Abstract
The research provides results of an expert review of data displays for a sensor system used to monitor functional abilities in the elderly. The research took place at TigerPlace, an assisted living facility, where the sensor system is currently being evaluated. A checklist of 16 heuristic criteria was used to evaluate the sensor data displays keeping in mind the users of the system, adults and elderly people. Results of our expert review indicate that flexibility and efficiency of use, help and documentation, navigation and skills were not well developed in our sensor data displays. Conversely, sensor data displays were rated highly for their aesthetic value and for their ample visual contrast for the main parts of the data displays. Researchers believe that through the use of a sensor system we can accomplish new ways of detecting functional decline in elderly residents living in assisted living facilities.
INTRODUCTION
Demand for assisted living facilities is expected to increase as the baby-boom generation ages and the percentage of older Americans increases over the next 25 years. Older adults prefer aging-in-place. If they can't live at home a second choice might be in the home-like environment of an assisted living facility rather than moving to the more restrictive nursing home environment (Chapin & Dobbs-Kepper, 2001). One factor limiting aging-in-place in an assisted living environment is age-related functional decline ( i.e., decline in performance of basic and instrumental activities of daily living, and increased need for assistance from caregivers) (Aud, 2004; Hawes, Phillips, Rose, Holan, & Sheridan, 2003; Kissam, Gifford, Vor, & Patry, 2003). Thus, while consumers prefer to remain in the least restrictive environment possible, increasing dependency and functional decline often result in transfer to a nursing home.
With the assistance of technology, early recognition of functional decline, and prompt treatment of acute illnesses or exacerbations of chronic illnesses, we anticipate older adults will be able to remain in assisted living longer, improving their quality of life and independence. The pilot study reported here describes preliminary results of an expert review of computer interfaces for a sensor system installed in TigerPlace, an assisted living facility at the University of Missouri. To date 9 residents are living with sensor systems installed in their apartments; data on 14 residents have been collected since the study started. Inclusion criteria included living at TigerPlace and living alone. These residents, their families and healthcare providers are participating in ongoing interviews, further aiding researchers understanding of how sensors can assist to monitor people in these settings and why residents would choose to use these devices. Clinical implications for how these data can be used to monitor for increasing dependency and functional decline will be discussed.
BACKGROUND
Detecting functional decline in elders
Clinicians have anecdotally reported for many years that decline in function is often an early indicator of an impending acute illness or an exacerbation of a chronic illness. Researchers have confirmed these observations and have identified risk factors to detect those older adults most at risk of experiencing decline in physical function (Fried, Bandeen-Roche, Chaves, & Johnson, 2000; Onder et al., 2005; Wolinsky, Miller, Andresen, Malmstrom, & Miller, 2005). Early illness recognition and early treatment is not only a key to improved health status with more rapid recovery after an acute illness or exacerbation of a chronic illness but also a key to morbidity and mortality in older adults (Boockvar & Lachs, 2003; Hogan, 2006; Ridley, 2005).
While traditional assessments by health care providers often reveal signs of impending or early decline in function, typically the older adult must be physically present with the health care provider or in some cases connected by expensive telemedicine equipment (Alexander et al., 2000; Wolinsky et al., 2005). Self report of functional performance and early decline in function predicts actual functional performance and decline (Fried, Young, Rubin, Bandeen-Roche, & WHAS II Collaborative Research Group, 2001; Wakefield & Holman, 2007).
However, researchers have concluded that asking older adults to self-report functional limitations or disability “captures only the tip of the ice-berg” (Wolinsky et al., 2005). New ways of detecting decline in physical function are needed, including ways that can be unobtrusive yet accurately assess physical function and detect declines from an individual's normal functional performance; do not require face-to-face assessment of the individual by a health care provider; and can use what people normally do in the course of their daily activities of living that can reveal changes in physical function and alert health care providers that they need to assess for changes. We believe the use of a sensor system can accomplish these new ways of detecting decline in physical function. Using and evaluating the impact of such a sensor system is especially critical given the rapidly expanding elderly population.
