A 52-year-old woman was referred for evaluation of a persistent dry cough and episodic hemoptysis of about 20 years’ duration. These symptoms were thought to be caused by chronic laryngopharyngitis and had been treated with various antitussive agents. Her medical history was otherwise unremarkable, and physical examination showed no abnormalities.
Serial chest radiographs over the years had been normal. Multidetector computed tomography (CT) of the chest showed multiple calcified nodules protruding from the anterolateral wall of the trachea and sparing of the posterior tracheal membrane (Figures 1A and 1B). These projecting spicules involved the whole length of the trachea and did not obstruct the lumen (Figure 1B). Three-dimensional volume-rendered imaging, functioning as virtual bronchoscopy (Figure 1C), delineated the distinct nodular mucosa of the anterolateral tracheal wall and its extent. These findings were confirmed with conventional fibreoptic bronchoscopy. On microscopy, sections of the spicules showed bronchial cartilage and lamellar bone negative for amyloid staining, which was compatible with a diagnosis of tracheobronchopathia osteochondroplastica.
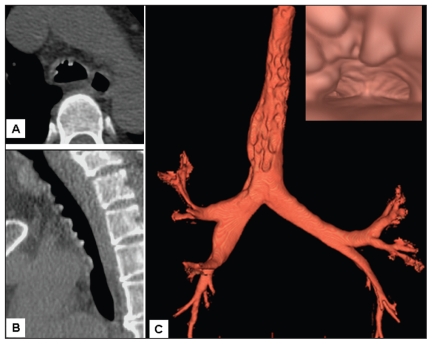
Figure 1:
Chest multidetector computed tomography in a 52-year-old woman with chronic cough. Transaxial section shows multiple calcified nodules at the anterolateral wall of the trachea (A), and sagittal section of the trachea shows typical sparing of the posterior membrane (B). Three-dimensional volume-rendered imaging, functioning as virtual bronchoscopy, shows protruding nodules along the whole trachea (C); the nodules look like stalactites (insert).
Tracheobronchopathia osteochondroplastica is an uncommon disorder of unknown cause. Incidence rates range from 1 in 125 to 1 in 6000 patients, as judged by in vivo bronchoscopy.1 It has been reported that 54% of patients with this disease have chronic cough.2 The diagnosis is usually established with bronchoscopy to assess lack of response to usual medical therapy. Chest CT may show multiple sessile submucosal nodules with or without calcification along the cartilaginous portion of trachea. However, CT is not sensitive enough to detect milder forms of the disease.1 Bronchoscopy is useful for ruling out other causes based on findings from computed tomography, such as amyloidosis, sarcoidosis or infection.1
Although tracheobronchopathia osteochondroplastica is generally a benign disease that progresses very slowly and needs no specific treatment,3 it has been reported to cause respiratory insufficiency from tracheal stenosis, which requires surgical intervention.4,5
Footnotes
This article has been peer reviewed.
Competing interests: None declared.
REFERENCES
- 1.Prakash UB. Uncommon causes of cough: ACCP evidence-based clinical practice guidelines. Chest 2006;129(Suppl):206S–19S [DOI] [PubMed] [Google Scholar]
- 2.Leske V, Lazor R, Coetmeur D, et al. Tracheobronchopathia osteochondroplastica: a study of 41 patients. Medicine 2001;80:378–90 [DOI] [PubMed] [Google Scholar]
- 3.Shigematsu Y, Sugio K, Yasuda M, et al. Tracheobronchopathia osteochondroplastica occurring in a subsegmental bronchus and causing obstructive pneumonia. Ann Thorac Surg 2005;80:1936–8 [DOI] [PubMed] [Google Scholar]
- 4.Hantous-Zannad S, Sebai L, Zidi A, et al. Tracheobronchopathia osteochondroplastica presenting as a respiratory insufficiency: diagnosis by bronchoscopy and MRI. Eur J Radiol 2003;45:113–6 [DOI] [PubMed] [Google Scholar]
- 5.Molloy AR, McMahon JN. Rapid progression of tracheal stenosis associated with tracheopathia osteochondroplastica. Intensive Care Med 1988;15:60–2 [DOI] [PubMed] [Google Scholar]