SYNOPSIS
Objectives
We determined the prevalence of first lifetime use of cigarettes during pregnancy or in the early postpartum period (incident smoking) and identified sociodemographic and health-related characteristics of incident smokers.
Methods
We used statistics based on data from a longitudinal study of a large cohort of pregnant, low-income, urban women (n=1,676) to describe the timing of first-time use and to compare incident smokers with those who had never smoked and those who had already smoked prior to pregnancy.
Results
About one in 10 (10.2%) women who had not previously smoked initiated cigarette smoking during pregnancy or in the early postpartum period. Compared with those who had never smoked, incident smokers were more likely to report high levels of stress and to have elevated levels of depressive symptomatology, which may be rooted in relatively poor social and economic conditions.
Conclusion
A significant number of women may be initiating smoking during pregnancy or in the early postpartum period. These women have characteristics that are consistent with the risk factors associated with smoking. Further research is warranted to determine prevalence in other populations, identify the risk factors for incident smoking, and assess the potential for primary prevention efforts designed to help women who had previously avoided cigarette use to remain smoke-free throughout pregnancy and in the postpartum period.
Smoking during pregnancy has been demonstrated to be one of the most significant, as well as preventable, risk factors for poor pregnancy outcomes, including low birthweight and preterm delivery.1–3 Newborns exposed to tobacco smoke from maternal cigarette use are also at increased risk for sudden infant death syndrome, respiratory illness, lung malfunction, ear infections, and even developmental delay.1 The importance of addressing the adverse consequences of maternal tobacco use is reflected in the large and growing body of research focusing on the most effective ways to identify pregnant women who smoke,4–7 the efficacy of interventions designed to help women quit or reduce cigarette consumption during pregnancy,5,8,9 and the prevention of relapse in the postpartum period among women who managed to quit while pregnant.10–14 The societal cost of maternal tobacco consumption and the benefits associated with decreasing the overall exposure of mother, fetus, and infant to tobacco smoke have also been longstanding health policy concerns, ranking high on the list of priorities for public health research and action.15–18
Conspicuously absent from the maternal smoking literature are any published data or serious discussion of the problems associated with incident smoking—the first-time use of tobacco during pregnancy or in the postpartum period. Information is lacking despite the fact that the typical age of onset for smoking among female adolescents and young adults clearly overlaps with the childbearing years.19,20 It also seems reasonable to suggest that some nonsmoking women, especially those with limited resources, may experience additional stressful life events, financial difficulties, and social dislocations that are sometimes associated with pregnancy and parenthood,21,22 and which can be triggers for the initiation or resumption of tobacco use.4,23 Although it appears that some women who smoke and are aware of the risks of exposure are motivated to quit or reduce cigarette consumption when they learn they have become pregnant,14 others may be vulnerable to initiation depending on their circumstances and the stressful changes that pregnancy and caring for a newborn may cause.
We are unaware of any studies documenting the number of women who initiate smoking during pregnancy or in the postpartum period, or the factors that might predispose women to do so. Given the absence of any data addressing this issue, we sought to explore the frequency with which incident smoking occurs among this group and the characteristics of incident smokers, based on a study cohort of low-income, urban childbearing women residing in Philadelphia, Pennsylvania.
METHODS
Overview
This study was part of a larger federally funded, prospective, community-based investigation of the relationship between psychosocial, behavioral, and neighborhood-level factors, and bacterial vaginosis and pregnancy outcomes.24 The larger study initially involved interviews conducted with more than 2,300 pregnant women. Women were recruited for the study at the time of enrollment in prenatal care at any of 10 neighborhood health centers located in underserved areas in Philadelphia from February 1999 to November 2002. More than 97% of the women who were eligible agreed to participate in this larger study. Eligibility criteria included having an intrauterine pregnancy and the ability to speak English.
Beginning in February 2000, the study was expanded to include postpartum follow-up interviews. The expanded study widened the scope of investigation to explore issues related to parenting behavior, health-care utilization, child health and development, as well as postpartum depression and morbidity. Additional findings from and details about the larger study have been published elsewhere.25–28 The study was approved by the Institutional Review Boards of Drexel University, the University of Pennsylvania, and the Philadelphia Department of Public Health.
Study sample
Data for this study were based on those women with both prenatal and postpartum interviews enrolling in prenatal care after February 2000. A total of 1,676 women were successfully interviewed at least once, either at approximately three months (±1 month), 11 months (±1 month), or 24 months (±2 months) following delivery, representing 85% of all those who were eligible and targeted for postpartum follow-up and who delivered a live infant. All interviews included documentation of smoking status, as well as a variety of measures assessing the mother's social and economic conditions, and physical and emotional health, including depressive symptomatology and perceived stress. A wide range of basic, descriptive sociodemographic and obstetrical information was also collected at the time of the prenatal interview.
Measures
The objectives of the analyses were twofold: (1) to document the frequency with which the first-time-ever use of tobacco occurred either during the prenatal or postpartum period and (2) to identify characteristics, markers, or potential risk factors associated with incident smoking, which could be used to target or otherwise inform future primary prevention efforts.
