an appointment for osteoporosis screening by DEXA. We worked with our patient correspondence center to develop a simple-to-understand letter at the 8th-grade education level to explain both the need for osteoporosis screening and where to call to have this scheduled. For patients who responded to the letter and if the screening was acceptable to the patient, the appointment secretaries scheduled the DEXA.
Once the DEXA scan was completed, one of three nurses who participated in the study reviewed the results. If results of the scan were normal, a letter was sent to the patient stating that the results were satisfactory and suggesting weight-bearing exercise and adequate calcium and vitamin D supplementation. If DEXA results indicated either osteopenia or osteoporosis, the primary care physician was contacted for a plan of management.
Control group
Patients in the section chosen as the control group received usual care. A DEXA scan was ordered by the PCIM provider or proxied by the nurse on behalf of the provider if the patient was noted to be due for osteoporosis screening at the time of an office visit.
Outcome measurement
Mayo Clinic has developed a quality reporting system called Physician Portal. The Primary Care Physician Portal reports quality measures at the levels of individual provider, section (group of physicians), and practice. It uses the clinical record and billing data to determine the rates of completion of preventive services. The portal was used to determine the rates of DEXA screening in the intervention group and control group among women aged 65 years and older at baseline and 3 months after the letters were sent. The 3-month interval was chosen to allow time for patients to receive the letter and call to schedule an appointment for DEXA and for the test to be completed.
A detailed chart review was also undertaken to determine not only the frequency of diagnosis of osteopenia and osteoporosis as a result of the intervention but also whether these patients received appropriate treatment. The chart review was conducted 4 months after the letters were sent. This gave physicians an additional month to review the results of abnormal bone densities and develop a plan for management.
At the time of this study, the WHO had not released the fracture risk calculator, and the National Osteoporosis Foundation had not released its specific guidelines for treatment on the basis of fracture risk. Therefore, appropriate treatment for osteopenia was considered at least calcium and vitamin D supplementation, and appropriate treatment for osteoporosis was considered calcium and vitamin D supplementation along with a bisphosphonate, a selective estrogen-receptor modulator, hormone replacement therapy, or parathyroid hormone treatment.
The Mayo Clinic Institutional Review Board approved this study. Only data from patients who had previously completed a research authorization form and had been sent a Health Insurance Portability and Accountability Act form were included in the study.8
Statistical analysis
The percentages of patients of a particular age and race and with a particular type of insurance were compared at baseline between the intervention and control groups using the χ2 test. The percentages of patients current with osteoporosis screening at baseline and 3 months after the intervention were compared between the intervention and control groups using the χ2 test. Descriptive statistics were used to summarize the frequency of response to the letter, as well as the frequency of diagnosis of osteopenia and osteoporosis and the frequency of appropriate treatment for these conditions among patients who had their first DEXA scan as a result of the intervention. Among patients who had a repeat DEXA scan as a result of the intervention, descriptive statistics were used to summarize the frequency of worsening in bone density and the frequency of change in treatment. p<0.05 was considered statistically significant.
Results
The two sections of PCIM that composed the intervention group included 3152 women aged 65 years and older, and the one section that composed the control group included 1344 women aged 65 years and older. Age, race, insurance type, and percentage of patients current with osteoporosis screening were similar between the intervention and control groups at the beginning of the study (table 1). In August 2007, letters were sent to patients in the intervention group who were due for screening and who were not excluded. The percentages of patients who were current with DEXA screening in the intervention group and the control group were compared using the portal in mid November 2007, after conclusion of the intervention. The rate of osteoporosis screening improved significantly in the intervention group (76.4%; 2409 of 3152 patients) compared with that in the control group (69.0%; 928 of 1344 patients) (p<0.001).
Table 1.
Baseline characteristics of intervention and control groups*
| Characteristic | Intervention group (n=3152)† | Control group (n=1344)† | p Value |
| Patients with current | 2209 (70.1) | 914 (68.0) | 0.17 |
| osteoporosis screening | |||
| Age, y | 0.50 | ||
| 65–75 | 141 (4.5) | 75 (5.6) | |
| 76–85 | 1156 (36.7) | 478 (35.6) | |
| ≥86 | 1855 (58.8) | 791 (58.9) | |
| Race | 0.70 | ||
| White | 2970 (94.2) | 1250 (93.0) | |
| Asian | 39 (1.2) | 19 (1.4) | |
| Black | 14 (0.4) | 7 (0.5) | |
| Other | 25 (0.8) | 11 (0.8) | |
| Unknown | 104 (3.3) | 57 (4.2) | |
| Insurance type | 0.12 | ||
| Medicare | 2652 (84.1) | 1108 (82.4) | |
| Employee | 119 (3.8) | 67 (5.0) | |
| Blue Cross | 56 (1.8) | 12 (0.9) | |
| Other | 122 (3.9) | 49 (3.6) | |
| None | 18 (0.6) | 6 (0.4) | |
| Unknown | 185 (5.9) | 102 (7.6) | |
Values are number (percentage) of patients unless indicated otherwise.
