Abstract
Background
Obesity prevalence has continuously increased in Northern Sweden as elsewhere. A cohort effect has been shown and an increasing proportion of the middle-aged population is maintaining body weight.
Objective
To test the hypothesis that the obesity epidemic continues but at different speeds that are dependent on socioeconomic status.
Design
Cross-sectional (103,940 adults) and longitudinal (26,872 adults) data from the Västerbotten Intervention Program 1990–2007 were included. All adults in Västerbotten County are invited to a health examination at the ages of 40, 50, and 60 years. Body mass index (BMI) and socioeconomic status, assessed by residence location, marital status, and education were evaluated.
Results
BMI increased in all groups but was greater among men. During 1990–1995 and 2002–2007, mean BMIs were 25.9 and 26.8 among men and 25.2 and 25.9 among women. The trend of increasing BMI slowed around the year 2000 (p<0.001), but this was only observed among the highly educated adults in the most urbanized area. The difference between educational groups increased throughout the study period (men p=0.014, women p=0.002). Longitudinal data for both sexes showed a twofold higher baseline prevalence of obesity among individuals with basic compared to high education and it nearly doubled in all groups during the 10-year follow-up. Low education, living in a rural environment, and living alone were independent predictors of obesity development. The overall cumulative 10-year incidence was 9.4% in men, 9.1% in women, and twofold higher among those with basic and mid-level education who live in rural areas compared to those with high education who live in cities.
Conclusion
The trend of increasing obesity has slowed in this middle-aged Northern Sweden population, but this trend shift occurred primarily among those with high education who live in an urban environment. Greater efforts to combat obesogenic environments are needed and should take socioeconomic and sociocultural aspects into account.
Keywords: obesity/epidemiology, prevalence, incidence, socioeconomic status, environmental impact
Obesity is increasing in most populations and is identified by the WHO as a major health problem (1, 2). In developed countries, obesity is the sixth most important health risk and is associated with a dose-response relation to disease burden (3), primarily cardiovascular diseases, diabetes, and cancer (4–6). Although the situation in Sweden has been less alarming than in some other countries (7–10), the increase in body mass index (BMI) across all age groups has followed the same pattern (11). Cohort data that compare the Northern Sweden MONICA population with a US population showed that the Swedish 1999 BMI distribution was similar to the US 1989 pattern. This suggested that if the trend continued, the 2009 obesity prevalence in Sweden would be the same as the US in 1999 (12).
The highest increase in obesity has occurred among young adults (13, 14). A social gap, with higher obesity prevalence among adult groups with lower education occurs in Sweden as elsewhere (14–19). An urban–rural gradient is also demonstrated (18, 19) but this inequality has been declining since the mid-1990s, at least among younger men (19). In 2002, the prevalence of overweight (BMI 25–29.9) in the middle-aged Swedish population was 34% in women and 54% in men living in rural areas (20). In urban environments, prevalence of overweight was 27% for women and 43% for men (13). Obesity prevalence (BMI ≥ 30) was 19% for both sexes in rural areas (20) compared to 11% of women and 15% of men living in urban environments (13).
A greater increase in obesity among younger age groups, as well as increasing abdominal obesity in all groups aged 25–74 years during 1986–2004, was demonstrated in the Northern Sweden WHO-MONICA study performed in Västerbotten and Norrbotten counties (21, 22). In the Västerbotten Intervention Program (VIP), an ongoing study in Västerbotten separate from the WHO-MONICA study, annual cross-sectional surveys of 30–60 year olds between 1990 and 2004 showed similar patterns (23). Obesity prevalence increased from 9.4 to 17.5%, with the highest prevalence among 60 year olds. Longitudinal data in this study show that the individuals most likely to gain weight are the youngest, those with normal body weight, and those without health problems. After 1993, the increase of obesity slowed among 60-year-old women. A time trend was also observed, with an increasing proportion of individuals maintaining body weight. This suggests that the obesity epidemic might be slowing. However, such a trend is not yet evident in cross-sectional data (23).
This study aims to further investigate these trends and uses both cross-sectional and longitudinal data collected in the VIP between 1990 and 2007. The hypothesis is that the obesity epidemic continues in northern Sweden but at speeds dependent upon socioeconomic status as measured by educational level, marital status, and location of residence.
Methods
Setting
Västerbotten County is located in Northern Sweden and covers an eighth of the country, from the Gulf of Bothnia to the Scandinavian Mountains. Its population of approximately 250,000 is concentrated on the coast and about 40% lives in the city of Umeå. Umeå is a medium-sized city (population 112,000 during 2007) and contains the regional administrative center, a university, and the regional hospital. A third of the population lives in two small cities that are commercial and industrial centers: the coastal city of Skellefteå (population 72,000) and the inland city of Lycksele (population 13,000). The rest of the population is spread out in smaller municipalities and sparsely populated rural areas.
Västerbotten intervention program
The VIP has been conducted in Västerbotten County since 1985. The cardiovascular disease (CVD) mortality rate in Västerbotten was the highest in the country and, therefore, VIP was launched by local authorities to reduce CVD and diabetes. VIP was planned in collaboration with health care providers and Umeå University, tested in a single community, and then extended to the rest of the county in 1990. Two sustaining principles are that the program is integrated into routine activities at every primary health care center and all inhabitants are invited to a health examination the years they turn 40, 50, or 60 years old. Initially, those aged 30 years were also invited. Due to low participation rates and economic restrictions, 30 year olds were not included after 1995. The standardized health examinations are conducted by trained district nurses and include assessment of classical risk factors for CVD and a comprehensive questionnaire regarding socioeconomic status, housing situation, and self-reported health and lifestyle habits. The results of the examination are discussed individually with each participant following principles of motivational interviewing. Health promotion activities are suggested. Details of the development, design, and methodology of VIP have been described elsewhere (24).
Study population
This report is based on consecutive cross-sectional surveys conducted during 1990–2007 with 112,920 subjects. Results will be presented for three periods: 1990–1995, 1996–2001, and 2002–2005. Participation rates were 48–57% during 1990–1995, 57–65% during 1996–2001, and 63–66% during 2002–2007. Since inclusion of 30-year olds was discontinued in 1995, data from this age group (n=8,980) were excluded from the cross-sectional analyses. This left 103,940 subjects (48.1% men). Of these, a few subjects were missing BMI data (0.6%), educational level (1.1%), or marital status (1.2%).
