Abstract
Purpose
Tobacco use using a waterpipe is an emerging trend among college students. Although cigarette smoking is low among college athletes, waterpipe tobacco smoking may appeal to this population. The purpose of this study was to compare cigarette and waterpipe tobacco smoking in terms of their associations with organized sport participation.
Methods
In the spring of 2008, we conducted an online survey of 8,745 college students at eight institutions as part of the revised National College Health Assessment. We used multivariable regression models to assess the associations between tobacco use (cigarette and waterpipe) and organized sports participation.
Results
Participants reported participation in varsity (5.2%), club (11.9%), and intramural (24.9%) athletics. Varsity athletes and individuals who were not varsity athletes had similar rates of waterpipe tobacco smoking (27.6% vs. 29.5%, p = .41). However, other types of athletes were more likely than their counterparts to have smoked waterpipe tobacco (35.1% vs. 28.7%, p < .001 for club sports and 34.8% vs. 27.7%, p < .001 for intramural sports). In fully-adjusted multivariable models, sports participants of any type had lower odds of having smoked cigarettes, whereas participants who played intramural sports (odds ratio = 1.15, 95% confidence interval = 1.03, 1.29) or club sports (odds ratio = 1.15, 95% confidence interval = 1.001, 1.33) had significantly higher odds of having smoked waterpipe tobacco.
Conclusions
College athletes are susceptible to waterpipe tobacco use. In fact, compared with their nonathletic counterparts, club sports participants and intramural sports participants generally had higher odds of waterpipe tobacco smoking. Allure for waterpipe tobacco smoking may exist even for individuals who are traditionally considered at low risk for tobacco use.
Keywords: Athletes, Waterpipe, Hookah, Tobacco, Team sports, Club sports, Intramural sports, Varsity sports, Organized sports, College
Although tobacco use remains the leading cause of death and disease in the United States [1], cigarette use has declined substantially over the past 2 decades, with proportional decreases in the college population [2–4]. However, tobacco smoking using a waterpipe (a.k.a., hookah, narghile, arghile, or shisha-pipe) seems to be an emerging trend [5–9], especially among college students, who have an estimated lifetime prevalence of 20–40% [5–8].
Despite the increased prevalence of waterpipe tobacco smoking, available research indicates that waterpipe tobacco smoke contains large amounts of toxicants; for example, a single waterpipe session produces about 46 times the tar of a single cigarette [10–13]. Furthermore, a single waterpipe use episode can increase smokers’ expired air carbon monoxide level five times as much as a single cigarette [14], and the blood nicotine levels of daily waterpipe users are similar to those of an individual who smokes 10 cigarettes per day [15]. These data are consistent with preliminary reports linking waterpipe tobacco smoking to cancer, cardiovascular disease, decreased pulmonary function, and nicotine dependence [16–19].
Compared with nonathletes, college athletes of various types are less prone to cigarette smoking; studies estimate that smoking is as much as 50% lower among athletes compared with nonathletes [20–24]. It has been further suggested that there may be an association between the intensity of athletic involvement and risk behavior. For example, one large study of students at 140 U.S. colleges showed that only 15% of male students who participated in athletics daily were current smokers, compared with 20% of those who were only somewhat involved and 26% of those who were not involved [21,24]. Thus, it seems that different types of athletic engagement (e.g., varsity, club, and intramural sports) carry various degrees of risk for cigarette smoking.
However, despite trends toward lower cigarette use among college athletes, waterpipe tobacco smoking seems to be garnering increasing appeal among mainstream college populations and attracting a constituency among youth who do not use other forms of tobacco. In fact, as many as 35–65% of waterpipe tobacco users do not use cigarettes [5–8]. This may be because of its esthetic appeal—including the sweet smell and taste of the flavored tobacco and the exotic nature of the ritual—and because of the belief that water somehow “filters” smoke, rendering it less harmful than cigarette smoking [5,7,8].
However, it is not currently known whether waterpipe tobacco smoking is common among U.S. college athletes, and whether its popularity is different among participants of different types of organized sports (e.g., varsity, club, and intramural sports). Determining which populations are at greatest risk may help us to develop effective, targeted interventions and policies to reduce the potential harm of waterpipe tobacco use among college students.
