Abstract
Objectives
Regional variation in health care use in the last 6 months of life is well documented. Our objective was to examine whether an association exists between cardiologists' tendencies to discuss palliative care for patients with advanced heart failure and the regional use of health care in the last 6 months of life.
Methods
We performed a national mail survey of a random sample of 994 eligible Cardiologists from the American Medical Association Masterfile. Hypothetical patient scenarios were used to explore physician management of patient scenarios.
Results
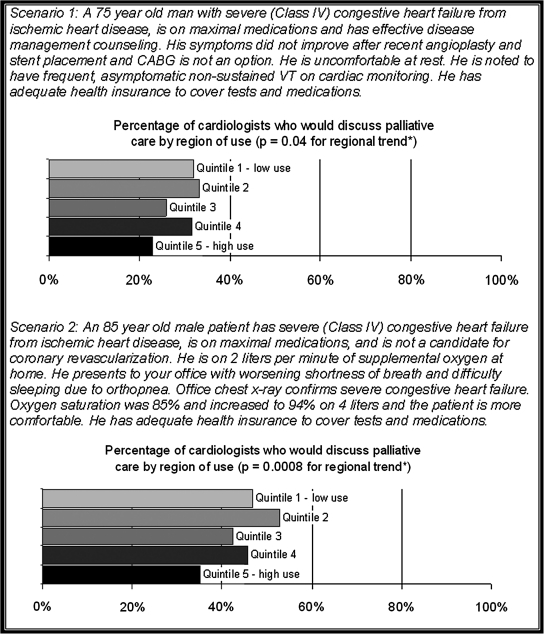
We received 614 responses (response rate: 62%). In a 75-year-old with symptomatic chronic heart failure and asymptomatic nonsustained ventricular tachycardia, cardiologists in regions with high use in the last 6 months of life were less likely to have discussions about palliative care (23% versus 32% for comparisons between the highest and lowest quintiles, p = 0.04). Similarly, in an 85 year-old with symptomatic chronic heart failure and an acute exacerbation, cardiologists in high use regions were less likely to have discussions about palliative care (35% versus 47%, p = 0.0008).
Conclusions
Despite professional guidelines suggesting that cardiologists discuss palliative care with patients with late stage heart failure, less than half of cardiologists would discuss palliative care in two elderly patients with late-stage heart failure and this guideline discordance was worse in the regions with more health care use in the last 6 months of life.
Introduction
Use of health care in the last 6 months of life varies markedly across the United States.1 In relation to this, hospice and palliative care also exhibit particularly dramatic variation. In 2006, approximately half of the hospitals in the country had hospital-based palliative care teams ranging from over 80% in Montana to less than 20% in Alabama and Mississippi.2 Likewise, referrals to hospice prior to death ranged from 11% to 43% among a cohort of the highest rated hospitals in the country.3 These wide variations in health care do not appear to relate to patient preferences or disease severity4,5 nor are they associated with better outcomes or increased patient satisfaction.6,7 Physician practice patterns may be responsible for geographic variations in health care spending,8 but this association has been difficult to demonstrate.9
Heart disease remains the leading cause of death and as a consequence, cardiologists frequently encounter patients in the last six months of their lives. In the case of heart failure, the American College of Cardiology/American Heart Association (ACC/AHA) Guidelines recommend “palliative care” in the context of signs and symptoms of heart failure despite therapy.10,11 This study evaluates the regional association between cardiologists' reported tendency to discuss palliative care and the regional intensity of care in the last 6 months of life.
Methods
Study design
A national survey of cardiologists was conducted to test whether the intensity of treatment recommendations in clinical scenarios was associated with the regional use of medical resources. Overall results of the survey are reported elsewhere.12 This report focuses on items from the parent survey specifically addressing palliative care. The survey was conducted between May and July, 2004. This research was approved by the Institutional Review Boards at Dartmouth Medical School and the University of Massachusetts.
Survey development
The survey was developed in several steps. First, the research team developed the initial draft of two surveys (one for internists and one for cardiologists) based on their lessons learned from prior surveys.13,14 Next, modifications were made based on feedback from four focus groups of cardiologists and internists in areas of high (Miami, FL) and low intensity (Portland, OR). Finally, 12 cognitive interviews were conducted (8 with internists and 4 with cardiologists) to ensure clarity of the questions and answer choices. The final survey contained questions about the demographics of the clinician followed by hypothetical patient scenarios commonly encountered in cardiology.
