Abstract
Hypothermia among newborns is considered an important contributor to neonatal morbidity and mortality in low resource settings. However, in these settings only limited progress has been made towards understanding the risk of mortality subsequent to hypothermia, describing how this relationship is dependent on both the degree or severity of exposure and the gestational age and weight status of the baby, and implementing interventions to mitigate both exposure and the associated risk of poor outcomes. Given the centrality of averting neonatal mortality to achieving global milestones towards reductions in child mortality by 2015, recent years have seen substantial resources and efforts to improve understanding of global epidemiology of neonatal health. In this seminar, a summary of the burden, consequences, and risk factors of neonatal hypothermia in low-resources settings is presented, with a particular focus on community-based data. Context-appropriate interventions for reducing hypothermia exposure and the role of these interventions in reducing global neonatal mortality burden are explored.
Introduction
Each year an estimated 3.6 million neonatal deaths occur1, primarily due to infection, complications of preterm birth, and intrapartum-related hypoxic events2. Infections are estimated to account for approximately one-third of the global burden of neonatal death, with estimates rising to more than half in high mortality settings2. One of the best-recognized signs of infection is fever, or an increase in body temperature of the newborn. However, the importance of abnormally low body temperature (hypothermia) in newborns remains less well understood in terms of its contribution to neonatal mortality and morbidity, especially in low resource settings. The study of hypothermia, its incidence, risk factors, and consequences is not new. For at least two hundred years, the need to maintain an optimal body temperature for babies, especially those born prematurely, has been recognized, and is reflected by the development and improvement of early models of incubators during the 19th century3. These efforts were led by Parisian obstetrician, Dr. Pierre Budin (1846-1907), who was among the first to demonstrate a potential relationship between temperature and mortality risk among newborns3,4, and who included “warmth” and “keeping the baby with the mother” as two of the key components of appropriate management of the newborn infant. Reports of sclerema neonatorum and its possible association with neonatal cold injury also date to the 19th century5,6. More concentrated efforts to understand neonatal thermal regulation, the optimal thermal environment, and factors related to maintaining this environment were carried out via a series of studies in the mid 20th century, establishing our basic knowledge of the physiology of temperature control in newborns7-10.
Neonatal hypothermia as a factor contributing to morbidity and mortality risk of newborns has been recognized by the World Health Organization (WHO)11. Hypothermia has been defined by WHO as body temperature below the normal range (36.5°C – 37.5°C) and has been sub-classified into three grades: mild (36.0°C – 36 .5°C), moderate (32.0°C – 35.9°C), and severe (<32.0°C) hypothermia 11. For each of these classifications, there are guidelines in place for responding to or managing hypothermia12. Furthermore, the WHO has published guidelines on thermal care and has included thermal care of newborns as one of the elements of essential newborn care (ENC) that should be provided to all newborns regardless of setting13. Despite this recognition within global guidelines and recommendations for neonatal care, there are major gaps in our understanding of the burden, risk factors, and consequences of neonatal hypothermia in the very settings where exposure is greatest14. Additionally, there has been limited progress in identifying the optimal approaches to preventing hypothermia or mitigating its consequences through rapid and appropriate management in low-resource settings15. This is especially true in locations where a large proportion of births occur at home; in these settings there are very few data available even on the epidemiology of neonatal hypothermia, much less sufficient evidence on the role that thermal care practices may have in either hypothermia prevention or management, and thus, their potential role in improving neonatal survival.
In this seminar, the pathophysiology of neonatal hypothermia is briefly discussed and the epidemiology of neonatal hypothermia in low-resource settings is reviewed. Studies that have estimated the incidence/prevalence of hypothermia in both hospital and community settings are summarized. The association between hypothermia and mortality is examined; particular attention is placed on estimation of how this relationship changes across the range of temperatures in the hypothermic range and is followed by a discussion on how variability in this relationship can inform choice of cutoffs for defining severity grades for hypothermia. Risk factors for developing hypothermia in low-resource settings are reviewed and intervention approaches and the potential of these approaches for both reducing burden and impacting upon neonatal deaths is discussed.
Thermal Regulation of the Newborn
Unlike poikilotherms whose body temperature can vary substantially with the external environment, humans are homeotherms and must generate heat to maintain a body temperature that varies only within a relatively small range (i.e. normal variance of only 0.3%)7. During development, the core body temperature of the fetus is closely correlated with the mother, and as such, the core temperature of the fetus will normally remain a consistent and approximate 1°C above that of the mother. After bir th, however, the baby is exposed to an environment that is often substantially cooler, and is subject to the four basic mechanisms through which all humans will start to lose heat. These processes are evaporative heat loss, which is a function of humidity, conduction (direct transfer of heat from baby to contact surface), convection (loss of heat to cooler surrounding air), and radiation (indirect transfer of heat to nearby lower temperature objects)7,11.
In order to avoid substantial heat loss due to these mechanisms, the core body temperature in children and adults is maintained through regulatory processes that include vasoconstriction, and shivering and non-shivering thermogenesis. However, the extent to which newborn babies can control thermoregulation to maintain an optimal core body temperature is limited, relative to children and adults. While shivering thermogenesis is quantitatively the most important mechanism in adults, for newborns the primary mechanism is through chemical thermogenesis, in the absence of muscular contraction and shivering3. Beyond the fact that physiological and behavioral responses are relatively immature in the term newborn, the limited ability of newborns to maintain core body temperature is particularly compromised among babies born prematurely or those with low birth weight. These babies have limited vasoconstriction capability compared to term infants16, greater surface-to-mass ratios, and preterm and/or low birth weight babies have lower brown fat deposits17 which are essential for non-shivering thermogenesis.