The purpose of this study was to compare cigarette and waterpipe tobacco smoking in terms of their associations with organized sport participation. We hypothesized that waterpipe tobacco smoking would be common among all athletes but especially club and intramural athletes. We further hypothesized that, whereas cigarette smoking would be inversely associated with sports participation, waterpipe tobacco smoking would have no significant association—positive or negative—with sports participation.
Methods
Design, setting, and procedures
The American College Health Association (ACHA) conducts an annual assessment of college students’ health called the National College Health Assessment (NCHA). The NCHA is a bi-annual, national data collection effort including more than 90,000 college students. The original data collection instrument has been under revision since 2006. An item measuring lifetime and 30-day waterpipe tobacco smoking, as well as frequency of use in the last 30 days, is included in the revised survey, which is called the NCHA II.
The first pilot test of the NCHA II was conducted in Spring 2008. A total of 113 institutions self-selected to participate in the original NCHA in Spring 2008. Eight of the larger institutions surveyed in February 2008 were recruited by ACHA to pilot test the NCHA II. Although specific school identities are not revealed to outside researchers, we are allowed to know and to report a summary of the demographic characteristics of the institutions. As a whole, the eight universities represented the South, Northeast, and Western regions of the United States, and they were roughly divided among the 5,000–9,999, 10,000–19,999, and 20,000+ size brackets. Two of the eight institutions were private and six were public; all of the schools were 4-year institutions, and none had religious affiliations.
At each of the eight campuses, the original NCHA sample was doubled so that both the original and revised versions of the survey could be administered. Each campus submitted a list of randomly selected students for surveying. The ACHA used each campus list to assign students randomly to receive the two versions of the survey. All students were contacted by e-mail and asked to complete the confidential survey online. Nonresponders were contacted twice with reminder messages. Each institution was required to obtain institutional review board approval before data collection.
Measures
Sociodemographic data
We used student report of age, gender, race, and ethnicity as covariates.
Waterpipe and cigarette tobacco smoking
The waterpipe tobacco smoking item added to the NCHA II, which follows the pattern of all other substance use items on the survey instrument, asks: “Within the past 30 days, on how many days did you use tobacco from a water pipe (hookah)? The answer choices are: (a) never used; (b) have used, but not in the past 30 days; (c) 1–2 days; (d) 3–5 days; (e) 6–9 days; (f) 10–19 days; (g) 20–29 days; and (h) all 30 days.” We used these data to measure (1) waterpipe tobacco smoking in the past 30 days (choices c, d, e, f, g, or h), and (2) ever waterpipe tobacco smoking (choices b, c, d, e, f, g, or h). A similarly worded item assessed cigarette smoking (1) over the past 30 days, and (2) ever.
Organized sports
The NHCA II asked all students to self-report whether they had actively participated in (1) intramural sports, (2) club sports, and/or (3) varsity sports, each within the past 12 months. The instrument did not use more specific language to define each of these types of sports.
Statistical analysis
We first computed the prevalence of waterpipe and cigarette smoking in each of our various subgroups (all participants, varsity athletes, club sports athletes, and intramural athletes). We used chi-square tests for categorical data to compare tobacco smoking rates in athletes vs. their nonathletic counterparts (i.e., varsity athletes vs. those who were not varsity athletes; club sports athletes vs. those who were not club sports athletes, etc.). We then used multiple logistic regression to model the relationship between sports participation and each type of tobacco smoking while adjusting for covariates. We used three multivariate models to represent each type of organized sport: varsity, club, and intramural. For each model we used athlete status (yes vs. no) as the independent variable and tobacco use (yes vs. no) as the dependent variable. We included all covariates (age, gender, race, and ethnicity) in all of our models. We used a two-tailed alpha = .05 to define statistical significance.
Results
Of the students eligible to complete the survey at the eight institutions, 8,801 (28% of all eligible) responded. Of those, 8,745 (99%) responded to the outcome of interest for this study (waterpipe tobacco smoking). Thus, the final sample size for our study was 8,745 individuals, of whom 2,910 (33.3%) reported participating in any organized sports in the past 12 months of the survey, 447 (5.2%) reported playing varsity sports, 1,023 (11.9%) reported playing club sports, and 2,142 (24.9%) reported playing intramural sports.
