Abstract
Objectives
Most Burkholderia pseudomallei strains are intrinsically resistant to macrolides, mainly due to AmrAB-OprA- and/or BpeAB-OprB-mediated efflux. We assessed the in vitro anti-B. pseudomallei efficacy of cethromycin, a novel ketolide with broad-spectrum activity against Gram-negative and Gram-positive pathogens.
Methods
The 2-fold broth microdilution technique was used to assess the in vitro cethromycin susceptibility of a prototype strain, efflux mutants, and a panel of 60 clinical and environmental strains. Time–kill curves were used to assess the mode of action. Spontaneous resistant mutants were isolated and AmrAB-OprA efflux pump expression assessed by quantitative real-time PCR. Deletion and complementation analyses were performed to demonstrate AmrAB-OprA efflux pump mutant involvement in high-level cethromycin resistance.
Results
In contrast to macrolides, cethromycin was a weak substrate of AmrAB-OprA and BpeAB-OprB. Cethromycin was bactericidal at high concentrations and bacteriostatic at MIC levels. The ketolide showed efficacy against clinical and environmental strains of B. pseudomallei, with MIC values ranging from 4 to 64 mg/L. Environmental isolates were consistently more susceptible than clinical isolates. High-level cethromycin resistance (MIC 128 mg/L) was due to constitutive AmrAB-OprA efflux pump overexpression, but other mechanisms also seem to contribute.
Conclusions
In contrast to macrolides, which are readily effluxed, cethromycin is weakly extruded in wild-type strains and thus demonstrates significant in vitro anti-B. pseudomallei activity against diverse strains. Acquired high-level cethromycin resistance is caused by constitutive AmrAB-OprA efflux pump overexpression and other, probably non-efflux, mechanisms may also contribute to lower-level acquired resistance.
Keywords: melioidosis, therapy, ketolides, efflux
Introduction
Burkholderia pseudomallei is the aetiological agent of melioidosis, a rare but serious disease endemic to Southeast Asia and northern Australia, and other parts of the tropics around the world.1–3 Treatment of melioidosis is challenging and complicated by the bacterium's intrinsic antibiotic resistance.4 Currently, recommended treatment for acute human melioidosis is intravenous ceftazidime or a carbapenem for ≥10–14 days, followed by oral eradication therapy consisting of trimethoprim/sulfamethoxazole with or without doxycycline for 12–20 weeks. Depending on patient circumstances (e.g. childhood or pregnancy) or drug tolerance, oral eradication therapy may consist of amoxicillin/clavulanic acid.5 Because of biodefence implications, B. pseudomallei is listed as a select agent by US federal authorities.6 To counter a possible compromise of melioidosis therapy by naturally occurring or maliciously engineered resistant strains, efforts are underway to understand this bacterium's drug resistance mechanisms and to test novel therapeutic agents. Preliminary data by Advanced Life Sciences, Inc. indicated that cethromycin has potent, broad-spectrum activity against the biodefence pathogens Francisella tularensis, Yersinia pestis and Bacillus anthracis. Here, we assessed the in vitro activity of cethromycin against B. pseudomallei as well as its mechanism of resistance.
Materials and methods
Bacterial strains, media and growth conditions
Escherichia coli DH5α was used for routine cloning experiments.7 B. pseudomallei strains used in this study are listed in Table 1, except for the panel of 30 clinical and 30 environmental isolates for which details are available from the authors. Bacteria were routinely grown at 37°C in Luria broth, Lennox formula (LB) or on LB agar purchased from MO BIO Laboratories (Carlsbad, CA, USA). Antibiotics were added at the following concentrations: 100 mg/L ampicillin, 15 mg/L gentamicin, 35 mg/L kanamycin and 25 mg/L zeocin for E. coli; and 1000 mg/L kanamycin and 2000 mg/L zeocin for wild-type B. pseudomallei. For Δ(amrRAB-oprA) B. pseudomallei efflux pump mutants, gentamicin, kanamycin and zeocin were used at 15, 50 and 100 mg/L, respectively. Commercially available antibiotics were purchased from the following manufacturers: carbenicillin (Duchefa Biochemie via Gold Biotechnology, St Louis, MO, USA); ciprofloxacin (LKT Laboratories, St Paul, MN, USA); gentamicin (EMD Biosciences, San Diego, CA, USA); spectinomycin (Miomol Research Laboratories via VWR International, West Chester, PA, USA); zeocin (Invitrogen, Carlsbad, CA, USA); and all others (Sigma, St Louis, MO, USA). Cethromycin was provided by Advanced Life Sciences, Inc. (Woodridge, IL, USA).