Heat loss through evaporation of the amniotic fluid from the baby's skin is the most important mechanism11. In addition, specific newborn care practices can contribute substantially to the loss of heat, especially in the first hours of life; these practices are more common in home births in developing countries, but unfortunately also occur among facility births. For example, birthing in an insufficiently warmed room, placing the baby uncovered on the ground, floor, or other surface while awaiting delivery of the placenta, insufficient or delayed drying or wrapping of the baby after birth, immediate bathing of the baby with cool or cold water and delayed drying, and delayed breastfeeding are all practices that might increase the risk of heat loss11. The heat loss occurs immediately after birth; continuous recording of body temperature in a variety of settings has demonstrated the initial drop is normally followed by a subsequent rise, which may depend on birth weight, ambient temperature, and proximity to the mother18-20. The initial loss of heat can be quite large; for example in the first 10-20 minutes after birth it is not uncommon for a baby to lose 2-4°C, with further subsequent losses possible in the presence of the above practices15.
Incidence of neonatal hypothermia in low-resource settings
As a consequence of both the factors surrounding the immediate care of newborns and the risk these pose for heat loss, and the innate features of the neonate, it is of little surprise that hypothermia is a common phenomenon in low resources settings, including among babies born in facilities and in the community.
Hospital-based studies
There have been numerous studies that have attempted to quantify the burden of neonatal hypothermia in low resource settings, but the majority of these has been conducted in hospital settings and thus do not necessarily provide a representation of the population-based burden. A sample of these hospital-based studies is described in Table 1; those selected represent both middle and low resource settings, are geographically variable, and from a variety of institutions. Overall, these hospital-based studies indicate that exposure to hypothermia as defined by the WHO is substantial, but also demonstrate the wide range of estimates of the proportion of babies that are observed as hypothermic. For example, near universal observation of temperatures in the hypothermia range has been reported among babies from Senegal21, Uganda22, Nepal23, and Turkey24 (Table 1). However, when the cutoff for defining hypothermia is reduced well below the WHO cutoff for any (i.e. mild, moderate, or severe) hypothermia (<36.5°C), the observed proportion of b abies deemed hypothermic is lower. For example studies with cutoffs at 35.0°C or 34.5°C in Table 1 (see Shimla, India25 and Bissau, Guinea-Bissau26) report much lower proportion of hypothermia babies. The frequent use of different cutoffs for defining hypothermia poses some difficulty for comparison across sites.
Table 1.
Selected facility-based estimates of the burden of hypothermia in newborns of low-resource settings
| Author, Year | Location | N | Definition | Outcome measure | Estimate |
|---|---|---|---|---|---|
| Briend, 198121 | Dakar, Senegal | 78 | <36.0°C | Point Prevalence | 94.9% |
| Byaruhanga, 200522 | Nsambya, Uganda | 300 | <36.5°C | Prevalence at 60 minutes after birtha | 83.0% |
| da Mota Silveira, 200335 | Recife, Brazil | 320 | <36.5°C | Prevalence at Admission | 31.6% |
| Zayeri, 200749 | Tehran, Iran | 900 | <36.5°C | Prevalence at 20 minutes after birth | 53.3% |
| Ogunlesi, 200837 | Sagamu, Nigeria | 150 | <36.5°C | Prevalence at admission | 62.0% |
| Sodemann, 200826 | Bissau, Guinea-Bissau | 2926 | <34.5°C | Prevalence with in 12 hours of birth | 8.1% |
| Johanson, 199223 | Kathmandu, Nepal | 495 | <36.0°C | Prevalence within 2 hours of birthb | 85.0% |
| Kambarami, 200350 | Harare, Zimbabwe | 313 | <36.0°C | Prevalence at admission to neo unit | 85.0% |
| Cheah, 200051 | Kuala Lumpur, Malaysia | 227 | <36.5°C | Prevalence immediately after birth | 25.6% |
| Sarman, 198924 | Istanbul, Turkey | 60 | <36.0°C | Prevalence at admission | 88.3% |
| Manji, 200352 | Dar-es-Salaam, Tanzania | 1632 | <36.0°C | Prevalence at admission | 22.4% |
| Kaushik, 199925 | Shimla, India | 2063 | <35.0°C | Prevalence within 24 hours | 2.9% |
Temperature was also assessed at 10, 30, and 90 minutes post delivery; proportion was 29, 82, and 79%, respectively
Temperature was also assessed at 24 hours after birth; the proportion was 48.9%
In addition to the underlying true variability in incidence of hypothermia, there are many study-specific factors that contribute to the wide range of estimates seen in these hospital-based studies. The most important of such factors is seasonality (i.e. when during the year was the study conducted), the age of the infants at first measurement, and the weight and gestational age distribution of the infants included. Other important elements to consider are method of measuring temperature (i.e. axillary vs rectal)27, frequency of measurement, and the cutoff used to classify babies as hypothermic26,28. Furthermore some of the estimates shown in Table 1 are among out-born sick babies presenting to a hospital, some included only hospital births that are admitted for special care to a neonatal nursery or intensive care unit, while others include a combination of in/out born as well as sick and well babies.