Overall, 2,576 (29.5%) reported ever trying waterpipe tobacco smoking and 631 (7.2%) reported waterpipe tobacco smoking in the past 30 days (Table 1). Of those individuals who had used waterpipe tobacco in the past 30 days, the majority (69.7%) had only done so one to two times in the past 30 days. By comparison, slightly more than one-sixth (17.3%) had used waterpipe tobacco three to five times in the past 30 days, 7.1% had done so 6–9 days, 1.2% 10–19 days, 1.4% 20–29 days, and .8% every day.
Table 1.
Demographic characteristics of sample by waterpipe tobacco smoking
| Characteristic | Whole sample* | Ever smoked tobacco from a waterpipe |
p† | Smoked tobacco from a waterpipe in the past 30 days |
p† |
|---|---|---|---|---|---|
| N = 8,745 | N = 2,576 | N = 631 | |||
| N (Column %) | Row % | Row % | |||
| Age (y) | |||||
| 18–19 | 2,752 (31.7) | 31.8 | <.001 | 10.3 | <.001 |
| 20–21 | 2,806 (32.3) | 34.2 | 8.5 | ||
| 22+ | 3,119 (36.0) | 23.1 | 3.3 | ||
| Gender | |||||
| Male | 3,240 (37.3) | 34.2 | <.001 | 9.7 | <.001 |
| Female | 5,452 (62.7) | 26.6 | 5.7 | ||
| Race | |||||
| White | 6,023 (68.4) | 31.4 | <.001 | 7.5 | <.001 |
| Black | 628 (7.1) | 13.3 | 1.8 | ||
| Asian | 967 (11.0) | 23.2 | 5.8 | ||
| Other or mixed | 1,183 (13.4) | 33.2 | 9.7 | ||
| Ethnicity | |||||
| Hispanic | 524 (6.0) | 31.1 | .39 | 8.2 | .37 |
| Not Hispanic | 8,221 (94.0) | 29.4 | 7.2 | ||
| Varsity sports (last 12 months) | |||||
| Yes | 447 (5.2) | 27.6 | .41 | 6.1 | .36 |
| No | 8,102 (94.8) | 29.5 | 7.2 | ||
| Club sports (last 12 months) | |||||
| Yes | 1,023 (11.9) | 35.1 | <.001 | 10.0 | <.001 |
| No | 7,547 (88.1) | 28.7 | 6.8 | ||
| Intramural sports (last 12 months) | |||||
| Yes | 2,142 (24.9) | 34.8 | <.001 | 9.4 | <.001 |
| No | 6,457 (75.1) | 27.7 | 6.5 |
Data do not always sum to total sample sizes because of missing data. Percentages are based on the total for each category and may not total 100 due to rounding.
Chi-square analyses comparing athletes vs. non-athletes (e.g., varsity sports participants vs. those who did not participate in varsity athletics).
Ever waterpipe tobacco smokers were significantly more likely to be younger, male, and not black (Table 1). Compared with nonparticipants, club sport participants and intramural participants were more commonly ever waterpipe tobacco smokers (p < .001 for both). However, compared with nonparticipants, varsity sports participants had no increased odds of having smoked tobacco from a waterpipe (Table 1).
Of the full sample, 2,979 (34.1%) reported ever trying cigarette smoking, and 1,433 (16.4%) reported cigarette smoking in the past 30 days. Ever cigarette smokers were significantly more likely to be older, male, and Caucasian (Table 2). Compared with nonparticipants, participants in varsity, club sports, and intramurals were all less commonly ever cigarette smokers (p < .001, p = .006, and p = .02 respectively, Table 2). Outcomes related to 30-day use exhibited similar overall patterns (Tables 1 and 2).
Table 2.
