Abstract
There is increasing evidence that cerebrovascular dysfunction plays a role not only in vascular causes of cognitive impairment but also in Alzheimer’s disease (AD). Vascular risk factors and AD impair the structure and function of cerebral blood vessels and associated cells (neurovascular unit), effects mediated by vascular oxidative stress and inflammation. Injury to the neurovascular unit alters cerebral blood flow regulation, depletes vascular reserves, disrupts the blood–brain barrier, and reduces the brain’s repair potential, effects that amplify the brain dysfunction and damage exerted by incident ischemia and coexisting neurodegeneration. Clinical-pathological studies support the notion that vascular lesions aggravate the deleterious effects of AD pathology by reducing the threshold for cognitive impairment and accelerating the pace of the dementia. In the absence of mechanism-based approaches to counteract cognitive dysfunction, targeting vascular risk factors and improving cerebrovascular health offers the opportunity to mitigate the impact of one of the most disabling human afflictions.
Introduction
Alzheimer’s disease (AD) and vascular dementia are the most common forms of cognitive impairment in the elderly [28]. The pathogenic mechanisms underlying these two conditions have traditionally been considered separate, even mutually exclusive [23]. At the time of Alois Alzheimer, dementia was most often attributed to vascular insufficiency or syphilis [70]. Over the next several decades, the emergence of AD as a distinct clinical-pathological entity established this condition as the prevailing cause of dementia. Biochemical, cellular, and molecular studies provided evidence that AD is caused by a neurodegenerative process leading to neuronal dysfunction and death related mainly to the amyloid-β peptide (Aβ) and hyperphosphorylation of the microtubule-associated protein tau [85]. Diagnostic criteria were drafted and widely applied, establishing AD as the predominant cause of senile cognitive impairment, a course of action aptly referred to as “alzheimerization” of dementia [70]. On the other hand, vascular dementia evolved from the concept of “arteriosclerotic dementia”, in which hardening of cerebral arteries leads to diffuse ischemia and neuronal loss [70], to “multiinfarct dementia”, caused by multiple infarcts resulting in cognitive impairment due to progressive brain loss [36]. In the early 1990s, the broader term “vascular cognitive impairment” (VCI) was introduced to encompass the wide spectrum of cognitive alterations associated with cerebrovascular pathologies, including more subtle deficits that would not fulfill AD criteria [35]. Standards for the diagnosis of VCI were established [13, 34, 86], and vascular causes of cognitive impairment have regained the attention of the basic and clinical neuroscience communities [23, 49]. In addition, it has become widely recognized that a large proportion of dementias is caused by mixed AD and vascular pathology, especially in older individuals [28, 50]. Importantly, coexistence of ischemic and neurodegenerative pathology was found to have a profound impact on the expression of the dementia, suggesting reciprocal interactions between ischemia and neurodegeneration [75, 102]. These observations, in concert with epidemiological studies indicating that AD and cerebrovascular diseases share the same risk factors [10], has revived the interest in the idea that vascular factors may play a role in the pathogenesis of AD [17, 43, 56]. This hypothesis has received support from experimental studies indicating that Aβ has potent cerebrovascular effects, and that hypoxia–ischemia is a powerful modulator of cerebral amyloidogenesis [41]. Both Aβ and vascular risk factors target the structure and function of cerebrovascular cells, glia, and neurons (neurovascular unit), resulting in neurovascular dysfunction. This brief review examines the neurovascular alterations underlying AD and VCI, and discusses their implications for the prevention and treatment of vascular and neurodegenerative dementia.
The neurovascular unit: the guardian of cerebral homeostasis
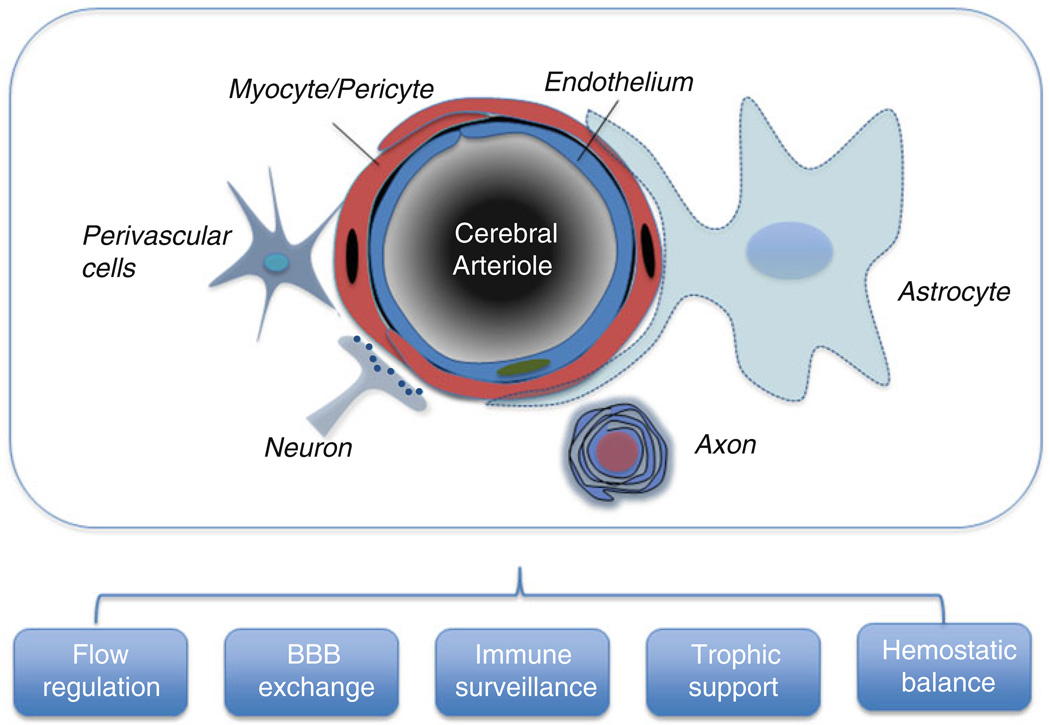
Neurons, glia, perivascular, and vascular cells, collectively termed the neurovascular unit, are closely interrelated and work in concert to maintain the homeostasis of the cerebral microenvironment (Fig. 1). Thus, the neurovascular unit regulates blood flow, controls the exchange across the blood–brain barrier (BBB), contributes to immune surveillance in the brain, and provides trophic support to brain cells.
Fig. 1.
The neurovascular unit is constituted by endothelial cells, myocytes, neurons and their processes, astrocytes, and perivascular cells (microglia, macrophages, mast cells, etc.). In arterioles and capillaries, the foot processes of astrocytes envelop the majority of the abluminal vascular surface. In capillaries, myocytes are replaced by pericytes. The function of the neurovascular unit is to maintain the homeostasis of the cerebral microenvironment. Thus, the neurovascular unit is involved in cerebral blood flow regulation, blood–brain barrier (BBB) exchange, immune surveillance, trophic support, and hemostatic balance. Cardiovascular risk factors and Aβ alter the structure and function of the neurovascular unit leading to neurovascular dysfunction
Blood flow regulation
The brain’s structural and functional integrity depends on a continuous and well-regulated blood supply, and interruption of cerebral blood flow (CBF) leads to brain dysfunction and death [74]. Consequently, the brain is equipped with control mechanisms that assure that the brain’s blood supply is well matched to its energetic needs [44]. Thus, neural activity induces a powerful increase in CBF (functional hyperemia) that is thought to deliver energy substrates and remove toxic byproducts of brain activity [83]. Astrocytes, whose end-feet encircle the outer wall of cerebral microvessels (arterioles, capillaries, and venules), act as a link between synaptic activity and the cerebrovascular cells mediating the increase in CBF [44]. Cerebrovascular autoregulation holds CBF relatively constant despite changes in perfusion pressure and protect cerebral perfusion from potentially damaging fluctuations in arterial pressure [114]. Specialized receptors on the endothelial cell membrane initiate intracellular signaling cascades in response to mechanical (shear stress), chemical (neurotransmitters and neuromodulators) and cellular (circulating immune cells) stimuli, and release potent signaling molecules, like nitric oxide, endothelin, and prostanoids [124]. These endothelial mediators contribute to local flow distribution [3] and to other functions of the neurovascular unit as well (see below).