Data collection
Study population
The physician sample was obtained from the American Medical Association Masterfile. To be eligible, the respondent had to be an actively practicing cardiologist seeing patients at least 20 hours per week. Eligibility was verified by telephone prior to mailing the survey with a maximum of three call attempts during the daytime and evening. For this analysis, subspecialty within cardiology was determined based on self-reported scope of practice rather than board certification: any cardiologist who reported performing electrophysiologic procedures was categorized as an “electrophysiologist”; those reporting performing percutaneous interventions but not electrophysiologic procedures were classified as “interventional”; cardiologists who reported performing cardiac catheterizations without interventions or electrophysiologic procedures were classified as “invasive”; and if none of the above were true, they were classified as “general cardiologists.” A sample of 1340 cardiologists was identified. Of these, 183 were deemed ineligible based on the initial telephone screening. Of the 1157 remaining, 999 were randomly chosen to receive the mail survey. Of these, 5 additional respondents were determined to be ineligible.
Mail procedures
Each potential respondent was sent an initial questionnaire packet with a letter explaining the study, a $20 cash incentive, the survey, and a postage-paid return envelope. Nonresponders were sent a second survey 2 weeks after the initial mailing absent the cash incentive.
Measures
Recommend palliative care
One scenario described a 75-year-old man with New York Heart Association (NYHA) class IV (severely symptomatic) heart failure symptoms and nonsustained ventricular tachycardia and another described an 85-year-old man with NHYA class IV heart failure with an acute heart failure exacerbation. Each scenario was followed by a question asking how often would you “initiate or continue discussions about palliative care.” Response choices, along a 5-point Likert scale, ranged from “always/almost always” to “never.”
Regions
The regional unit used in this analysis was the Hospital Referral Region (HRR). HRRs were developed by researchers at Dartmouth using the Medicare claims data to identify regions with common referral patterns for major cardiovascular and neurosurgical procedures. Each cardiologist was assigned to an HRR based on the zip code of his practice address.
End-of-life intensity
To determine the intensity of care in the last 6 months of life for each region, we used the end-of-life expenditure index (EOL-EI). This is a measure based on mean Medicare expenditures for beneficiaries aged 65 and older in the last 6 months of life. The development of this measure is described elsewhere.4,5 The mean EOL-EI was calculated for each of 306 HRRs, which were then grouped into five quintiles of equal populations.
Statistical analysis
Responses were dichotomized using “always/almost always” and “most of the time” to indicate an affirmative response that the clinician would recommend “discussions about palliative care.” Logistic regression was used to evaluate the association between end-of-life intensity and guideline concordance with the dichotomized responses as the dependent variable and regional spending as determined by the EOL-EI as a continuous independent variable. Results were adjusted for physician age, gender, and specialty.
Results
In total, we received 614 completed surveys of the 994 surveys sent to eligible respondents (response rate of 62%).15 There were no differences between responders and nonresponders in terms of gender, practice type, and year of medical school graduation (p > 0.05 for all comparisons). Despite prescreening for specialty, an additional 16 physicians reported their specialties as something other than cardiology on the survey; these observations were excluded, leaving a total analytic sample of 598.
The physician sample consisted predominantly of white (81%), male (93.1%), board certified (94.6%) cardiologists with an average age of 52 (Table 1). Categorized according to self-reported scope of practice, 36% of participants were classified as general cardiologists, 21% as invasive cardiologists, 36% as interventional cardiologists, and 7% as electrophysiologists. Other information on payment sources and practice type is shown in Table 1.
Table 1.