Demographic characteristics of sample by cigarette smoking
| Characteristic | Whole sample* | Ever smoked cigarettes | p† | Smoked cigarettes in last 30 days |
p† |
|---|---|---|---|---|---|
| N = 8,728‡ | N = 2,979 | N = 1,433 | |||
| N (Column %) | Row % | Row % | |||
| Age (y) | |||||
| 18–19 | 2,749 (31.7) | 29.4 | <.001 | 16.3 | .02 |
| 20–21 | 2,880 (32.3) | 36.1 | 17.9 | ||
| 22+ | 3,111 (35.9) | 36.6 | 15.1 | ||
| Gender | |||||
| Male | 3,227 (37.4) | 36.4 | .001 | 18.8 | <.001 |
| Female | 5,413 (62.7) | 32.8 | 14.9 | ||
| Race | |||||
| White | 5,986 (68.6) | 38.5 | <.001 | 18.8 | <.001 |
| Black | 624 (7.2) | 15.7 | 6.3 | ||
| Asian | 959 (11.0) | 21.5 | 9.5 | ||
| Other or mixed | 1,159 (13.3) | 31.8 | 15.4 | ||
| Ethnicity | |||||
| Hispanic | 524 (6.0) | 31.3 | .16 | 15.3 | .46 |
| Not Hispanic | 8,204 (94.0) | 34.3 | 16.5 | ||
| Varsity sports (last 12 months) | |||||
| Yes | 445 (5.2) | 27.0 | .001 | 9.7 | <.001 |
| No | 8,054 (94.8) | 34.6 | 16.9 | ||
| Club sports (last 12 months) | |||||
| Yes | 1,016 (11.9) | 30.4 | .006 | 14.8 | .11 |
| No | 7,502 (88.1) | 34.8 | 16.7 | ||
| Intramural sports (last 12 months) | |||||
| Yes | 2,129 (24.9) | 32.1 | .02 | 15.5 | .16 |
| No | 6,420 (75.1) | 34.9 | 16.8 |
Data do not always sum to total sample sizes because of missing data. Percentages are based on the total for each category and may not total 100 due to rounding.
Chi-square analyses comparing athletes vs. non-athletes (e.g., varsity sports participants vs. those who did not participate in varsity athletics).
Total N for this table is slightly smaller compared with the previous table (8728 vs. 8745) since 17 participants did not respond to cigarette smoking items.
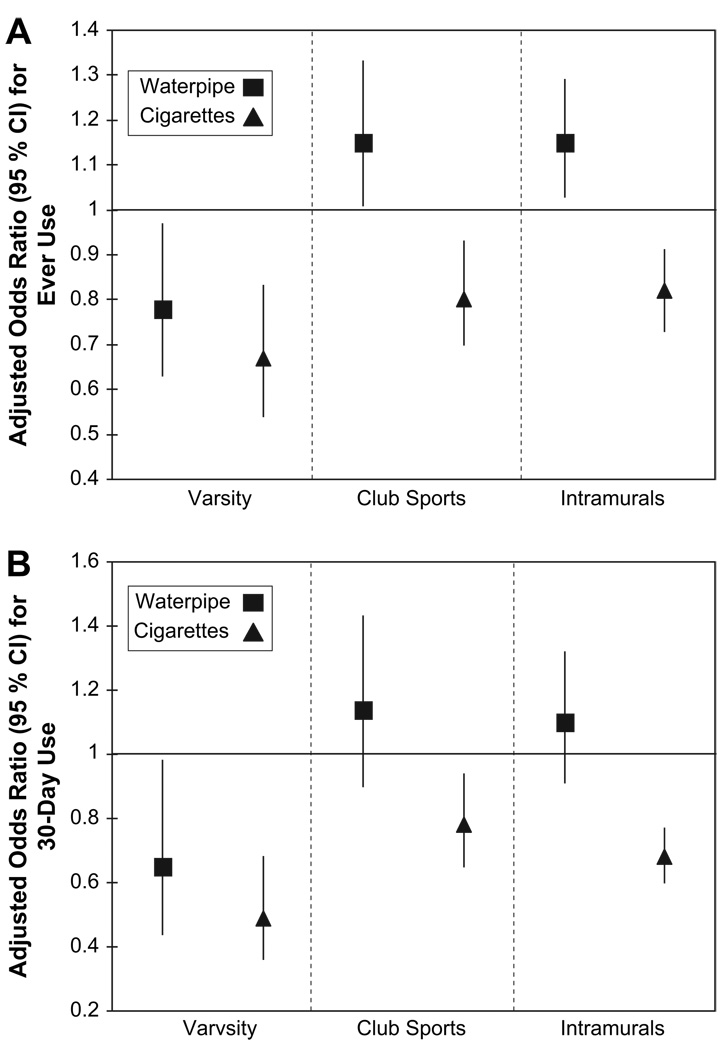
In the fully adjusted multivariable models, varsity, club, and intramural sports participants all had lower odds of having smoked cigarettes compared with their nonathletic counterparts (Figure 1A). In contrast, intramural sport (odds ratio [OR] = 1.15, 95% confidence interval [95% CI] = 1.03, 1.29) and club sport (OR = 1.15, 95% CI = 1.001, 1.33) participants had significantly higher odds of having smoked waterpipe tobacco, compared with their counterparts (Figure 1A). Varsity sports players, however, had significantly lower odds for ever waterpipe tobacco smoking (OR = .78, 95% CI = .63, .97, Figure 1A).