Blood–brain barrier exchange
Owing to the tight junctions between cerebral endothelial cell, highly specialized endothelial membrane transporters regulate the trafficking of macromolecules, ions, amino acids, peptides, neurotransmitters, and other signaling molecules between the blood and the brain, which is at the basis of the BBB [1]. Transporters on the abluminal side of the vessel regulate the removal of metabolic byproducts form the brain. Relevant to the mechanisms of AD and VCI, the BBB plays a critical role in the transport of Aβ to and from the brain [132]. Thus, circulating Aβ is transported into the brain via receptors for advanced glycation products (RAGE) on endothelial cells [18]. Intracerebral Aβ, normally produced by synaptic activity [15], is cleared from the brain through vascular mechanisms involving the lipoprotein receptor protein 1 (LRP1) and P-glycoprotein, a process controlled by the serum response factor and myocardin [8, 14, 93].
Immune surveillance
Endothelial cells are able to detect blood-borne immune signals and express adhesion molecules (P- and E-selectin, intercellular adhesion molecule, vascular cell adhesion molecule, etc.) that recognize cognate molecules on circulating immune cells leading to the attachment and transmigration of these cells into the brain [118]. Cytokines produced by perivascular macrophages, endothelium, and glia regulate the expression of adhesion molecules, cytokines, and chemokines, and promote the trafficking of leukocytes across the BBB [64]. This process is vital both for immune surveillance in the normal brain and for the immune response of the brain to injury.
Hemostatic balance
Cells in the neurovascular unit play a critical role also in hemostatic balance. Whereas the prothrombotic effects of collagen and tissue factor in the vascular wall protect the tissue from hemorrhage, antithrombotic and profibrinolytic factors in the endothelium (NO, prostacylin, CD39, plasminogen activators, etc.) prevent vascular occlusion [29]. Furthermore, the cerebrovascular endothelium is involved in the removal of intravascular clots, a process that may reestablish flow after microvascular embolism [65].
Trophic function
Endothelial cells exert trophic actions that are essential to the well-being of neurons and glia [128]. In turn, neurons and glia produce growth factors that provide trophic support to vascular cells. Such reciprocal trophic interaction is critical during development when ephrins, slit ligands, semaphorins, and netrins act as guiding cues for both migrating axons and vessels [119]. Furthermore, after brain injury, growth factors released from endothelial cells like brain derived neurotrophic factor (BDNF), vascular endothelial derived growth factor (VEGF), stromal-derived factor 1, and angiopoietin-1 orchestrate the migration and differentiation of neuroblasts [16, 78, 101]. Therefore, the survival of vascular cells neurons and glia relies on reciprocal trophic interactions, and the proper functioning of the neurovascular unit depends on the health of all its cellular constituents.
The neurovascular unit in VCI and AD
The structure and function of the neurovascular unit are profoundly impaired in VCI and AD [9, 41]. These alterations disrupt the homeostasis of the cerebral microenvironment and promote the neuronal dysfunction underlying the impairment in cognition.
Structural alterations
Both VCI and AD are associated with marked alterations in cerebrovascular structure [57, 92, 120]. Large intracranial vessels exhibit atherosclerotic plaques not only in VCI but also in AD [7, 40]. At the microvascular level, arterioles and capillaries are reduced in number, tortuous, and have thickened basement membranes [11, 27, 92, 125]. The arteriolar wall exhibits degenerative changes and, in cases associated with hypertension, undergoes hyaline degeneration (lipohyalinosis), causing microhemorrhages [92]. In the periventricular white matter, a region prone to injury, reactive astrocytosis and microglial activation are associated with expression of hypoxia inducible genes, suggesting local energy deficit [27, 99]. In AD or in cerebral amyloid angiopathy (CAA), accumulation of Aβ in the media of cortical arterioles leads to weakening of the vessel wall, increasing the chance of lobar hemorrhages [120].
Cerebrovascular dysregulation
Animal and human studies indicate that risk factors for VCI and AD, such as hypertension, aging, dyslipidemia, and diabetes, have profound effects on cerebrovascular regulation, and disrupt endothelium-dependent vasodilatation, functional hyperemia, and autoregulation [42, 53, 60, 66, 73, 80, 91]. Similarly, Aβ is a potent vasoconstrictor [111], and impairs the fundamental mechanisms regulating the cerebral circulation [45, 76, 77]. CBF is reduced, and functional hyperemia is attenuated in patients with AD [6, 47, 54, 72, 84, 87, 108, 117, 127]. Furthermore, endothelial-dependent responses are impaired in systemic vessels of patients with AD [20]. Cerebral smooth muscle cells have a hypercontractile phenotype [12], which increases the constrictor tone of cerebral arteries and contributes to reduce resting CBF and its reactivity [41]. Vascular oxidative stress and inflammation have emerged as key pathogenic factors in neurovascular dysfunction [25, 42, 98]. In particular, experimental studies suggest that free radicals produced by the enzyme NADPH oxidase are responsible for the cerebrovascular alterations induced by VCI risk factors and Aβ [59, 61, 80, 81]. Free radicals can trigger inflammation by activating redox sensitive transcription factors, like NFkb and AP1. In addition, the endothelial dysfunction induced by oxidative stress can lead to release of VEGF and prostanoids, which promote vascular leakage, protein extravasation, and inflammation [71]. Inflammation, in turn, enhances oxidative stress by upregulating the expression of free radical-producing enzymes and by downregulating antioxidant defenses [30]. Inflammation and oxidative stress not only affect CBF regulation, but, as discussed below, have a profound impact on the other functions of the neurovascular unit as well.
Blood–brain barrier dysfunction
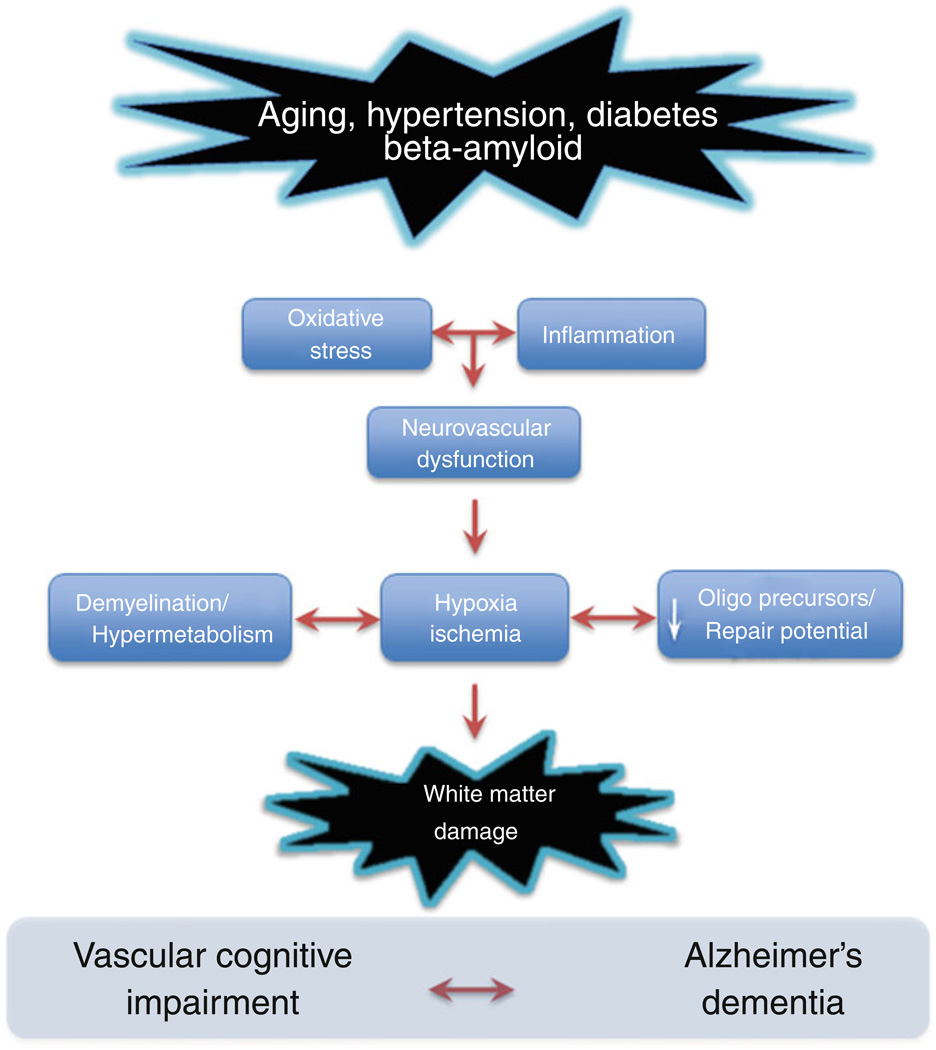
Alteration of the BBB is an early finding in white matter lesions associated with VCI and AD [26, 132]. Extravasation of plasma protein triggers vascular inflammation, oxidative stress, perivascular edema, and axonal demyelination [26] (Fig. 2). Demyelination slows the transmission of nerve impulses, and contributes to the neural dysfunction that underlies cognitive impairment. In addition, in models of multiple sclerosis, the loss of saltatory conduction between nodes of Ranvier induced by demyelination, coupled with the expression of leaky Na+ channels on denuded axons, increases the inefficiency of action potential conduction [113]. Therefore, demyelination increases the oxygen demands of axons and enhances the local energy deficit and hypoxia [113]. A similar process could take place in the white matter lesions observed in AD and VCI [28], but additional evidence of demyelination with axonal preservation is needed to establish this point more firmly, especially in AD [46].