In addition to cross-sectional data, longitudinal data were available. Three panels of VIP-participants aged 30, 40, and 50 years were surveyed at baseline during 1990–1997 and returned for a follow-up visit 10 years later (during 2000–2007). Of the 38,041 participants in 1990–1997, 2,657 were not eligible for follow-up due to death (n=909), migration out from the region (n=1,688), or other causes (n=60). Among eligible subjects, 26,872 participants returned a second time and the participation rate was 75%. A dropout analysis showed that the mean BMI was 25.0 among participants and 25.4 among non-participants. There were 46% men among participants and 50.1% among non-participants. Educational levels among participants were 22.7% with basic, 53.4% with mid-level, and 23.9% with high education. The corresponding proportions among non-participants were 22.7% with basic, 51.9% with mid-level, and 25.4% with high education.
Measurements
Height and weight were measured in light indoor clothing and used to calculate BMI (kg/m2). Participant BMI was categorized as normal (18.5–24.9), overweight (25–29.9), or obese (≥30) according to WHO definitions (7).
Socioeconomic status was assessed by marital status, location of residence, and education. Marital status was categorized into married/cohabitant or single. Single denoted living alone, divorced, or widowhood. Living with or without children was not recorded. Education was assessed as highest attained education level according to the Swedish education system. Nine years of school is compulsory and this was defined as basic education. Completion of 12 years of school was defined as mid-level education. University (postsecondary education) was defined as high education. Geographical residence location was categorized as living in a medium-sized city (i.e. Umeå where the administrative center and a university are located), in a small city (Skellefteå or Lycksele, which are commercial and industrial centers), or in a rural area (small municipalities and sparsely populated areas).
Statistics
Descriptive statistics for continuous variables are presented as mean±SD. Categorical variables are presented as percentages. Independent sample t-tests were used to compare means and χ2 tests to compare distributions. Analyses of BMI with categorical and continuous covariates were done with ANOVA. A linear regression model including a second degree time-component was used to test for BMI trend. Univariate and multivariate logistic regression analyses with calculation of odds ratios (ORs) and 95% confidence intervals were used to study the association between obesity and several predictors. When applicable, age standardization was performed and done separately for men and women using the age distribution of the whole dataset as the standard. Unless noted as relative changes (% change), differences in prevalence are reported as absolute changes (% units). Statistical significance was assumed at p<0.05. Statistical analyses were performed with the SPSS 15.0/PC version.
Ethical considerations
This study was approved by the regional Research Ethics Board in Umeå (08-131M and 07-142Ö). Individuals gave informed consent prior to each health screening.
Results
Cross-sectional data: population trends in BMI and BMI categories
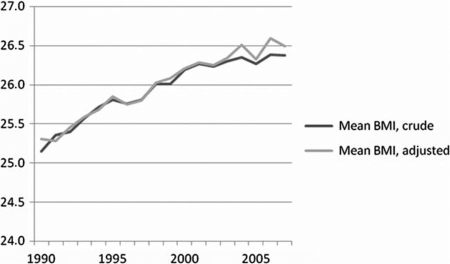
Distribution and characteristics of the participants during the three periods (1990–1995, 1996–2001, and 2002–2007) are presented in Table 1. For men and women, the proportion of 40-year olds decreased by 6% from 1990–1995 to 2002–2007 and the proportion of 60-year olds increased correspondingly. From 1990–1995 to 2002–2007, mean BMI increased from 25.9 to 26.8 among men and from 25.2 to 25.9 among women. BMI units increased by 0.5 for both sexes from 1990–1995 to 1996–2001. From 1996–2001 to 2002–2007, BMI units increased 0.4 among men and 0.2 among women. In 1990–1995, 47% of men and 32% of women were overweight, 10% of men and 13% of women were obese. The prevalence of overweight increased by 2–3% for men and women during 1996–2001 and then decreased by 0.4% in men and 0.9% in women. Among men, obesity prevalence increased between the periods by 3.6 and 3.7%. The corresponding increases among women were 2.4 and 1.4%. Thus, during 2002–2007, 17% of both men and women were obese and 50% of men and 33% of women were overweight. The trends in BMI were significant in the linear component (p<0.001) and the second degree component (p<0.001) and slowed from about 2000 (Fig. 1). During 1995–2007, there was a population shift from rural to urban areas. Educational levels increased in the population as a whole, but the majority of those with high education lives in the largest city. When surveyed in 2002–2007, the proportion of men with high education by residence location was 35% in the largest city, 20% in the small cities, and 14% in rural areas and for women 46, 29, and 23%.
Table 1.
Characteristics of Västerbotten Intervention Program participants, 1990–2007. There were highly significant differences (p<0.005) for all variables except marital status between 1990–1995 versus 1996–2001, and 1996–2001 versus 2002–2007 for men and women. Marital status differed between the two first periods for men (p=0.023) but not for women (p=0.92)
| Men | Women | |||||
|---|---|---|---|---|---|---|
| Time period | 1990–1995 | 1996–2001 | 2002–2007 | 1990–1995 | 1996–2001 | 2002–2007 |
| Number of participants | 13,737 | 16,774 | 19,506 | 15,544 | 18,081 | 20,298 |
| Age (%) | ||||||
| 40 years | 37.9 | 32.7 | 32.0 | 37.2 | 32.8 | 31.7 |
| 50 years | 35.6 | 38.5 | 33.7 | 35.3 | 37.4 | 34.0 |
| 60 years | 26.5 | 28.8 | 34.4 | 27.4 | 29.8 | 34.3 |
| BMI, mean±SD | 25.9±3.4 | 26.4±3.5 | 26.8±3.9 | 25.2±4.2 | 25.7±4.4 | 25.9±4.7 |
| BMI categoriesa (%) | ||||||
| Overweight | 47.2 | 49.8 | 49.4 | 32.2 | 34.2 | 33.3 |
| Obese | 10.0 | 13.6 | 17.3 | 12.7 | 15.1 | 16.5 |
| Education (%) | ||||||
| Basic:≤9 years | 35.6 | 27.5 | 18.5 | 33.8 | 25.2 | 16.3 |
| Mid-level: 10–12 years | 45.5 | 51.6 | 56.8 | 42.7 | 46.1 | 48.9 |
| High:≥13 years | 18.9 | 20.8 | 24.7 | 23.6 | 28.7 | 34.8 |
| Marital status (%) | ||||||
| Married/cohabitant | 82.4 | 81.3 | 79.6 | 82.0 | 82.0 | 80.5 |
| Location of residenceb (%) | ||||||
| Medium-sized city | 38.3 | 34.1 | 40.4 | 39.5 | 36.2 | 41.9 |
| Small cities | 31.4 | 36.7 | 34.1 | 32.7 | 37.0 | 34.1 |
| Rural | 30.3 | 29.2 | 25.4 | 27.8 | 26.8 | 24.0 |
BMI: overweight 25–29.9 and obesity ≥30.
