Abstract
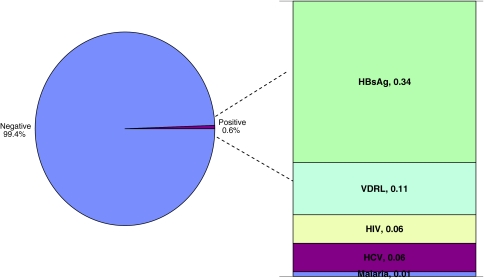
The aim of the study was to find out the prevalence of transfusion transmitted infections (TTI) in voluntary and replacement donors. A total of 9599 donors were analysed for the prevalence of TTI over a period of 2 years.Of these 61.2% were voluntary donors and 38.8% were replacement donors. Prevalence of TTI in total donors was 0.6%. Prevalence of hepatitis B was highest (0.34%) followed by syphilis (0.11%), HIV&HCV (0.06%) and malaria (0.01%). Prevalence was more in male replacement donors. Extensive donor selection and screening procedures will help in improving the blood safety.
Keywords: Voluntary, Replacement, Transfusion transmitted infections
Introduction
Transfusion of blood and its components is life saving as well as it has life threatening hazards. With every unit of blood there is a 1% chance of transfusion associated problems including transfusion transmitted diseases [1]. A majority of known cases of post transfusion diseases have been caused by human immunodeficiency virus (HIV), hepatitis B virus (HBV), hepatitis C virus (HCV), Treponema Pallidum and Malaria parasites. Preventing the transmission of infectious diseases through blood transfusion in developing countries is difficult given that the resources required are not always available even when policies and strategies are in place. These strategies have been extremely effective but transmission of diseases still occurs, primarily because of the inability of the test to detect the disease in the pre-seroconversion or ‘window’ phase of their infection, high cost of screening, a lack of funds and trained personnel, immunologically variant viruses, non-seroconverting chronic or immuno silent carriers and inadvertent laboratory testing errors. Transfusion Transmitted Infections is still a major concern to patients, physicians and policy makers who wish to see a risk free blood supply.
The aim of the present study was to find out prevalence of transfusion transmitted infections(TTI) in voluntary and replacement donors in our hospital transfusion service set up. This study also aids in evaluating the safety of the collected donations.
Materials and Methods
The present study was carried out in Father Muller Medical College Hospital, Mangalore. A total of 9,599 donors were analyzed for the prevalence of Transfusion Transmitted Diseases over a period of 2 years from July 2007 to June 2009. These included replacement donors who donated for ailing patients and were family members, close relatives or friends of the recipient. The voluntary donations primarily were obtained from walk in donors, students and employees of the institution and neighbouring colleges and outdoor blood donation camps. Care was taken to eliminate professional and paid donors by taking history and clinical examination. Basic information regarding age, sex, occupation, number of previous donations was obtained. All samples were screened for hepatitis B surface antigen (ELISA, Hepalisa—J. Mitra & Co.), human immunodeficiency virus (ELISA, Microlisa—J. Mitra & Co), Hepatitis C Virus (ELISA, Microlisa—J. Mitra & Co.), Venereal disease research laboratory test (VDRL) [RPR, Omega Diagnostics Ltd., confirmed by TPHA, Syphicheck—Zephyr Bio medicals] and malaria by rapid card test (parascreen-Zyphyr Biomedicals). Tests were performed according to the manufacturers instructions. All the reactive samples were repeated in duplicate before labeling them seropositive. The donated blood was discarded whenever the pilot donor sample was found positive for any TTI.
The statistical analysis was done using the χ2 test.
Results
A total of 9,599 donors were enlisted in the study. Of these, 5,874 (61.2%) were voluntary and 3,725 (38.8%) replacement donors. Only 681 units were collected through out door camps. Males outnumbered females with 9,357 (97.5%) donations while only 242 (2.5%) donors were females. Among these, 6,576 (68.5%) of the donors aged from 18 to 30 years, 2,273 (23.67%) from 31 to 40 years and 750 (7.83%) were in the 41–55 years age group. Out of the 9,599 blood donors, 58(0.6%) were tested reactive for blood transmitted infection (Fig. 1). Out of this, 38 (65%) were replacement donors. Thirty-three (57%) donors had donated previously, when compared to the 25 first time donors. The prevalence for HIV was 0.06% (6 cases) in total donors, more in replacement (four donors) as compared to voluntary (two donors). The seroprevalence of HBsAg in total donors was 0.34% (33 cases). Replacement donors (19) had a high incidence as compared to voluntary donor s (14 donors). The sero prevalence of VDRL among all donors was 0.11% (11 donors) with the replacement donors(seven donors) having a marginally higher prevalence as compared to voluntary donors (four donors). The sero positivity of HCV in total donors was 0.06% (six donors), with an equal positivity in both the groups of donors. One (0.01%) voluntary blood donor tested positive for malarial parasite. In all the five diseases the incidence was high in males and in replacement donors. The concurrent rates for seroreactivity were highest for HBsAg followed by VDRL, HIV, HCV, and malaria in descending order.
Fig. 1.
Prevalence and distribution of TTI in the present study
Discussion
Transfusion of blood and blood products is a life saving measure and helps innumerable people world wide. At the same time however, blood transfusion is an important mode of transmission of infection to the recipients. In developing countries the prevalence of TTI is much higher and quite far from attaining a zero risk level at the present moment.