Women were divided into one of three groups based on responses to interviews collected at one or more points in time: (1) “incident” smokers were defined as those who indicated that they had never smoked before pregnancy, but subsequently reported they had started smoking during pregnancy or following delivery; (2) “smoke-free” mothers were defined as women who reported to have never smoked before pregnancy and based on postpartum interviewing, never to have started; and (3) “prepregnancy” smokers were those who indicated that they had initiated cigarette smoking at some point before they became pregnant. These three groups were compared and contrasted on several characteristics.
We first examined basic sociodemographic behavioral characteristics, including median age, household income, marital status, education, race/ethnicity, nativity (foreign- vs. U.S.-born), age at first intercourse, and recent alcohol and marijuana use. We then used levels of perceived stress, based on the Cohen Perceived Stress Scale,29 and depressive symptomatology, based on the Center for Epidemiologic Studies Depression (CES-D) scale,30 as well as self-reported overall emotional and physical health data collected at the time of the prenatal interview to compare the three groups.
Additional variables likely to indicate extreme material deprivation or dislocation were also available from the prenatal surveys and were used to compare the three groups. These variables included participants' reported concern about physical safety while living in their current neighborhood, living in a house that was in physically poor condition, and the experience of having one or more recent utility shutoffs (gas, water, or electric). A woman was classified as having a serious concern about physical safety if she rated her worry about being robbed or murdered in the neighborhood as being relatively high (i.e., ≥8 on a “worry” scale of 1 to 10). A woman was defined as living in a house in poor condition if she reported two or more serious problems with the house she was currently living in, including peeling paint; leaking roof; broken windows; broken or dangerous steps; clogged or overflowing toilets or broken plumbing; or the presence of bugs, mice, or rats.
Women in the three groups were also compared based on their levels of perceived stress, depressive symptomatology, and overall self-reported physical and emotional health in the postpartum period. The Cohen Perceived Stress Scale, CES-D scores, and self-reported physical and emotional health ratings were collected at each of the postpartum interviews and, thus, were available for analyses. Because not all women had all three interviews, we used the results from the most recently completed postpartum interview to assign values to participants on these variables.
Additional variables of interest pertaining to living conditions of the women in the postpartum period were also included in the protocol for the second postpartum interview at nine to 12 months following delivery. For the subsample of these women for whom this second postpartum interview was available (n=1,142), we compared incident, smoke-free, and prepregnancy groups based on whether they indicated they had been homeless or had a utility shutoff since delivery. We also compared the groups based on how worried they were about money, and whether they were living in poor housing conditions or overcrowded households. Living in poor housing conditions in the postpartum period was defined as described previously. A woman was determined to be worried about money if, in the second prenatal interview, she responded that she was very (or extremely) worried about not having enough money from one month to the next. A woman was classified as living in an overcrowded household if she described the conditions in her house or apartment as very cramped with no private space.
Analysis
We used simple cross-tabulations among the three groups and the characteristics described in the previous section to compare and contrast the groups, with the primary focus on the group of women who reported their first lifetime use of cigarettes during this pregnancy or in the early postpartum period (incident smoking). We used Chi-square tests to identify statistically significant differences. To highlight the most salient factors associated with incident smoking, we further explored statistically significant relationships at the univariate level using multivariate analyses. Consistent with the primary focus of the article, the multivariate analysis examined those factors that were most important in terms of distinguishing between women who initiated smoking prenatally or in the early postpartum period and those who remained smoke-free.
We applied stepwise logistic regression using the backward elimination method to arrive at the final, “best” combination of study variables that define incident as opposed to smoke-free respondents. Study variables were removed from the model based on the change in the model log likelihood statistic; a change resulting in Chi-square values with p<0.05 was the criterion for retention. We also calculated adjusted odds ratios associated with each retained variable and their respective 95% confidence intervals. All univariate and multivariate analyses were conducted using SPSS® 15.0 for Windows.31
RESULTS
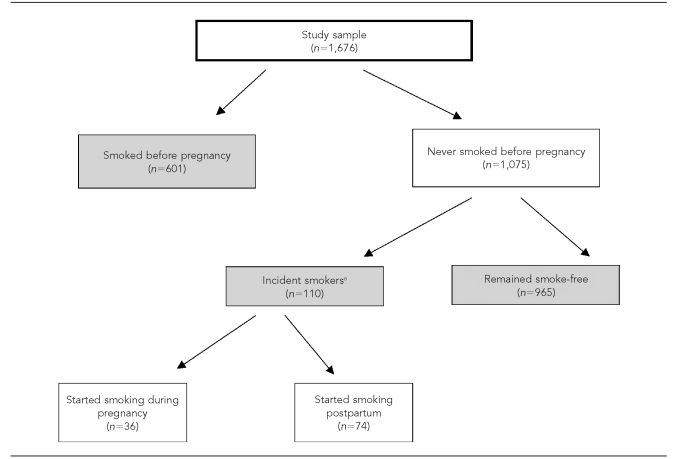
As the Figure shows, 601 women (36%) were prepregnancy smokers, while 1,075 women (64%) reported never having smoked prior to pregnancy. Using data from all of the interviews available, we identified 110 women (10%), among the 1,075 women who had never smoked prior to pregnancy, who initiated smoking during pregnancy or in the postpartum period. Of these incident smokers, 36 women (33%) reported having initiated smoking during pregnancy, while the remaining 74 women (67%) indicated that they had initiated smoking at some point during the postpartum period.