Fig. 2.
Mechanisms of white matter damage produced by cardiovascular risk factors and Aβ. Oxidative stress and inflammation induced by these factors are responsible for disruption of the functions of the neurovascular unit (see Fig. 1), which, in turn, leads to local hypoxia–ischemia, axonal demyelination, and reduced repair potential of the white matter by altering oligodendrocyte progenitor cells. Data in autoimmune models of demyelination suggest that loss of myelin increases the energy consumption of the affected axons and aggravates local hypoxia. The resulting white matter damage contributes to both VCI and AD
Alterations in BBB transport processes may also have an impact on the brain accumulation of Aβ in patients with AD [55, 132]. The downregulation of the BBB receptors LRP-1 and P-glycoprotein promotes vascular Aβ deposition and may worsen the vascular dysfunction [8]. Furthermore, elevated circulating levels of Aβ in patients with VCI and AD could also promote cerebrovascular insufficiency, inflammation, and oxidative stress, and play a role in the white matter alterations observed in both conditions [31, 33] (Fig. 2).
Loss of trophic support
Vascular oxidative stress, aging, and inflammation disrupt neurovascular trophic function [16]. Pro-inflammatory cytokines impair growth factor signaling inducing a state of “neurotrophin resistance” [112, 115]. Furthermore, oxidative stress attenuates the growth factor support provided by endothelial cells to oligodendrocyte precursors [4]. Loss of trophic support may impede the proliferation, migration, and differentiation of oligodendrocyte progenitor cells, and compromise the repair of the damaged white matter in AD and VCI [5, 79, 96, 97] (Fig. 2). Loss of neurovascular trophic support is also observed in AD. Inflammation and oxidative stress can result in neurotrophin resistance (see above), but other factors also contribute to impair trophic support at the microvascular level. For example, the homeobox gene MEOX, critical for vascular differentiation, is suppressed in patients with AD and may mediate the cerebral microvascular rarefaction observed in this disease [125]. Aβ induces endothelial cell autophagy [37], and inhibits vasculogenesis, effects mediated by inhibition of VEGF signaling [82]. In AD patients, the perivascular accumulation of endostatin, a neurally derived antiangiogenic factor, may also contribute to the vascular damage [21]. Although CSF levels of VEGF are increased in AD [109], brain VEGF is sequestered by amyloid plaques [126], reducing its bioactivity. Furthermore, BDNF levels are low in AD brains [94]. Collectively, these alterations in growth factors expression, localization, and signaling are likely to have a major impact not only in the vascular alterations observed in AD and VCI, but also in the brain atrophy associated with these conditions [88, 106].
Interactions between ischemia and neurodegeneration
The profound effects of cerebrovascular risk factors and Aβ on the neurovascular unit suggest a pathogenic link between ischemia and neurodegeneration [48]. The pathological changes characteristic of AD, i.e., amyloid plaques and neurofibrillary tangles, are observed together with vascular pathology (subcortical white matter lesions, lacunes, infarcts, etc.) in more than 40% of elderly demented individuals [49]. This finding is not surprising since both neurodegenerative and ischemic changes are common in the elderly and would be anticipated to coexist in a large number of cases [48]. Volume of ischemic lesions and their location play a critical role in the expression of the dementia in mixed cases [49]. Nevertheless, the coexistence of ischemic and neurodegenerative pathologies raises a number of questions related to their effects on cognition, and has important implications for the prevention, diagnosis, and treatment of VCI and AD.
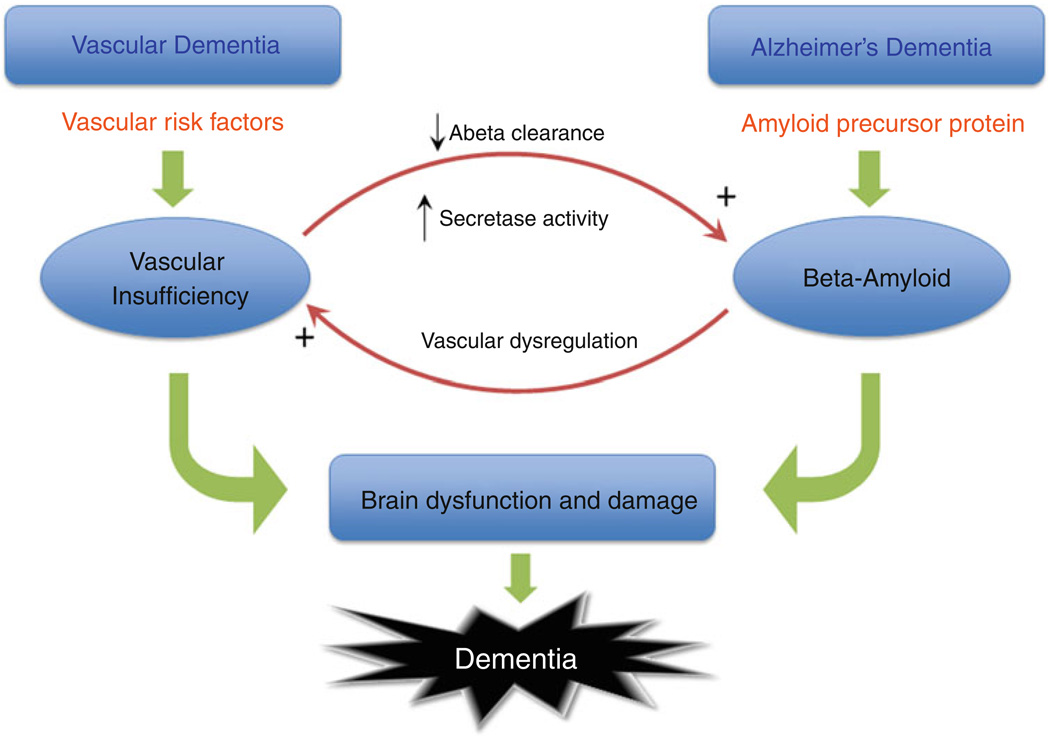
Does vascular insufficiency promote neurodegenerative changes and vice versa?
Ischemia may promote Aβ accumulation by reducing the vascular clearance of this peptide, its major elimination pathway [15, 19]. In addition, hypoxia and/or ischemia promote the cleavage of Aβ from the amyloid precursor protein (APP) by upregulating β-secretase expression and activity [62, 69, 107, 110, 121, 131]. These experimental findings indicate that increased production and reduced clearance could enhance Aβ deposition in brain and favor the formation of amyloid plaques and CAA (Fig. 3). Indeed, brain Aβ levels and amyloid plaques are elevated in patients with cerebrovascular insufficiency and VCI [68]. On the other hand, the cerebrovascular dysfunction induced by Aβ could threaten cerebral perfusion, reduce vascular reserves, and increase the propensity to ischemic damage. Consistent with this hypothesis, focal cerebral ischemia produces larger infarcts in mice overexpressing APP [63, 130], an effect associated with Aβ-induced vascular dysregulation, reduced collateral flow, and more severe ischemia [130]. Similarly, patients with AD have heavier burden of cerebrovascular lesions [51]. Paradoxically, some cardiovascular risk factors can increase the risk of AD without aggravating neurodegenerative pathology. For example, diabetes mellitus doubles the risk of AD without a corresponding increase in plaques and tangles [58, 104]. Rather, a prominent increase in microinfarcts is observed [58], suggesting that the effect of diabetes on AD risk is related to microvascular lesions that amplify the consequences of the neurodegenerative pathology [58]. The interaction between vascular lesions and neurofibrillary tangles is less well understood. Focal cerebral ischemia promotes tau phosphorylation in animal models [122], and hypertension increases neurofibrillary tangles in the hippocampus of non-demented elderly persons [105], suggesting a link between tau hyperphosphorylation and vascular factors. But, in triple transgenic mice expressing plaques and tangles, transient cerebral hypoperfusion, a more global yet milder ischemic insult, reduces tau levels [62]. Although this finding is reminiscent of the reduced neurofibrillary tangles observed in patients with mixed dementia [32, 75], to what extent ischemia modulates neurofilament dynamics and phosphorylation remains unclear. Therefore, while there is evidence that ischemia promotes Aβ accumulation by enhancing production and reducing its clearance, the impact that ischemia exerts on tau pathology is less well understood.