Voluntary donors constituted 61% as compared to 39% of replacement donors. This finding is similar the study done by Gupta et al. [2]. The increase in voluntary donors may be attributed to the increasing public awareness and involvement of government bodies like NACO (National AIDS control organisation) who actively propagate voluntary donation in our country. However, many earlier studies have reported increased number of replacement donors [3–8]. Majority of the donors were aged between 18 and 30 years which is in keeping with the age of college students who are often called to donate at our institution. Other studies have similar age distribution [6]. Ninety-seven percent (97%) donations were from males, a finding similar to the other studies [3, 4, 8]. This could be explained on the basis that the Indian women have a very high incidence of anaemia especially in the child bearing age and hence are likely to face disqualification while being screened for blood donation.
Overall prevalence of TTI was 0.6% with a higher prevalence in replacement donors and male donors which correlates well with other studies [2, 4, 5, 9, 10]. Fifty-seven percent (57%) of the seropositive donors had donated previously indicating an increase in prevalence of TTI in repeated donors when compared to the first time donors. Many of the Indian studies show prevalence rates for HIV—0.51–3.87%, HCV 0.12–4%, HBV (HBsAg) 1.2–3.5%, and Syphilis 0.3–0.82% [4, 5, 8, 9, 11–14]. A very low prevalence rate in our study may be attributed to increased number of donors donating at the blood bank with strict screening criteria when compared to the number of donations from the camps. Difference in infection rates between voluntary and replacement donors have been observed in many earlier studies [6, 10, 14]. Concealment of the medical history by professional or replacement donors poses a great threat to the safety of blood supply.
Based on the results we feel that to reduce the risk of these infections non-remunerated repeat voluntary donor services need to be instituted. Extensive donor selection and screening procedures can improve the blood safety. The emphasis must also be laid on voluntary risk reduction, which will require increased awareness and change in the attitude of people. Voluntary blood donation has to be made a part of healthy lifestyle, enlightening the public about the benefits of voluntary blood donations.
References
- 1.Widman FK (ed) (1985) Technical manual. American Association of Blood Banks, Arlington, pp 325–344
- 2.Gupta PK, Kumar H, Basannar DR, Jaiprakash M. Transfusion transmitted infections in armed forces: prevalence and trends. MJAFI. 2006;62:348–350. doi: 10.1016/S0377-1237(06)80105-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kakkar N, Kaur R, Dhanoa J. Voluntary donors—need for a second look. Indian J Pathol Microbiol. 2004;47:381–383. [PubMed] [Google Scholar]
- 4.Garg S, Mathur DR, Garg DK. Comparison of seropositivity of HIV. HBV, HCV and syphilis in replacement and voluntary blood donors in western India. Indian J Pathol Microbiol. 2001;44:409–412. [PubMed] [Google Scholar]
- 5.Sing B, Verma M, Verma K. Markers for transfusion associated hepatitis in north Indian blood donors: prevalence and trends. Jpn J Infect Dis. 2004;57:49–51. [PubMed] [Google Scholar]
- 6.Asif N, Kokhar N, Ilahi F. Seroprevalence of HBC, HCV and HIV infection among voluntary non-remunerated and replacement donors in northern Pakistan. Pak J Med Sci. 2004;1:24–28. [Google Scholar]
- 7.Matee MIN, Magesa PM, Lyamuya EF. Seroprevalence of human immunodeficiency virus, hepatitis B and C viruses and syphilis infections among blood donors at the Muhimbili National Hospital in Dar Es Salaam, Tanzania. BMC Public Health. 2006;6:21. doi: 10.1186/1471-2458-6-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Srikrishna A, Sitalaxmi S, Prema Damodar S. How safe are our safe donors? Indian J Pathol Microbiol. 1999;42:411–416. [PubMed] [Google Scholar]
- 9.Ekadashi R, Langer S (2009) Seroprevalence of Human Immunodeficiency Virus and syphilis in blood donors of Delhi. Indian J Microbiol 27:167–168 [DOI] [PubMed]
- 10.Mujeeb SA, Mehmood K. Prevalence of HBV, HCV and HIV infections among family blood donors. Ann Saudi Med. 1996;16:702–703. doi: 10.5144/0256-4947.1996.702. [DOI] [PubMed] [Google Scholar]
- 11.Makroo RN, Sahil P, Vashist RP, Lal S. Trends of HIV infection in blood donors of Delhi. Indian J Pathol Microbiol. 1996;39:139–142. [PubMed] [Google Scholar]
- 12.Choudhury N, Phadke S. Transfusion transmitted disease. Indian J Paediatr. 2001;68:951–958. doi: 10.1007/BF02722595. [DOI] [PubMed] [Google Scholar]
- 13.Sawke N, Sawke GK, Chawla S. Seroprevalence of common transfusion—transmitted infections among blood donors. People’s J Sci Res. 2010;30:5–7. [Google Scholar]
- 14.Chandra T, Kumar A, Gupta A. Prevalence of transfusion transmitted infections in blood donors: an Indian experience. Trop Doct. 2009;39:152–154. doi: 10.1258/td.2008.080330. [DOI] [PubMed] [Google Scholar]