Sensor Technology to Detect Functional Decline in Older Adults
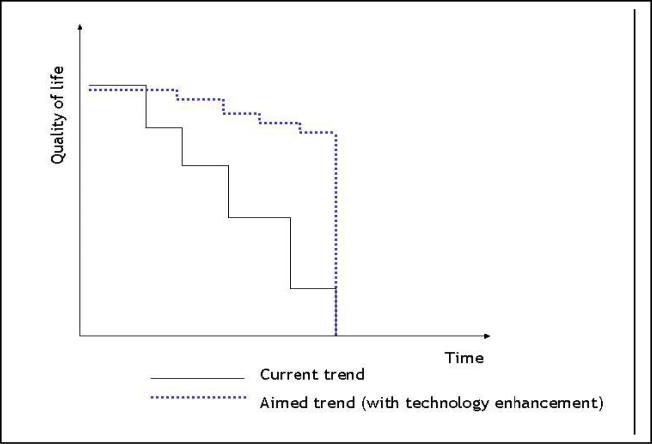
Our research team is searching for opportunities to use technology to enhance the quality of life for residents who may be nearing the end of their life. Figure 1 illustrates that overall function for elders remains fairly constant for a period of time until some change in mobility, cognition, or sensation alters the functional status of an individual. In current practice (current trend), these changes are not detected as quickly and interventions are delayed that could prevent functional deterioration. In our ideal scenario (aimed trend), technology should enhance the formal and informal caregiver's ability to detect fluctuations in activity levels from the elder's baseline activity sooner. This early warning system will enable caregivers to implement necessary assistive interventions such as medication management, fall risk protection measures, and assistance in daily living requirements sooner, thereby delaying functional decline for these residents.
Figure 1.
Trajectory of Functional Decline With and Without Technology
The pilot study reported here is part of a larger study evaluating use of passive sensor technology to assess activity levels of elder residents living in an assisted living facility. A model used by our research team (Rantz, M.J., Dorman-Marek, K., Aud, M.A., Tyrer, H.W., Skubic, M., Demiris, G. et al. 2005; Tyrer, Aud, Alexander, Skubic, & Rantz, 2007) illustrated in Figure 1 shows the trajectory of functional decline in a current trend (without sensor technology) and an aimed trend (with sensor technology). The current trend without technology has a much steeper rate of decline in functional abilities which leaves the resident at a much lower level of functioning in later stages of life. Technology should help the user of the system identify sentinel health events affecting functional ability earlier, resulting in a quicker response rate to the problem and less decline in functional ability toward the end of life.
METHODS
Sensor Data Displays
The University of Missouri Institutional Research Board approved all research procedures before they were conducted. A multidisciplinary taskforce of our research team has been working on developing sensor data displays during the past year. The data display or interface is described as a connection between two systems through which information is exchanged. For example, the sensors are hardware interfaces that detect resident motions, such as a bed sensor or a wall mounted room sensor. Other sensors detect stove temperature, restlessness in bed measured by the frequency of fidgeting while lying down in bed and physiological parameters such as pulse rate and rate of breathing. The sensors are connected to small computers to produce a sensor network. In our sensor network, the information that was captured through the sensor hardware was stored on a computer until software programs in the form of data displays were developed to allow humans to interact with the data for decision making purposes.
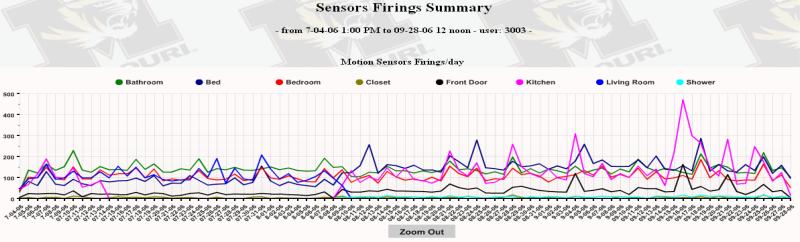
The team has used data captured from the sensors (hardware) since 2004 to develop data displays (software) as shown in Figure 2. The data displayed in Figure 2 provide a detailed account of the activity frequency for one resident from July to September 2006. An activity graph is shown for each sensor installed in this user's apartment. These sensors are located in the bathroom, bed, bedroom, closet, front door, kitchen, living room, and shower. To develop these displays experts from multiple disciplines (Gerontological nursing, informatics, computer science, physical/occupational therapy and health management) came together and iteratively reviewed the data and displays, offered suggestions for improvement, participated in development and refinement of each version, and studied changes in activity patterns as the data were displayed.