Women aged 65 years or older.
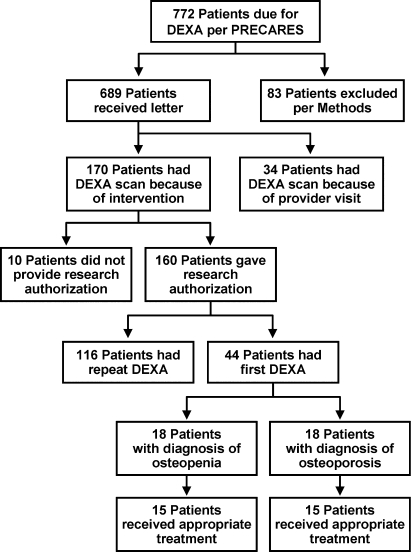
Among the intervention group, 772 patients were due for osteoporosis screening at the start of the study and did not have an upcoming appointment in PCIM according to PRECARES (figure 1). Of the patients, 83 were excluded for the reasons outlined in the Methods section and 689 were sent the letter requesting them to call and schedule a DEXA scan. Between mid August and December 2007, 204 patients in the intervention group had osteoporosis screening. Detailed review of the charts showed that 170 of these 204 patients received screening as a result of the intervention. The other 34 patients had screening as a result of a visit with a PCIM provider. Therefore, 170 (25%) of the 689 patients who received the letter completed osteoporosis screening.
Figure 1.
Summary of patients in the intervention group identified by PRECARES as due for osteoporosis screening. DEXA, dual-energy x-ray absorptiometry.
Among the 170 patients who had a DEXA scan as a result of the intervention, 160 had provided research authorization (figure 1). Of these 160 patients, 44 had DEXA for the first time as a result of the intervention. Within this group undergoing DEXA for the first time, 18 (41%) were diagnosed as having osteopenia and 18 (41%) were diagnosed as having osteoporosis. Fifteen patients (83%) in the osteopenia group and 15 patients (83%) in the osteoporosis group received appropriate treatment as a result of the study.
Of the 160 patients who had provided research authorization, 116 had repeat DEXA as a result of the intervention. Within this group undergoing repeat DEXA, 14 (12%) had worsening of bone density from normal to osteopenia and five (4%) had worsening of bone density from osteopenia to osteoporosis. Among the 116 patients, treatment changes included adding calcium and vitamin D for 32 patients (27.5%); adding calcium, vitamin D, and a bisphosphonate for three patients (2.6%); and adding only a bisphosphonate for seven patients (6%).
Discussion
Our results show that a system-based change, in which allied health staff work at their maximum level of licensure, can significantly improve the rate of osteoporosis screening with minimal involvement of the primary care provider. In our study, appointment secretaries identified patients due for osteoporosis screening through a population-based informatics system (PRECARES). The identified patients in the intervention group were then sent one letter requesting that they call to set up a DEXA scan. Three months after the letters were sent, the rate of osteoporosis screening was significantly improved in the intervention group compared with that in the control group. In the intervention group, 25% of the patients who received the letter responded and completed osteoporosis screening. In a prior study on breast cancer screening at Mayo Clinic, the percentage improvement with use of two reminder letters was greater than that observed in this study using only one letter.8 Therefore, more than one reminder letter for a preventive service may have an added benefit at a population level.
For the 44 patients who had their first DEXA scan as a result of the intervention, 82% received a diagnosis of osteopenia or osteoporosis. Review of their charts showed that most of these patients received appropriate treatment for low bone density. Among patients who had a repeat DEXA scan as a result of the intervention, very few (16%) had worsening of their bone density. This finding is consistent with those of a prior study showing that for healthy women aged 65 years and older, a repeat DEXA scan adds little value to initial bone mineral density measurement.9 However, in 36% of the patients in our study, repeat DEXA did result in the addition of calcium and vitamin D supplementation and/or the addition of a bisphosphonate.
The combination of short, 15 to 20 min primary care visits and an expanding list of clinical recommendations leads to significant pressure on the provider to address preventive care while also attempting to manage chronic diseases and acute needs.7 Therefore, population-based systems that can accurately identify the preventive needs of patients have considerable potential. If accurate and easy-to-use systems are available, allied health staff can provide timely reminders to patients due for preventive services, and protocols can enable them to order the tests on behalf of the primary care provider.10 11
Without PRECARES, population management would not be possible in our practice. The appointment staff would have to review the electronic medical record for all of the 5259 women patients aged 65 years and older in our practice to determine who had already completed osteoporosis screening and who was eligible for screening. Although it was still substantial, the effort needed to review the records of 772 patients to determine if they truly were eligible for screening was much less than it would have been for 5259 patients. For our study, our two appointment secretaries required less than 5 days to review the records and determine which patients were eligible for screening. We have now enhanced our population management system to further automate some of the prior manual processes.