Figure.
Breakdown by smoking status of a study sample of low-income pregnant women, Philadelphia, 1999–2002
aThose who started smoking during pregnancy and those who started smoking postpartum were not significantly different on any of the important variables examined; as a result, and because the subgroup numbers were small, incident smokers were considered a single group in all of the analyses for this study.
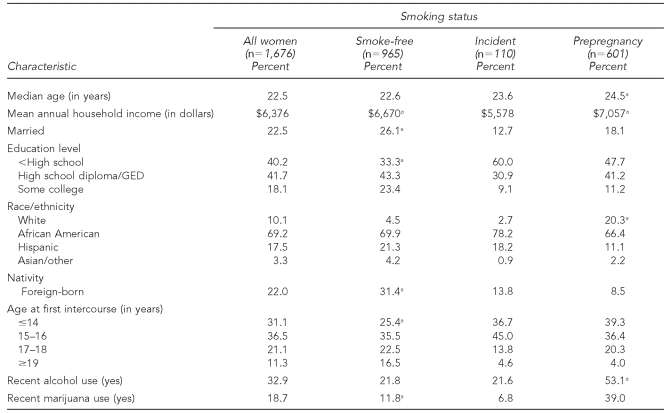
The data in Table 1, based on the prenatal surveys, revealed that incident smokers were more likely to be unmarried, to be less educated, and to have lower mean household incomes than the smoke-free group. Compared with the smoke-free group, incident smokers were also less likely to be foreign-born and more likely to have reported having had sexual intercourse for the first time at 16 years of age or younger. Compared with the prepregnancy smokers, incident smokers had lower mean household incomes, were more likely to be of nonwhite race/ethnicity, and were less likely to have reported recent use of alcohol and marijuana.
Table 1.
Demographic and other characteristics of smoke-free women, incident smokers, and prepregnancy smokers at enrollment for prenatal care in a study of low-income pregnant women, Philadelphia, 1999–2002
aStatistically significant (p≤0.05) differences when compared with incident smokers
GED = general equivalency diploma
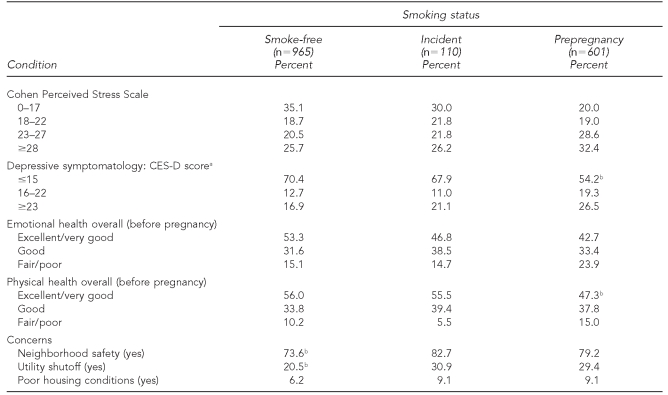
Results from the analyses of additional data collected from the prenatal surveys are presented in Table 2. In general, only small and statistically nonsignificant differences among the groups were found with respect to perceived stress and overall emotional health measured prior to pregnancy. However, self-reported overall physical health was reported to be generally better for incident smokers compared with prepregnancy smokers. Compared with the smoke-free group, incident smokers were more likely to report serious concerns about the safety of their neighborhood (82.7% vs. 73.6%) and to have experienced a recent utility shutoff (30.9% vs. 20.5%).
Table 2.
Health-related and material conditions of smoke-free women, incident smokers, and prepregnancy smokers at enrollment for prenatal care (n=1,676) in a study of low-income pregnant women, Philadelphia, 1999–2002
aRespondents with CES-D scores ≥23 are generally classified as “probably depressed,” those with scores of 16–22 are classified as “possibly depressed,” and those with scores ≤15 are classified as “not depressed.”