Figure 2.
Sensor Data Display of Motion Sensors in Resident Apartment
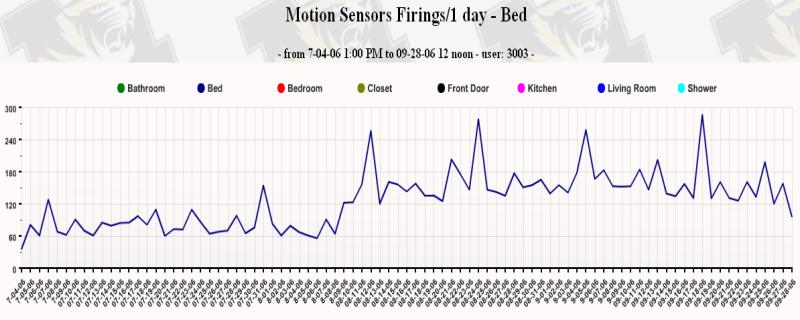
The data display has many functions that the residents, their families, and healthcare providers can use to monitor activities of residents who have sensors installed in their apartments. For example, each individual line graph located within Figure 2 can be viewed separately. This enables the user of the data to get a better picture of individual activities throughout the apartment and can be more revealing for users. A nurse who was interested in the amount of time a resident was spending in bed can view the line graph for the bed as shown in Figure 3. These data show only a section of the graph from Figure 2 for the bed activity for this user during the same time frame. As you look at the data in Figure 3 note the change in the baseline data during the first week of August. This increase in the baseline indicates that this user had a change in the frequency for which his bed sensor was being activated. This increase in time in bed might warrant further investigation.
Figure 3.
Sensor Data Display for Motion Sensors on Bed
A healthcare provider or family member might also want to know if the resident was experiencing more restlessness during this increased time in bed. Therefore, our team established a scale for restlessness that ranges from low restlessness lasting 1-3 seconds to highest restlessness lasting greater than 9 seconds while the user is lying in bed. This scale allows us to detect periodic changes in restlessness while residents are sleeping.
In some situations, the research team has modified the use of the sensors to accommodate a resident's activity habits. For example, one resident who had poor heart function was having difficulty sleeping while lying flat in bed; we noted in sensor data that the resident was spending a great majority of time in a chair sitting up while sleeping. Upon further investigation we found this was a normal activity for the resident. Knowing this allowed us to redefine how we used the sensor system in the apartment to better monitor the resident while sleeping.
Sensor data display expert usability review
In August 2007, the taskforce hired an outside expert review panel (three reviewers trained in usability evaluation) to conduct an expert review of the TigerPlace sensor data display (partially illustrated in Figures 2-3). The three reviewers were graduate PhD students working in a usability laboratory with expertise in information science including interface design, information access design and information organization. A heuristic evaluation was specially created to suit the interface being evaluated keeping in mind the audience of the website—healthcare provider, family and elderly resident. The expert review was based on a heuristic evaluation checklist (Table 1).
Table 1. Findings from Sensor Data Display Expert Usability Review.
The table provides the descriptive data of the heuristic evaluation done by three expert reviewers’ based on the sensor data display's compliance with the 16 heuristic criteria.