Table 1.
Burkholderia pseudomallei strains used in this study
| Strain or plasmid | Relevant genotype or properties | Reference or source |
|---|---|---|
| 1026b | wild-type strain; clinical isolate | 21 |
| Bp50 | 1026b with Δ(amrRAB-oprA)::FRTa | 13 |
| Bp58 | Bp50 with ΔbpeR::FRTb | 10 |
| Bp207 | Bp50 with Δ(bpeAB-oprB)::FRT | 10 |
| Bp216 | Bp207::mini-Tn7Tc | 10 |
| Bp217 | Bp207::mini-Tn7T-bpeT+d | this study |
| Bp246 | Bp207::mini-Tn7T-amrA+B+-oprA+e | this study |
| Bp289 | cethromycin-resistant derivative of 1026b | this study |
| Bp290 | cethromycin-resistant derivative of 1026b | this study |
| Bp328 | Bp289 with Δ(amrRAB-oprA) | this study |
| Bp340 | 1026b with Δ(amrRAB-oprA) | this study |
| Bp383 | Bp328::mini-Tn7T | this study |
| Bp384 | Bp328::mini-Tn7T-amrA+B+-oprA+ | this study |
aamrR encodes a repressor of amrAB-oprA.
bbpeR encodes a repressor of bpeAB-oprB; repressor-deficient strains overexpress BpeAB-OprB.
cAll chromosomal mini-Tn7 insertions used in this study are located at the glmS2-associated attachment site.
dbpeT encodes an activator of bpeEF-oprC. This strain overexpresses BpeT, which in turn leads to overexpression of BpeEF-OprC.
eamrA+B+-oprA+ expression is driven from its own promoter.
DNA methods
Published procedures were employed for manipulation of DNA and transformation of E. coli.8 DNA fragments were purified from agarose gels using the Fermentas DNA Extraction Kit (Glen Burnie, MD, USA). Custom oligonucleotides were synthesized by Integrated DNA Technologies (Coralville, IA, USA). Quantitative real-time PCR (qRT–PCR) was performed using the methods and primer sets described by Kumar et al.,9 with minor modifications. Briefly, cells were grown at 37°C in LB medium to mid-log phase (optical density at 600 nm, ∼0.7). Total RNA was extracted from 1 mL of culture using the RNeasy Mini kit from QIAGEN (Valencia, CA, USA). Then, 1 µg of RNA was treated with RNase-free DNase I from Fermentas and cDNA was synthesized using the Invitrogen SuperScript III First-Strand Synthesis SuperMix for qRT–PCR. qRT–PCR was performed with an iQ5 real-time PCR detection system (Bio-Rad, Hercules, CA, USA), using Invitrogen's SYBR GreenER qPCR SuperMix for iCycler. Primers were designed using the OligoPerfect primer-designing tool from Invitrogen. The primers used were amrB_RT_Rev (5′-GTCAGCACGTTGATCGAGAA-3′) and amrB_RT_For (5′-CGCTGTGATGTTCCTCTTCA-3′) for amrB, and Bp23S-F (5′-GTAGACCCGAAACCAGGTGA-3′) and Bp23S-R (5′-CACCCCTATCCACAGCTCAT-3′) for the 23S rRNA housekeeping control. Melt-curve analysis was performed on all reactions to rule out secondary products and primer–dimer formation. Standard curves were constructed using a series of DNA concentrations of extracted chromosomal DNA from a B. pseudomallei 1026b culture. A 944 bp DNA fragment containing the amrR gene and the amrR-amrA intergenic region was PCR amplified using primers 1599 (5′-CGCGCGCAATTGTTCCTC-3′) and 1602 (5′-CGCGTGCGTGCCCATTCG-3′), and its sequence was determined using the same primers.