Fig. 3.
In vascular dementia, cerebrovascular risk factors induce neurovascular dysfunction (see Fig. 2), leading to cerebrovascular insufficiency, which, in turn, leads to brain dysfunction and damage. In AD, cleavage of the amyloid precursor protein by β- and γ-secretases leads to Aβ accumulation, which also causes brain dysfunction and damage. Although individually these pathways are capable of inducing cognitive impairment, their interaction enhances their pathogenic effects. Thus, Aβ induces vascular dysregulation and aggravates the vascular insufficiency, thereby enhancing the brain dysfunction and damage associated with vascular risk factors. On the other hand, the hypoxia–ischemia resulting from the vascular insufficiency increases Aβ cleavage from APP and reduces Aβ clearance through the cerebral vasculature, promoting Aβ accumulation and the attendant deleterious effects on the brain
Does the vascular pathology worsen the cognitive dysfunction in AD?
Ischemic lesions enhance the severity of the dementia in AD patients. Thus, most studies, with notable exceptions [67], found that moderate AD pathology has a much greater cognitive impact in patients who also exhibit basal ganglia lacunes, ischemic white matter lesions, symptomatic, or silent infarcts [39, 75, 89, 102, 103, 116, 123]. The effect of vascular lesions is more pronounced in patients in the early stages of AD [24, 90]. In addition, ischemic lesions and vascular risk factors also accelerate the tempo of the dementia [38]. AD patients with a reduced cerebrovascular reactivity to hypercapnia, an index of cerebrovascular function, have a more rapid cognitive decline [95], linking disease progression with cerebrovascular dysfunction. Therefore, coexisting cerebrovascular disease or incident ischemic lesions may shorten the preclinical stage of AD and accelerate disease progression.
Are the cognitive effects of vascular and AD pathology additive or synergistic?
In mixed dementias, the vascular pathology may worsen the cognitive effects of neurodegeneration by different mechanisms. Neurodegeneration and ischemic lesions could contribute independently to the dementia, the cumulative cognitive decline being the sum of the deleterious cognitive effects exerted by each pathology (additive effects). Alternatively, the vascular pathology could interact synergistically with the neurodegenerative changes resulting in a cognitive decline greater than that produced by each pathology alone (synergistic effects). Furthermore, there could be a “pathogenic” synergy between the two disease processes, such that the tissue damage produced by vascular factors could enhance the damage produced by neurodegeneration and vice versa. The evidence reviewed above indicates that synergistic pathogenic interaction between vascular and neurodegenerative pathologies is biologically plausible because in animal models ischemia promotes Aβ accumulation and, in turn, Aβ aggravates ischemic injury (Fig. 3). The observation that patients with AD have more cerebrovascular lesions at autopsy [51] would support this possibility. Furthermore, with exceptions [2], cerebrovascular insufficiency has been reported to promote formation of amyloid plaques [52]. On the other hand, synergistic effects on cognition are suggested by clinical-pathological studies demonstrating that minimal cerebrovascular pathology worsens the cognitive impact of mild AD pathology [24, 102, 129]. However, in patients with more severe vascular and AD lesions, the cognitive effects seem to be additive [90]. Therefore, it is likely that both additive and synergistic effects can be observed depending on the magnitude of vascular and neurodegenerative pathology and the stage of evolution of the disease process.
In conclusion, vascular lesions are detrimental to cognitive function either by directly damaging neural pathways involved in higher integrated functions or by worsening the impact of AD pathology. Considering that modifiable vascular risk factors can be controlled, approaches to treat dementia should rely heavily on strategies to preserve cerebrovascular health. In support of this approach, treatment of vascular risk factors in AD patients slows down the cognitive decline [22]. A healthy diet and exercise can help minimize the deleterious effects of cardiovascular risk factors and have a positive effect on cognition [16, 100]. In the absence of specific interventions targeting the mechanisms of vascular or neurodegenerative dementia, lifestyle modification and risk factor control may be valuable initial steps to mitigate the cognitive decline associated both with AD and VCI.
Acknowledgments
Supported by NIH grants NS37806 and HL96571.
References
- 1.Abbott NJ, Patabendige AAK, Dolman DEM, Yusof SR, Begley DJ. Structure and function of the blood-brain barrier. Neurobiol Dis. 2010;37:13–25. doi: 10.1016/j.nbd.2009.07.030. [DOI] [PubMed] [Google Scholar]
- 2.Aho L, Jolkkonen J, Alafuzoff I. Beta-amyloid aggregation in human brains with cerebrovascular lesions. Stroke. 2006;37:2940–2945. doi: 10.1161/01.STR.0000248777.44128.93. [DOI] [PubMed] [Google Scholar]
- 3.Andresen J, Shafi NI, Bryan RM., Jr Endothelial influences on cerebrovascular tone. J Appl Physiol. 2006;100:318–327. doi: 10.1152/japplphysiol.00937.2005. [DOI] [PubMed] [Google Scholar]
- 4.Arai K, Lo EH. An oligovascular niche: cerebral endothelial cells promote the survival and proliferation of oligodendrocyte precursor cells. J Neurosci. 2009;29:4351–4355. doi: 10.1523/JNEUROSCI.0035-09.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Arai K, Lo EH. Astrocytes protect oligodendrocyte precursor cells via MEK/ERK and PI3K/Akt signaling. J Neurosci Res. 2010;88:758–763. doi: 10.1002/jnr.22256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bateman GA, Levi CR, Schofield P, Wang Y, Lovett EC. Quantitative measurement of cerebral haemodynamics in early vascular dementia and Alzheimer’s disease. J Clin Neurosci. 2006;13:563–568. doi: 10.1016/j.jocn.2005.04.017. [DOI] [PubMed] [Google Scholar]
- 7.Beach TG, Wilson JR, Sue LI, et al. Circle of Willis atherosclerosis: association with Alzheimer’s disease, neuritic plaques and neurofibrillary tangles. Acta Neuropathol. 2007;113:13–21. doi: 10.1007/s00401-006-0136-y. [DOI] [PubMed] [Google Scholar]
- 8.Bell RD, Deane R, Chow N, et al. SRF and myocardin regulate LRP-mediated amyloid-beta clearance in brain vascular cells. Nat Cell Biol. 2009;11:143–153. doi: 10.1038/ncb1819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bell RD, Zlokovic BV. Neurovascular mechanisms and blood-brain barrier disorder in Alzheimer’s disease. Acta Neuropathol. 2009;118:103–113. doi: 10.1007/s00401-009-0522-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Breteler MM. Vascular risk factors for Alzheimer’s disease: an epidemiologic perspective. Neurobiol Aging. 2000;21:153–160. doi: 10.1016/s0197-4580(99)00110-4. [DOI] [PubMed] [Google Scholar]