| *Heuristic | Number of Criteria | Meets heuristics | Does not Meet heuristics | Heuristics not applicable | Agreement with heuristic criteria | Potential Problem 1=Least Importance 4=High Importance |
|---|---|---|---|---|---|---|
| 1. Visibility of system status | 10 | 2 | 7 | 1 | 22% | 3 |
| 2. Match between system and the real world | 5 | 0 | 3 | 2 | 0 | 2 |
| 3. User control and freedom | 8 | 2 | 3 | 3 | 40% | 3 |
| 4. Consistency and standards | 4 | 2 | 2 | 0 | 50% | 2 |
| 5. Help users recognize, diagnose, and recover from errors | 2 | 0 | 1 | 1 | 0 | 3 |
| 6. Error prevention | 4 | 0 | 2 | 2 | 0 | 3 |
| 7. Recognition rather than recall | 16 | 7 | 4 | 5 | 64% | 2 |
| 8. Flexibility and minimalist design | 5 | 0 | 3 | 2 | 0 | 4 |
| 9. Aesthetic and minimalist design | 4 | 2 | 0 | 2 | 100% | 1 |
| 10. Help and documentation | 9 | 0 | 5 | 4 | 0 | 4 |
| 11. Skills | 4 | 0 | 2 | 2 | 0 | 4 |
| 12. Pleasurable and respectful interaction with the user | 13 | 5 | 7 | 1 | 42% | 3 |
| 13. Privacy | 1 | 1 | 0 | 0 | 100% | 1 |
| 14. Navigation | 2 | 0 | 2 | 0 | 0 | 4 |
| 15. Structure of information | 6 | 1 | 2 | 3 | 33% | 3 |
| 16. Extraordinary users | 3 | 0 | 1 | 2 | 0 | 3 |
| TOTAL | 96 | 22 | 44 | 30 | 33% |
The 96 items under the 16 heuristic criteria were marked by reviewers in terms of Yes, No and Not Applicable (N/A), and the severity of each potential problem on a scale of 1 to 4 (1-least importance, 4-high importance). A ‘Yes’ represented ‘Meets heuristics’, a ‘No’ represented ‘Does not meet heuristics’ and a ‘N/A’ represented ‘Heuristic not applicable’. A final value was assigned to each criteria along with its severity in the negotiation meeting between the reviewers. The number of Yes , No and N/A were calculated for each of the 16 heuristic and percentage of ‘Yes’ or ‘Agreement with heuristic criteria’ was then calculated within the applicable heuristics.
A heuristic evaluation is a commonly used usability evaluation method. It is carried out by a small set of evaluators examining a user interface and judging its compliance with a set of usability principles or heuristics. The checklist consisted of 16 usability heuristics (Pierotti, 2005; Sharp, Rogers, & Preece, 2007). Heuristics were chosen that applied to websites that have elderly individuals as their audience. For example, visibility of system status is improved if the data display provides feedback to the user about progress through the data or their current location in the system. A rating was given to each of the heuristic criteria using a 1 to 4 scale, from least important to most important potential problems recognized in the data display, respectively. The focus of the evaluation was the usability of the data displays. Two specific audience groups were considered in the evaluation, nurses and elderly residents. Individual reviews were conducted separately before the reviewers came together for a negotiation meeting to discuss each of the items under the criteria.
RESULTS
There were 96 items distributed under the 16 heuristic criteria. Thirty of these items were not applicable to the interface mostly because it is at a very nascent stage. One example of criteria determined to be not applicable by reviewers in our study included if the website was intended for a native English-speaking audience as well as an international audience. The display interface at this point is not being considered for an international audience so the criterion is considered not applicable. In the future, when the website is used for international audiences’ reviewers will determine if the language on the website avoids colloquialisms and slang resulting in fewer potential problems under this heuristic and a more usable interface.
The percent agreement with the applicable criteria was very low (33%) and disagreement was 67%. Eleven out of 16 of the heuristic criteria received a score of three or above indicating our interface has potential problems with high importance, which still require intervention to be considered highly usable. Conversely, less than half (5/16) received a 1 or 2 indicating potential problems with little importance, which have less affect on the overall usability of the interface. A summary of the percentage disagreement on each criteria are included in Table 1.
Heuristics recognized to have the most important potential problems for users (rating of 4) were flexibility and efficiency of use, help and documentation, navigation and skills. Availability of help and documentation data were also rated very poorly, including help and documentation instructions that allow users to drill down on specific areas within the data they want to assess. Navigation of the system was rated poorly because there was little feedback provided for users to know where they are in the system and where they should go to efficiently access other information. Additionally, in the interface too many windows open up and users get lost oftentimes closing the main window resulting in the need to reopen the website to continue browsing. Skills deficiencies were given because the data interface did not support all the skill levels necessary for all users, adults and elderly residents.