Mutant construction and complementation
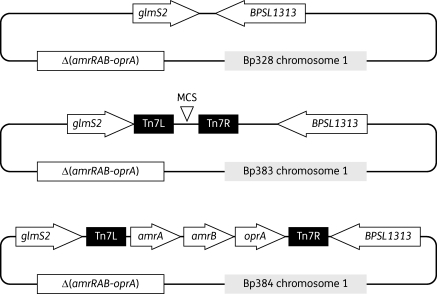
Plasmid pPS2557 was used for the construction of Δ(amrRAB-oprA) mutants containing the same amrRAB-oprA deletion as Bp50 but without the FRT scar.10 The Δ(amrRAB-oprA) allele contained on this plasmid was transferred to the Bp289 chromosome 1, using a previously described method.11 This resulted in strain Bp328 (Figure 1). For single-copy complementation of the Δ(amrRAB-oprA) mutation in Bp328, strain Bp384, containing a chromosomally integrated mini-Tn7 element expressing the amrAB-oprA operon from 1026b, was constructed using the delivery plasmid pPS2470 and previously published procedures.12,13 Plasmid pUC18T-mini-Tn7T-Km-FRT was used for the construction of control strain Bp383, containing the empty mini-Tn7T vector integrated at the same chromosomal site.13
Figure 1.
Single-copy complementation of efflux mutant strains. The mini-Tn7 system was used for single-copy complementation. The empty mini-Tn7 element or the mini-Tn7 element expressing the amrAB-oprA operon from its own promoter was integrated into the Δ(amrRAB-oprA) strain Bp328 genome to yield strains Bp383 and Bp384, respectively. PCR analysis revealed that both strains had the respective mini-Tn7 elements integrated at the glmS2-associated integration site on chromosome 1.
Isolation of cethromycin-resistant mutants
Strain 1026b was grown in 2 mL of LB medium overnight at 37°C with shaking to full saturation. A 100 µL aliquot of this culture was transferred into 2 mL of LB broth + 16 mg/L cethromycin (∼4× the MIC). This culture was incubated at 37°C until fully turbid, which took ∼5 days. A 100 µL aliquot of the culture was then transferred into 2 mL of LB broth + 32 mg/L cethromycin and incubated at 37°C. After 27 h incubation, the culture was fully grown, suggesting that the mutant(s) growing in the LB + 16 mg/L cethromycin culture were already resistant to the higher cethromycin concentration. Two resistant mutants were isolated from the LB + 32 mg/L cethromycin culture by streaking for single colonies on LB + 32 mg/L cethromycin plates. The two mutants were named Bp289 and Bp290. In an attempt to isolate mutants that became cethromycin resistant independent of AmrAB-OprA expression, 1 mL of an overnight culture of Δ(amrRAB-oprA) mutant Bp340 was plated on LB agar containing 4 mg/L (2× MIC) cethromycin. Colonies growing on this plate were purified on LB agar with 4 mg/L cethromycin.
Antimicrobial susceptibility testing
MICs were determined in Mueller–Hinton broth (Becton Dickinson, Franklin Lakes, NJ, USA) by the 2-fold broth microdilution technique following Clinical and Laboratory Standards Institute guidelines.14 The MICs were recorded after incubation at 37°C for 24 h. For cethromycin time–kill curves, flasks containing LB medium with varied amounts of cethromycin were inoculated with ∼106 cfu/mL 1026b. The cultures were shaken at 37°C, aliquots removed at the indicated timepoints and 10-fold serial dilutions in LB medium plated on LB plates. The plates were incubated for 24 h at 37°C before counting the cfu.