Figure 1.
(A) Ever tobacco use among college athletes (waterpipe vs. cigarette). (B) Current (30-day) tobacco use among college athletes (waterpipe vs. cigarette). All analyses were adjusted for age, gender, race, and ethnicity. The reference group for each analysis was nonparticipants (e.g., varsity athletes vs all who are not varsity athletes; club sports participants vs. non–club sports participants). Data represent the results of six separate analyses based on data in Table 3.
Overall patterns were the same for multivariable models using current use (30-day) outcomes (Figure 1B). However, in these models club sport and intramural participation were associated with nonsignificant trends toward higher odds of waterpipe tobacco smoking (OR = 1.14, 95% CI = .90, 1.43, and OR= 1.10, 95% CI = .91, 1.32, respectively). All results for unadjusted and adjusted models are available in Table 3.
Table 3.
Odds ratios (95% confidence intervals) for different types tobacco use, by sports participation
| Sports type | Waterpipe | Cigarettes | |||
|---|---|---|---|---|---|
| Ever | Past 30 days | Ever | Past 30 days | ||
| Varsity sports | Unadjusted | .92 (.74, 1.13) | .83 (.56, 1.24) | .71 (.57, .88)† | .55 (.40, .75)‡ |
| Adjusted* | .78 (.63, .97)† | .65 (.44, .98)† | .67 (.54, .83)‡ | .49 (.36, .68)‡ | |
| Club sports | Unadjusted | 1.35 (1.17, 1.55)‡ | 1.52 (1.21, 1.90)‡ | .82 (.71, .94)† | .86 (.72, 1.03) |
| Adjusted* | 1.15 (1.001, 1.33)† | 1.14 (.90, 1.43) | .80 (.70, .93)† | .78 (.65, .94)† | |
| Intramural sports | Unadjusted | 1.39 (1.25, 1.54)‡ | 1.48 (1.24, 1.77)‡ | .88 (.80, .98)† | .91 (.80, 1.04) |
| Adjusted* | 1.15 (1.03, 1.29)† | 1.10 (.91, 1.32) | .82 (.73, .91)‡ | .78 (.68, .90)† | |
Adjusted for age, gender, race, and ethnicity.
p < .05.
p < .001.
Discussion
In this national sample of 8,745 college students, we found that participation in organized sports was associated with highly variable odds of tobacco use, depending on the type of sport and type of tobacco use. Although all organized sports participants were significantly less likely to smoke cigarettes, only varsity sports participants had lower odds of waterpipe tobacco smoking. In some analyses, club sports participants and intramural sports participants had higher odds of waterpipe tobacco smoking.
These rates we found for waterpipe tobacco smoking, among athletes and nonathletes alike, are of concern, as we do not yet fully understand the public health risks of waterpipe tobacco smoking. Although further research is necessary, available evidence suggests that the practice is associated with substantial risk for both harm and nicotine dependence [16–19]. This study suggests that many college athletes who would have otherwise been nicotine naive may be vulnerable to developing lifelong nicotine dependence via waterpipe tobacco smoking.
