Sir,
The mechanisms of peripheral neuropathy in any malignancy can be because of a direct effect of the cancer by invasion or compression of nerves, a remote or paraneoplastic effect, or an iatrogenic effect of treatment. Focal or multifocal cranial neuropathies, radiculopathies, and plexopathies typically result from tumor infiltration, herpes zoster infection, or radiation-induced injury. Apart from sensorimotor polyneuropathies, which are the most frequently encountered peripheral nerve syndromes, motor neuropathies, sensory neuronopathies, polyradiculoneuropathies, and autonomic neuropathies can also occur. Although uncommon, paraneoplastic mechanisms should be considered in a patient with malignancy and an associated peripheral nerve disorder, especially in the setting of small-cell lung cancer or lymphoproliferative cancer [1].
A 63 years old, non alcoholic, male presented to us with chief complaints of tingling paresthesias in glove and stocking distribution of the limbs and mild weakness in feet since 3 months. The complaints were insidious in onset and were progressive. He gave history of inability to hold the chappals and frequent slipping of the chappals from feet. There were no weakness in the hands. He did not give any history suggestive of proximal muscle weakness. He was nondiabetic and was not taking any drugs. There was no history of fever of weight loss. General examination did not reveal anything significant apart from mild pallor. There was no evidence of postural hypotension. Examination of skin was normal and there were no thickened/tender nerves on palpation. Other systems examination was normal. In CNS examination higher functions, cranial nerves were normal. Motor system examination revealed mild weakness in plantar flexors of the ankle (patient was unable to stand on the ball of feet without support). Bilateral ankle and knee reflexes were lost. Sensory examination showed hyperasthesia in both legs up to knee joints, position sense was intact and vibration sensation was impaired up to both medial malleolus.
On investigations Hb was 9 gm%, TLC 5500/mm3, DLC polymorphs 62%, lymphocytes 34%, monocytes 2%, eosinophil 2%, few atypical lymphocytes were seen. Absolute platelet count 225000/mm3. All red cell indices (MCV, MCH, MCHC) were within normal limits. Urine examination was normal. Liver and kidney function tests were normal. Fasting blood sugar 98 mg%, PPBS 138 mg%. Serum electrophoresis did not reveal any M spike. ELISA for HIV was negative. Bone marrow examination revealed marrow hyperplasia with some places showing infiltration by atypical lymphocytes. Thyroid profile was normal. CXR showed rounded, homogenous opacity in the left hilar region suggestive of mass (Fig. 1). USG abdomen was normal. EMG/NCV was conducted which revealed decreased nerve conduction velocities, prolonged distal latencies without any conduction block. Compound muscle action potential (CMAP) was normal, suggesting a predominantly demyelinating type of neuropathy. HRCT of thorax revealed left hilar mass (Fig. 2). A CT-guided FNA was done from the left hilar mass for cytological analysis and non Hodgkin’s lymphoma (NHL) was diagnosed (Fig. 3a, b). Immunophenotyping was carried out which was positive for CD 20 and CD 22 suggesting that the lymphoma was of B cell origin. Patient did not give consent for sural nerve biopsy and immunophenotyping. Anti neuronal antibodies status was not done because the patient could not afford.
Fig. 1.
Chest X-ray PA view showing left sided hilar opacity suggestive of mass
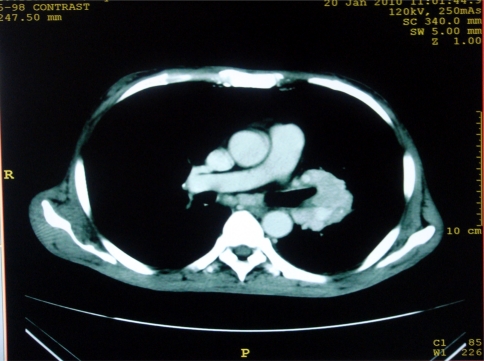
Fig. 2.
HRCT of thorax highlighting the mass and mediastinal lymphadenopathy
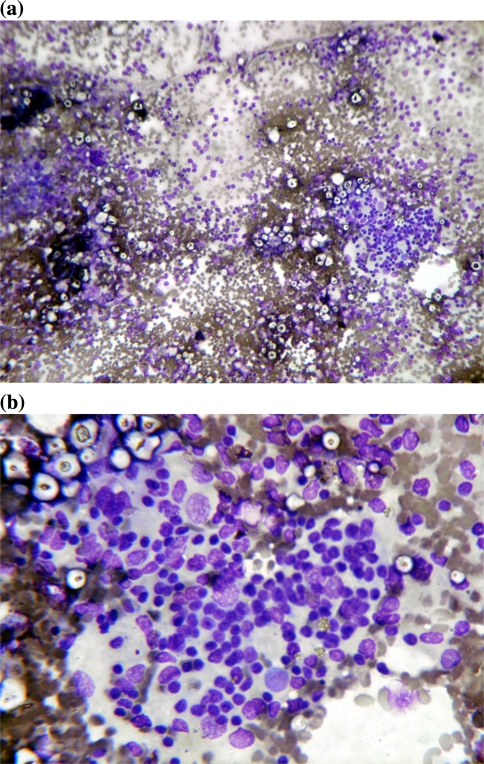
Fig. 3.
a, b Cytological smears 10× and 40× view stained with MGG stain showing cellular smears with predominant lymphocytic population. Lymphocytes are large and atypical with coarse chromatin and prominent nuclei, there is also presence of macrophages, occasional mature lymphocytes with RBCs in background. Cytological features suggestive of lymphoreticular malignancy suspicious of NHL (large cell type)
He was started with CHOP (cyclophosphamide, doxorubicin, vincristine, and prednisone), regime. He tolerated the first cycle well though there was no significant improvement in the symptoms of neuropathy and awaits the second cycle.