It is difficult to draw conclusions about either the overall incidence of hypothermia or the mortality risk associated with hypothermia from these studies. In addition to the lack of adjustment for important variables of seasonality, age at measurement, weight, and gestational age, these studies have other substantial sources of heterogeneity discussion above, and are not population-based. Given that a large proportion of babies are born at home and do not access the formal health system during the early neonatal period, and that these births contribute disproportionately to the global burden of neonatal death, it is critical to examine data available from community settings on both the incidence and association with mortality.
Community-Based Studies
There have been relatively few population-based studies that provide an estimate of the burden in specific settings; none are currently available from sub Saharan Africa. Three small cohort studies conducted in India have been published29-31. Among 189 home-born infants in villages of Haryana, the axillary temperature was less than 36.5°C among 21 babies (11.1%). In this study, temperature was recorded once within 24 hours after birth29. More frequent observation of babies occurred in another study, conducted as part of the SEARCH project in Gadchiroli30. Among 763 infants (95% of which were born at home), 130 (17.0%) were observed with temperatures less than 35.0°C over multiple vi sits through the first month of life (days 1, 2, 3, 5, 7, 15, 21, and 28). A larger and more recent study conducted by Darmstadt et al in Uttar Pradesh31 where 1732 babies had axillary temperature measures recorded within 36 hours (median age 16.0 hours), almost half (45%) of the infants were observed with temperatures <36.5°C. In all three of these studies there was so me evidence of seasonality; the proportion of hypothermic babies increased in the winter season, but still remained high in the warm period. For example, in the Haryana study, hypothermia was observed within 24 hours among 19.3% of babies in winter compared with 3.1% in summer, and in Uttar Pradesh, 70.0% of babies were hypothermic in the coldest quarter of the year, compared with 32.1% in the warmest quarter.
More recently, our group has published a series of articles14,28,32 on hypothermia among a large, population-based, universal cohort of newborns born in Sarlahi District in southern Nepal. Between 2002 and 2006, more than 23,000 babies from the northern third of the district (population ~280,000) were enrolled in a community-based cluster randomized trial of chlorhexidine antisepsis interventions of the skin33 and umbilical cord34. All live born babies during the period of the study were included in the cohort, regardless of the place of birth; approximately 92% of babies were born at home. The infants were visited at home repeatedly by project workers: daily through the first 4 days after birth, then every other day until mid-way through the neonatal period, and then on days 21 and 28 (maximum 11 visits). At each of these visits, project workers recorded axillary temperature using a digital thermometer (a total of 213,616 axillary temperature measures were collected). Ambient temperature and age of measurements in hours was available for each one of these measurements.
In this study, 21,459 of 23,240 babies (92.3%) had one or more axillary temperature measures <36.5°, half of babies were moderately to severely hypothermic, and risk peaked in the first 24-72 hours of life. The risk of moderate-to-severe hypothermia increased by 41.3% for each 5°C decrease in ambient temperature. Even in t he hottest season of the year, almost one-fifth of babies were hypothermic. The key results of the smaller community studies and the data from this large population-based cohort are presented in Table 2.
Table 2.
Incidence of hypothermia in community-based studies from South Asia
| Author, Year | Location | N | Measurement(s) and Definition(s) | Key Findings | |
|---|---|---|---|---|---|
| Kumar, 199829 | Haryana, India | 189 | Axillary temperatures within 24 hours of life | <35.6°C | •11.1% hypothermic •19.3% winter vs. 3.1% in summer |
| Bang, 200530 | Gadchiroli, India | 763 | Axillary temperatures on days 1, 2,3,5,7,15,21,28 | <35.0°C | •17.0% hypothermic •21.5% winter vs. 13.8% in summer |
| Darmstadt, 200631 | Uttar Pradesh, India | 1732 | Axillary temperatures as soon as possible after birth (range 3-36 h) | <36.5°C | •45% overall •70% in coldest quarter vs 20% in warmest quarter |
| Mullany, 201014 | Sarlahi, Nepal | 23,240 | Axillary temperatures on days 1-4,6,8,10,14,21,28 | <36.5°C | •92.3% overall •RR of hypothermia 4.03 times higher in coldest quintile vs warmest quintile of ambient temperature |
| <36.0°C <32.0 |
• 48.6% overall | ||||
Consequences of neonatal hypothermia in low-resource settings
A number of the hospital- and community-based studies described above have also examined case-fatality rates between those babies with and without hypothermia, and concluded that the risk of mortality is higher among those exposed (Table 3). An analysis of 320 babies arriving at a tertiary care facility in Recife, Brazil indicated that moderate (32.0°C – 35.9°C) hypothermia on admission was an independent risk factor for neonatal death (adjusted OR=3.49 [95%CI: 3.18 – 3.81])35. In Iran, mortality was higher among babies with rectal temperatures less than 36.5°C 20 minutes after birt h (8.8%) compared to normothermic babies (2.6%), but these were not adjusted for important factors such as weight and gestational age36.
Table 3.