Waterpipe tobacco smoking varied among different types of college athletes. Varsity athlete status was associated with lower odds of any type of tobacco use (cigarette or waterpipe). Compared with other athletes, because of intensive training schedules, varsity athletes simply may have less time to engage in risk-taking behaviors such as waterpipe tobacco smoking. They may also be less willing to experiment with a new behavior, such as waterpipe tobacco smoking, that may carry respiratory or cardiovascular risks because of the demands of their sports and the seriousness of their athletic commitment. In addition, in 1994 the NCAA passed a ban on the use of all tobacco products during practice and competition for both students and personnel, and many individual universities may have similar regulations as well.
We were surprised to discover that club and intramural athletes were at higher risk of waterpipe tobacco smoking, especially since involvement in sports is protective against cigarette use. It seems paradoxical that these athletes would reject the harmful chemicals in cigarettes while embracing them (perhaps unwittingly) in waterpipe form. One reason for this discrepancy may be misinformation. Qualitative investigations may help us understand what educational gaps may exist that lead certain athletes to be willing to smoke tobacco from a waterpipe but not from a cigarette.
Another possible explanation is that, as involved campus leaders, club and intramural sports participants are likely to be involved in “trendy” activities such as waterpipe tobacco smoking. Cigarette smoking, however, is now generally frowned upon in fashionable circles because of increasing understanding of tobacco industry manipulation and vilification of cigarettes in the popular press. Others have had similar findings for fashionable risk-taking behaviors such as alcohol use [25,26]. It may be that, whereas public health professionals perceive waterpipe use as most similar to cigarette use, college athletes perceive it as more similar to alcohol use.
Our findings suggest that emphasizing the similarities between waterpipe and cigarette smoking (i.e., “tobacco is tobacco”) may be a valuable health education strategy, particularly for athletes, because these college students seem to perceive waterpipe tobacco smoking as somehow different. Such education may emphasize that (1) the chemicals in the two smoking methods are the same, (2) the water does not provide a valuable “filter,” and (3) there is risk of both harm and dependence from waterpipe tobacco smoking. Although our results suggest that there would be limited value in conducting cigarette smoking education among athletes, similar programs related specifically to waterpipe tobacco smoking may be valuable. Brief interventions with personalized feedback tailored to college athletes, related to both in- and off-season substance use, are examples of interventions that have been valuable for cigarettes and alcohol [26,27].
We found somewhat different results for each of the two waterpipe outcomes. Whereas club and intramural athlete participation was associated with higher odds of ever waterpipe tobacco smoking, it was associated with a nonsignificant trend of higher odds for current waterpipe tobacco smoking (within the past 30 days). This may simply be because there were many fewer current waterpipe smokers versus ever waterpipe smokers (7.2% vs. 29.5%), substantially lowering the statistical power for analyses involving current smoking. However, it may also be that club and intramural athletes are inclined to try waterpipe smoking once or twice, to be part of the “crowd,” but that they do not tend to do so frequently. They may not be able to do so frequently, for example, since their time is occupied with extracurricular activities. Again, qualitative investigations may help explore these issues.
The present study was limited in that the sample, although it was national, was not nationally representative. Because schools self-selected to participate, findings may not be broadly generalizable. For example, cigarette smoking in this sample was relatively low (16.4%). This could be because the ACHA sample has a high proportion of female participants, who are generally less likely to be tobacco users. Although the overall response rate was about one in three, this is actually considered excellent for e-mail surveys, which typically generate response rates of 10–30% [28–30]. However, this is also a potential source of selection bias. In addition, this analysis was limited in that it relied on self-report of athletic status and did not differentiate between types of sports played or intensity of athletic activity. It may be valuable for future investigators to use more specific assessment of these independent variables. Finally, statistical analyses may have been affected by disparate proportions of student athletes from the various groups.
In summary, we found that although overall sport participation among U.S. college students confers protection against cigarette smoking, only varsity sports players have lower odds of waterpipe tobacco smoking, while club and intramural sports players are at increased risk of waterpipe tobacco smoking. Knowing that the allure of waterpipe tobacco smoking may exist for athletically minded individuals, it may be valuable for prevention programs to emphasize the public health message that “tobacco is tobacco.” These findings should help guide future research as well as the development of educational interventions that may be able to substantially reduce tobacco use—the leading cause of death and disease in the U.S.—among college students.