bStatistically significant (p≤0.05) differences when compared with incident smokers
CES-D = Center for Epidemiologic Studies Depression
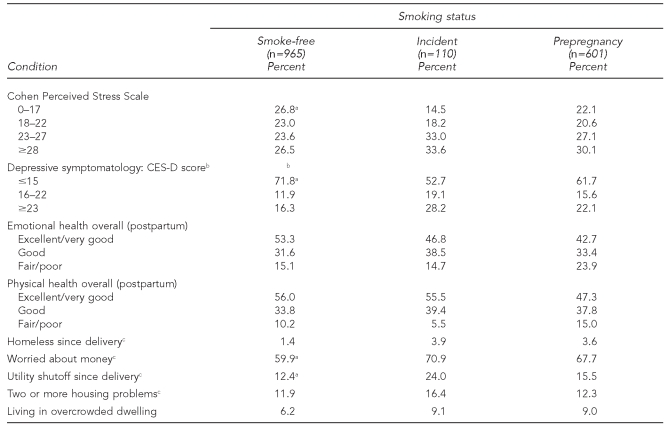
The results from the postpartum interview responses are presented in Table 3. They indicate that differences between the incident smokers and the smoke-free group related to perceived stress and depressive symptomatology, as measured during the postpartum period, were more pronounced, with incident smokers reporting significantly more perceived stress and higher levels of depressive symptomatology than the smoke-free group. Specifically, only 14.5% of incident smokers were in the lowest quartile of the Cohen Perceived Stress Scale compared with 26.8% of smoke-free mothers, while 33.6% of incident smokers were in the highest quartile compared with 26.5% of smoke-free mothers. Consistent with this pattern, only 52.7% of the incident smokers, compared with 71.8% of the smoke-free mothers, had CES-D scores of ≤15, while 28.2% of incident smokers vs. only 16.3% of smoke-free mothers had CES-D scores of ≥23. Although the incident smokers were slightly less likely than the smoke-free group to report their overall emotional health as excellent or very good (as opposed to fair or poor), these two groups did not differ markedly or statistically significantly in this respect. However, both incident and prepregnancy smokers had more perceived stress and depressive symptomatology when compared with the smoke-free group.
Table 3.
Health-related and material conditions of smoke-free women, incident smokers, and prepregnancy smokers during the postpartum period (latest interview) (n=1,676) in a study of low-income pregnant women, Philadelphia, 1999–2002
aStatistically significant (p≤0.05) differences when compared with incident smokers
bRespondents with CES-D scores ≥23 are generally classified as “probably depressed,” those with scores of 16–22 are classified as “possibly depressed,” and those with scores ≤15 are classified as “not depressed.”
cItem was available only from the interview at nine to 12 months (n=1,142) and, thus, the denominators are n=651 for the smoke-free, n=76 for the incident, and n=415 for the prepregnancy groups.
CES-D = Center for Epidemiologic Studies Depression
Additional findings based on the analyses of responses available only from the second postpartum interview, which was conducted at nine to 12 months postpartum, are also presented in Table 3. The findings are consistent with the overall pattern of increased hardship and the occurrence of stressful life events for incident smokers compared with the smoke-free group. Specifically, incident smokers were more likely to have experienced a utility shutoff since delivery (24% of incident smokers vs. 12% of smoke-free mothers) and more likely to have reported being worried about money (71% of incident smokers vs. 60% of smoke-free mothers). They were also more likely to indicate that they had become homeless at some point since childbirth, to have two or more serious housing problems, and to report living in an overcrowded household; however, these differences were not statistically significant.
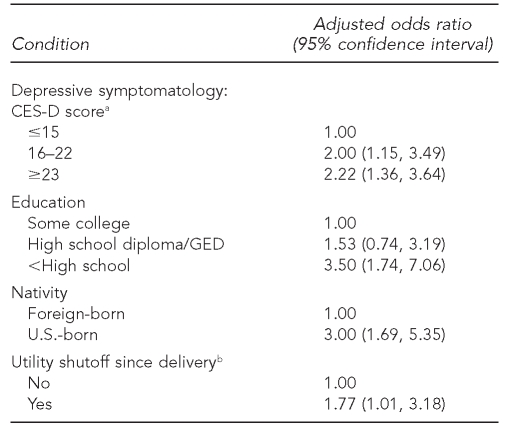
The results of the multivariate analyses are presented in Table 4. Of the variables previously shown to have significantly different distributions between the incident smokers and the smoke-free group, depressive symptomatology, education, nativity, and having had a utility shutoff were independently associated with incident smoking. Specifically, among the women who had never smoked prior to becoming pregnant, those with the highest levels of depressive symptomatology were more than 2.2 times as likely as those with the lowest levels of depressive symptomatology to begin smoking, either prenatally or in the early postpartum period. Compared with women who had the highest levels of education, those with the least amount of education were 3.5 times as likely to initiate smoking during this period. In addition, U.S.-born women, as compared with foreign-born women, and women who had experienced a utility shutoff were 3.0 times and 1.8 times as likely, respectively, to initiate smoking while pregnant or during the postpartum period in which they were interviewed for this study.
Table 4.
Results of logistic regression analyses for selected characteristics and conditions of incident smokers vs. smoke-free women in a study of low-income pregnant women, Philadelphia, 1999–2002
aRespondents with CES-D scores ≥23 are generally classified as “probably depressed,” those with scores of 16–22 are classified as “possibly depressed,” and those with scores ≤15 are classified as “not depressed.”
bOdds ratios and 95% confidence intervals reflect values for the final model using the stepwise logistic regression/backward elimination method.