Location of residence: Umeå is a medium-sized city with administrative centers and a university. The small cities are Skellefteå and Lycksele, which are commercial and industrial centers. Rural is the remainder of the county and includes provincial municipalities and sparsely populated areas.
Fig. 1.
Mean body mass index (BMI) of Västerbotten Intervention Program participants during 1990–2007, crude and adjusted for age, sex, and education.
Prevalences of obesity increased, normal weight decreased, and overweight was relatively stable in all educational groups. The absolute increase in obesity prevalence from the first period 1990–1995 to the third period 2002–2007 was 4.9–10.3% among men and 3.2–6.5% among women. The largest increases were seen in the basic and mid-level educational groups. Those groups also had the highest obesity prevalence during the first period. Among men, the relative increase was 80% in the basic and the mid-level educational groups and 70% in the high educational group. Among women, the relative increases were 40, 50, and 40% for advancing educational groups. In contrast to the basic education group and men with mid-level education, obesity prevalence in the other educational and sex groups increased to a smaller extent between the second and third periods compared to the first and second periods (Table 2a). In all educational groups, obesity was more prevalent among women than men during the first period. Due to a marked increase among men, the obesity prevalence was higher among men during the third period. During the three study periods, the difference in obesity prevalence between men with basic versus high education was 5.3, 6.6, and 10.7%. Among women, the differences were 8.2, 9.1, and 11.5%. Thus, increasing divergence in obesity prevalences were seen between educational groups over time. These differences were statistically significant in both men (p=0.014) and women (p=0.002). Normal weight decreased in all educational groups. Overweight showed a decreasing tendency among men and women with basic education, while increases were seen among those with mid-level and high education. When overweight and obesity categories were combined (BMI ≥ 25) for men, an absolute increase of 8.9% and a relative increase of 10% was seen from the first to the third period in the group with basic education, 10.1% absolute and 10% relative increase in the group with mid-level education, and 8.9% absolute and 20% relative increase in the high education group. Increases among the women were in absolute estimates 5.4, 6.5, and 4.4% and the relative increases were 10% in all educational groups. Thus, increases of BMI ≥ 25 were similar across all educational groups of men and women but larger among men.
Table 2a and 2b.
Prevalence of age-adjusted body mass index (BMI) categories (%) by educational level (2a) and location of residence (2b) among men and women in the Västerbotten Intervention Program, Sweden, 1990–2007. Columns entitled ‘Change’ show the absolute increase or decrease between the first and third study periods
| 2a | Men | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Basic educationa | Mid-level education | Higher education | ||||||||||
| 1990–1995 | 1996–2001 | 2002–2007 | Change | 1990–1995 | 1996–2001 | 2002–2007 | Change | 1990–1995 | 1996–2001 | 2002–2007 | Change | |
| BMI <18.5 | 0.3 | 0.3 | 0.3 | 0.0 | 0.3 | 0.3 | 0.2 | −0.1 | 0.1 | 0.3 | 0.2 | 0.1 |
| BMI 18.5–24.9 | 37.4 | 32.6 | 28.4 | −8.9 | 41.5 | 35.8 | 31.5 | −10.0 | 48.7 | 42.1 | 39.7 | −9.0 |
| BMI 25–29.9 | 49.7 | 50.7 | 48.3 | −1.4 | 48.4 | 50.5 | 50.2 | 1.8 | 43.9 | 47.7 | 47.9 | 4.0 |
| BMI ≥30 | 12.6 | 16.5 | 22.9 | 10.3 | 9.9 | 13.4 | 18.1 | 8.2 | 7.3 | 9.9 | 12.2 | 4.9 |
| Women | ||||||||||||
| Basic education | Mid-level education | Higher education | ||||||||||
| 1990–1995 | 1996–2001 | 2002–2007 | Change | 1990–1995 | 1996–2001 | 2002–2007 | Change | 1990–1995 | 1996–2001 | 2002–2007 | Change | |
| BMI <18.5 | 1.1 | 0.7 | 1.1 | 0.0 | 0.9 | 0.9 | 1.0 | 0.1 | 1.0 | 0.8 | 1.2 | 0.2 |
| BMI 18.5–24.9 | 48.3 | 43.5 | 42.9 | −5.4 | 53.2 | 48.6 | 46.6 | −6.7 | 61.2 | 56.8 | 56.7 | −4.5 |
| BMI 25 − 29.9 | 34.2 | 36.4 | 33.1 | −1.1 | 33.7 | 34.8 | 34.7 | 0.9 | 29.5 | 32.2 | 30.7 | 1.2 |
| BMI ≥30 | 16.4 | 19.3 | 22.9 | 6.5 | 12.2 | 15.7 | 17.8 | 5.6 | 8.2 | 10.2 | 11.4 | 3.2 |
Level of education: basic is ≤9 years (which is compulsory), mid-level is 10–12 years, and high is ≥13 years or university.