The highest ratings representing those areas with the least important potential problems (1) were given for heuristics related to ‘aesthetic value’ and ‘recognition rather than recall’. Aesthetic value was given a positive rating because the essential information for decision making was displayed prominently on the screens, icons used in the displays were clearly understood by reviewers, and data entry screens had short, simple, clear and distinctive titles directing users to choose the graphs they needed to view. The displays met the heuristic for ‘recognition rather than recall’ based upon ample visual contrast for the main parts of the website, use of visual cues (i.e. colors and graphs), features that emphasize quantity with graphic displays, grouping of related items, consistency of color coding and contrast between images and background. These areas are especially important for elderly residents who may have decreased color discrimination and poorer depth perception resulting from normal aging processes.
DISCUSSION
The value of usability assessment for these types of systems is that these systems most often get designed, marketed and implemented without much (or any) input from end users, especially healthcare consumers. The value of this paper was to describe an approach to usability assessment and show how, even after the researchers spent many meetings designing the sensor displays, it still didn't measure up to recommended guidelines. Our task force is using the results of this expert review to improve the sensor display by focusing on the areas recognized as having the most important potential for problems (ratings of 3 and 4 in Table 1). Future research will include more usability assessments of this interface focused on end users including healthcare providers who care for the elderly, family members of residents, and residents themselves who are eager to see what data is being captured by the sensors.
Especially, important for this study will be the development of help screens and documentation to train users on how to use the information system. Help documentation will support users who are both novice and expert and who are adults and elderly. Also improvements in the flexibility and efficiency of use of this data interface could be realized if better design features were included for novice and expert users of all age categories. Furthermore, we will be developing better designs to support the skills of the users; this includes using more distinct color variations so that elders with poor vision will be able to distinguish between colors on line graphs in charts. We will also be focused on developing better navigational feedback for users of the interface to let them know where they are presently in the system and where they should go to efficiently access other information in the system.
User Feedback
In a related study, residents were asked to discuss their experiences living with the sensors. Overall, there are positive perceptions of the sensor technology and there were no reports of interference with daily activities (Courtney, Demiris, Rantz, & Skubic, 2007; Demiris G et al., 2004). In conducting these interviews, three distinct phases were identified that residents experienced with the technology (Dickey, 2007). First, familiarization occurred when residents familiarized themselves with the installed technology and identified any issues or concerns. For instance a few residents reported bed sensors were noticeable when they slept; the research team addressed this issue by developing a new sheath that covered the sensor so that it was softer to lie on in bed. This familiarization phase lasted 2 to 3 weeks, and the novelty of the technology was obvious as residents were showing it to other residents. Adjustment and curiosity was the second phase which also lasted about 2 to 3 weeks. During this period residents continued to express curiosity about the sensors functions; one resident reported “I try to see if the lights are blinking...I often forget it is there, and then I will look”. Residents reported they did not show technology to visitors and most people did not notice. During integration, the third phase, residents stated they forgot about the technology, expressed no privacy concerns and felt that sensor monitoring provided a certain ease of mind and/or the sense of contributing to a generation of new knowledge (Demiris, Parker-Oliver, Dickey, Skubic & Rantz, 2008).
Advantages of interviewing residents and including their perceptions in the development of sensor technologies is to allow for assessment of residents’ perceptions, concerns and attitudes over time to increase understanding and acceptance of technology and to empower end users as their concerns and suggestions are being addressed by the systems designers (Demiris, Finkelstein, & Speedie, 2001). During the final phases of research now underway, the team will again include users’ perceptions of the sensor technology. However, we will take this approach one step further by including the visualization of sensor data by elder residents and their families through our newly developed computer displays.