CES-D = Center for Epidemiologic Studies Depression
GED = general equivalency diploma
DISCUSSION
In our study of a large cohort of low-income, urban women, we found that slightly more than 10% of those who had never smoked prior to pregnancy initiated the use of tobacco during pregnancy or in the postpartum period. Consistent with other investigations of adult smoking behavior,1,15 incident smoking in our study sample was inversely related to socioeconomic status and positively associated with indicators of material deprivation, stressful life events (e.g., homelessness, housing disrepair, and utility shutoffs), depressive symptomatology, and higher perceived levels of stress. Compared with smoke-free women, incident smokers tended to become sexually active at a younger age and to have recently smoked marijuana; both findings are consistent with studies of the risk factors or markers of the initiation of tobacco use by adolescents and young adults.20,32
The findings are more meaningfully interpreted within the context of the existing body of literature pertaining to smoking during pregnancy and the postpartum period. Recent data indicate that about 40% of pregnant smokers quit during pregnancy, either spontaneously or as the result of cessation interventions.4,6 Randomized controlled trials have shown that, in addition to those who quit with no assistance, 10% to 20% of pregnant women will quit if obstetrical providers adopt systematic protocols to identify, counsel, and otherwise assist women in efforts to quit or reduce cigarette consumption.4 The American College of Obstetricians and Gynecologists has formally endorsed and encouraged obstetrical providers to implement the U.S. Public Health Service (PHS) recommendations to “institutionalize the consistent identification, documentation, and treatment of every tobacco user seen in a health care setting.”33 The importance of implementing these guidelines for improving pregnancy outcomes is underscored by the fact that the typical pregnant woman has numerous contacts with obstetrical providers during the normal course of prenatal care.4
In contrast to the documented benefits associated with the repeated, structured, but brief interventions that providers can offer at every prenatal visit, studies of cessation interventions involving more intensive group or one-on-one counseling have shown that participation rates are low and that such interventions have very limited potential to reduce aggregate levels of maternal and fetal exposure to tobacco smoke.4 Thus, the PHS recommendations and the justification for implementing them rest in large part on the notion of “teachable moments”—the repeated, numerous opportunities that prenatal care providers have to deliver practical advice and assistance to women, opportunities that are by-products of the frequent maternal visits typically involved with the prenatal care regimen.34
With respect to maternal smoking in the postpartum period, there has been considerable discussion about the role that pediatric providers can play, given that exposure to tobacco smoke introduces serious risks to both mother and child. Of the approximately 40% of women who manage to quit smoking during pregnancy, an estimated 80% will resume cigarette use within the child's first year of life, and most of those who relapse do so within the first six months after delivery.6,23 Studies comparing those who relapse with those who remain abstinent are consistent with the findings presented in this article—that is, relapse is associated with lower socioeconomic status, African American race/ethnicity, diminished self-efficacy, and more stressful life events.12,14 Observers have noted that maternal tobacco use is not as systematically addressed in pediatric vs. prenatal care settings.35 This is unfortunate in light of the known risks of exposure to both mother and infant, extremely high relapse rates, and the fact that new mothers typically have numerous contacts with pediatric providers in the form of both well- and sick-child visits.
Findings from the relatively few studies of interventions designed to reduce relapse rates and, thus, exposure of children to maternal tobacco use are generally disappointing, demonstrating little or no differences between treatment and control groups.13,36 Again, repeated, brief, but structured interventions by pediatric providers, consistently delivered over time, may hold the most promise for reducing relapse and maternal smoking rates.37 Although further studies are clearly warranted, the American Academy of Pediatrics, through its policy statements and published guidelines,38 has acknowledged that pediatric settings represent appropriate places to address maternal tobacco use, and it strongly encourages practitioners to incorporate systematic cessation interventions with parents, similar to those articulated and recommended by the PHS for all adult smokers.34,39 The emphasis is again on the numerous opportunities that occur, as a result of mothers' frequent appearances in pediatric settings, for pediatric providers to offer maternal interventions to prevent relapses. Nationwide, infants are seen in ambulatory, pediatric care settings an average of seven times during the first year of life40 and are most often accompanied by their mothers. Although the data are not presented in this article in detail, the women in our study cohort made an average of eight visits to pediatric providers during the baby's first year of life.
There is virtually no mention of women who may initiate smoking during pregnancy or in the postpartum period in the literature. This is somewhat surprising in that many pregnant/postpartum women are adolescents or young adults, reaching age milestones associated with the initiation of smoking. It is also widely recognized that for some women, pregnancy and parenting can cause social, emotional, and economic stress and disruption, which are known triggers for the resumption, as well as the initiation, of tobacco use.1,6 Multiple contacts with medical providers during pregnancy and postpartum could, therefore, be viewed as opportunities for primary prevention (i.e., teachable moments) pertaining not only to the goals of smoking cessation during pregnancy and relapse prevention, but also to the goal of encouraging and supporting those who have never smoked to remain smoke-free.