| 2b | Men | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Medium-sized citya | Small cities | Rural | ||||||||||
| 1990–1995 | 1996–2001 | 2002–2007 | Change | 1990–1995 | 1996–2001 | 2002–2007 | Change | 1990–1995 | 1996–2001 | 2002–2007 | Change | |
| BMI < 18.5 | 0.3 | 0.2 | 0.2 | −0.1 | 0.2 | 0.4 | 0.2 | 0.0 | 0.3 | 0.2 | 0.3 | 0.0 |
| BMI18.5–24.9 | 44.2 | 38.1 | 35.3 | −8.9 | 42.4 | 36.9 | 34.9 | −7.5 | 38.2 | 33.4 | 27.7 | −10.5 |
| BMI 25–29.9 | 47.2 | 49.5 | 49.5 | 2.3 | 47.4 | 50.0 | 48.8 | 1.4 | 48.8 | 50.0 | 49.6 | 0.8 |
| BMI ≥30 | 8.4 | 12.2 | 15.1 | 6.7 | 10.0 | 12.7 | 16.1 | 6.1 | 12.8 | 16.4 | 22.5 | 9.7 |
| Women | ||||||||||||
| Medium-sized city | Small cities | Rural | ||||||||||
| 1990–1995 | 1996–2001 | 2002–2007 | Change | 1990–1995 | 1996–2001 | 2002–2007 | Change | 1990–1995 | 1996–2001 | 2002–2007 | Change | |
| BMI <18.5 | 1.0 | 0.9 | 1.2 | 0.2 | 1.0 | 1.0 | 1.1 | 0.0 | 0.9 | 0.7 | 0.9 | 0.1 |
| BMI 18.5–24.9 | 59.0 | 54.8 | 53.7 | −5.3 | 53.1 | 50.8 | 50.8 | −2.3 | 47.1 | 43.5 | 42.9 | −4.3 |
| BMI 25–29.9 | 31.3 | 33.6 | 32.2 | 0.9 | 33.2 | 33.8 | 33.1 | −0.1 | 35.9 | 37.1 | 35.6 | −0.3 |
| BMI ≥30 | 9.7 | 11.8 | 13.9 | 4.2 | 13.6 | 15.4 | 16.0 | 2.4 | 17.1 | 19.7 | 21.6 | 4.5 |
Location of residence: Umeå is a medium-sized city with administrative centers and a university. The small cities are Skellefteå and Lycksele, which are commercial and industrial centers. Rural is the remainder of the county and includes provincial municipalities and sparsely populated areas.
When BMI development was evaluated by urban–rural categorization, similar trends were seen with a stable prevalence of overweight, an increase in obesity, and a decrease in prevalence of normal weight. The largest increase in age-adjusted obesity, both in absolute (6.7–9.7%) and relative (60–80%) estimates, occurred among men and was most pronounced in the rural areas. Obesity increased less markedly among women (2.4–4.5% absolute and 20–40% relative, respectively) and among those in the small cities. In all three residence locations, obesity prevalence was higher among women in the first period, but the men caught up and passed them during the last period when obesity was slightly more common among men (Table 2b).
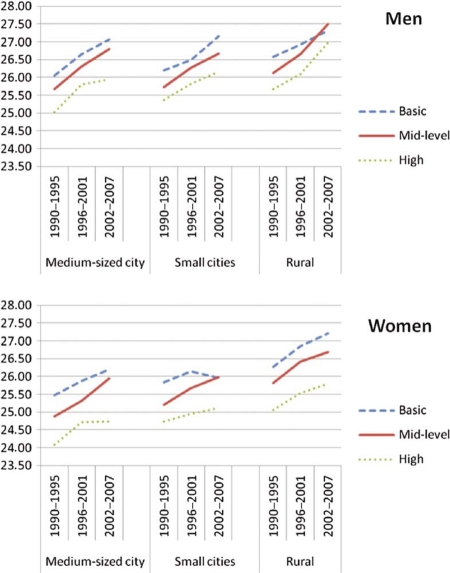
Age-adjusted mean BMI across time periods by education and residence location are shown in Fig. 2. There were different patterns of BMI development within educational groups when controlled for residence location. Among men in the rural area, BMI increased more between 1996–2001 and 2002–2007 compared to 1990–1995 and 1996–2001, irrespective of educational level. A similar increase in BMI was seen among men with basic education who live in small cities. By contrast, BMI increases slowed in 2002–2007 among men with high education in the medium-sized city of Umeå. Overall, there were only small differences between educational groups among men in rural areas after the year 2000, while differences between educational groups increased in Umeå. The differences between educational groups among women were more pronounced in all residence locations compared to men. Women with high education living in the medium-sized city of Umeå had only small increases in BMI during 2002–2007. Thus, differences in mean BMI between educational groups increased in both men and women in the most urbanized area. In the small cities, mean BMI declined among women with basic education. Age-adjusted BMI development over time differed by residence location for men (p=0.009) and women (p=0.008), i.e. there were time-by-residence location interactions. Similar patterns were found for education and residence location among men (p=0.020) and for education and time among women (p=0.020). In addition, an interaction that included time, residence location, and education was observed among men (p=0.036) but not among women (p=0.096).
Fig. 2.
1990–2007 cross-sectional data of mean age-adjusted body mass index (BMI) among Västerbotten Intervention Program participants by sex and education in three geographical areas. Location of residence: Umeå is a medium-sized city with administrative centers and a university. The small cities are Skellefteå and Lycksele, which are commercial and industrial centers. Rural is the remainder of the county and includes provincial municipalities and sparsely populated areas. Level of education: basic is ≤ 9 years (which is compulsory), mid-level is 10–12 years, and high is ≥13 years or university.
Longitudinal data: obesity changes over 10 years among men and women who were 30, 40, or 50 years old at baseline
The prevalence of obesity at baseline was twofold higher among participants with basic education compared to those with high education and nearly doubled in all groups during the 10-year period (Table 3). The prevalence of obesity increased by 7.6, 8, and 5.4% among men with basic, mid-level, and high education and by 8.9, 7.6, and 5.5%, respectively, among women.
Table 3.
Prevalence (%) of overweight and obesity by educational level among men and women who participated in the Västerbotten Intervention Program for the first time during 1990–1997 (baseline) and at a 10-year follow-up survey. Data for men and women were adjusted separately to the age distribution of the dataset
| Men | Women | |||||||
|---|---|---|---|---|---|---|---|---|
| Overweighta (%) | Obesity (%) | Overweight (%) | Obesity (%) | |||||
| Baseline | Follow-up | Baseline | Follow-up | Baseline | Follow-up | Baseline | Follow-up | |
| Educationb | ||||||||
| Basic | 45.9 | 52.8 | 10.5 | 18.1 | 31.4 | 36.3 | 12.0 | 20.9 |
| Mid-level | 45.4 | 52.1 | 8.3 | 16.3 | 29.0 | 36.1 | 9.4 | 17.0 |
| High | 38.9 | 49.4 | 5.3 | 10.7 | 23.6 | 32.1 | 6.0 | 11.5 |
BMI: overweight 25–29.9, obesity ≥30.