Results and discussion
Activity of cethromycin against prototype and efflux pump mutant strains
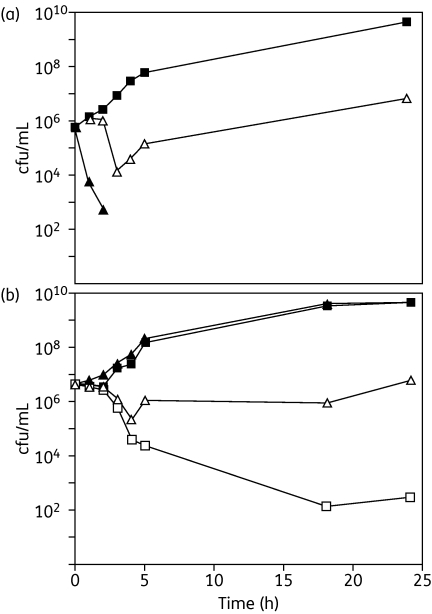
Since B. pseudomallei wild-type (prototype) strains are generally resistant to macrolides because of AmrAB-OprA and BpeAB-OprB efflux pump expression,15,16 we initially tested the susceptibility of strain 1026b and several of its isogenetic efflux pump-proficient or -deficient strains. These experiments revealed that in contrast to the macrolides clarithromycin and erythromycin, cethromycin is a weak substrate for AmrAB-OprA and BpeAB-OprB, but not BpeEF-OprC (Table 2). Time–kill curves with prototype strain 1026b revealed that cethromycin is bacteriostatic at the MIC and bactericidal above the MIC (Figure 2a). Similar observations were made with two clinical isolates, 2637a and 2660a, from Thailand that were less susceptible to cethromycin (measured MICs of 16 and 32 mg/L, respectively) (Figure 2b). As could be predicted by the MICs, the time–kill curves show that at 16 mg/L cethromycin was bactericidal for 2637a and bacteriostatic for 2660a.
Table 2.
Cethromycin and macrolide susceptibilities of Burkholderia pseudomallei wild-type and efflux pump mutant strains
| Pump expressed |
MIC (mg/L) |
|||||
|---|---|---|---|---|---|---|
| Strain | AmrAB-oprA | BpeAB-OprB | BpeEF-OprC | cethromycin | erythromycin | clarithromycin |
| 1026b | + | + | − | 4–8 | 128 | 128 |
| Bp50 | − | + | − | 2 | 8 | 8 |
| Bp58 | − | ++ | − | 4 | 32 | 32 |
| Bp207 | − | − | − | 0.25 | 0.5 | 0.5 |
| Bp216 | − | − | − | 0.25 | 0.5 | ND |
| Bp217 | − | − | + | 0.25 | 0.5 | ND |
| Bp246 | + | − | − | 2 | 64 | 64 |
ND, not done.
Figure 2.
Cethromycin time–kill curves for Burkholderia pseudomallei strains. At time 0, LB medium containing the indicated amounts of cethromycin were inoculated with ∼106 to 107 cfu/mL of the strains listed below. The cultures were shaken at 37°C, aliquots removed at the indicated timepoints and 10-fold serial dilutions plated on LB plates before counting the cfu. (a) Strain 1026b. Filled squares, culture without antibiotic; open triangles, culture with 4 mg/L cethromycin; filled triangles, culture with 16 mg/L cethromycin. (b) Other strains. Filled squares and filled triangles, strains 2637a and 2660a, respectively, in cultures without antibiotic; open symbols, 2637a (squares) or 2660a (triangles) cultures with 16 mg/L cethromycin.
Activity of cethromycin against a panel of B. pseudomallei clinical and environmental isolates
Because of the genetic diversity of B. pseudomallei, it is important to evaluate the in vitro activity of cethromycin against a larger number of strains from diverse sources, e.g. clinical versus environmental strains. Inclusion of environmental isolates is important, because patients in endemic regions acquire their infections from the environment,1,2,17 and environmental and clinical isolates are equally virulent (K. L. Propst, A. Goodyear, S. W. Dow and H. P. Schweizer, unpublished results). We assessed cethromycin activity against a panel of 60 (30 clinical and 30 environmental) isolates from Thailand. While there was some variability between MIC assays conducted at different times, especially with clinical isolates, the MIC range observed with clinical and environmental isolates was similar (4–64 mg/L with clinical and 4–32 mg/L with environmental isolates), and there was no indication of exceptionally susceptible or resistant strains. Overall, the MIC50 and MIC90 were 16 and 29.3 mg/L, respectively. Environmental isolates were consistently more susceptible (MIC50 = 13.3 mg/L and MIC90 = 21.3 mg/L) than clinical isolates (MIC50 = 17.3 mg/L and MIC90 = 29.3 mg/L).