Acknowledgments
Dr. Primack is supported in part by a Physician Faculty Scholar Award from the Robert Wood Johnson Foundation, a career development award from the National Cancer Institute (K07-CA114315), and a grant from the Maurice Falk Foundation. Dr. Primack had full access to all data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. The authors thank Drs. Mary Hoban and E. Victor Leino for their assistance with data management.
References
- 1.Mokdad AH, Marks JS, Stroup DF, et al. Actual causes of death in the United States, 2000. J Am Med Assoc. 2004;291:1238–1245. doi: 10.1001/jama.291.10.1238. [DOI] [PubMed] [Google Scholar]
- 2.Centers for Disease Control and Prevention. Cigarette use among high school students—United States, 1991–2005. MMWR Morb Mortal Wkly Rep. 2006;55:724–726. [PubMed] [Google Scholar]
- 3.Kilmer G, Roberts H, Hughes E, et al. Surveillance of certain health behaviors and conditions among states and selected local areas—Behavioral Risk Factor Surveillance System (BRFSS). United States, 2006. MMWR Surveill Summ. 2008;57:1–188. [PubMed] [Google Scholar]
- 4.Cigarette sales in US reach historic 55-year low. Washington, DC: National Association of Attorneys General; 2006. Mar 8, National Assocation of Attorneys General. [Google Scholar]
- 5.Primack BA, Sidani JE, Agarwal AA, et al. Prevalence of and associations with waterpipe smoking among US university students. Ann Behav Med. 2008;36:81–86. doi: 10.1007/s12160-008-9047-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Eissenberg T, Ward KD, Smith-Simone S, et al. Waterpipe tobacco smoking on a U.S. college campus: Prevalence and correlates. J Adolesc Health. 2008;10:526–529. doi: 10.1016/j.jadohealth.2007.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Smith SY, Curbow B, Stillman FA. Harm perception of nicotine products in college freshmen. Nicotine Tob Res. 2007;9:977–982. doi: 10.1080/14622200701540796. [DOI] [PubMed] [Google Scholar]
- 8.Smith-Simone S, Maziak W, Ward KD, et al. Waterpipe tobacco smoking: Knowledge, attitudes, beliefs, and behavior in two U.S. samples. Nicotine Tob Res. 2008;10:393–398. doi: 10.1080/14622200701825023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Primack BA, Walsh M, Eissenberg TE. Waterpipe tobacco smoking among middle and high school students. Pediatrics. 2009;123:e282–e288. doi: 10.1542/peds.2008-1663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.World Health Organization. TobReg Advisory Note: Waterpipe tobacco smoking: Health effects, research needs and recommended actions by regulators. Geneva, Switzerland: World Health Organization; 2005
- 11.Shafagoj YA, Mohammed FI, Hadidi KA. Hubble-bubble (water pipe) smoking: Levels of nicotine and cotinine in plasma, saliva and urine. Int J Clin Pharmacol Ther. 2002;40:249–255. doi: 10.5414/cpp40249. [DOI] [PubMed] [Google Scholar]
- 12.Shihadeh A. Investigation of the mainstream smoke aerosol of the argileh water pipe. Food Chem Toxicol. 2003;41:143–152. doi: 10.1016/s0278-6915(02)00220-x. [DOI] [PubMed] [Google Scholar]
- 13.Shihadeh A, Saleh R. Polycyclic aromatic hydrocacrbons, carbon monoxide, “tar”, and nicotine in the mainstream smoke aerosol of the narghile water pipe. Food Chem Toxicol. 2005;43:655–661. doi: 10.1016/j.fct.2004.12.013. [DOI] [PubMed] [Google Scholar]
- 14.El-Nachef WN, Hammond SK. Exhaled carbon monoxide with waterpipe use in US students. J Am Med Assoc. 2008;299:36–38. doi: 10.1001/jama.2007.6. [DOI] [PubMed] [Google Scholar]