Level of education: basic ≤9 years (which is compulsory), mid-level is 10–12 years, and high is ≥13 years or university.
The 10-year cumulative incidence of obesity in this population was 9.4% among men and 9.1% among women. The incidence was twofold higher among men and women with basic and mid-level education who live in rural areas compared to those with high education who live in medium-sized or small cities (Table 4). Men and women with high education who live in cities had similar risks of developing obesity. These were clearly lower than similarly educated citizens living in rural areas. Among men and women with basic and mid-level education, the obesity incidence was lowest in the small cities. Overall, the highest incidences were seen in the rural areas: Men with mid-level education had a 13.1% incidence and women with basic education had a 12.9% incidence. In rural areas, the incidence of obesity was of the same magnitude (10–13%) regardless of education or sex. Men and women with basic education had similar risks irrespective of where they lived. By contrast, among those with high education, the obesity risk was almost twofold in rural areas compared to the medium-sized city of Umeå. Analyses that used educational level and residence location at follow-up instead of baseline were similar (data not shown).
Table 4.
10-year incidence (%) of obesity (BMI ≥ 30) among middle-aged Västerbotten Intervention Program participants by educational level and location of residence
| Men | Women | |||||||
|---|---|---|---|---|---|---|---|---|
| Basica | Mid-level | High | χ2-test | Basic | Mid-level | High | χ2-test | |
| Location of residenceb | ||||||||
| Medium-sized city | 9.4 | 9.6 | 5.6 | <0.001 | 11.5 | 9.2 | 5.7 | <0.001 |
| Small cities | 8.5 | 8.2 | 5.9 | ns | 10.5 | 8.7 | 6.1 | 0.002 |
| Rural | 11.6 | 13.1 | 9.8 | ns | 12.9 | 10.7 | 9.7 | ns |
| χ2-test | ns | <0.001 | 0.009 | ns | ns | 0.001 | ||
Level of education: basic ≤ 9 years (which is compulsory), mid-level is 10–12 years, and high is ≥13 years or university.
Location of residence: Umeå is a medium-sized city with administrative centers and a university. The small cities are Skellefteå and Lycksele, which are industrial and commercial centers. Rural is the remainder of the county and includes provincial municipalities and sparsely populated areas.
Multivariate logistic regression was used to evaluate the effect of baseline socioeconomic status on the 10-year risk of developing obesity (Table 5). In this analysis, participants were excluded if they were obese at baseline. In the univariate analysis, the risk of developing obesity was significantly higher among those who lived alone, had an education of <13 years, or lived in rural areas. There were no differences by sex, age, or between residence in the medium-sized city versus the small cities. The ORs for education, marital status, and residence location remained significant and were minimally attenuated after adjustment for all covariates in the multivariate analysis. Thus, the risk of developing obesity was 50% higher among those with mid-level education and 60% higher among individuals with basic education compared to those with high education. In addition, a 40% higher risk of becoming obese was observed for those living in rural areas compared to the most urbanized area and a 30% higher risk among those who lived alone compared to those who were married or cohabitating.
Table 5.
Univariate and multivariate logistic regression analyses with an outcome of obesity (BMI ≥ 30) at 10-year follow-up among Västerbotten Intervention Program participants who were not obese at baseline during 1990–1997. All variables in the univariate model are included in the multivariate model
| Univariate | Multivariate | |||||
|---|---|---|---|---|---|---|
| n | Developed obesity (%) | OR | CI (95%) | OR | CI (95%) | |
| Age at baseline | ||||||
| 30 years | 4 810 | 9.3 | 1.0 | 1.0 | ||
| 40 years | 9 780 | 9.0 | 1.0 | 0.86–1.09 | 1.0 | 0.88–1.13 |
| 50 years | 9 613 | 9.5 | 1.3 | 0.91–1.15 | 1.0 | 0.89–1.14 |
| Sex | ||||||
| Men | 11,324 | 9.4 | 1.0 | 1.0 | ||
| Women | 12,879 | 9.1 | 1.0 | 0.89–1.06 | 1.0 | 0.93–1.11 |
| Marital status | ||||||
| Married/cohabitant | 20,107 | 8.8 | 1.0 | 1.0 | ||
| Single | 3,771 | 11.6 | 1.4 | 1.22–1.52 | 1.3 | 1.20–1.51 |
| Educationa | ||||||
| High | 5,899 | 6.5 | 1.0 | 1.0 | ||
| Mid-level | 13,061 | 9.8 | 1.6 | 1.40–1.77 | 1.5 | 1.34–1.71 |
| Basic | 4,937 | 10.8 | 1.7 | 1.52–2.01 | 1.6 | 1.41–1.88 |
| Location of residenceb | ||||||
| Medium-sized city | 9,475 | 8.3 | 1.0 | 1.0 | ||
| Small cities | 7,933 | 8.4 | 1.0 | 0.91–1.13 | 0.9 | 0.85–1.06 |
| Rural | 6,795 | 11.6 | 1.5 | 1.31–1.62 | 1.4 | 1.21–1.51 |
Level of education: Basic is ≤9 years (which is compulsory), mid-level is 10–12 years in school, and high is ≥13 years or university.
Location of residence: Umeå is a medium-sized city with administrative centers and a university. The small cities are Skellefteå and Lycksele, which are commercial and industrial centers. Rural is the remainder of the county and includes provincial municipalities and sparsely populated areas.
Discussion
The obesity epidemic is still on the rise but slowing is observed among the middle-aged population in Northern Sweden. This corresponds to a previous finding that a higher proportion of adults in later cohorts from this population did not gain weight (23). The obesity prevalences and increases are similar in magnitude to those seen in other recent Swedish studies (13, 18, 20). However, this is the first time that the trend of increasing BMI is observed to be slowing among adults. The findings suggest that obesity trends in Sweden during 2009 were not the same as those seen in 1999 in the US as was previously assumed (11, 12, 22). Recently it was reported that the increasing prevalence of obesity slowed among US adults during 1999–2008 (25). Thus, obesity trends are slowing concurrently in the US and Sweden.