High-level cethromycin resistance is due to AmrAB-OprA overexpression
To assess the propensity of B. pseudomallei for the development of cethromycin resistance and to elucidate possible resistance mechanisms, we selected spontaneous cethromycin-resistant mutants of 1026b. Two isolates that were resistant to ≥32 mg/L cethromycin were retained for further studies, and named Bp289 and Bp290. The two mutants exhibited the same MIC patterns and were multidrug resistant, including against macrolides and aminoglycosides (Table 3). The drug resistance profiles were reminiscent of AmrAB-OprA-expressing strains. Strain 1026b constitutively expresses AmrAB-OprA at some level and is thus resistant to high levels of aminoglycosides and macrolides, yet is fairly susceptible to cethromycin. If this pump is indeed responsible for the high-level cethromycin resistance of Bp289 and Bp290, then these strains must be mutants that overexpress AmrAB-OprA. To assess the suspected role of AmrAB-OprA in the observed high-level cethromycin resistance, we therefore decided to: (i) assess amrB transcript levels in strain Bp289; (ii) check the amrR repressor gene and the amrR-amrA intergenic region for presence of mutations; and (iii) delete the amrAB-oprA operon from strain Bp289. Since Bp289 and Bp290 were derived from the same culture and exhibited the same resistance patterns, we decided to focus on Bp289.
Table 3.
Antimicrobial susceptibilities of prototype strain 1026b and its cethromycin-resistant derivatives
| MIC (mg/L) |
|||||||
|---|---|---|---|---|---|---|---|
| Antibiotic | 1026b | Bp50 | Bp289 | Bp290 | Bp328 | Bp383 | Bp384 |
| Cethromycin | 4–8 | 2 | 128 | 128 | 32 | 32 | 128 |
| Gentamicin | 256 | 1 | 256 | 256 | 1 | 1 | 512 |
| Kanamycin | 64 | 2 | 128 | 128 | 2 | 2 | 128 |
| Erythromycin | 128 | 8 | 512 | 512 | 32 | 32 | 256 |
| Clarithromycin | 128 | 8 | 256 | 256 | 32 | 32 | 256 |
| Norfloxacin | 64 | 16 | 64 | 64 | 64 | 64 | 64 |
| Ciprofloxacin | 16 | 2 | 16 | 16 | 32 | 32 | 32 |
| Tetracycline | 2 | 0.5 | 2 | 2 | 1 | 1 | 2 |
| Doxycycline | 1 | 0.13 | 0.5 | 0.5 | 0.5 | 0.5 | 1 |
| Chloramphenicol | 8 | 8 | 8 | 8 | 16 | 16 | 16 |
| Carbenicillin | 512 | 512 | 256 | 256 | 512 | 512 | 256 |
| Acriflavine | 32 | 16 | 32 | 32 | 8 | 8 | 32 |
The following strains were tested: 1026b, prototype; Bp50, Δ(amrRAB-oprA) derivative of 1026b; Bp289 and Bp290, spontaneous cethromycin-resistant derivatives of 1026b; Bp328, Δ(amrRAB-oprA) derivative of Bp289; Bp383, Bp328 with mini-Tn7T; and Bp384, Bp328 with mini-Tn7T carrying the amrAB-oprA operon from 1026b expressed from its own promoter.
To determine whether AmrAB-OprA was overexpressed in Bp289 versus 1026b, we assessed amrB transcript levels in both isolates by qRT–PCR. These analyses showed that amrB transcripts were increased 4-fold in Bp289 when compared with the parental strain 1026b. This is more than sufficient to achieve the high resistance levels observed in this mutant.