Characteristics of the Survey Study Respondents
| Age, mean (SD) | 52.3 (9) |
| Gender—Male, no. (%) | 556 (93) |
| Race, no. (%) | |
| White | 479 (81.5) |
| Black | 7 (1.2) |
| Asian | 82 (14.0) |
| Other | 30 (5.0) |
| Board certified, no. (%) | 559 (95) |
| Subspecialty, no. (%) | |
| General cardiology | 214 (35.8) |
| Invasive | 128 (21.4) |
| Interventional | 212 (35.5) |
| Electrophysiology | 44 (7.4) |
| Practice Type, no. (%) | |
| Solo or two-person practice | 115 (19.3) |
| Single specialty group | 323 (54.2) |
| Multispecialty group | 89 (14.4) |
| Group or staff model HMO | 9 (1.5) |
| Hospital-based practice (VA or other) | 46 (7.7) |
| Other | 14 (2.4) |
| Payment Type, (%) | |
| Medicare | 52.4 |
| Medicaid | 8.6 |
| Other Insurance | 34.1 |
| No Insurance | 5.0 |
| Capitated | 11.5 |
HMO, health maintenance organization.
In a 75-year-old patient with stage IV heart failure and nonsustained ventricular tachycardia, less than a third of the cardiologists would “initiate or continue discussions about palliative care” and this was lower in the higher spending regions (23% versus 32% for comparison between the lowest and highest quintiles, p = 0.04 for trend). In an 85 year-old patient with stage IV heart failure and an acute exacerbation, less than half of the cardiologists would “initiate or continue discussions about palliative” and this was also lower in the higher spending regions (35% versus 47%, p = 0.0008; Fig. 1).
FIG. 1.
Cardiologists tendency to discuss palliative care across regions of health care use in the last 6 months of life for two patients with late-stage heart failure.
Discussion
ACC/AHA guidelines for chronic heart failure clearly recommended that cardiologists engage in discussions about prognosis, advanced directives, care coordination, and symptom control in patients with late stage heart failure (e.g., symptomatic despite therapy).10,11 Over half of the cardiologists sampled for this study recommended care that was discordant from these guidelines and this discordance was worse in the regions performing more intense medical care in the last 6 months of life.
There are a few potential explanations for our findings. Most patients and their families want and expect an accurate and honest estimate of prognosis16,17 and they want their physicians to initiate these discussions.18 However, significant uncertainty in prognosticating heart failure makes initiating such discussions challenging and is a barrier to palliative care.19,20 Alternatively, cardiologists may have interpreted this question with the common misunderstanding that “initiating and continuing discussions about palliative care” means forgoing aggressive treatment.
Several factors should be considered in the interpretation of our findings. First, because we used Medicare data to measure end-of-life intensity of health care, the EOL-EI may not represent the intensity of end-of-life care in all age groups. However, both patients in the scenarios were over the traditional Medicare age of 65. Second, we used hypothetical scenarios to judge practice patterns. However, hypothetical scenarios are a particular strength of this study because they remove unmeasured patient confounders.21,22 Finally, the survey was performed in 2004 and may not reflect cardiologists' current inclinations to discuss palliative care. However, while the overall rate of palliative care discussions may be higher today than in 2004, regional variation in the intensity of care in the last 6 months of life remains1 and our finding that regional differences exist in cardiologists' propensity to discuss palliative care is likely unchanged as well.
The work to improve the care of patients with end-stage heart failure is important, challenging, and ongoing. While recent reviews on palliative care in HF have been published in major cardiovascular journals,23,24 the research on palliative care in heart failure is lagging.20 Furthermore, quality measures such as 30-day heart failure-specific mortality may create disincentives to discussing palliative care.25 Thus, efforts to increase awareness of palliative care among cardiologists and knowledge about how to best implement palliative care in heart failure populations are greatly needed.
Acknowledgments
This research was conducted while Dan Matlock, M.D. was supported by an institutional T32HP10006 as well as while he was a Hartford Geriatrics Health Outcomes Scholar. This study was supported by the National Institute on Aging (grant no. PO1 AG19783) and by a Research Enhancement Award no. O3-098 from the Department of Veterans Affairs.