BMI-development in this population was not equally distributed with respect to sex or socioeconomic factors. A plateau was seen in the most urbanized area among men and (especially) women with high education, while obesity continued to increase in other subgroups. The only exception was that of women with basic education who live in small cities. Furthermore, the absolute and relative increases in obesity prevalence were more pronounced among men and this trend was similar in all educational groups. Thus, the trend is more alarming among men. This is in agreement with results from other Swedish studies (11, 13, 15). Therefore, a gender perspective is important in the understanding of obesity development. In addition, men and women with basic education started at the highest obesity prevalence and increased the most in absolute estimates. The group with high education started at the lowest obesity prevalence and increased the least. In the longitudinal analysis, baseline prevalences of overweight and obesity were also highest among those with basic education. Certainly there were marked 10-year increases of overweight and obesity in all educational groups, but for both men and women the greatest increases in obesity were among those with basic and mid-level education.
Our results demonstrate that the gap between educational groups, with regard to obesity prevalence, is widening in this middle-aged population. Lifestyle habits, including physical activity, tobacco use, alcohol consumption, and dietary patterns, have changed considerably in this region (26, 27). However, the increase in physically active behaviors is observed mainly in the adults with high education and is greatest among women, while sedentary behaviors are stable in all educational groups (manuscript in preparation). Therefore, earlier adoption of healthy lifestyles among those with high education might contribute to the slowing trend of obesity.
Earlier phases of the obesity epidemic (during 1980–1997) were evaluated in a study that used a random sample from the entire Swedish population. That study used self-reported data that were calibrated to measured data, and found that obesity increased by 45% in men and 33% in women (relative increases) with the most rapid increase occurring from the end of the 1980s until the mid-1990s (14). Among 45–64-year olds, the relative increase of combined overweight and obesity prevalence (BMI ≥ 25) was similar to our study: 21% among men and 8% among women. This is in agreement with our results and lower than the increase in obesity (29% among men and 22% among women). There was a persistent gap between educational groups during 1980–1997. Evaluations of data from the same data source as the aforementioned study, but using data from 1996 to 2001, showed continuing increases in BMI and obesity (18). Again, these changes were less marked among those with higher education and who live in more urbanized regions. Our results are also in agreement with a study from the southernmost part of Sweden that showed increasing educational differences in obesity prevalence among men and persisting among women from the mid-1980s until the mid-1990s (17). However, the overall prevalence of overweight and obesity were consistently higher in our study. This might be because BMI was measured in our study but was self-reported in the study by Lindström et al. (17). Obesity prevalence in a rural area in the south of Sweden was recently evaluated using standardized measurements (20). That study found a prevalence similar to the rural areas of our study and also documented increasing trends of obesity.
These studies describe the Swedish obesity epidemic among adults and show that obesity prevalence continues to increase, although our study indicates that the incremental increases in obesity prevalence are slowing. A recent Swiss study showed stabilization in mean BMI since 2002, as well as a greater increase in BMI among those with low education (28). To our knowledge, no study has reported reduction of obesity prevalence among adult populations. Interestingly, our results are compatible with recent studies from different regions in Sweden that found that the prevalences of overweight and obesity are no longer increasing among school children. This decline in obesity is most marked among girls and the socioeconomic gradient persists (29–31). Further studies are needed to determine if the obesity epidemic among adults is also slowing in other parts of Sweden and whether it will spread out to all socioeconomic groups.
Besides education, other contextual factors need to be identified to help explain the development of obesity. We observed that the trend of a lesser increase in BMI among those with high education occurred only among those living in the most urbanized area. Likewise, there was no significant difference between educational groups with regard to the 10-year risk of obesity in rural areas for men and women, nor among men who live in small cities. The impact of educational level and location of residence is also demonstrated in the regression analysis, as both characteristics remained significant with little change in ORs in the multivariate model. Therefore, in spite of high education being more common in urbanized areas, the rural-urban difference in obesity development cannot be explained solely by differences in educational level alone. The population included in this health survey is homogeneous and therefore it is unlikely that the differences between residential areas are due to genetic variability. The finding of a higher vulnerability for obesity development among those who live alone, may have numerous explanations. As 20% of our study population is single, marital status may be an important factor in overall obesity development.
Our results indicate that in addition to individual characteristics, other social and cultural factors connected to the living environment are operational in the development of obesity. A strong urban-rural gradient of increasing BMI within all socioeconomic strata has previously been shown among young Swedish men (military conscripts) (19). The authors concluded that this gradient could not be explained by individual factors (parental education, socioeconomic position, or measured by IQ). Obesity as a social phenomenon is also emphasized in international reviews of cross-sectional (32, 33) and longitudinal (34) studies. In addition to education, economic and socio-cultural aspects are important. Thus, patterns of weight change are very complex. This is highlighted by the significant interactions between time, education and location of living with different patterns seen for men and women.
There is a need to elucidate why urban environments, with access to training facilities and an abundant choice of healthy foods, have more favorable effects on BMI among those with high compared to basic education. How does the rural environment, with its plentiful opportunities for outdoor life and healthy living differ from urban life irrespective of attained level of education? What is the role of motorized commuting (eg, car, bus, train) to work instead of travel by foot or bicycle? The decreases in BMI differences between educational groups among men who live in rural areas and concurrent increases in differences in urban environments also raises questions. The impact of attitudes and cultural norms, expectations and strategies in controlling BMI development within different socioeconomic groups and among both sexes needs to be addressed in further studies. Qualitative methodology may be the preferred way to clarify these factors (35).
Our results are consistent with the findings that most strategies designed to combat obesity and promote weight loss at an individual level through educational, behavioral, or pharmacological approaches have limited long-term success (36). It has been argued that there needs to be a shift from the view of obesity as a personal disorder to obesity as the consequence of an obesogenic environment (37–39). Obesogenic environments promote slow long-term weight gain through a small degree of positive energy balance resulting from marginal increases in food intake and/or sedentary behaviors. The challenge will be to find and implement structural changes that make it easier to adopt healthy lifestyles for those who need them most. These might include structural changes that support healthy choices such as those recommended by educational efforts. At a 2006 WHO ministerial conference, governmental representatives (including Swedes), experts, and civil society representatives declared their commitment to counter obesity in Europe (40). Our data, based on recent measurements, underscore that there is still much more to do.