- 11.Brown WR, Moody DM, Thore CR, Challa VR, Anstrom JA. Vascular dementia in leukoaraiosis may be a consequence of capillary loss not only in the lesions, but in normal-appearing white matter and cortex as well. J Neurol Sci. 2007;257:62–66. doi: 10.1016/j.jns.2007.01.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Chow N, Bell RD, Deane R, et al. Serum response factor and myocardin mediate arterial hypercontractility and cerebral blood flow dysregulation in Alzheimer’s phenotype. Proc Natl Acad Sci USA. 2007;104:823–828. doi: 10.1073/pnas.0608251104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Chui HC, Victoroff JI, Margolin D, et al. Criteria for the diagnosis of ischemic vascular dementia proposed by the State of California Alzheimer’s Disease Diagnostic and Treatment Centers. Neurology. 1992;42:473–480. doi: 10.1212/wnl.42.3.473. [DOI] [PubMed] [Google Scholar]
- 14.Cirrito JR, Deane R, Fagan AM, et al. P-glycoprotein deficiency at the blood-brain barrier increases amyloid-beta deposition in an Alzheimer disease mouse model. J Clin Invest. 2005;115:3285–3290. doi: 10.1172/JCI25247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Cirrito JR, Yamada KA, Finn MB, et al. Synaptic activity regulates interstitial fluid amyloid-beta levels in vivo. Neuron. 2005;48:913–922. doi: 10.1016/j.neuron.2005.10.028. [DOI] [PubMed] [Google Scholar]
- 16.Cotman CW, Berchtold NC, Christie L-A. Exercise builds brain health: key roles of growth factor cascades and inflammation. Trends Neurosci. 2007;30:464–472. doi: 10.1016/j.tins.2007.06.011. [DOI] [PubMed] [Google Scholar]
- 17.de la Torre JC, Mussivand T. Can disturbed brain microcirculation cause Alzheimer’s disease? Neurol Res. 1993;15:146–153. doi: 10.1080/01616412.1993.11740127. [DOI] [PubMed] [Google Scholar]
- 18.Deane R, Du Yan S, Submamaryan RK, et al. RAGE mediates amyloid-beta peptide transport across the blood-brain barrier and accumulation in brain. Nat Med. 2003;9:907–913. doi: 10.1038/nm890. [DOI] [PubMed] [Google Scholar]
- 19.Deane R, Wu Z, Sagare A, et al. LRP/amyloid beta-peptide interaction mediates differential brain efflux of Abeta isoforms. Neuron. 2004;43:333–344. doi: 10.1016/j.neuron.2004.07.017. [DOI] [PubMed] [Google Scholar]
- 20.Dede DS, Yavuz B, Yavuz BB, et al. Assessment of endothelial function in Alzheimer’s disease: is Alzheimer’s disease a vascular disease? J Am Geriatr Soc. 2007;55:1613–1617. doi: 10.1111/j.1532-5415.2007.01378.x. [DOI] [PubMed] [Google Scholar]
- 21.Deininger MH, Fimmen BA, Thal DR, Schluesener HJ, Meyermann R. Aberrant neuronal and paracellular deposition of endostatin in brains of patients with Alzheimer’s disease. J Neurosci. 2002;22:10621–10626. doi: 10.1523/JNEUROSCI.22-24-10621.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Deschaintre Y, Richard F, Leys D, Pasquier F. Treatment of vascular risk factors is associated with slower decline in Alzheimer disease. Neurology. 2009;73:674–680. doi: 10.1212/WNL.0b013e3181b59bf3. [DOI] [PubMed] [Google Scholar]
- 23.Erkinjuntti T, Gauthier S. The concept of vascular cognitive impairment. Front Neurol Neurosci. 2009;24:79–85. doi: 10.1159/000197886. [DOI] [PubMed] [Google Scholar]
- 24.Esiri MM, Nagy Z, Smith MZ, Barnetson L, Smith AD. Cerebrovascular disease and threshold for dementia in the early stages of Alzheimer’s disease. Lancet. 1999;354:919–920. doi: 10.1016/S0140-6736(99)02355-7. [DOI] [PubMed] [Google Scholar]
- 25.Faraci FM. Reactive oxygen species: influence on cerebral vascular tone. J Appl Physiol. 2006;100:739–743. doi: 10.1152/japplphysiol.01044.2005. [DOI] [PubMed] [Google Scholar]
- 26.Farrall AJ, Wardlaw JM. Blood-brain barrier: ageing and microvascular disease-systematic review and meta-analysis. Neurobiol Aging. 2009;30:337–352. doi: 10.1016/j.neurobiolaging.2007.07.015. [DOI] [PubMed] [Google Scholar]
- 27.Fernando MS, Simpson JE, Matthews F, et al. White matter lesions in an unselected cohort of the elderly: molecular pathology suggests origin from chronic hypoperfusion injury. Stroke. 2006;37:1391–1398. doi: 10.1161/01.STR.0000221308.94473.14. [DOI] [PubMed] [Google Scholar]
- 28.Fotuhi M, Hachinski V, Whitehouse PJ. Changing perspectives regarding late-life dementia. Nat Rev Neurol. 2009;5:649–658. doi: 10.1038/nrneurol.2009.175. [DOI] [PubMed] [Google Scholar]
- 29.Furie B, Furie BC. Mechanisms of thrombus formation. N Engl J Med. 2008;359:938–949. doi: 10.1056/NEJMra0801082. [DOI] [PubMed] [Google Scholar]
- 30.Gill R, Tsung A, Billiar T. Linking oxidative stress to inflammation: Toll-like receptors. Free Radic Biol Med. 2010;48:1121–1132. doi: 10.1016/j.freeradbiomed.2010.01.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Gomis M, Sobrino T, Ois A, et al. Plasma beta-amyloid 1–40 is associated with the diffuse small vessel disease subtype. Stroke. 2009;40:3197–3201. doi: 10.1161/STROKEAHA.109.559641. [DOI] [PubMed] [Google Scholar]
- 32.Goulding JM, Signorini DF, Chatterjee S, et al. Inverse relation between Braak stage and cerebrovascular pathology in Alzheimer predominant dementia. J Neurol Neurosurg Psychiatry. 1999;67:654–657. doi: 10.1136/jnnp.67.5.654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Gurol ME, Irizarry MC, Smith EE, et al. Plasma beta-amyloid and white matter lesions in AD, MCI, and cerebral amyloid angiopathy. Neurology. 2006;66:23–29. doi: 10.1212/01.wnl.0000191403.95453.6a. [DOI] [PubMed] [Google Scholar]
- 34.Hachinski V, Iadecola C, Petersen RC, et al. National Institute of Neurological Disorders and Stroke-Canadian Stroke Network vascular cognitive impairment harmonization standards. Stroke. 2006;37:2220–2241. doi: 10.1161/01.STR.0000237236.88823.47. [DOI] [PubMed] [Google Scholar]
- 35.Hachinski VC, Bowler JV. Vascular dementia. Neurology. 1993;43:2159–2160. doi: 10.1212/wnl.43.10.2159-a. author reply 2160–2161. [DOI] [PubMed] [Google Scholar]
- 36.Hachinski VC, Lassen NA, Marshall J. Multi-infarct dementia. A cause of mental deterioration in the elderly. Lancet. 1974;2:207–210. doi: 10.1016/s0140-6736(74)91496-2. [DOI] [PubMed] [Google Scholar]
- 37.Hayashi S, Sato N, Yamamoto A, et al. Alzheimer disease-associated peptide, amyloid beta40, inhibits vascular regeneration with induction of endothelial autophagy. Arterioscler Thromb Vasc Biol. 2009;29:1909–1915. doi: 10.1161/ATVBAHA.109.188516. [DOI] [PubMed] [Google Scholar]
- 38.Helzner EP, Luchsinger JA, Scarmeas N, et al. Contribution of vascular risk factors to the progression in Alzheimer disease. Arch Neurol. 2009;66:343–348. doi: 10.1001/archneur.66.3.343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Heyman A, Fillenbaum GG, Welsh-Bohmer KA, et al. Cerebral infarcts in patients with autopsy-proven Alzheimer’s disease: CERAD, part XVIII. Consortium to Establish a Registry for Alzheimer’s Disease. Neurology. 1998;51:159–162. doi: 10.1212/wnl.51.1.159. [DOI] [PubMed] [Google Scholar]
- 40.Honig LS, Kukull W, Mayeux R. Atherosclerosis and AD: analysis of data from the US National Alzheimer’s Coordinating Center. Neurology. 2005;64:494–500. doi: 10.1212/01.WNL.0000150886.50187.30. [DOI] [PubMed] [Google Scholar]
- 41.Iadecola C. Neurovascular regulation in the normal brain and in Alzheimer’s disease. Nat Rev Neurosci. 2004;5:347–360. doi: 10.1038/nrn1387. [DOI] [PubMed] [Google Scholar]