GAPS IN CURRENT KNOWLEDGE
During preliminary work, we learned that residents who have used the sensor network have identified positive experiences with the technology; that residents’ and their families are eager to see the sensor data; the sensor system works reliably, continually detecting motion activities in residents’ apartments and on a few occasions, sensor data appears to have changed when a sentinel health event occurred. However, we are unable to verify the relationship between the sensor data changes and sentinel health events because residents’ have not been involved in the actual sensor data review when sentinel health events occurred. It is critical now that residents’ become involved in this evaluation process by identifying when sentinel health events occur and discussing their perceptions of the sensor data, this will provide means for us to validate the sensor network before we can further evaluate its usefulness and disseminate it widely to other settings.
CONCLUSION
The goal of this research is to expand on integrating sensor systems for monitoring elder residents. In order to accomplish our aims we are planning to use usability methods to help us understand how healthcare providers, residents and family members can use sensor networks to evaluate functional status by observing daily activity patterns recorded by sensors. We are interested in determining how sensor activity helps us to enhance the monitoring of functional status and activity levels in the lives of residents in assisted living facilities. Eventually we plan to use the sensor data system and interfaces to assist in the prediction of sentinel health events in elderly residents who want to age in place.
Acknowledgements
The project was supported by grant number K08HS016862 from the Agency for Healthcare Research and Quality (Alexander, PI); AOA Technology to Enhance Aging in Place at TigerPlace (Rantz, PI) grant number 90AM3013; and NSF Technology Interventions for Elders with Mobility and Cognitive Impairments (Skubic, PI) grant number 11S-0428420. The content is solely the responsibility of the authors and does not necessarily represent the official views of the Agency for Healthcare Research and Quality, the Administration on Aging, or the National Science Foundation.
We thank the Information Experience Laboratory, University of Missouri where the study was conducted.
We would also like to thank the Expert review team members – Dr. Sandra Erdelez, Borchuluun Yadamsuren, Jiazhen Wang, and Heather Hill, who helped in the Expert review.
Contributor Information
Gregory L. Alexander, University of Missouri Sinclair School of Nursing S415 Columbia, MO 65211 alexanderg@missouri.edu.
Marilyn Rantz, University of Missouri S406 Sinclair School of Nursing Columbia, MO 65211 rantzm@health.missouri.edu.
Marjorie Skubic, Center for Eldecare and Rehabilitation Technology 348 Engineering Building West University of Missouri Columbia, MO 65211 skubicm@missouri.edu.
Myra Aud, University of Missouri Sinclair School of Nursing Columbia, MO 65211 audm@missouri.edu.
Bonnie Wakefield, University of Missouri Sinclair School of Nursing Columbia, MO 65211 wakefieldb@missouri.edu.
Elena Florea, University of Missouri-Columbia Health Management and Informatics Department 601 S. Providence Rd. Apt. 709B Columbia, MO 65203 evfc99@mizzou.edu.
Anindita Paul, University of Missouri School of Information Science and Learning Technologies Columbia, MO 65211 Anindita.Paul@mizzou.edu.
Reference List
- Alexander NB, Guire KE, Thelen DG, Ashton-Miller JA, Schultz AB, Grunawalt JC, et al. Self-reported walking ability predicts functional mobility performance in frail older adults. Journal of the American Geriatrics Society. 2000;48:1408–1413. doi: 10.1111/j.1532-5415.2000.tb02630.x. [DOI] [PubMed] [Google Scholar]
- Aud MA. Resident with dementia in assisted living facilities: The role of behavior in discharge decisions. Journal of Gerontological Nursing. 2004;30:16–26. doi: 10.3928/0098-9134-20040601-06. [DOI] [PubMed] [Google Scholar]