Next, we analysed the amrR repressor gene and the amrR-amrA intergenic region for the presence of mutations that may have led to AmrAB-OprA expression in Bp289. The amrR gene and the amrR-amrA intergenic region were amplified from Bp289 genomic DNA, as described in the ‘Materials and methods’ section. The PCR yielded a 944 bp DNA fragment that contained the 672 bp amrR gene, the 143 bp amrR-amrA intergenic region and 26 bp of the amrA gene. This DNA fragment was sequenced using the same primers used for PCR and aligned with the wild-type 1026b sequence. DNA sequence analysis of two separate PCR products obtained from Bp289 chromosomal DNA templates revealed no mutations in the amrR coding sequence and the amrR-amrA intergenic region. This is consistent with previously reported studies from our laboratory, which showed that constitutive amrAB-oprA expression is not solely due to AmrR repressor mutations, but can also be achieved via a hitherto unknown mechanism(s).18
To demonstrate that the high-level cethromycin resistance of Bp289 was mainly due to AmrAB-OprA overexpression, we deleted the amrAB-oprA operon from this strain. Bp328, the resulting amrRAB-oprA deletion mutant, showed increased susceptibilities to cethromycin, aminoglycosides, macrolides and tetracycline compared with the parental strain Bp289 (Table 3). Single-copy complementation with the amrAB-oprA operon from 1026b in strain Bp384 restored the resistance pattern to that seen in Bp289. A control strain, Bp383, carrying the empty mini-Tn7 cloning and gene integration vector exhibited the same resistance profile as that seen in the recipient strain Bp328. These data unequivocally show that AmrAB-OprA contributes to the high-level cethromycin resistance of Bp289 and is a major cethromycin resistance mechanism. However, Bp328 was more resistant to cethromycin, erythromycin and clarithromycin than Bp50, a Δ(amrRAB-oprA) derivative of 1026b. This indicates that the overexpression of AmrAB-oprA is not the only cethromycin resistance mechanism operating in strain Bp289. Since Bp289 was isolated by growing 1026b in LB broth containing cethromycin, multiple mutations might have occurred during the incubation period.
Other mechanisms contribute to cethromycin resistance
In an attempt to isolate mutants that became cethromycin resistant independent of AmrAB-OprA expression, cells of the Δ(amrRAB-oprA) mutant strain Bp340 were plated on LB agar containing 4 mg/L (2× MIC) cethromycin. Of the nine colonies obtained with this selection procedure after a 100 h incubation at 37°C, eight were 4-fold more resistant to cethromycin (MIC = 8 mg/L) than the parental strain Bp340 (MIC = 2 mg/L). The MIC in one mutant was only marginally (2×) increased. The increased cethromycin MIC was accompanied by 2- to 4-fold increases in erythromycin MICs (from 8 mg/L in Bp340 to 16–32 mg/L in the mutants), but susceptibilities to other antimicrobial agents were unchanged. The simultaneously reduced susceptibilities to cethromycin and erythromycin may be indicative of a common macrolide/ketolide resistance mechanism, which is most likely not efflux as susceptibilities to unrelated drugs (e.g. chloramphenicol, tetracycline, gentamicin and norfloxacin) remained unchanged. The small number of colonies obtained after exposure to a low cethromycin concentration and their low-level resistance probably signifies that the underlying mechanism plays only a minor role in cethromycin resistance. It may, however, contribute to the previously observed residual cethromycin resistance of strain Bp328 (see preceding section).