- 42.Iadecola C, Davisson RL. Hypertension and cerebrovascular dysfunction. Cell Metab. 2008;7:476–484. doi: 10.1016/j.cmet.2008.03.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Iadecola C, Gorelick PB. Converging pathogenic mechanisms in vascular and neurodegenerative dementia. Stroke. 2003;34:335–337. doi: 10.1161/01.str.0000054050.51530.76. [DOI] [PubMed] [Google Scholar]
- 44.Iadecola C, Nedergaard M. Glial regulation of the cerebral microvasculature. Nat Neurosci. 2007;10:1369–1376. doi: 10.1038/nn2003. [DOI] [PubMed] [Google Scholar]
- 45.Iadecola C, Zhang F, Niwa K, et al. SOD1 rescues cerebral endothelial dysfunction in mice overexpressing amyloid precursor protein. Nat Neurosci. 1999;2:157–161. doi: 10.1038/5715. [DOI] [PubMed] [Google Scholar]
- 46.Ihara M, Polvikoski TM, Hall R, et al. Quantification of myelin loss in frontal lobe white matter in vascular dementia, Alzheimer’s disease, and dementia with Lewy bodies. Acta Neuropathol. 2010;119:579–589. doi: 10.1007/s00401-009-0635-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Jagust WJ, Haan MN, Reed BR, Eberling JL. Brain perfusion imaging predicts survival in Alzheimer’s disease. Neurology. 1998;51:1009–1013. doi: 10.1212/wnl.51.4.1009. [DOI] [PubMed] [Google Scholar]
- 48.Jellinger KA. The enigma of mixed dementia. Alzheimers Dement. 2007;3:40–53. doi: 10.1016/j.jalz.2006.09.002. [DOI] [PubMed] [Google Scholar]
- 49.Jellinger KA. Morphologic diagnosis of “vascular dementia”—a critical update. J Neurol Sci. 2008;270:1–12. doi: 10.1016/j.jns.2008.03.006. [DOI] [PubMed] [Google Scholar]
- 50.Jellinger KA, Attems J. Prevalence of dementia disorders in the oldest-old: an autopsy study. Acta Neuropathol. 2010;119:421–433. doi: 10.1007/s00401-010-0654-5. [DOI] [PubMed] [Google Scholar]
- 51.Jellinger KA, Mitter-Ferstl E. The impact of cerebrovascular lesions in Alzheimer disease—a comparative autopsy study. J Neurol. 2003;250:1050–1055. doi: 10.1007/s00415-003-0142-0. [DOI] [PubMed] [Google Scholar]
- 52.Jendroska K, Poewe W, Daniel SE, et al. Ischemic stress induces deposition of amyloid beta immunoreactivity in human brain. Acta Neuropathol. 1995;90:461–466. doi: 10.1007/BF00294806. [DOI] [PubMed] [Google Scholar]
- 53.Jennings JR, Muldoon MF, Ryan C, et al. Reduced cerebral blood flow response and compensation among patients with untreated hypertension. Neurology. 2005;64:1358–1365. doi: 10.1212/01.WNL.0000158283.28251.3C. [DOI] [PubMed] [Google Scholar]
- 54.Johnson KA, Albert MS. Perfusion abnormalities in prodromal AD. Neurobiol Aging. 2000;21:289–292. doi: 10.1016/s0197-4580(00)00137-8. [DOI] [PubMed] [Google Scholar]
- 55.Kalaria RN. The blood-brain barrier and cerebral microcirculation in Alzheimer disease. Cerebrovasc Brain Metab Rev. 1992;4:226–260. [PubMed] [Google Scholar]
- 56.Kalaria RN. The role of cerebral ischemia in Alzheimer’s disease. Neurobiol Aging. 2000;21:321–330. doi: 10.1016/s0197-4580(00)00125-1. [DOI] [PubMed] [Google Scholar]
- 57.Kalaria RN. Linking cerebrovascular defense mechanisms in brain ageing and Alzheimer’s disease. Neurobiol Aging. 2009;30:1512–1514. doi: 10.1016/j.neurobiolaging.2007.10.020. [DOI] [PubMed] [Google Scholar]
- 58.Kalaria RN. Neurodegenerative disease: diabetes, microvascular pathology and Alzheimer disease. Nat Rev Neurol. 2009;5:305–306. doi: 10.1038/nrneurol.2009.72. [DOI] [PubMed] [Google Scholar]
- 59.Kazama K, Anrather J, Zhou P, et al. Angiotensin II impairs neurovascular coupling in neocortex through NADPH-oxidase-derived radicals. Circ Res. 2004;95:1019–1026. doi: 10.1161/01.RES.0000148637.85595.c5. [DOI] [PubMed] [Google Scholar]
- 60.Kim YS, Immink RV, Stok WJ, et al. Dynamic cerebral autoregulatory capacity is affected early in Type 2 diabetes. Clin Sci. 2008;115:255–262. doi: 10.1042/CS20070458. [DOI] [PubMed] [Google Scholar]
- 61.Kitayama J, Faraci FM, Lentz SR, Heistad DD. Cerebral vascular dysfunction during hypercholesterolemia. Stroke. 2007;38:2136–2141. doi: 10.1161/STROKEAHA.107.481879. [DOI] [PubMed] [Google Scholar]
- 62.Koike MA, Green KN, Blurton-Jones M, LaFerla FM. Oligemic hypoperfusion differentially affects tau and amyloid-{beta} Am J Pathol. 2010 doi: 10.2353/ajpath.2010.090750. doi: 10.2353/ajpath.2010.090750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Koistinaho M, Kettunen MI, Goldsteins G, et al. Beta-amyloid precursor protein transgenic mice that harbor diffuse A beta deposits but do not form plaques show increased ischemic vulnerability: role of inflammation. Proc Natl Acad Sci USA. 2002;99:1610–1615. doi: 10.1073/pnas.032670899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Konsman JP, Drukarch B, Van Dam A-M. (Peri)vascular production and action of pro-inflammatory cytokines in brain pathology. Clin Sci. 2007;112:1–25. doi: 10.1042/CS20060043. [DOI] [PubMed] [Google Scholar]
- 65.Lam CK, Yoo T, Hiner B, Liu Z, Grutzendler J. Embolus extravasation is an alternative mechanism for cerebral microvascular recanalization. Nature. 2010;465:478–482. doi: 10.1038/nature09001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Last D, Alsop DC, Abduljalil AM, et al. Global and regional effects of type 2 diabetes on brain tissue volumes and cerebral vasoreactivity. Diabetes Care. 2007;30:1193–1199. doi: 10.2337/dc06-2052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Lee JH, Olichney JM, Hansen LA, Hofstetter CR, Thal LJ. Small concomitant vascular lesions do not influence rates of cognitive decline in patients with Alzheimer disease. Arch Neurol. 2000;57:1474–1479. doi: 10.1001/archneur.57.10.1474. [DOI] [PubMed] [Google Scholar]
- 68.Lewis H, Beher D, Cookson N, et al. Quantification of Alzheimer pathology in ageing and dementia: age-related accumulation of amyloid-beta(42) peptide in vascular dementia. Neuropathol Appl Neurobiol. 2006;32:103–118. doi: 10.1111/j.1365-2990.2006.00696.x. [DOI] [PubMed] [Google Scholar]
- 69.Li L, Zhang X, Yang D, et al. Hypoxia increases Abeta generation by altering beta- and gamma-cleavage of APP. Neurobiol Aging. 2009;30:1091–1098. doi: 10.1016/j.neurobiolaging.2007.10.011. [DOI] [PubMed] [Google Scholar]
- 70.Libon DJ, Price CC, Heilman KM, Grossman M. Alzheimer’s “other dementia”. Cogn Behav Neurol. 2006;19:112–116. doi: 10.1097/01.wnn.0000209870.69522.a3. [DOI] [PubMed] [Google Scholar]
- 71.Marchesi C, Paradis P, Schiffrin EL. Role of the reninangiotensin system in vascular inflammation. Trends Pharmacol Sci. 2008;29:367–374. doi: 10.1016/j.tips.2008.05.003. [DOI] [PubMed] [Google Scholar]
- 72.Mentis MJ, Alexander GE, Krasuski J, et al. q. Increasing required neural response to expose abnormal brain function in mild versus moderate or severe Alzheimer’s disease: PET study using parametric visual stimulation. Am J Psychiatry. 1998;155:785–794. doi: 10.1176/ajp.155.6.785. [DOI] [PubMed] [Google Scholar]