Author Disclosure Statement
No competing financial interests exist
References
- 1.The Dartmouth Atlas of Health Care. 2010. www.dartmouthatlas.org/topics/preference_sensitive.pdf. [Mar 29;2010 ]. www.dartmouthatlas.org/topics/preference_sensitive.pdf
- 2.Goldsmith B. Dietrich J. Du Q. Morrison RS. Variability in access to hospital palliative care in the United States. J Palliat Med. 2008;11:1094–1102. doi: 10.1089/jpm.2008.0053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Wennberg JE. Fisher ES. Stukel TA. Skinner JS. Sharp SM. Bronner KK. Use of hospitals, physician visits, and hospice care during last six months of life among cohorts loyal to highly respected hospitals in the United States. Br Med J. 2004;328:607. doi: 10.1136/bmj.328.7440.607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Barnato AE. Herndon MB. Anthony DL. Gallagher PM. Skinner JS. Bynum JP. Fisher ES. Are regional variations in end-of-life care intensity explained by patient preferences? A study of the US medicare population. Med Care. 2007;45:386–393. doi: 10.1097/01.mlr.0000255248.79308.41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Fisher ES. Wennberg DE. Stukel TA. Gottlieb DJ. Lucas FL. Pinder EL. The implications of regional variations in Medicare spending. Part 1: The content, quality, and accessibility of care. Ann Intern Med. 2003;138:273–287. doi: 10.7326/0003-4819-138-4-200302180-00006. [DOI] [PubMed] [Google Scholar]
- 6.Fisher ES. Wennberg DE. Stukel TA. Gottlieb DJ. Lucas FL. Pinder EL. The implications of regional variations in Medicare spending. Part 2: Health outcomes and satisfaction with care. Ann Intern Med. 2003;138:288–298. doi: 10.7326/0003-4819-138-4-200302180-00007. [DOI] [PubMed] [Google Scholar]
- 7.FJ Fowler., Jr Gallagher PM. Anthony DL. Larsen K. Skinner JS. Relationship between regional per capita Medicare expenditures and patient perceptions of quality of care. JAMA. 2008;299:2406–2412. doi: 10.1001/jama.299.20.2406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Skinner J. Chandra A. Goodman D. Fisher ES. The elusive connection between health care spending and quality. Health Aff. 2009;28:w119–w123. doi: 10.1377/hlthaff.28.1.w119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wennberg DE. Dikens JD. Soule DN. Kellett MA. Malenka DJ. Robb JF. T Ryan., Jr Bradley W. Vaitkus P. Hearne M. O'Connor G. Hillman R. The relationship between the supply of cardiac catheterization laboratories, cardiologists and the use of invasive cardiac procedures in northern New England. J Health Serv Res Policy. 1997;2:75–80. doi: 10.1177/135581969700200204. [DOI] [PubMed] [Google Scholar]
- 10.Hunt SA. Abraham WT. Chin MH. Feldman AM. Francis GS. Ganiats TG. Jessup M. Konstam MA. Mancini DM. Michl K. Oates JA. Rahko PS. Silver MA. Stevenson LW. Yancy CW. Antman EM. Smith SC., Jr Adams CD. Anderson JL. Faxon DP. Fuster V. Halperin JL. Hiratzka LF. Jacobs AK. Nishimura R. Ornato JP. Page RL. Riegel B. American College of Cardiology; American Heart Association Task Force on Practice Guidelines; American College of Chest Physicians; International Society for Heart Lung Transplantation; Heart Rhythm Society: ACC/AHA 2005 Guideline Update for the Diagnosis and Management of Chronic Heart Failure in the Adult. Circulation. 2005;112:e154–e235. doi: 10.1161/CIRCULATIONAHA.105.167586. [DOI] [PubMed] [Google Scholar]
- 11.Hunt SA. Baker DW. Chin MH. Cinquegrani MP. Feldman AM. Francis GS. Ganiats TG. Goldstein S. Gregoratos G. Jessup ML. Noble RJ. Packer M. Silver MA. Stevenson LW. Gibbons RJ. Antman EM. Alpert JS. Faxon DP. Fuster V. Jacobs AK. Hiratzka LF. Russell RO. Smith SC., Jr American College of Cardiology/American Heart Association: ACC/AHA guidelines for the evaluation and management of chronic heart failure in the adult: executive summary. A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee to revise the 1995 Guidelines for the Evaluation and Management of Heart Failure) J Am Coll Cardiol. 2001;38:2101–2113. doi: 10.1016/s0735-1097(01)01683-7. [DOI] [PubMed] [Google Scholar]
