Abstract
A two months old male infant, presented with fever, hepatosplenomegaly and pancytopenia. On bone marrow aspirate, hemophagocytosis was noted. Trephine biopsy showed epithelioid granulomas. ZN stain AFB detected, which confirmed the diagnosis of miliary tuberculosis. This case highlights the rare association of hemophagocytic syndrome with tuberculosis in infancy.
Keywords: AFB, Granulomas, Pancytopenia, Trephine biopsy
Introduction
The diagnosis of tuberculosis is more difficult in children because symptoms are non-specific; chest x ray scans are less specific; standard sputum samples can rarely be collected; and children have lower bacterial loads, making culture more difficult. Infants and young children are at much more risk of developing disseminated infection after primary tuberculosis and particularly tuberculosis meningitis, which has the highest mortality. The same is true for immunocompromised patients. Child to child transmission is rare because of lower bacterial loads. Children usually acquire infection from infected parents or household contacts, so the family should always be screened [1].
Based on previous publications, it appears that TB associated with HPS is more common in adults than in children. In the reported cases, pancytopenia was present in all at some point of illness [2].
In our case there were no pulmonary findings, with the initial presentation being pancytopenia and infection associated hemophagocytic syndrome. Hemophagocytic syndrome can be the initial presentation without pulmonary findings in miliary TB, so it should be considered as a differential diagnosis for fever of unknown origin associated with pancytopenia and hemophagocytosis [3].
Case Report
A two months old male infant, first born to parents of nonconsanguineous marriage, presented with fever since 15 days and abdominal distension since 7 days.
He was born after a full term normal delivery with birth weight of 2.8 kg. BCG had been administered.
On examination he was febrile (101F), pale, abdomen was distended, liver and spleen were palpable 4 cm. There was no peripheral lymphadenopathy. Examination of other systems revealed no abnormalities.
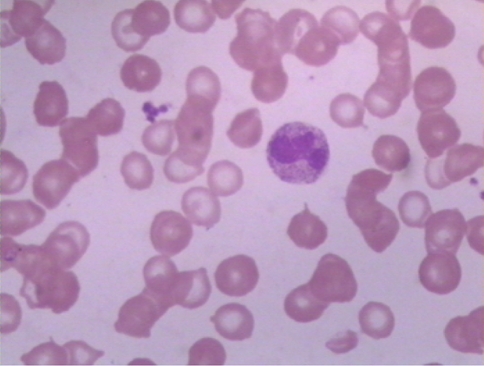
Initial laboratory work-up showed, Hb—5.6 gm%, WBC count—3,800/cmm, DLC—Metamyelocytes + Band—02%, Polymorphs—48%, Lymphocytes—46%, Monocytes—04%, Platelet count—1,18,000/cmm, PBS—Normocytic normochromic RBC’s, mild anisocytosis seen (Fig. 1). WBC—Mild leukopenia, few neutrophils show toxic changes and shift to left. Occasional atypical lymphocytes were seen. Platelets were mildly low on smear. Prothrombin Time and activated Partial Thromboplastin Time were normal. Total Bilirubin—0.6 mg/dl, Total protein—4.9 gm/l, Albumin—2.4 gm/dl, Globulin—2.5 gm/dl. USG—showed hepatosplenomegaly with multiple hypoechoic deposits. Chest radiograph was normal.CSF examination was normal and routine blood culture was sterile.
Fig. 1.
Peripheral Blood Smear—×100
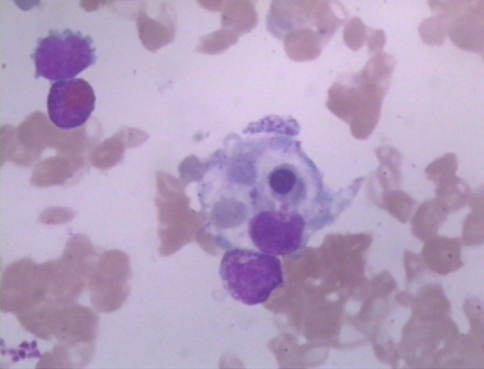
In view of fever and pancytopenia on hemogram, a bone marrow aspiration and biopsy was done. Bone marrow aspirate was adequate, normocellular marrow particles were seen. Erythroid series showed normal progressive maturation, myeloid series showed maturation arrest at myelocyte-metamyelocyte stage. Megakaryocytes were adequate and there was an increase in reticulum cells with few showing hemophagocytosis (Fig. 2).