Selected studies of the association between hypothermia and mortality risk in hospital and communities of low resource settings
| Author, Year | Location | N | Study Type | Key Mortality Findings |
|---|---|---|---|---|
| da Mota Silveira, 200335 | Recife, Brazil | 320 | Hospital | • Adjusted odds of death among babies with hypothermia was OR=3.49 [95%CI: 3.18 – 3.81]) |
| Zayeri, 200749 | Tehran, Iran | 900 | Hospital | • Unadjusted fatality was 8.8% among hypothermic babies compared to 2.6 among normothermic |
| Ogunlesi, 200837 | Sagamu, Nigeria | 150 | Hospital | • Unadjusted fatality rate among hypothermic babies was 2.26 [95%CI: 1.14 – 4.48] higher than normothermic babies |
| Bang, 200530 | Gadchiroli, India | 763 | Hospital to Community | • Case-fatality of hypothermia was 15.4%, and was significantly higher than those without hypothermia |
| Sodemann 200826 | Bissau, Guinea-Bissau | 2926 | Community | •Adjusted for weight, temperatures <34.5°C were associated with mortality 4.81 [95%CI: 2.90 – 8.00] times higher in the first 7 days of life •Hypothermia-associated mortality risk was elevated through 2 months of life |
| Mullany, 201014 | Sarlahi, Nepal | 23,240 | Community | •Adjusted mortality risk increased 80% for every 1°C decrease in first observed axillary temperature •Adjusted mortality risk was 6.11 [95%CI: 3.98 – 9.38] times higher among babies <35.0°C •Preterm babies at higher risk of hypothermia-associated mortality |
Relative to normothermic babies, unadjusted case-fatality was also more than two-fold higher among the 62.0% of babies who were hypothermic upon admission in Nigeria (CFR=2.26 [95%CI: 1.14 – 4.48])37.
Efforts to link population-based estimates of hypothermia exposure to subsequent mortality are even fewer. In the Bang study above30, the case-fatality among 130 infants with hypothermia was estimated at 15.4%. Unfortunately, the study size was small (763 infants with only 20 deaths) and only a single fixed axillary temperature cutoff (35.0°C) was used to classify infants. In one of the studies highlighted in Table 1 where temperature measurements were made in a hospital setting in Guinea Bissau26, investigators were able to go back to the community and estimate overall neonatal and post-neonatal mortality rates among infants with exposure to hypothermia. Strengths of this study include the early timing and near uniformity of the ambient temperature at the time of the measurement, and the high rates of community-based follow-up that was achieved. Since delivery rates in the hospital were very high, the near-complete follow up of vital status for each of the babies leads to a population-based estimate of mortality associated with temperature. Furthermore, the investigators had sufficient data to construct a limited temperature-specific mortality function, which was then utilized to select an appropriate cut-off for examining mortality. Those with temperatures <34.5°C were at almost 5 times higher mortality risk in the first week of life, and risk remained elevated through 2 months of age26.
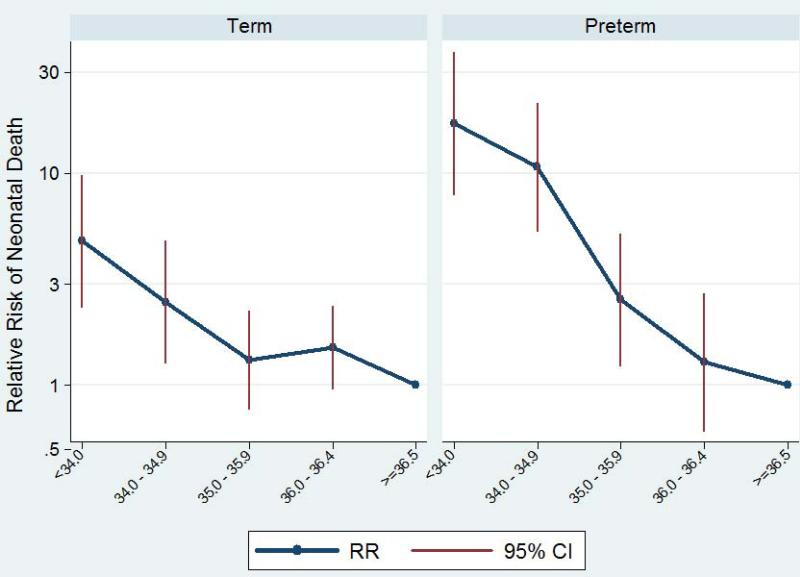
More recently, the population-based data from Nepal was utilized to examine the relationship between axillary temperature over the entire range of hypothermia values and mortality subsequent to the first temperature observed28. We found that after adjusting for age and ambient temperature at measurement and other covariates (such as sex, weight, gestational age, ethnicity, etc), mortality was increased by approximately 80% for every degree decrease in first observed axillary temperature. Mortality associated with hypothermia was substantially higher among preterm babies, and relative risk of death ranged from 2 to 30 times within the current WHO classification for moderate hypothermia, increasing with greater severity of hypothermia28.
Both our study and the work by Sodemann and colleagues in Guinea Bissau strongly suggest that the current WHO classification scheme for hypothermia might be adjusted to more appropriately reflect the overall mortality-hypothermia risk relationship. In particular, we have suggested that the current “moderate” category is too wide (32.0°C to 35.9°C) and includes in a single classification exposures that have substantially different consequences. One solution we have proposed28 is to expand the “severe” category to exposures <34.0°C (Grade 4) and split the remainder of the “moderate” category into two separate categories (Grade 3: 34.0°C – 34.9°C and Grade 2: 35.0°C – 35.9°C). This new clas sification system better reflects the dependence of subsequent mortality risk across the range of observable temperatures, heightens the awareness of hypothermia by expanding the most severe category, and allows better flexibility in guidelines for appropriate actions which can be targeted by risk profile (i.e. for low birth weight or premature babies) (Table 4).
Table 4.