- Boockvar KS, Lachs MS. Predictive value of nonspecific symptoms for acute illness in nursing home residents. Journal of the American Geriatrics Society. 2003;51:1111–1115. doi: 10.1046/j.1532-5415.2003.51360.x. [DOI] [PubMed] [Google Scholar]
- Chapin R, Dobbs-Kepper D. Aging in place in assisted living: Philosophy versus policy. The Gerontologist. 2001;41:43–50. doi: 10.1093/geront/41.1.43. [DOI] [PubMed] [Google Scholar]
- Demiris G, Parker-Oliver D, Dickey G, Skubic M, Rantz Findings from a participatory evaluation of a smart home application for older adults. Technology and Health Care. 2008;16(2):111–118. [PubMed] [Google Scholar]
- Demiris G, Rantz MJ, Aud MA, Marek KD, Tyrer HW, Skubic M, et al. Older adults’ attitudes towards and perceptions of ‘smart home’ technologies: a pilot study. Medical Informatics. 2004;29:87–94. doi: 10.1080/14639230410001684387. [DOI] [PubMed] [Google Scholar]
- Demiris G, Finkelstein SM, Speedie SM. Considerations for the design of a web-based clinical monitoring and educational system for elderly patients. Journal of the American Medical Informatics Association. 2001;8:468–472. doi: 10.1136/jamia.2001.0080468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fried LP, Bandeen-Roche K, Chaves PH, Johnson BA. Preclinical mobility disability predicts incident mobility disability in older women. Journals of Gerontology A Biological Science Medical Science. 2000;55:M43–M52. doi: 10.1093/gerona/55.1.m43. [DOI] [PubMed] [Google Scholar]
- Fried LP, Young Y, Rubin G, Bandeen-Roche K, WHAS II Collaborative Research Group Self-reported preclinical disability identifies older women with early declines in performance and early disease. Journal of Clinical Epidemiology. 2001;54:889–901. doi: 10.1016/s0895-4356(01)00357-2. [DOI] [PubMed] [Google Scholar]
- Hawes C, Phillips CD, Rose M, Holan S, Sheridan M. A national survey of assisted living facilities. The Gerontologist. 2003;43:875–882. doi: 10.1093/geront/43.6.875. [DOI] [PubMed] [Google Scholar]
- Hogan J. Why don't nurses monitor the respiratory rates of patients? British Journal of Nursing. 2006;15:489–492. doi: 10.12968/bjon.2006.15.9.21087. [DOI] [PubMed] [Google Scholar]
- Kissam S, Gifford DR, Vor V, Patry G. Admission and continued-stay criteria for assisted living facilities. Journal of the American Geriatrics Society. 2003;51:1651–1654. doi: 10.1046/j.1532-5415.2003.51519.x. [DOI] [PubMed] [Google Scholar]
- Onder G, Penninx BW, Ferrucci L, Fried LP, Guralnik JM, Pahor M. Measures of physical performance and risk for progressive and catastrophic disability: Results from the Women's Health and Aging Study. Journals of Gerontology A Biological Science Medical Science. 2005;60:74–79. doi: 10.1093/gerona/60.1.74. [DOI] [PubMed] [Google Scholar]
- Pierotti D. Heuristic Evaluation - A System Checklist. 2005 http://www.stcsig.org/usability/topics/articles/he-checklist.html [On-line]
- Rantz MJ, Dorman-Marek K, Aud MA, Tyrer HW, Skubic M, Demiris G, et al. A technology and nursing collaboration to help older adults age in place. Nursing Outlook. 2005;53:40–45. doi: 10.1016/j.outlook.2004.05.004. [DOI] [PubMed] [Google Scholar]
- Ridley S. The recognition and early management of critical illness. Annals of Coll Surgery England. 2005;87:315–322. doi: 10.1308/003588405X60669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sharp H, Rogers Y, Preece J. Interactive heuristic evaluation toolkit. 2007 http://www.id-book.com/catherb/index.htm [On-line]
- Tyrer HW, Aud MA, Alexander GL, Skubic M, Rantz M. Early detection of health changes in older adults.. Proceedings of the IEEE Engineering in Medicine and Biology; Lyon, France. 2007. pp. 4045–4048. [DOI] [PubMed] [Google Scholar]
- Wakefield BJ, Holman JE. Functional trajectories associated with hospitalization in older adults. Western Journal of Nursing Research. 2007;29:1–-17. doi: 10.1177/0193945906293809. [DOI] [PubMed] [Google Scholar]
- Wolinsky FD, Miller DK, Andresen EM, Malmstrom TK, Miller JP. Further evidence for the importance of subclinical functional limitation and subclinical disability assessment in gerontology and geriatrics. Journals of Gerontology B Psychology Social Sciences. 2005;60:S146–S151. doi: 10.1093/geronb/60.3.s146. [DOI] [PubMed] [Google Scholar]