- 15.Neergaard J, Singh P, Job J, et al. Waterpipe smoking and nicotine exposure: A review of the current evidence. Nicotine Tob Res. 2007;9:987–994. doi: 10.1080/14622200701591591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Bedwani R, Renganathan E, El-Kwhsky F, et al. Epidemiology of bladder cancer in Alexandria, Egypt: Tobacco smoking. Int J Cancer. 1997;73:64–67. doi: 10.1002/(sici)1097-0215(19970926)73:1<64::aid-ijc11>3.0.co;2-5. [DOI] [PubMed] [Google Scholar]
- 17.Maziak W, Ward WD, Eissenberg T. Factors related to frequency of narghile (waterpipe) use: The first insights on tobacco dependence in narghile users. Drug Alcohol Depend. 2004;76:101–106. doi: 10.1016/j.drugalcdep.2004.04.007. [DOI] [PubMed] [Google Scholar]
- 18.Ward KD, Eissenberg T, Rastam S, et al. The tobacco epidemic in Syria. Tob Control. 2006;15:24–29. doi: 10.1136/tc.2005.014860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Jabbour S, El-Roueiheb Z, Sibai AM. Narghile (water-pipe) smoking and incident coronary heart disease: A case-control study. Ann Epidemiol. 2003;13:570. [Google Scholar]
- 20.Nattiv A, Puffer JC, Green GA. Lifestyles and health risks of collegiate athletes: A multi-center study. Clin J Sport Med. 1997;7:262–272. doi: 10.1097/00042752-199710000-00004. [DOI] [PubMed] [Google Scholar]
- 21.Patterson F, Lerman C, Kaufmann VG, et al. Cigarette smoking practices among American college students: Review and future directions. J Am Coll Health. 2004;52:203–210. doi: 10.3200/JACH.52.5.203-212. [DOI] [PubMed] [Google Scholar]
- 22.Peretti-Watel P, Guagliardo V, Verger P, et al. Sporting activity and drug use: Alcohol, cigarette and cannabis use among elite student athletes. Addiction. 2003;98:1249–1256. doi: 10.1046/j.1360-0443.2003.00490.x. [DOI] [PubMed] [Google Scholar]
- 23.Rigotti NA, Lee JE, Wechsler H. US college students’ use of tobacco products: Results of a national survey. J Am Med Assoc. 2000;284:699–705. doi: 10.1001/jama.284.6.699. [DOI] [PubMed] [Google Scholar]
- 24.Wechsler H, Davenport AE, Dowdall GW, et al. Binge drinking, tobacco, and illicit drug use and involvement in college athletics. A survey of students at 140 American colleges. J Am Coll Health. 1997;45:195–200. doi: 10.1080/07448481.1997.9936884. [DOI] [PubMed] [Google Scholar]
- 25.Moore MJ, Werch C. Relationship between vigorous exercise frequency and substance use among first-year drinking college students. J Am Coll Health. 2008;56:686–690. doi: 10.3200/JACH.56.6.686-690. [DOI] [PubMed] [Google Scholar]
- 26.Yusko DA, Buckman JF, White HR, et al. Alcohol, tobacco, illicit drugs, and performance enhancers: A comparison of use by college student athletes and nonathletes. J Am Coll Health. 2008;57:281–290. doi: 10.3200/JACH.57.3.281-290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Martens MP, Dams-O’Connor K, Beck NC. A systematic review of college student-athlete drinking: Prevalence rates, sport-related factors, and interventions. J Subst Abuse Treat. 2006;31:305–316. doi: 10.1016/j.jsat.2006.05.004. [DOI] [PubMed] [Google Scholar]
- 28.Morrell HER, Cohen LM, Bacchi D, et al. Predictors of smoking and smokeless tobacco use in college students: A preliminary study using Web-based survey methodology. J Am College Health. 2005;54:108–115. doi: 10.3200/JACH.54.2.108-115. [DOI] [PubMed] [Google Scholar]
- 29.Sax LJ, Gilmartin SK, Bryant AN. Assessing response rates and nonresponse bias in web and paper surveys. Res High Educ. 2003;44:409–431. [Google Scholar]
- 30.White AM, Jamieson-Drake DW, Swartzwelder HS. Prevalence and correlates of alcohol-induced blackouts among college students: Results of an E-mail survey. J Am Coll Health. 2002;51:117–131. doi: 10.1080/07448480209596339. [DOI] [PubMed] [Google Scholar]