Possible new classification system for neonatal hypothermia
| Grade | Definition | Proportion in rural Nepala | Adjusted Mortality Riska | Possible Guideline | |
|---|---|---|---|---|---|
| Preterm | Full Term | ||||
| Normothermic | [36.5 – 37.5) | 42.8% | 1.00 | ||
| Grade 1 | [36.0 – 36.5) | 25.6% | 1.51 | • Reinforcement of thermal care messages | • Reinforcement of thermal care messages |
| Grade 2 | [35.0 – 36.0) | 21.1% | 1.75 | • Immediate in-home demonstration of improved thermal care plus follow up visits | • Reinforcement of thermal care messages |
| Grade 3 | [34.0 – 35.0) | 6.9% | 5.03 | • Immediate skilled care and referral | • Immediate in-home demonstration of improved thermal care plus follow up visits |
| Grade 4 | <34.0 | 3.6% | 9.21 | • Immediate skilled care and referral | |
Data from population-based study in rural Sarlahi District, Nepal28
Risk factors for neonatal hypothermia
In order to design effective strategies for reducing both the risk of hypothermia and the negative consequences, an improved understanding of factors that lead to hypothermia is required. Kumar et al provide a detailed discussion of possible risk factors for neonatal hypothermia, classifying these factors into contextual (e.g. seasonality), physiological (e.g. low birth weight), behavioral (e.g. early bathing), and socio-economic factors (e.g. poverty)15. Behavioral factors appear to play a central role in risk of hypothermia and are highlighted by the WHO's guidelines to optimize thermal care, described as a warm chain11. The warm-chain consists of 10 steps to minimize risk of exposure and includes the following: keeping the delivery room warm, drying immediately, skin-to-skin contact, breastfeeding, delayed bathing, appropriate clothing, warm transport (if necessary), keeping mother and baby together, warm resuscitation, and improved awareness and recognition of hypothermia risk. Importantly, there are very few data that explicitly link these factors, or other newborn care and behavioral practices to observations of neonatal hypothermia. Rather, the link has generally been ecological in nature; that is, in settings where hypothermia incidence or prevalence is high, this observation has been explained by describing concurrent observations of behaviors or factors that are obstacles to achieving the WHO-recommended warm-chain. While Kumar et al15 provide some specific examples of settings where behaviors such as early bathing or delayed wrapping are common, the authors also note that insufficient data are available on risk factors in community settings.
There are two factors that appear to be of paramount importance: seasonality and preterm/low birth weight; and substantially more information is available to quantify the role these factors play. Furthermore, the degree to which the above-discussed behavioral factors will increase risk of hypothermia depends significantly on the status of these two determining factors. Data in Table 2 provide an indication of the importance of ambient temperature. It is critical to note that risk of hypothermia remains high even in the hot season of tropical climates, and that the disparity between low birth weight and normal birth weight infants in terms of hypothermia risk may be elevated during warmer periods. Community-based data from Nepal32 indicate that hypothermia risk is correlated closely along the entire spectrum of body weight. For every 100 gram decrement in weight below 2000 grams, hypothermia risk increased by 31.3%; risks were lower but still significant for weight decrements between 2000 and 2500 grams (13.5% per 100 grams) and between 2500 and 3000 grams (7.4% per 100 grams).
The compromised ability of low birth weight and preterm babies to thermoregulate (discussed above) leads to both higher incidence of hypothermia among these babies and more severe consequences; this observation too is not new. Case-fatality in hospital settings was noted to vary substantially by weight and prematurity of the baby; more than 100 years ago Pierre Budin published case-fatality estimates by weight of the newborn4. Among 318 infants whose temperature upon admission was less than 33.5°C, case-fatality was uniformly high, but was highest among those <1500 grams (171/175, 97.7%) compared to babies 1500-1999 grams (109/122, 89.3%) or those >=2000 g (15/21, 71.4%)4. The community-based hypothermia-mortality risk relationship among rural babies from Nepal was modified substantially by pre-term status (Figure 1)28.
Figure 1.
Relative risk of neonatal death subsequent to hypothermia, by preterm status. (Adapted from Mullany, 201028)
Interventions to prevent neonatal hypothermia
Given the high incidence and serious consequences of hypothermia in low-resource settings and the limitations that these settings present in implementing standard warming techniques (including incubators) of higher-resource settings, the focus in low-resource facilities and communities is on behavioral practices. The WHO has provided guidelines for thermal care in low-resource settings and the 10-step warm chain described above highlights specific practices that need to be promoted for both home and facility births. A specific recommendation is to delay bathing for at least six hours after birth; a randomized trial in a Ugandan hospital showed that bathing of newborns increased hypothermia even in the presence of skin-to-skin contact and the use of warm water38. Another recommendation for reducing risk of hypothermia or for re-warming babies that are already exposed is skin-to-skin contact. The transfer of heat from mother (or other caretaker) to the newborn facilitated by direct skin contact has been demonstrated to be at least as effective as incubator care for rewarming39 and for preventing hypothermia in preterm low birth weight babies40. A number of summaries of skin to skin care and its benefits for reducing hypothermia risk have been published15,31, including a meta analysis indicating improved survival among preterm babies <2000 grams in hospitals41. Early initiation of breastfeeding (i.e. within 24 hours) can reduce the risk of hypothermia32, and exclusive breastfeeding was associated with lower hypothermia among babies in a Zambian hospital42. Early breastfeeding reduces hypothermia risk through close contact with the mother and provides the fat supply essential for active heat production in newborns20,43; this mechanism may be partially responsible for the observed lower mortality among newborns breastfed within 24 hours44,45.