Conclusions
Unlike macrolides, such as clarithromycin and erythromycin, which are readily effluxed by most B. pseudomallei strains, cethromycin has significant activity against most B. pseudomallei strains tested, with MICs ranging from 4 to 64 mg/L. The cethromycin MIC of prototype strain 1026b is 4–8 mg/L. For strain 1026b, this compares with MICs of 1.5, 4, 1 and 0.5 mg/L of amoxicillin + clavulanic acid, ceftazidime, doxycycline and trimethoprim + sulfamethoxazole, respectively, which are antibiotics currently used for melioidosis therapy. While cethromycin's anti-B. pseudomallei activity is not as potent as that of many current melioidosis therapeutic agents, it approaches that of some of the β-lactam antibiotics (e.g. ceftazidime) currently used for acute-phase treatment. Only in vivo animal experimentation will reveal whether cethromycin is effective for melioidosis therapy, either as a stand-alone drug or in combination with other antibiotics. The intrinsic resistance of B. pseudomallei to many antibiotics is well documented.1,4,19 Moreover, chromosomal mutations can cause resistance to many clinically significant antibiotics. For example, mutations in the chromosomally encoded PenA β-lactamase can cause high-level ceftazidime resistance.20 Strains expressing the BpeEF-OprC efflux pump are resistant to chloramphenicol, tetracyclines and trimethoprim (T. Mima and H. P. Schweizer, unpublished results). Novel therapeutic agents that are not subject to these resistance mechanisms are therefore needed.
Funding
This work was supported by contract number HDTRA1-08-C-0049 from the Joint Science and Technology Office for Chemical and Biological Defense (JSTO-CBD) and the Defense Threat Reduction Agency's (DTRA) Transformational Medical Technologies (TMT) Program (PI: Z.-Q. X.). Initial phases of this work were also supported by a grant (AI065357) from the National Institute of Allergy and Infectious Diseases of the NIH to H. P. S.
Transparency declarations
Z.-Q. X. is employed by and owns stocks and options in Advanced Life Sciences, Inc. Other authors: none to declare.
Acknowledgements
We thank Sharon Peacock for providing clinical and environmental B. pseudomallei isolates from Thailand.
References
- 1.Cheng AC, Currie BJ. Melioidosis: epidemiology, pathophysiology, and management. Clin Microbiol Rev. 2005;18:383–416. doi: 10.1128/CMR.18.2.383-416.2005. doi:10.1128/CMR.18.2.383-416.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wiersinga WJ, van der Poll T, White NJ, et al. Melioidosis: insights into the pathogenicity of Burkholderia pseudomallei. Nat Rev Microbiol. 2006;4:272–82. doi: 10.1038/nrmicro1385. doi:10.1038/nrmicro1385. [DOI] [PubMed] [Google Scholar]
- 3.Currie BJ, Dance DAB, Cheng AC. The global distribution of Burkholderia pseudomallei and melioidosis: an update. Trans R Soc Trop Med Hyg. 2008;102(Suppl 1):S1–4. doi: 10.1016/S0035-9203(08)70002-6. doi:10.1016/S0035-9203(08)70002-6. [DOI] [PubMed] [Google Scholar]
- 4.Wuthiekanun V, Peacock SJ. Management of melioidosis. Expert Rev Anti Infect Ther. 2006;4:445–55. doi: 10.1586/14787210.4.3.445. doi:10.1586/14787210.4.3.445. [DOI] [PubMed] [Google Scholar]
- 5.Peacock SJ, Schweizer HP, Dance DAB, et al. Management of accidental laboratory exposure to Burkholderia pseudomallei and Burkholderia mallei. Emerg Infect Dis. 2008;14 doi: 10.3201/eid1407.071501. doi:10.3201/eid1407.071501, Available from http://www.cdc.gov/EID/content/14/7/e2.htm . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Dance DAB. Melioidosis and glanders as possible biological weapons. In: Fong W, Alibek K, editors. Bioterrorism and Infectious Agents: A New Dilemma for the 21st Century. New York: Springer Science and Business Media; 2005. pp. 99–145. [Google Scholar]
- 7.Liss L. New M13 host: DH5αF′ competent cells. Focus. 1987;9:13. [Google Scholar]