Successfully getting women to quit or substantially reduce cigarette consumption during pregnancy, and then to avoid relapse following delivery, has proved to be a challenging task for medical providers. Behavioral habituation and/or chemical dependency are recognized as important barriers.15 Yet, by definition, these barriers are not present in the case of women who have never smoked, but who may be susceptible to doing so, precisely during a time when it is critical that they remain smoke-free. The underlying motivation for lifetime nonsmokers to remain smoke-free during pregnancy is arguably as salient as that for prepregnancy smokers to reduce or quit smoking—i.e., to avoid poor pregnancy outcomes. In the same vein, the motivation for nonsmokers to remain smoke-free in the postpartum period may be as strong as that for “quitters” to avoid relapse —i.e., the protection of the infant from the adverse health effects of environmental exposure to tobacco smoke. Thus, some optimism may be warranted for successful primary prevention targeting nonsmokers who may be susceptible to initiating smoking during pregnancy or following delivery.
Limitations
Some limitations were associated with this study, which should be regarded as a first step that will hopefully lead to further research in this area. We used existing data from a study designed specifically to examine smoking behaviors, and the sample was deliberately confined to pregnant women who enrolled for prenatal care at community health centers located in underserved areas and serving almost exclusively low-income women. The comparisons we made to help identify those most at risk for first-time use may not necessarily be the most informative, nor are they likely to provide the most comprehensive profile of these women.
Our measures of incident smoking were based on self-reported smoking status, which is widely regarded to underestimate smoking rates for pregnant women. A previous analysis of data from a subsample of the women included in this study confirmed a bias in reporting consistent with other studies.41 We cross-checked self-reported smoking status with laboratory results based on urine dipstick testing for cotinine levels for 175 women in the study sample who said that they were not smokers during pregnancy. Of those, 32 (18.3%) had cotinine levels equal to or higher than those indicating exposure from active smoking. Consequently, the rates reported in this study may represent minimum estimates, and, if anything, may somewhat underestimate the problems associated with incident smoking. Moreover, the results may not be generalized to other populations, particularly those women in non-urban areas or in higher socioeconomic groups.
Because our research was a descriptive study, we were unable to make causal statements. We could not fully explore the extent to which emotional difficulties, material hardships, and stressful life events that were more characteristic of the incident smokers, compared with the smoke-free women, were directly tied to pregnancy and the demands of parenting—as opposed to preexisting conditions that predisposed some pregnant and postpartum women to initiate smoking.
CONCLUSIONS
The important questions highlighted by the results from this study are the extent to which incident smoking occurs in other populations, and the extent to which it may be preventable and by what means. Further research in this area is warranted, especially given the possibility that primary preventive intervention to successfully reduce the number of incident smokers may involve a simple extension of existing guidelines, including a protocol that identifies pregnant and postpartum women most at risk for initiating tobacco use and that encourages and assists such women in their efforts to maintain their smoke-free status.
Footnotes
This work was supported by the National Institutes of Health and Human Development (R01HD36462-01 A1) and the Centers for Disease Control and Prevention/Association of Teachers of Preventive Medicine (TS-0626 and TS-0561).
REFERENCES
- 1.Cnattingius S. The epidemiology of smoking during pregnancy: smoking prevalence, maternal characteristics, and pregnancy outcomes. Nicotine Tob Res. 2004;6(Suppl 2):S125–40. doi: 10.1080/14622200410001669187. [DOI] [PubMed] [Google Scholar]
- 2.Hammoud AO, Bujold E, Sorokin Y, Schild C, Krapp M, Baumann P. Smoking in pregnancy revisited: findings from a large population-based study. Am J Obstet Gynecol. 2005;192:1856–62. doi: 10.1016/j.ajog.2004.12.057. [DOI] [PubMed] [Google Scholar]