In recent years, a number of studies have demonstrated that packages of neonatal care practices delivered at the community level can substantially reduce mortality46,47. Many of these integrated packages include messages targeted towards improved thermal care and it is possible that the thermal care component played a critical role in the overall mortality reductions observed. An excellent example is provided by an integrated package of behavioral interventions promoted by outreach workers in rural Shivgarh, India48. Here behavioral change communications focused on early breastfeeding initiation, skin-to-skin contact, delayed bathing, and immediate wrapping and drying, as well as hygiene (clean delivery and cord care), and resulted in a 54% reduction in neonatal mortality. Teasing out individual components of studies like these that test integrated packages is challenging, and further work is needed to refine estimates of the potential reductions in all-cause and cause-specific neonatal mortality that are achievable through improved thermal care practices.
Conclusion
Newborn hypothermia remains one of the most important contributors to neonatal mortality and morbidity in both facilities and communities of low-resource settings. Recent data from the community in Nepal and India have expanded our understanding of the population-based burden in South Asia, and the hypothermia-mortality risk relationship is becoming increasingly clear. While no community-based data are available from sub-Saharan Africa, a number of current and future studies of interventions to improve neonatal survival will likely provide clarity on the burden and consequences of hypothermia in these settings. Neonatal health promotion programs for home births need to focus on the behavioral changes necessary to optimize thermal care of newborns, especially in the hours immediately after birth. Research to further elucidate both the impact of specific thermal care interventions on hypothermia risk and the overall contribution of these practices in improving survival is required.
Acknowledgments
Support: This work was supported by a grant from the National Institute of Child Health and Development (NICHD, HD0553466).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Black RE, Cousens S, Johnson HL, Lawn JE, Rudan I, Bassani DG, et al. Global, regional, and national causes of child mortality in 2008: as systematic analyis. Lancet. 2010;375:1969–87. doi: 10.1016/S0140-6736(10)60549-1. [DOI] [PubMed] [Google Scholar]
- 2.Lawn JE, Wilczynska-Ketende K, Cousens SN. Estimating the causes of 4 million neonatal deaths in the year 2000. Int J Epidemiol. 2006;35:706–718. doi: 10.1093/ije/dyl043. [DOI] [PubMed] [Google Scholar]
- 3.Stern L. Thermoregulation in the Newborn Infant: Historical, Physiological and Clinical Considerations In: Historical Review and Recent Advances in Neonatal and Perinatal Medicine. In: Smith George F, Vidyasagar Dharmapuri., editors. Published by Mead Johnson Nutritional Division; 1980. [Google Scholar]
- 4.Budin P, Carr WL. The nursling.the feeding and hygiene of premature and full-term infants. Imperial Publ. Co.,Caxton Publ. Co; New York,London: 1906. [Google Scholar]
- 5.Ballantyne JW. Remarks On Sclerema & Œdema Neonatorum. The British Medical Journal. 1890;1:403–406. doi: 10.1136/bmj.1.1521.403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Zeb A, Darmstadt GL. Sclerema neonatorum: a review of nomenclature, clinical presentation, histological features, differential diagnoses and management. J Perinatol. 2008;28:453–460. doi: 10.1038/jp.2008.33. [DOI] [PubMed] [Google Scholar]
- 7.Polin RA, Fox WW, Abman SH. Fetal and neonatal physiology. 3rd ed. Saunders; Philadelphia: 2004. [Google Scholar]
- 8.Day RL, Caliguiri L, Kamenski C, Ehrlich F. Body Temperature and Survival of Premature Infants. Pediatrics. 1964;34:171–181. [PubMed] [Google Scholar]
- 9.Silverman WA, Fertig JW, Berger AP. The influence of the thermal environment upon the survival of newly born premature infants. Pediatrics. 1958;22:876–886. [PubMed] [Google Scholar]
- 10.Brueck K. Temperature regulation in the newborn infant. Biol Neonat. 1961;3:65–119. [Google Scholar]
- 11.World Health Organization . Thermal protection of the newborn: A practical guide. World Health Organization; Geneva: 1997. Report No.: WHO/RHT/MSM/97.2. [Google Scholar]
- 12.World Health Organization . Pregnancy, childbirth, postpartum, and neonatal care: A guide for essential practice. World Health Organization; Geneva: 2007. [PubMed] [Google Scholar]
- 13.World Health Organization . Essential newborn care. 1996. Report No.: WHO/FRH/MSM/96.13. [Google Scholar]
- 14.Mullany LC, Katz J, Khatry SK, Leclerq SC, Darmstadt GL, Tielsch JM. Incidence and seasonality of hypothermia among newborns in southern Nepal. Arch Pediatr Adolesc Med. 2010;164:71–77. doi: 10.1001/archpediatrics.2009.239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kumar V, Shearer JC, Kumar A, Darmstadt GL. Neonatal hypothermia in low resource settings: a review. J Perinatol. 2009;29:401–412. doi: 10.1038/jp.2008.233. [DOI] [PubMed] [Google Scholar]