This study was performed in a setting that allows for long-term population-based standardized measurements with high participation rates. One limitation is that only middle-aged subjects are included and this restricts our conclusions to those aged 30–60 years. Concordant with a previous evaluation of longitudinal data, our dropout analysis showed that participants with higher education and higher baseline BMI were less likely to return for a follow-up visit (23). However, since these groups also are at the lowest risk of gaining weight, our results can be viewed as a conservative perspective on obesity trends.
In conclusion, mean BMI and obesity prevalence are still increasing within this population in Northern Sweden. The increase is most marked among men, those with basic education, or living in rural areas. The overall trend of increasing obesity has slowed since 2000, but this has occurred primarily among citizens with high education who live in an urban environment. The gap in obesity development between urban and rural areas cannot be explained by educational differences alone or vice versa. Efforts are needed to counteract obesity development among people living in more obesogenic environments. This is a challenge for health care providers, policy makers, and social planners.
Conflict of interest and funding
This research was supported by the Västerbotten County Council and by a grant from the Swedish Council for Working Life and Social Research (FAS), and is included in the Ageing and Living Conditions Programme at Umeå University that is financed by the Swedish Research Council's ‘Linnestöd,’ no 2006-21576-36119-66.
References
- 1.WHO. Geneva: WHO; 2000. Obesity: preventing and managing the global epidemic. Report of a WHO Consultation (WHO Technical Report Series 894) Available from: http://www.who.int/nutrition/publications/obesity/WHO_TRS_894/en/index.html [cited 25 February 2010] [PubMed] [Google Scholar]
- 2.Kumanyika S, Jeffery RW, Morabia A, Ritenbaugh C, Antipatis VJ. Obesity prevention: the case for action. Int J Obes Relat Metab Disord. 2002;26:425–36. doi: 10.1038/sj.ijo.0801938. [DOI] [PubMed] [Google Scholar]
- 3.Ezzati M, Lopez AD, Rodgers A, Vander Hoorn S, Murray CJ. Selected major risk factors and global and regional burden of disease. Lancet. 2002;360:1347–60. doi: 10.1016/S0140-6736(02)11403-6. [DOI] [PubMed] [Google Scholar]
- 4.Peeters A, Barendregt JJ, Willekens F, Mackenbach JP, Al Mamun A, Bonneux L. Obesity in adulthood and its consequences for life expectancy: a life-table analysis. Ann Intern Med. 2003;138:24–32. doi: 10.7326/0003-4819-138-1-200301070-00008. [DOI] [PubMed] [Google Scholar]
- 5.Haslam DW, James WP. Obesity. Lancet. 2005;366:1197–209. doi: 10.1016/S0140-6736(05)67483-1. [DOI] [PubMed] [Google Scholar]
- 6.Field AE, Coakley EH, Must A, Spadano JL, Laird N, Dietz WH, et al. Impact of overweight on the risk of developing common chronic diseases during a 10-year period. Arch Intern Med. 2001;161:1581–6. doi: 10.1001/archinte.161.13.1581. [DOI] [PubMed] [Google Scholar]
- 7.Global database on body mass index [database on the Internet] 2008. Available from: http://www.who.int/bmi/index.jsp [cited 25 February 2010]
- 8.Andreyeva T, Michaud PC, van Soest A. Obesity and health in Europeans aged 50 years and older. Public Health. 2007;121:497–509. doi: 10.1016/j.puhe.2006.11.016. [DOI] [PubMed] [Google Scholar]
- 9.Silventoinen K, Sans S, Tolonen H, Monterde D, Kuulasmaa K, Kesteloot H, et al. Trends in obesity and energy supply in the WHO MONICA Project. Int J Obes Relat Metab Disord. 2004;28:710–8. doi: 10.1038/sj.ijo.0802614. [DOI] [PubMed] [Google Scholar]
- 10.Berghofer A, Pischon T, Reinhold T, Apovian CM, Sharma AM, Willich SN. Obesity prevalence from a European perspective: a systematic review. BMC Public Health. 2008;8:200. doi: 10.1186/1471-2458-8-200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Neovius M, Janson A, Rossner S. Prevalence of obesity in Sweden. Obes Rev. 2006;7:1–3. doi: 10.1111/j.1467-789x.2006.00190.x. [DOI] [PubMed] [Google Scholar]
- 12.Nafziger AN, Stenlund H, Wall S, Jenkins PL, Lundberg V, Pearson TA, et al. High obesity incidence in northern Sweden: how will Sweden look by 2009? Eur J Epidemiol. 2006;21:377–82. doi: 10.1007/s10654-006-9001-5. [DOI] [PubMed] [Google Scholar]
- 13.Berg C, Rosengren A, Aires N, Lappas G, Toren K, Thelle D, et al. Trends in overweight and obesity from 1985 to 2002 in Goteborg, West Sweden. Int J Obes (Lond) 2005;29:916–24. doi: 10.1038/sj.ijo.0802964. [DOI] [PubMed] [Google Scholar]
- 14.Lissner L, Johansson SE, Qvist J, Rossner S, Wolk A. Social mapping of the obesity epidemic in Sweden. Int J Obes Relat Metab Disord. 2000;24:801–5. doi: 10.1038/sj.ijo.0801237. [DOI] [PubMed] [Google Scholar]
- 15.Eiben G, Dey DK, Rothenberg E, Steen B, Bjorkelund C, Bengtsson C, et al. Obesity in 70-year-old Swedes: secular changes over 30 years. Int J Obes (Lond) 2005;29:810–7. doi: 10.1038/sj.ijo.0802940. [DOI] [PubMed] [Google Scholar]
- 16.Kark M, Rasmussen F. Growing social inequalities in the occurrence of overweight and obesity among young men in Sweden. Scand J Public Health. 2005;33:472–7. doi: 10.1080/14034940510032130. [DOI] [PubMed] [Google Scholar]