Fig. 2.
Bone Marrow Aspirate- Hemophagocytosis—×100
As bone marrow aspirate was showing hemophagocytosis, further investigations were advised to rule out hemophagocytic syndrome. Fibrinogen was 120 mg% (150–450 mg%), Serum Triglycerides was 285 mg% (up to 160 mg%), Serum Ferritin—582 mcg/dl (9.3—278 mcg/dl). As the child was fulfilling five out of eight criterions, the diagnosis of hemophagocytic syndrome was offered.
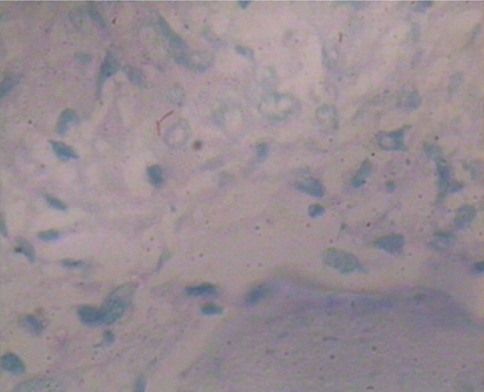
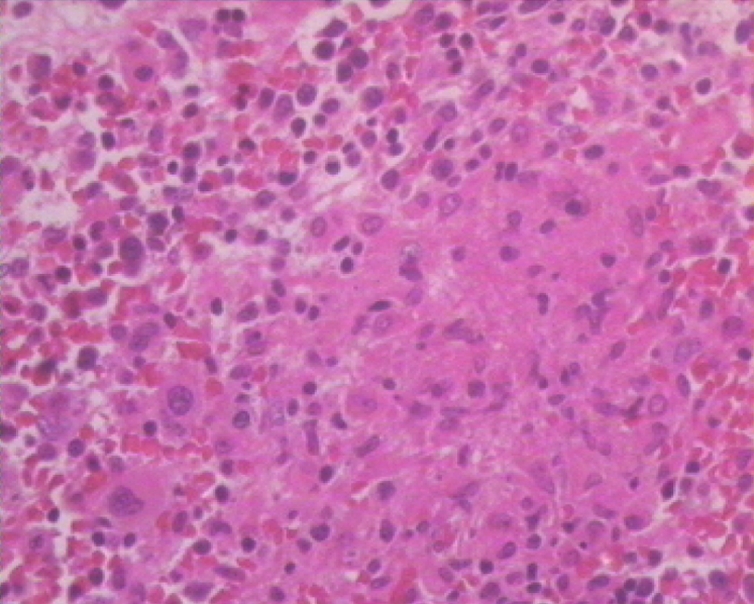
The bone marrow trephine biopsy showed foci of normal hemopoiesis, megakaryocytes were adequate. Few epithelioid granulomas (Fig. 3) and occasional Langhan’s giant cell were seen. Z N stain done on the biopsy revealed AFB1+ in the granulomas (Fig. 4). Thus the diagnosis of Miliary tuberculosis with secondary hemophagocytic syndrome was given.
Fig. 3.
Trephine biopsy Epithelioid Granulomas—×40
Fig. 4.
Trephine biopsy ZN stain—×100
ToRCH, HIV and HBsAg was negative.Serum IgM, IgG and IgA levels were normal. Lymphocyte subset analysis was advised.
To find the source of infection, the family history was reviewed and the parents were investigated. No family history of sibling deaths was found. No history of infection of family members could be documented. Chest radiograph of parents were normal. Mantoux test was negative in both the parents. Both the parents were HIV negative.
No past history of TB was found in mother. A high cervical swab did not reveal AFB, so a D&C was advised.
Anti- tubercular therapy was initiated with isoniazid (INH) 5 mg/kg/day, rifampicin 10 mg/kg/day, ethambutol 15 mg/kg/day, pyrazinamide 20 mg/kg/day (2HRZE + 7HR) regimen and hydrocortisone 2 mg/kg/day tapered over a period of one month. Child responded well to the treatment, fever subsided & hematological parameters reverted back to normal.
Discussion
This case report highlights the importance of a trephine biopsy in infants, which is generally avoided. The AFB positive epithelioid granuloma on the biopsy (Fig. 3), enabled us to offer the diagnosis to the patient. On initiating Anti Koch’s treatment, the patient’s clinical condition improved.