- 16.Knobel RB, Holditch-Davis D, Schwartz TA, Wimmer JE., Jr Extremely low birth weight preterm infants lack vasomotor response in relationship to cold body temperatures at birth. J Perinatol. 2009;29:814–821. doi: 10.1038/jp.2009.99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Aherne W, Hull D. Brown adipose tissue and heat production in the newborn infant. J Pathol Bacteriol. 1966;91:223–234. doi: 10.1002/path.1700910126. [DOI] [PubMed] [Google Scholar]
- 18.Ellis M, Manandhar N, Shakya U, Manandhar DS, Fawdry A, Costello AM. Postnatal hypothermia and cold stress among newborn infants in Nepal monitored by continuous ambulatory recording. Arch Dis Child Fetal Neonatal Ed. 1996;75:F42–5. doi: 10.1136/fn.75.1.f42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Robertson NJ, Nakakeeto M, Hagmann C, Cowan FM, Acolet D, Iwata O, Allen E, Elbourne D, Costello A, Jacobs I. Therapeutic hypothermia for birth asphyxia in low-resource settings: a pilot randomised controlled trial. Lancet. 2008;372:801–803. doi: 10.1016/S0140-6736(08)61329-X. [DOI] [PubMed] [Google Scholar]
- 20.Christensson K, Ransjo-Arvidson AB, Kakoma C, Lungu F, Darkwah G, Chikamata D, Sterky G. Midwifery care routines and prevention of heat loss in the newborn: a study in Zambia. J Trop Pediatr. 1988;34:208–212. doi: 10.1093/tropej/34.5.208-a. [DOI] [PubMed] [Google Scholar]
- 21.Briend A, de Schampheleire I. Neonatal hypothermia in West Africa. Lancet. 1981;1:846–847. doi: 10.1016/s0140-6736(81)92730-6. [DOI] [PubMed] [Google Scholar]
- 22.Byaruhanga R, Bergstrom A, Okong P. Neonatal hypothermia in Uganda: prevalence and risk factors. J Trop Pediatr. 2005;51:212–215. doi: 10.1093/tropej/fmh098. [DOI] [PubMed] [Google Scholar]
- 23.Johanson RB, Spencer SA, Rolfe P, Jones P, Malla DS. Effect of post-delivery care on neonatal body temperature. Acta Paediatr. 1992;81:859–863. doi: 10.1111/j.1651-2227.1992.tb12123.x. [DOI] [PubMed] [Google Scholar]
- 24.Sarman I, Can G, Tunell R. Rewarming preterm infants on a heated, water filled mattress. Arch Dis Child. 1989;64:687–692. doi: 10.1136/adc.64.5.687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kaushik S, Grover N, Parmer VR, Grover PS, Kaushik R. Neonatal morbidity in a hospital at Shimla. Indian J Pediatr. 1999;66:15–19. doi: 10.1007/BF02752343. [DOI] [PubMed] [Google Scholar]
- 26.Sodemann M, Nielsen J, Veirum J, Jakobsen MS, Biai S, Aaby P. Hypothermia of newborns is associated with excess mortality in the first 2 months of life in Guinea-Bissau, West Africa. Trop Med Int Health. 2008;13:980–986. doi: 10.1111/j.1365-3156.2008.02113.x. [DOI] [PubMed] [Google Scholar]
- 27.Craig JV, Lancaster GA, Williamson PR, Smyth RL. Temperature measured at the axilla compared with rectum in children and young people: systematic review. BMJ. 2000;320:1174–1178. doi: 10.1136/bmj.320.7243.1174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Mullany LC, Katz J, Khatry SK, LeClerq SC, Darmstadt GL, Tielsch JM. Hypothermia during the neonatal period and associated risk of mortality in southern Nepal. Arch Ped Adolesc Med. 2010;164:650–656. doi: 10.1001/archpediatrics.2010.103. [DOI] [PubMed] [Google Scholar]
- 29.Kumar R, Aggarwal AK. Body temperatures of home delivered newborns in north India. Trop Doct. 1998;28:134–136. doi: 10.1177/004947559802800304. [DOI] [PubMed] [Google Scholar]
- 30.Bang AT, Reddy HM, Baitule SB, Deshmukh MD, Bang RA. The incidence of morbidities in a cohort of neonates in rural Gadchiroli, India: seasonal and temporal variation and a hypothesis about prevention. J Perinatol. 2005;25(Suppl 1):S18–28. doi: 10.1038/sj.jp.7211271. [DOI] [PubMed] [Google Scholar]
- 31.Darmstadt GL, Kumar V, Yadav R, Singh V, Singh P, Mohanty S, Baqui AH, Bharti N, Gupta S, Misra RP, Awasthi S, Singh JV, Santosham M. Introduction of community-based skin-to-skin care in rural Uttar Pradesh, India. J Perinatol. 2006;26:597–604. doi: 10.1038/sj.jp.7211569. [DOI] [PubMed] [Google Scholar]
- 32.Mullany LC, Katz J, Khatry SK, LeClerq SC, Darmstadt GL, Tielsch JM. Neonatal hypothermia and associated risk factors among newborns of southern Nepal. BMC Medicine. 2010;8:43. doi: 10.1186/1741-7015-8-43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Tielsch JM, Darmstadt GL, Mullany LC, Khatry SK, Katz J, LeClerq SC, Shrestha S, Adhikari R. Impact of newborn skin-cleansing with chlorhexidine on neonatal mortality in southern Nepal: a community-based, cluster-randomized trial. Pediatrics. 2007;119:e330–40. doi: 10.1542/peds.2006-1192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Mullany LC, Darmstadt GL, Khatry SK, Katz J, LeClerq SC, Shrestha S, Adhikari R, Tielsch JM. Topical applications of chlorhexidine to the umbilical cord for prevention of omphalitis and neonatal mortality in southern Nepal: a community-based, cluster-randomised trial. Lancet. 2006;367:910–918. doi: 10.1016/S0140-6736(06)68381-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.da Mota Silveira SM, Goncalves de Mello MJ, de Arruda Vidal S, de Frias PG, Cattaneo A. Hypothermia on admission: a risk factor for death in newborns referred to the Pernambuco Institute of Mother and Child Health. J Trop Pediatr. 2003;49:115–120. doi: 10.1093/tropej/49.2.115. [DOI] [PubMed] [Google Scholar]