- 3.Shea AK, Steiner M. Cigarette smoking during pregnancy. Nicotine Tob Res. 2008;10:267–78. doi: 10.1080/14622200701825908. [DOI] [PubMed] [Google Scholar]
- 4.Crawford JT, Tolosa JE, Goldenberg RL. Smoking cessation in pregnancy: why, how, and what next? Clin Obstet Gynecol. 2008;51:419–35. doi: 10.1097/GRF.0b013e31816fe9e9. [DOI] [PubMed] [Google Scholar]
- 5.Ershoff D, Ashford TH, Goldenberg R. Helping pregnant women quit smoking: an overview. Nicotine Tob Res. 2004;6(Suppl 2):S101–5. doi: 10.1080/14622200410001669204. [DOI] [PubMed] [Google Scholar]
- 6.Giglia RC, Binns CW, Alfonso HS, Zhao Y. Which mothers smoke before, during and after pregnancy? Public Health. 2007;121:942–9. doi: 10.1016/j.puhe.2007.04.007. [DOI] [PubMed] [Google Scholar]
- 7.Melvin CL, Dolan-Mullen P, Windsor RA, Whiteside HP, Goldenberg RL. Recommended cessation counselling for pregnant women who smoke: a review of the evidence. Tob Control. 2000;9(Suppl 3):iii80–4. doi: 10.1136/tc.9.suppl_3.iii80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Chapin J, Root W American College of Obstetricians and Gynecologists. Improving obstetrician-gynecologist implementation of smoking cessation guidelines for pregnant women: an interim report of the American College of Obstetricians and Gynecologists. Nicotine Tob Res. 2004;6(Suppl 2):S253–7. doi: 10.1080/14622200410001669123. [DOI] [PubMed] [Google Scholar]
- 9.Donatelle R, Hudson D, Dobie S, Goodall A, Hunsberger M, Oswald K. Incentives in smoking cessation: status of the field and implications for research and practice with pregnant smokers. Nicotine Tob Res. 2004;6(Suppl 2):S163–79. doi: 10.1080/14622200410001669196. [DOI] [PubMed] [Google Scholar]
- 10.Bottorff JL, Kalaw C, Johnson JL, Stewart M, Greaves L, Carey J. Couple dynamics during women's tobacco reduction in pregnancy and postpartum. Nicotine Tob Res. 2006;8:499–509. doi: 10.1080/14622200600789551. [DOI] [PubMed] [Google Scholar]
- 11.French GM, Groner JA, Wewers ME, Ahijevych K. Staying smoke free: an intervention to prevent postpartum relapse. Nicotine Tob Res. 2007;9:663–70. doi: 10.1080/14622200701365277. [DOI] [PubMed] [Google Scholar]
- 12.Hymowitz N, Schwab M, McNerney C, Schwab J, Eckholdt H, Haddock K. Postpartum relapse to cigarette smoking in inner city women. J Natl Med Assoc. 2003;95:461–74. [PMC free article] [PubMed] [Google Scholar]
- 13.Letourneau AR, Sonja B, Mazure CM, O'Malley SS, James D, Colson ER. Timing and predictors of postpartum return to smoking in a group of inner-city women: an exploratory pilot study. Birth. 2007;34:245–52. doi: 10.1111/j.1523-536X.2007.00177.x. [DOI] [PubMed] [Google Scholar]
- 14.Solomon L, Quinn V. Spontaneous quitting: self-initiated smoking cessation in early pregnancy. Nicotine Tob Res. 2004;6(Suppl 2):S203–16. doi: 10.1080/14622200410001669132. [DOI] [PubMed] [Google Scholar]
- 15.Fagerstrom K. The epidemiology of smoking: health consequences and benefits of cessation. Drugs. 2002;6(Suppl 2):1–9. doi: 10.2165/00003495-200262002-00001. [DOI] [PubMed] [Google Scholar]
- 16.Halpern-Felsher BL, Orrell-Valente JK. Reducing and preventing tobacco use among pregnant women, parents, and families. In: Bonnie RJ, Stratton K, Wallace RB, editors. Ending the tobacco problem: a blueprint for the nation. Washington: National Academies Press; 2007. pp. 503–15. [Google Scholar]
- 17.Haviland L, Thornton AH, Carothers S, Hund L, Allen JA, Kastens B, et al. Giving infants a great start: launching a national smoking cessation program for pregnant women. Nicotine Tob Res. 2004;6(Suppl 2):S181–8. doi: 10.1080/14622200410001669114. [DOI] [PubMed] [Google Scholar]
- 18.Department of Health and Human Services (US). Healthy people 2010. 2nd ed. Washington: U.S. Government Printing Office; 2000. [Google Scholar]
- 19.Castrucci BC, Culhane JF, Chung EK, Bennett I, McCollum KF. Smoking in pregnancy: patient and provider risk reduction behavior. J Public Health Manag Pract. 2006;12:68–76. doi: 10.1097/00124784-200601000-00013. [DOI] [PubMed] [Google Scholar]
- 20.Lenney W, Enderby B. “Blowing in the wind”: a review of teenage smoking. Arch Dis Child. 2008;93:72–5. doi: 10.1136/adc.2006.109702. [DOI] [PubMed] [Google Scholar]
- 21.Hobel C, Culhane J. Role of psychosocial and nutritional stress on poor pregnancy outcome. J Nutr. 2003;133(5 Suppl 2):S1709–17. doi: 10.1093/jn/133.5.1709S. [DOI] [PubMed] [Google Scholar]