Discussion
Lymphoma occasionally affects the peripheral nervous system. Peripheral nervous system abnormalities occur in 5% of patients with lymphoma [2]. The diagnosis can be elusive since many patients present without known lymphoma as in this case. Most peripheral nerve complications are due to NHL, which infiltrates nerves causing axonal damage. Though nerve biopsy could have thrown more light about the pathologic process in our case, the demyelinating nature of the neuropathy probably rules out infiltration. The structures that can be involved in NHL are nerve roots and cranial nerves, often associated with lymphomatous meningitis. NHL may also infiltrate peripheral nerves and cause plexopathy, mononeuropathy, or generalized neuropathy. These neuropathies may resemble an asymmetric mononeuropathy multiplex or a generalized disorder such as chronic inflammatory demyelinating polyradiculoneuropathy (CIDP). When NHL infiltrates diffusely, the term neurolymphomatosis is used. Hodgkin’s lymphoma (HL), by contrast, rarely infiltrates nerves, rather HL causes immunological disorders of the peripheral nervous system such as inflammatory plexopathy or Guillain-Barré syndrome. Other rare lymphomas such as intravascular lymphoma and Waldenstrom’s macroglobulinemia can also affect peripheral nerves in specific ways. In addition, other malignant and nonmalignant lymphoproliferative disorders enter into the differential diagnosis of lymphomatous neuropathy [3].
NHL are malignant lymphoid proliferations which may be of B or T cell type. In a study of 13 observations of association between peripheral neuropathy and B type NHL, it was found that none of the cases had evidence of meningeal propagation or neurotoxicity from chemotherapy. The various mechanisms of peripheral neuropathy in these cases were split into four broad groups [4].
Group I: Peripheral nerve lesions were directly linked to a propagation of malignant cells into the peripheral nervous system; this was revealed by autopsy and/or nerve biopsy. Malignant B cell proliferation was demonstrated in three out of four of these cases by immunolabelling of the infiltrates. This category suggested the direct infiltration of the NHL in the nervous tissue.
Group II: This group included three patients whose serum contained a monoclonal immunoglobulin (IgM) with antimyelin activity, and two of them had pathological IgM deposits in endoneurial connective tissue.
Group III: In this group the peripheral neuropathy was immune mediated. The immune dysfunction of the NHL was responsible for a Guillain-Barré syndrome in one, and for a chronic inflammatory demyelinating polyneuropathy in the other.
Group IV: Included two patients in whom the mechanism of the peripheral neuropathy, although almost certainly directly related to the NHL, was hypothetised to be paraneoplastic manifestation or, possibly, an undetected lymphomatous invasion of nervous tissue.
Immunolabelling of lymphomatous proliferations and nerves is now of considerable value for classifying and indicating the exact aetiology of the peripheral neuropathy. It can also detect pathogenic consequences of any associated monoclonal dysglobulinemia.
As per the above observations, the cause of neuropathy in our case was probably paraneoplastic in etiology as a diagnosis of exclusion, because, it was predominantly demyelinating type, serum electrophoresis ruled out monoclonal gammopathy, clinical examination did not favour Guillain-Barré or CIDP.
Nervous system affection in lymphoma demands aggressive chemotherapy. There are evidences where therapy can regress the neuropathic symptoms [4], but a lot of literature suggest that, treatment of the underlying lymphoma is only rarely followed by recovery of the associated neuropathy.
References
- 1.Amato AA, Collins MP. Neuropathies associated with malignancy. Semin Neurol. 1998;18(1):125–144. doi: 10.1055/s-2008-1040868. [DOI] [PubMed] [Google Scholar]
- 2.Kelly JJ, Karcher DS. Lymphoma and peripheral neuropathy: a clinical review. Muscle Nerve. 2005;31(3):301–313. doi: 10.1002/mus.20163. [DOI] [PubMed] [Google Scholar]
- 3.Vallat JM, Mascarel HA, Bordessoule D, Jauberteau MO, Tabaraud F, Gelot A, Vallat AV. Non-Hodgkin malignant lymphomas and peripheral neuropathies—13 cases. Brain. 1995;118(5):1233–1245. doi: 10.1093/brain/118.5.1233. [DOI] [PubMed] [Google Scholar]
- 4.Hughes RA, Britton T, Richards M. Effects of lymphoma on the peripheral nervous system. J R Soc Med. 1994;87(9):526–530. doi: 10.1177/014107689408700915. [DOI] [PMC free article] [PubMed] [Google Scholar]