- 12.Lucas FL. Sirovich BE. Gallagher PM. Siewers AE. Wennberg DE. Variation in cardiologists' propensity to test and treat: Is it associated with regional variation in utilization? Circ Cardiovasc Qual Outcomes. 2010;3:253–260. doi: 10.1161/CIRCOUTCOMES.108.840009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wennberg DE. Dickens JD., Jr Biener L. Fowler FJ., Jr Soule DN. Keller RB. Do physicians do what they say? The inclination to test and its association with coronary angiography rates. J Gen Intern Med. 1997;12:172–176. doi: 10.1007/s11606-006-5025-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Sirovich BE. Gottlieb DJ. Welch HG. Fisher ES. Variation in the tendency of primary care physicians to intervene. Arch Intern Med. 2005;165:2252–2256. doi: 10.1001/archinte.165.19.2252. [DOI] [PubMed] [Google Scholar]
- 15.Standard Definitions: final Dispositions of Case Codes and Outcome Rates for Surveys. 3rd ed. Lenexa, KS: AAPOR; 2004. American Association for Public Opinion Research. [Google Scholar]
- 16.Back AL. Arnold RM. Discussing prognosis: “How much do you want to know?” Talking to patients who are prepared for explicit information. J Clin Oncol. 2006;24:4209–4213. doi: 10.1200/JCO.2006.06.007. [DOI] [PubMed] [Google Scholar]
- 17.Apatira L. Boyd EA. Malvar G. Evans LR. Luce JM. Lo B. White DB. Hope, truth, and preparing for death: Perspectives of surrogate decision makers. Ann Intern Med. 2008;149:861–868. doi: 10.7326/0003-4819-149-12-200812160-00005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hanson LC. Danis M. Garrett J. What is wrong with end-of-life care? Opinions of bereaved family members. J Am Geriatr Soc. 1997;45:1339–1344. doi: 10.1111/j.1532-5415.1997.tb02933.x. [DOI] [PubMed] [Google Scholar]
- 19.Hanratty B. Hibbert D. Mair F. May C. Ward C. Capewell S. Litva A. Corcoran G. Doctors' perceptions of palliative care for heart failure: focus group study. Br Med J. 2002;325:581–585. doi: 10.1136/bmj.325.7364.581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Goodlin SJ. Hauptman PJ. Arnold R. Grady K. Hershberger RE. Kutner J. Masoudi F. Spertus J. Dracup K. Cleary JF. Medak R. Crispell K. Piña I. Stuart B. Whitney C. Rector T. Teno J. Renlund D. Consensus statement: Palliative and supportive care in advanced heart failure. J Card Fail. 2004;10:200–209. doi: 10.1016/j.cardfail.2003.09.006. [DOI] [PubMed] [Google Scholar]
- 21.Peabody JW. Luck J. Glassman P. Dresselhaus TR. Lee M. Comparison of vignettes, standardized patients, and chart abstraction: A prospective validation study of 3 methods for measuring quality. JAMA. 2000;283:1715–1722. doi: 10.1001/jama.283.13.1715. [DOI] [PubMed] [Google Scholar]
- 22.Peabody JW. Luck J. Glassman P. Jain S. Hansen J. Spell M. Lee M. Measuring the quality of physician practice by using clinical vignettes: A prospective validation study. Ann Intern Med. 2004;141:771–780. doi: 10.7326/0003-4819-141-10-200411160-00008. [DOI] [PubMed] [Google Scholar]
- 23.Goodlin SJ. Palliative care in congestive heart failure. J Am Coll Cardiol. 2009;54:386–396. doi: 10.1016/j.jacc.2009.02.078. [DOI] [PubMed] [Google Scholar]
- 24.Adler ED. Goldfinger JZ. Kalman J. Park ME. Meier DE. Palliative care in the treatment of advanced heart failure. Circulation. 2009;120:2597–2606. doi: 10.1161/CIRCULATIONAHA.109.869123. [DOI] [PubMed] [Google Scholar]
- 25.Holloway RG. Quill TE. Mortality as a measure of quality: Implications for palliative and end-of-life care. JAMA. 2007;298:802–804. doi: 10.1001/jama.298.7.802. [DOI] [PubMed] [Google Scholar]