- 22.Webb DA, Culhane J, Metraux S, Robbins JM, Culhane D. Prevalence of episodic homelessness among adult childbearing women in Philadelphia, PA. Am J Public Health. 2003;93:1895–6. doi: 10.2105/ajph.93.11.1895. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Solomon LJ, Higgins ST, Heil SH, Badger GJ, Thomas CS, Bernstein IM. Predictors of postpartum relapse to smoking. Drug Alcohol Depend. 2007;90:224–7. doi: 10.1016/j.drugalcdep.2007.03.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Culhane JF, Rauh V, McCollum KF, Elo IT, Hogan V. Exposure to chronic stress and ethnic differences in rates of bacterial vaginosis among pregnant women. Am J Obstet Gynecol. 2002;187:1272–6. doi: 10.1067/mob.2002.127311. [DOI] [PubMed] [Google Scholar]
- 25.Bennett IM, Culhane JF, McCollum KF, Elo IT. Unintended rapid repeat pregnancy and low education status: any role for depression and contraceptive use? Am J Obstet Gynecol. 2006;194:749–54. doi: 10.1016/j.ajog.2005.10.193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Chung EK, McCollum KF, Elo IT, Culhane JF. Does prenatal care at community-based health centers result in infant primary care at these sites? Ambul Pediatr. 2006;6:25–31. doi: 10.1016/j.ambp.2005.08.002. [DOI] [PubMed] [Google Scholar]
- 27.Chung EK, McCollum KF, Elo IT, Lee HJ, Culhane JF. Maternal depressive symptoms and infant health practices among low-income women. Pediatrics. 2004;113:e523–9. doi: 10.1542/peds.113.6.e523. [DOI] [PubMed] [Google Scholar]
- 28.Webb DA, Bloch JR, Coyne JC, Chung EK, Bennett IM, Culhane JF. Postpartum physical symptoms in new mothers: their relationship to functional limitations and emotional well-being. Birth. 2008;35:179–87. doi: 10.1111/j.1523-536X.2008.00238.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Cohen S, Kamarack T, Mermelstein R. A global measurement of perceived stress. J Health Soc Behav. 1983;24:385–96. [PubMed] [Google Scholar]
- 30.Okun A, Stein RE, Bauman LJ, Silver EJ. Content validity of the Psychiatric Symptom Index, CES-Depression Scale, and State-Trait Anxiety Inventory from the perspective of DSM-IV. Psychol Rep. 1996;79(3 Pt 1):1059–69. doi: 10.2466/pr0.1996.79.3.1059. [DOI] [PubMed] [Google Scholar]
- 31.SPSS Inc. SPSS®: Version 15.0 for Windows. Chicago: SPSS Inc.; 2009. [Google Scholar]
- 32.Kreslake JM, Wayne GF, Alpert HR, Koh HK, Connolly GN. Tobacco industry control of menthol in cigarettes and targeting of adolescents and young adults. Am J Public Health. 2008;98:1685–92. doi: 10.2105/AJPH.2007.125542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Fiore MC, Bailey WC, Cohen SJ, Dorfman SF, Goldstein MG, Gritz ER, et al. Clinical practice guideline: treating tobacco use and dependence. Rockville (MD): Department of Health and Human Services, Public Health Service (US); 2000. [Google Scholar]
- 34.Fiore MC, Jaen CR, Baker TB, Bailey WC, Benowitz NL, Curry SJ, et al. Clinical practice guideline: treating tobacco use and dependence: 2008 update. Rockville (MD): Department of Health and Human Services, Public Health Service (US); 2008. [Google Scholar]
- 35.Stein RJ, Haddock CK, O'Byrne KK, Hymowitz N, Schwab J. The pediatrician's role in reducing tobacco exposure in children. Pediatrics. 2000;106:e66. doi: 10.1542/peds.106.5.e66. [DOI] [PubMed] [Google Scholar]
- 36.Pbert L, Ockene JK, Zapka J, Ma Y, Goins KV, Oncken C, et al. A community health center smoking-cessation intervention for pregnant and postpartum women. Am J Prev Med. 2004;26:377–85. doi: 10.1016/j.amepre.2004.02.010. [DOI] [PubMed] [Google Scholar]
- 37.Wall MA, Severson HH, Andrews JA, Lichtenstein E, Zoref L. Pediatric office-based smoking intervention: impact on maternal smoking and relapse. Pediatrics. 1995;96(4 Pt 1):622–8. [PubMed] [Google Scholar]
- 38.Winickoff JP, Berkowitz AB, Brooks K, Tanski SE, Geller A, Thomson C, et al. State-of-the-art interventions for office-based parental tobacco control. Pediatrics. 2005;115:750–60. doi: 10.1542/peds.2004-1055. [DOI] [PubMed] [Google Scholar]
- 39.Winickoff JP, Tanski SE, McMillen RC, Hipple BJ, Friebely J, Healey EA. A national survey of the acceptability of quitlines to help parents quit smoking. Pediatrics. 2006;117:e695–700. doi: 10.1542/peds.2005-1946. [DOI] [PubMed] [Google Scholar]
- 40.Hagan JF Jr, Shaw JS, Duncan P, editors. Bright futures: guidelines for health supervision of infants, children and adolescents. 3rd ed. Elk Grove Village (IL): American Academy of Pediatrics; 2008. [Google Scholar]
- 41.Russell T, Crawford M, Woodby L. Measurements for active cigarette smoke exposure in prevalence and cessation studies: why simply asking pregnant women isn't enough. Nicotine Tob Res. 2004;6(Suppl 2):S141–51. doi: 10.1080/14622200410001669141. [DOI] [PubMed] [Google Scholar]