- 36.Zayeri F, Kazemnejad A, Ganjali M, Babaei G, Khanafshar N, Nayeri F. Hypothermia in Iranian newborns. Incidence, risk factors and related complications. Saudi Med J. 2005;26:1367–1371. [PubMed] [Google Scholar]
- 37.Ogunlesi TA, Ogunfowora OB, Adekanmbi FA, Fetuga BM, Olanrewaju DM. Point-of-admission hypothermia among high-risk Nigerian newborns. BMC Pediatr. 2008;8:40. doi: 10.1186/1471-2431-8-40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Bergstrom A, Byaruhanga R, Okong P. The impact of newborn bathing on the prevalence of neonatal hypothermia in Uganda: a randomized, controlled trial. Acta Paediatr. 2005;94:1462–1467. doi: 10.1111/j.1651-2227.2005.tb01821.x. [DOI] [PubMed] [Google Scholar]
- 39.Christensson K, Bhat GJ, Amadi BC, Eriksson B, Hojer B. Randomised study of skin-to-skin versus incubator care for rewarming low-risk hypothermic neonates. Lancet. 1998;352:1115. doi: 10.1016/S0140-6736(98)00028-2. [DOI] [PubMed] [Google Scholar]
- 40.Ibe OE, Austin T, Sullivan K, Fabanwo O, Disu E, Costello AM. A comparison of kangaroo mother care and conventional incubator care for thermal regulation of infants < 2000 g in Nigeria using continuous ambulatory temperature monitoring. Ann Trop Paediatr. 2004;24:245–251. doi: 10.1179/027249304225019082. [DOI] [PubMed] [Google Scholar]
- 41.Lawn JE, Mwansa-Kambafwile J, Horta BL, Barros FC, Cousens S. ‘Kangaroo mother care’ to prevent neonatal deaths due to preterm birth complications. Int J Epidemiol. 2010;39(Suppl 1):i144–54. doi: 10.1093/ije/dyq031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Christensson K, Bhat GJ, Eriksson B, Shilalukey-Ngoma MP, Sterky G. The effect of routine hospital care on the health of hypothermic newborn infants in Zambia. J Trop Pediatr. 1995;41:210–214. doi: 10.1093/tropej/41.4.210. [DOI] [PubMed] [Google Scholar]
- 43.Huffman SL, Zehner ER, Victora C. Can improvements in breast-feeding practices reduce neonatal mortality in developing countries? Midwifery. 2001;17:80–92. doi: 10.1054/midw.2001.0253. [DOI] [PubMed] [Google Scholar]
- 44.Mullany LC, Katz J, Li YM, Khatry SK, LeClerq SC, Darmstadt GL, Tielsch JM. Breast-feeding patterns, time to initiation, and mortality risk among newborns in southern Nepal. J Nutr. 2008;138:599–603. doi: 10.1093/jn/138.3.599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Edmond KM, Zandoh C, Quigley MA, Amenga-Etego S, Owusu-Agyei S, Kirkwood BR. Delayed breastfeeding initiation increases risk of neonatal mortality. Pediatrics. 2006;117:e380–6. doi: 10.1542/peds.2005-1496. [DOI] [PubMed] [Google Scholar]
- 46.Friberg IK, Bhutta ZA, Darmstadt GL, Bang A, Cousens S, Baqui AH, Kumar V, Walker N, Lawn JE. Comparing modelled predictions of neonatal mortality impacts using LiST with observed results of community-based intervention trials in South Asia. Int J Epidemiol. 2010;39(Suppl 1):i11–20. doi: 10.1093/ije/dyq017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Baqui AH. Cross Reference this journal issue - Newborn Care Packages Paper. Semin Perinatol. 2010;X:YYY–ZZZ. [Google Scholar]
- 48.Kumar V, Mohanty S, Kumar A, Misra RP, Santosham M, Awasthi S, Baqui AH, Singh P, Singh V, Ahuja RC, Singh JV, Malik GK, Ahmed S, Black RE, Bhandari M, Darmstadt GL, Saksham Study Group Effect of community-based behaviour change management on neonatal mortality in Shivgarh, Uttar Pradesh, India: a cluster-randomised controlled trial. Lancet. 2008;372:1151–1162. doi: 10.1016/S0140-6736(08)61483-X. [DOI] [PubMed] [Google Scholar]
- 49.Zayeri F, Kazemnejad A, Ganjali M, Babaei G, Nayeri F. Incidence and risk factors of neonatal hypothermia at referral hospitals in Tehran, Islamic Republic of Iran. East Mediterr Health J. 2007;13:1308–1318. doi: 10.26719/2007.13.6.1308. [DOI] [PubMed] [Google Scholar]
- 50.Kambarami R, Chidede O. Neonatal hypothermia levels and risk factors for mortality in a tropical country. Cent Afr J Med. 2003;49:103–106. [PubMed] [Google Scholar]
- 51.Cheah FC, Boo NY. Risk factors associated with neonatal hypothermia during cleaning of newborn infants in labour rooms. J Trop Pediatr. 2000;46:46–50. doi: 10.1093/tropej/46.1.46. [DOI] [PubMed] [Google Scholar]
- 52.Manji KP, Kisenge R. Neonatal hypothermia on admission to a special care unit in Dar-es-Salaam, Tanzania: a cause for concern. Cent Afr J Med. 2003;49:23–27. [PubMed] [Google Scholar]