Clinical manifestations with fever, abdominal distension, and hepatosplenomegaly are common in newborn with tuberculosis [4, 5]. In our case, the infant presented with similar clinical features and hemophagocytic syndrome. According to the Histiocytic Society protocol entitled HLH 2004 [6] the diagnosis of HLH can be established if 5 out of 8 diagnostic criteria are fulfilled (i) Fever (>7 days), (ii) Splenomegaly, (iii) Cytopenia(>2 lineage)—anaemia <9 gm%, thrombocytopenia (<1,00,000/cmm) and ANC (<1,000/cmm). (iv) Hypertriglyceridemia(>265 mg/dl), (v) Hemophagocytosis (bone marrow, spleen, lymph node.), (vi) Low or absent natural killer cell activity, (vii) Hyperferritinemia (500 mcg/dl), (viii) Increased soluble CD25 > 2400 u/ml. In our case 5 out of 8 criteria were fulfilled, so the diagnosis of tuberculosis associated with hemophagocytic syndrome was given.
In this case the mother was asymptomatic. This is consistent with a previous report that up to 75% mother whose newborn had TB were asymptomatic before delivery [4].
Shaw et al. [7] recently reported a 7-week-old girl who developed IAHS and rapidly died of undiagnosed pulmonary tuberculosis. Successful treatment of IAHS usually depends on a specific treatment for the known infectious agent and adequate supportive care. In this infant resolution of HPS seems to be the result of adequate treatment of tuberculosis and adjunct doses of steroids. Two weeks course of hydrocortisone (4 mg/kg/day) in disseminated TB with DIC was reported with a favorable outcome [4]. In most pediatric cases success of therapy was attributed to initiation of therapy early in the course of illness [2].
Acknowledgments
We thank Dr. Anand Pandit, Head of Department of Pediatrics, KEM hospital, Pune for referring this case.
Abbrevations
- AFB
Acid fast bacilli
- HPS
Hemophagocytic syndrome
- ZN Stain
Zeihl Neelsen stain
- ANC
Absolute neutrophil count
- HIV
Human immunodeficiency virus
- D&C
Dilation and curettage
- TB
Tuberculosis
- IAHS
Infection associated hemophagocytic syndrome
References
- 1.Pavithra Logitharajah, Beate Kampamann (2008) Tuberculosis in children.In: student BMJ Archive. Available via http://archive.student.bmj.com/issues/08/09 education/326.php. Accessed 3 June 2009
- 2.Balasubramanian S, Kaarthigeyan K, Aparna V, Srinivas S. Tuberculosis-associated Haemophagocytic Syndrome in Infancy. Indian Pediatr. 2008;45:593–595. [PubMed] [Google Scholar]
- 3.Dilber E, Erduran E, Kalyocu M, Aynaci FM, Okten A, Ahmetoglu A. Hemophagocytic syndrome as an initial presentation of miliary tuberculosis without pulmonary findings. Scand J Infect Dis. 2002;34:689–692. doi: 10.1080/00365540210147840. [DOI] [PubMed] [Google Scholar]
- 4.Adhikari M, Pillay T, Pillay DG. Tuberculosis in the newborn: an emerging disease. Pediatr Infect Dis J. 1997;16:1108–1112. doi: 10.1097/00006454-199712000-00003. [DOI] [PubMed] [Google Scholar]
- 5.Abughali N, Kuyp F, Annable W, Kumar ML. Congenital tuberculosis. Pediatr Infect Dis J. 1994;13:738–741. doi: 10.1097/00006454-199408000-00012. [DOI] [PubMed] [Google Scholar]
- 6.Henter JI, Home A, Arico M, Egeler RM, Filipovin AH, Imashuku S, et al. HLH-2004: Diagnostic and therapeutic guidelines for hamophagocytic lymphohistiocytosis. Pediatr Blood Cancer. 2007;48:124–131. doi: 10.1002/pbc.21039. [DOI] [PubMed] [Google Scholar]
- 7.Shaw PH, Brown D, Shulman ST( Tuberculosis-associated hemophagocytic syndrome in an infant. Pediatr Infect Dis J. 2000;19::475–477. doi: 10.1097/00006454-200005000-00018. [DOI] [PubMed] [Google Scholar]