A limitation of our study is the small number of patients who underwent initial osteoporosis screening. However, we were encouraged that among the patients who had their first DEXA scan, the intervention enabled us to identify a large percentage of patients who had osteopenia or osteoporosis and to begin appropriate treatment.
By developing information systems that serve the needs of patients who have not been seen in the office or who will not need a visit in the near future, we can ensure that their preventive care needs continue to be addressed. Information systems must be developed to support the workflow of the primary care practice and enable physicians to provide care for their population of patients. Population-based surveillance and delivery systems have the most promise to allow care for many patients who otherwise might not be receiving services.
As seen in our control group, many patients currently depend on receiving preventive services only through face-to-face contact with a provider. However, if patients have confidence that primary care practices have available the information systems and processes to address their needs for future preventive services, they might not request unnecessary visits to receive those services. If preventive services are being addressed by allied health staff using information systems, this will allow physicians more time to focus on acute care issues and chronic disease management. This holds especially true as we face a crisis in healthcare, with a future shortage of primary care physicians.12 13
Within our organization, the demonstrable early successes we had with breast cancer screening, osteoporosis screening, and population management of patients with diabetes mellitus helped us to convince our institutional leadership to invest further in the development of population management systems. We now also have dedicated staff in our appointment office to proactively manage not only our division's patient population, but also those of family medicine and pediatrics. Future reports will describe the ongoing initiatives we have for the management of diabetes mellitus and other conditions at a population level for all of our primary care patients.
Footnotes
Competing interests: None.
Provenance and peer review: Not commissioned; externally peer reviewed.
Ethics approval: The Mayo Clinic Institutional Review Board approved this study.
References
- 1.U.S. Department of Health and Human Services Bone health and osteoporosis: a report of the Surgeon General. Rockville, MD: U.S. Department of Health and Human Services, Office of the Surgeon General, 2004 [Google Scholar]
- 2.Burge R, Dawson-Hughes B, Solomon DH, et al. Incidence and economic burden of osteoporosis-related fractures in the United States, 2005-2025. J Bone Miner Res 2007;223:465–75 [DOI] [PubMed] [Google Scholar]
- 3.U.S. Preventive Services Task Force Screening for osteoporosis: topic page [Internet]. Rockville, MD: U.S. preventive services task force, agency for healthcare research and quality, 2002. [cited 2008 Jun 30]: http://www.ahrq.gov/clinic/uspstf/uspsoste.htm [Google Scholar]
- 4.National Osteoporosis Foundation Clinician's guide to prevention and treatment of osteoporosis. Washington, DC: National Osteoporosis Foundation, 2008 [Google Scholar]
- 5.Gallagher TC, Geling O, Comite F. Missed opportunities for prevention of osteoporotic fracture. Arch Intern Med 2002;162:450–6 [DOI] [PubMed] [Google Scholar]
- 6.The World Health Organization FRAX: WHO fracture risk assessment tool. [Internet]. Sheffield, UK: World Health Organization Collaborating Centre for Metabolic Bone Diseases, University of Sheffield; [cited 2008 Jun 30] http://www.shef.ac.uk/FRAX/ [Google Scholar]
- 7.Yarnall KS, Pollak KI, Ostbye T, et al. Primary care: is there enough time for prevention? Am J Public Health 2003;93:635–41 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Chaudhry R, Scheitel SM, McMurtry EK, et al. Web-based proactive system to improve breast cancer screening: a randomized controlled trial. Arch Intern Med 2007;167:606–11 [DOI] [PubMed] [Google Scholar]
- 9.Hillier TA, Stone KL, Bauer DC, et al. Evaluating the value of repeat bone mineral density measurement and prediction of fractures in older women: the study of osteoporotic fractures. Arch Intern Med 2007;167:155–60 [DOI] [PubMed] [Google Scholar]
- 10.Kottke TE, Solberg LI. STEP(ing)-UP to deliver clinical preventive services. Am J Prev Med 2001;21:68–9 [DOI] [PubMed] [Google Scholar]
- 11.Hung DY, Rundall TG, Crabtree BF, et al. Influence of primary care practice and provider attributes on preventive service delivery. Am J Prev Med 2006;30:413–22 [DOI] [PubMed] [Google Scholar]
- 12.Moore G, Showstack J. Primary care medicine in crisis: toward reconstruction and renewal. Ann Intern Med 2003;138:244–7 [DOI] [PubMed] [Google Scholar]
- 13.Sandy LG, Schroeder SA. Primary care in a new era: disillusion and dissolution? Ann Intern Med 2003;138:262–7 [DOI] [PubMed] [Google Scholar]