- 73.Modrick ML, Didion SP, Sigmund CD, Faraci FM. Role of oxidative stress and AT1 receptors in cerebral vascular dysfunction with aging. Am J Physiol Heart Circ Physiol. 2009;296:H1914–H1919. doi: 10.1152/ajpheart.00300.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Moskowitz MA, Lo EH, Iadecola C. The science of stroke: mechanisms in search of treatments. Neuron. 2010 doi: 10.1016/j.neuron.2010.07.002. doi: 10.1016/j.neuron.2010.07.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Nagy Z, Esiri MM, Jobst KA, et al. The effects of additional pathology on the cognitive deficit in Alzheimer disease. J Neuropathol Exp Neurol. 1997;56:165–170. doi: 10.1097/00005072-199702000-00007. [DOI] [PubMed] [Google Scholar]
- 76.Niwa K, Kazama K, Younkin L, et al. Cerebrovascular autoregulation is profoundly impaired in mice overexpressing amyloid precursor protein. Am J Physiol Heart Circ Physiol. 2002;283:H315–H323. doi: 10.1152/ajpheart.00022.2002. [DOI] [PubMed] [Google Scholar]
- 77.Niwa K, Younkin L, Ebeling C, et al. Abeta 1–40-related reduction in functional hyperemia in mouse neocortex during somatosensory activation. Proc Natl Acad Sci USA. 2000;97:9735–9740. doi: 10.1073/pnas.97.17.9735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Ohab J, Fleming S, Blesch A, Carmichael S. A neurovascular niche for neurogenesis after stroke. J Neurosci. 2006;26:13007–13016. doi: 10.1523/JNEUROSCI.4323-06.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Pang Y, Campbell L, Zheng B, et al. Lipopolysaccharide-activated microglia induce death of oligodendrocyte progenitor cells and impede their development. Neuroscience. 2010;166:464–475. doi: 10.1016/j.neuroscience.2009.12.040. [DOI] [PubMed] [Google Scholar]
- 80.Park L, Anrather J, Girouard H, Zhou P, Iadecola C. Nox2-derived reactive oxygen species mediate neurovascular dysregulation in the aging mouse brain. J Cereb Blood Flow Metab. 2007;27:1908–1918. doi: 10.1038/sj.jcbfm.9600491. [DOI] [PubMed] [Google Scholar]
- 81.Park L, Zhou P, Pitstick R, et al. Nox2-derived radicals contribute to neurovascular and behavioral dysfunction in mice overexpressing the amyloid precursor protein. Proc Natl Acad Sci USA. 2008;105:1347–1352. doi: 10.1073/pnas.0711568105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Patel NS, Mathura VS, Bachmeier C, et al. Alzheimer’s beta-amyloid peptide blocks vascular endothelial growth factor mediated signaling via direct interaction with VEGFR-2. J Neurochem. 2010;112:66–76. doi: 10.1111/j.1471-4159.2009.06426.x. [DOI] [PubMed] [Google Scholar]
- 83.Paulson OB, Hasselbalch SG, Rostrup E, Knudsen GM, Pelligrino D. Cerebral blood flow response to functional activation. J Cereb Blood Flow Metab. 2010;30:2–14. doi: 10.1038/jcbfm.2009.188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Prohovnik I, Mayeux R, Sackeim HA, et al. Cerebral perfusion as a diagnostic marker of early Alzheimer’s disease. Neurology. 1988;38:931–937. doi: 10.1212/wnl.38.6.931. [DOI] [PubMed] [Google Scholar]
- 85.Querfurth HW, LaFerla FM. Alzheimer’s disease. N Engl J Med. 2010;362:329–344. doi: 10.1056/NEJMra0909142. [DOI] [PubMed] [Google Scholar]
- 86.Roman GC, Takemici TK, Erkinjuntti T, et al. Vascular dementia: diagnostic criteria for research studies: report of the NINDS-AIREN international workshop. Neurology. 1993;43:250–260. doi: 10.1212/wnl.43.2.250. [DOI] [PubMed] [Google Scholar]
- 87.Ruitenberg A, den Heijer T, Bakker SL, et al. Cerebral hypoperfusion and clinical onset of dementia: the Rotterdam Study. Ann Neurol. 2005;57:789–794. doi: 10.1002/ana.20493. [DOI] [PubMed] [Google Scholar]
- 88.Savva GM, Wharton SB, Ince PG, et al. Age, neuropathology, and dementia. N Engl J Med. 2009;360:2302–2309. doi: 10.1056/NEJMoa0806142. [DOI] [PubMed] [Google Scholar]
- 89.Schneider JA, Arvanitakis Z, Leurgans SE, Bennett DA. The neuropathology of probable Alzheimer disease and mild cognitive impairment. Ann Neurol. 2009;66:200–208. doi: 10.1002/ana.21706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Schneider JA, Wilson RS, Bienias JL, Evans DA, Bennett DA. Cerebral infarctions and the likelihood of dementia from Alzheimer disease pathology. Neurology. 2004;62:1148–1155. doi: 10.1212/01.wnl.0000118211.78503.f5. [DOI] [PubMed] [Google Scholar]
- 91.Schroeter ML, Cutini S, Wahl MM, Scheid R, Yves von Cramon D. Neurovascular coupling is impaired in cerebral microangiopathy—an event-related Stroop study. Neuroimage. 2007;34:26–34. doi: 10.1016/j.neuroimage.2006.09.001. [DOI] [PubMed] [Google Scholar]
- 92.Selnes OA, Vinters HV. Vascular cognitive impairment. Nat Clin Pract Neurol. 2006;2:538–547. doi: 10.1038/ncpneuro0294. [DOI] [PubMed] [Google Scholar]
- 93.Shibata M, Yamada S, Kumar SR, et al. Clearance of Alzheimer’s amyloid-beta (1–40) peptide from brain by LDL receptor-related protein-1 at the blood-brain barrier. J Clin Invest. 2000;106:1489–1499. doi: 10.1172/JCI10498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Siegel GJ, Chauhan NB. Neurotrophic factors in Alzheimer’s and Parkinson’s disease brain. Brain Res Brain Res Rev. 2000;33:199–227. doi: 10.1016/s0165-0173(00)00030-8. [DOI] [PubMed] [Google Scholar]
- 95.Silvestrini M, Pasqualetti P, Baruffaldi R, et al. Cerebrovascular reactivity and cognitive decline in patients with Alzheimer disease. Stroke. 2006;37:1010–1015. doi: 10.1161/01.STR.0000206439.62025.97. [DOI] [PubMed] [Google Scholar]
- 96.Sim FJ, Zhao C, Penderis J, Franklin RJ. The age-related decrease in CNS remyelination efficiency is attributable to an impairment of both oligodendrocyte progenitor recruitment and differentiation. J Neurosci. 2002;22:2451–2459. doi: 10.1523/JNEUROSCI.22-07-02451.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Simpson JE, Fernando MS, Clark L, et al. White matter lesions in an unselected cohort of the elderly: astrocytic, microglial and oligodendrocyte precursor cell responses. Neuropathol Appl Neurobiol. 2007;33:410–419. doi: 10.1111/j.1365-2990.2007.00828.x. [DOI] [PubMed] [Google Scholar]
- 98.Simpson JE, Ince PG, Haynes LJ, et al. Population variation in oxidative stress and astrocyte DNA damage in relation to Alzheimer-type pathology in the ageing brain. Neuropathol Appl Neurobiol. 2010;36:25–40. doi: 10.1111/j.1365-2990.2009.01030.x. [DOI] [PubMed] [Google Scholar]
- 99.Simpson JE, Ince PG, Higham CE, et al. Microglial activation in white matter lesions and nonlesional white matter of ageing brains. Neuropathol Appl Neurobiol. 2007;33:670–683. doi: 10.1111/j.1365-2990.2007.00890.x. [DOI] [PubMed] [Google Scholar]
- 100.Smith PJ, Blumenthal JA, Babyak MA, et al. Effects of the dietary approaches to stop hypertension diet, exercise, and caloric restriction on neurocognition in overweight adults with high blood pressure. Hypertension. 2010;55:1331–1338. doi: 10.1161/HYPERTENSIONAHA.109.146795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Snapyan M, Lemasson M, Brill MS, et al. Vasculature guides migrating neuronal precursors in the adult mammalian forebrain via brain-derived neurotrophic factor signaling. J Neurosci. 2009;29:4172–4188. doi: 10.1523/JNEUROSCI.4956-08.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Snowdon DA, Greiner LH, Mortimer JA, et al. Brain infarction and the clinical expression of Alzheimer disease. The Nun Study. JAMA. 1997;277:813–817. [PubMed] [Google Scholar]
- 103.Song IU, Kim JS, Kim YI, Eah KY, Lee KS. Clinical significance of silent cerebral infarctions in patients with Alzheimer disease. Cogn Behav Neurol. 2007;20:93–98. doi: 10.1097/WNN.0b013e31805d859e. [DOI] [PubMed] [Google Scholar]