- 8.Sambrook J, Russell DW. Molecular Cloning. Cold Spring Harbor: Cold Spring Harbor Laboratory Press; 2001. [Google Scholar]
- 9.Kumar A, Mayo M, Trunck LA, et al. Expression of resistance–nodulation–cell division efflux pumps in commonly used Burkholderia pseudomallei strains and clinical isolates from northern Australia. Trans R Soc Trop Med Hyg. 2008;102(Suppl 1):S145–51. doi: 10.1016/S0035-9203(08)70032-4. doi:10.1016/S0035-9203(08)70032-4. [DOI] [PubMed] [Google Scholar]
- 10.Mima T, Schweizer HP. The BpeAB-OprB efflux pump of Burkholderia pseudomallei 1026b does not play a role in quorum sensing, virulence factor production, or extrusion of aminoglycosides but is a broad-spectrum drug efflux system. Antimicrob Agents Chemother. 2010;54:3113–20. doi: 10.1128/AAC.01803-09. doi:10.1128/AAC.01803-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lopez CM, Rholl DA, Trunck LA, et al. Versatile dual-technology system for markerless allele replacement in Burkholderia pseudomallei. Appl Environ Microbiol. 2009;75:6496–503. doi: 10.1128/AEM.01669-09. doi:10.1128/AEM.01669-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Choi K-H, DeShazer D, Schweizer HP. Mini-Tn7 insertion in bacteria with multiple glmS-linked attTn7 sites: example Burkholderia mallei ATCC 23344. Nat Protocols. 2006;1:162–9. doi: 10.1038/nprot.2006.25. doi:10.1038/nprot.2006.25. [DOI] [PubMed] [Google Scholar]
- 13.Choi K-H, Mima T, Casart Y, et al. Genetic tools for select agent compliant manipulation of Burkholderia pseudomallei. Appl Env Microbiol. 2008;74:1064–75. doi: 10.1128/AEM.02430-07. doi:10.1128/AEM.02430-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Clinical and Laboratory Standards Institute. Methods for Dilution Antimicrobial Susceptibility Tests for Bacteria That Grow Aerobically—Seventh Edition: Approved Standard M7-A7. Wayne, PA, USA: 2006. CLSI. [Google Scholar]
- 15.Moore RA, DeShazer D, Reckseidler S, et al. Efflux-mediated aminoglycoside and macrolide resistance in Burkholderia pseudomallei. Antimicrob Agents Chemother. 1999;43:465–70. doi: 10.1128/aac.43.3.465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Chan YY, Tan TMC, Ong YM, et al. BpeAB-OprB, a multidrug efflux pump in Burkholderia pseudomallei. Antimicrob Agents Chemother. 2004;48:1128–35. doi: 10.1128/AAC.48.4.1128-1135.2004. doi:10.1128/AAC.48.4.1128-1135.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Inglis TJJ. Melioidosis in man and other animals: epidemiology, ecology and pathogenesis. Vet Bulletin. 2004;74:39N–48N. [Google Scholar]
- 18.Trunck LA, Propst KL, Wuthiekanun V, et al. Molecular basis of rare aminoglycoside susceptibility and pathogenesis of Burkholderia pseudomallei clinical isolates from Thailand. PLoS Negl Trop Dis. 2009;3:e0000519. doi: 10.1371/journal.pntd.0000519. doi:10.1371/journal.pntd.0000519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Holden MTG, Titball RW, Peacock SJ, et al. Genomic plasticity of the causative agent of melioidosis, Burkholderia pseudomallei. Proc Natl Acad Sci USA. 2004;101:14240–5. doi: 10.1073/pnas.0403302101. doi:10.1073/pnas.0403302101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Sam IC, See KH, Puthucheary SD. Variations in ceftazidime and amoxicillin–clavulanate susceptibilities within a clonal infection of Burkholderia pseudomallei. J Clin Microbiol. 2009;47:1556–8. doi: 10.1128/JCM.01657-08. doi:10.1128/JCM.01657-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.DeShazer D, Brett P, Carlyon R, et al. Mutagenesis of Burkholderia pseudomallei with Tn5-OT182: isolation of motility mutants and molecular characterization of the flagellin structural gene. J Bacteriol. 1997;179:2116–255. doi: 10.1128/jb.179.7.2116-2125.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]