- 104.Sonnen JA, Larson EB, Brickell K, et al. Different patterns of cerebral injury in dementia with or without diabetes. Arch Neurol. 2009;66:315–322. doi: 10.1001/archneurol.2008.579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Sparks DL, Scheff SW, Liu H, et al. Increased incidence of neurofibrillary tangles (NFT) in non-demented individuals with hypertension. J Neurol Sci. 1995;131:162–169. doi: 10.1016/0022-510x(95)00105-b. [DOI] [PubMed] [Google Scholar]
- 106.Staekenborg SS, Koedam ELGE, Henneman WJP, et al. Progression of mild cognitive impairment to dementia: contribution of cerebrovascular disease compared with medial temporal lobe atrophy. Stroke. 2009;40:1269–1274. doi: 10.1161/STROKEAHA.108.531343. [DOI] [PubMed] [Google Scholar]
- 107.Sun X, He G, Qing H, et al. Hypoxia facilitates Alzheimer’s disease pathogenesis by up-regulating BACE1 gene expression. Proc Natl Acad Sci USA. 2006;103:18727–18732. doi: 10.1073/pnas.0606298103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Tanaka M, Fukuyama H, Yamauchi H, et al. Regional cerebral blood flow abnormalities in nondemented patients with memory impairment. J Neuroimaging. 2002;12:112–118. doi: 10.1111/j.1552-6569.2002.tb00106.x. [DOI] [PubMed] [Google Scholar]
- 109.Tarkowski E, Issa R, Sjögren M, et al. Increased intrathecal levels of the angiogenic factors VEGF and TGF-beta in Alzheimer’s disease and vascular dementia. Neurobiol Aging. 2002;23:237–243. doi: 10.1016/s0197-4580(01)00285-8. [DOI] [PubMed] [Google Scholar]
- 110.Tesco G, Koh YH, Kang EL, et al. Depletion of GGA3 stabilizes BACE and enhances beta-secretase activity. Neuron. 2007;54:721–737. doi: 10.1016/j.neuron.2007.05.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Thomas T, Thomas G, McLendon C, Sutton T, Mullan M. β-Amyloid-mediated vasoactivity and vascular endothelial damage. Nature. 1996;380:168–171. doi: 10.1038/380168a0. [DOI] [PubMed] [Google Scholar]
- 112.Tong L, Balazs R, Soiampornkul R, Thangnipon W, Cotman CW. Interleukin-1 beta impairs brain derived neurotrophic factor-induced signal transduction. Neurobiol Aging. 2008;29:1380–1393. doi: 10.1016/j.neurobiolaging.2007.02.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Trapp BD, Stys PK. Virtual hypoxia and chronic necrosis of demyelinated axons in multiple sclerosis. Lancet Neurol. 2009;8:280–291. doi: 10.1016/S1474-4422(09)70043-2. [DOI] [PubMed] [Google Scholar]
- 114.van Beek AH, Claassen JA, Rikkert MG, Jansen RW. Cerebral autoregulation: an overview of current concepts and methodology with special focus on the elderly. J Cereb Blood Flow Metab. 2008;28:1071–1085. doi: 10.1038/jcbfm.2008.13. [DOI] [PubMed] [Google Scholar]
- 115.Venters HD, Dantzer R, Kelley KW. A new concept in neurodegeneration: TNFalpha is a silencer of survival signals. Trends Neurosci. 2000;23:175–180. doi: 10.1016/s0166-2236(99)01533-7. [DOI] [PubMed] [Google Scholar]
- 116.Vermeer SE, Prins ND, den Heijer T, et al. Silent brain infarcts and the risk of dementia and cognitive decline. N Engl J Med. 2003;348:1215–1222. doi: 10.1056/NEJMoa022066. [DOI] [PubMed] [Google Scholar]
- 117.Warkentin S, Passant U. Functional imaging of the frontal lobes in organic dementia. Regional cerebral blood flow findings in normals, in patients with frontotemporal dementia and in patients with Alzheimer’s disease, performing a word fluency test. Dement Geriatr Cogn Disord. 1997;8:105–109. doi: 10.1159/000106614. [DOI] [PubMed] [Google Scholar]
- 118.Weber C, Fraemohs L, Dejana E. The role of junctional adhesion molecules in vascular inflammation. Nat Rev Immunol. 2007;7:467–477. doi: 10.1038/nri2096. [DOI] [PubMed] [Google Scholar]
- 119.Weinstein BM. Vessels and nerves: marching to the same tune. Cell. 2005;120:299–302. doi: 10.1016/j.cell.2005.01.010. [DOI] [PubMed] [Google Scholar]
- 120.Weller RO, Boche D, Nicoll JA. Microvasculature changes and cerebral amyloid angiopathy in Alzheimer’s disease and their potential impact on therapy. Acta Neuropathol. 2009;118:87–102. doi: 10.1007/s00401-009-0498-z. [DOI] [PubMed] [Google Scholar]
- 121.Wen Y, Onyewuchi O, Yang S, Liu R, Simpkins JW. Increased beta-secretase activity and expression in rats following transient cerebral ischemia. Brain Res. 2004;1009:1–8. doi: 10.1016/j.brainres.2003.09.086. [DOI] [PubMed] [Google Scholar]
- 122.Wen Y, Yang S-H, Liu R, et al. Cdk5 is involved in NFT-like tauopathy induced by transient cerebral ischemia in female rats. Biochim Biophys Acta. 2007;1772:473–483. doi: 10.1016/j.bbadis.2006.10.011. [DOI] [PubMed] [Google Scholar]
- 123.White L. Brain lesions at autopsy in older Japanese-American men as related to cognitive impairment and dementia in the final years of life: a summary report from the Honolulu-Asia aging study. J Alzheimers Dis. 2009;18:713–725. doi: 10.3233/JAD-2009-1178. [DOI] [PubMed] [Google Scholar]
- 124.Wolburg H, Noell S, Mack A, Wolburg-Buchholz K, Fallier-Becker P. Brain endothelial cells and the glio-vascular complex. Cell Tissue Res. 2009;335:75–96. doi: 10.1007/s00441-008-0658-9. [DOI] [PubMed] [Google Scholar]
- 125.Wu Z, Guo H, Chow N, et al. Role of the MEOX2 homeobox gene in neurovascular dysfunction in Alzheimer disease. Nat Med. 2005;11:959–965. doi: 10.1038/nm1287. [DOI] [PubMed] [Google Scholar]
- 126.Yang S-P, Bae D-G, Kang HJ, et al. Co-accumulation of vascular endothelial growth factor with beta-amyloid in the brain of patients with Alzheimer’s disease. Neurobiol Aging. 2004;25:283–290. doi: 10.1016/S0197-4580(03)00111-8. [DOI] [PubMed] [Google Scholar]
- 127.Yoshiura T, Hiwatashi A, Yamashita K, et al. Simultaneous measurement of arterial transit time, arterial blood volume, and cerebral blood flow using arterial spin-labeling in patients with Alzheimer disease. Am J Neuroradiol. 2009;30:1388–1393. doi: 10.3174/ajnr.A1562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Zacchigna S, Lambrechts D, Carmeliet P. Neurovascular signalling defects in neurodegeneration. Nat Rev Neurosci. 2008;9:169–181. doi: 10.1038/nrn2336. [DOI] [PubMed] [Google Scholar]
- 129.Zekry D, Duyckaerts C, Moulias R, et al. Degenerative and vascular lesions of the brain have synergistic effects in dementia of the elderly. Acta Neuropathol. 2002;103:481–487. doi: 10.1007/s00401-001-0493-5. [DOI] [PubMed] [Google Scholar]
- 130.Zhang F, Eckman C, Younkin S, Hsiao KK, Iadecola C. Increased susceptibility to ischemic brain damage in transgenic mice overexpressing the amyloid precursor protein. J Neurosci. 1997;17:7655–7661. doi: 10.1523/JNEUROSCI.17-20-07655.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Zhiyou C, Yong Y, Shanquan S, et al. Upregulation of BACE1 and beta-amyloid protein mediated by chronic cerebral hypoperfusion contributes to cognitive impairment and pathogenesis of Alzheimer’s disease. Neurochem Res. 2009;34:1226–1235. doi: 10.1007/s11064-008-9899-y. [DOI] [PubMed] [Google Scholar]
- 132.Zlokovic BV. The blood-brain barrier in health and chronic neurodegenerative disorders. Neuron. 2008;57:178–201. doi: 10.1016/j.neuron.2008.01.003. [DOI] [PubMed] [Google Scholar]