- 17.Lindstrom M, Isacsson SO, Merlo J. Increasing prevalence of overweight, obesity and physical inactivity: two population-based studies 1986 and 1994. Eur J Public Health. 2003;13:306–12. doi: 10.1093/eurpub/13.4.306. [DOI] [PubMed] [Google Scholar]
- 18.Sundquist K, Qvist J, Johansson SE, Sundquist J. Increasing trends of obesity in Sweden between 1996/97 and 2000/01. Int J Obes Relat Metab Disord. 2004;28:254–61. doi: 10.1038/sj.ijo.0802553. [DOI] [PubMed] [Google Scholar]
- 19.Neovius M, Rasmussen F. Place of residence and obesity in 1,578,694 young Swedish men between 1969 and 2005. Obesity (Silver Spring) 2008;16:671–6. doi: 10.1038/oby.2007.115. [DOI] [PubMed] [Google Scholar]
- 20.Nyholm M, Gullberg B, Haglund B, Rastam L, Lindblad U. Higher education and more physical activity limit the development of obesity in a Swedish rural population. The Skaraborg Project. Int J Obes (Lond) 2008;32:533–40. doi: 10.1038/sj.ijo.0803725. [DOI] [PubMed] [Google Scholar]
- 21.Eliasson M, Lindahl B, Lundberg V, Stegmayr B. Diabetes and obesity in Northern Sweden: occurrence and risk factors for stroke and myocardial infarction. Scand J Public Health Suppl. 2003;61:70–7. doi: 10.1080/14034950310001360. [DOI] [PubMed] [Google Scholar]
- 22.Lilja M, Eliasson M, Stegmayr B, Olsson T, Soderberg S. Trends in obesity and its distribution: data from the Northern Sweden MONICA survey, 1986–2004. Obesity (Silver Spring) 2008;16:1120–8. doi: 10.1038/oby.2008.8. [DOI] [PubMed] [Google Scholar]
- 23.Nafziger AN, Lindvall K, Norberg M, Stenlund H, Wall S, Jenkins PL, et al. Who is maintaining weight in a middle-aged population in Sweden? A longitudinal analysis over 10 years. BMC Public Health. 2007;7:108. doi: 10.1186/1471-2458-7-108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Norberg MW, S. Boman K, Weinehall L. The Västerbotten intervention programme: background, design and implications. Global Health Action. 2010;3:4643. doi: 10.3402/gha.v3i0.4643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Flegal KM, Carroll MD, Ogden CL, Curtin LR. Prevalence and trends in obesity among US adults, 1999–2008. JAMA. 2010;303:235–41. doi: 10.1001/jama.2009.2014. [DOI] [PubMed] [Google Scholar]
- 26.Krachler B, Eliasson M, Stenlund H, Johansson I, Hallmans G, Lindahl B. Population-wide changes in reported lifestyle are associated with redistribution of adipose tissue. Scand J Public Health. 2009;37:545–53. doi: 10.1177/1403494808099971. [DOI] [PubMed] [Google Scholar]
- 27.Lindahl B, Stegmayr B, Johansson I, Weinehall L, Hallmans G. Trends in lifestyle 1986–99 in a 25- to 64-year-old population of the Northern Sweden MONICA project. Scand J Public Health Suppl. 2003;61:31–7. doi: 10.1080/14034950310001414. [DOI] [PubMed] [Google Scholar]
- 28.Marques-Vidal P, Bovet P, Paccaud F, Chiolero A. Changes of overweight and obesity in the adult Swiss population according to educational level, from 1992 to 2007. BMC Public Health. 2010;10:87. doi: 10.1186/1471-2458-10-87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Lissner L, Sohlstrom A, Sundblom E, Sjoberg A. Trends in overweight and obesity in Swedish schoolchildren 1999–2005: has the epidemic reached a plateau? Obes Rev. 2010;11:553–9. doi: 10.1111/j.1467-789X.2009.00696.x. [DOI] [PubMed] [Google Scholar]
- 30.Sjoberg A, Lissner L, Albertsson-Wikland K, Marild S. Recent anthropometric trends among Swedish school children: evidence for decreasing prevalence of overweight in girls. Acta Paediatr. 2008;97:118–23. doi: 10.1111/j.1651-2227.2007.00613.x. [DOI] [PubMed] [Google Scholar]
- 31.Sundblom E, Petzold M, Rasmussen F, Callmer E, Lissner L. Childhood overweight and obesity prevalences levelling off in Stockholm but socioeconomic differences persist. Int J Obes (Lond) 2008;32:1525–30. doi: 10.1038/ijo.2008.104. [DOI] [PubMed] [Google Scholar]
- 32.McLaren L. Socioeconomic status and obesity. Epidemiol Rev. 2007;29:29–48. doi: 10.1093/epirev/mxm001. [DOI] [PubMed] [Google Scholar]
- 33.Roskam AJ, Kunst AE. The predictive value of different socio-economic indicators for overweight in nine European countries. Public Health Nutr. 2008;11:1256–66. doi: 10.1017/S1368980008002747. [DOI] [PubMed] [Google Scholar]
- 34.Ball K, Crawford D. Socioeconomic status and weight change in adults: a review. Soc Sci Med. 2005;60:1987–2010. doi: 10.1016/j.socscimed.2004.08.056. [DOI] [PubMed] [Google Scholar]
- 35.Lindvall K, Larsson C, Weinehall L, Emmelin M. Weight maintenance as a tight rope walk – a grounded theory study. BMC Public Health. 2010;10:51. doi: 10.1186/1471-2458-10-51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Weiss EC, Galuska DA, Kettel Khan L, Gillespie C, Serdula MK. Weight regain in U.S. adults who experienced substantial weight loss, 1999–2002. Am J Prev Med. 2007;33:34–40. doi: 10.1016/j.amepre.2007.02.040. [DOI] [PubMed] [Google Scholar]
- 37.Egger G, Swinburn B. An “ecological” approach to the obesity pandemic. BMJ. 1997;315:477–80. doi: 10.1136/bmj.315.7106.477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Hill JO. Understanding and addressing the epidemic of obesity: an energy balance perspective. Endocr Rev. 2006;27:750–61. doi: 10.1210/er.2006-0032. [DOI] [PubMed] [Google Scholar]
- 39.Swinburn B, Egger G, Raza F. Dissecting obesogenic environments: the development and application of a framework for identifying and prioritizing environmental interventions for obesity. Prev Med. 1999;29:563–70. doi: 10.1006/pmed.1999.0585. [DOI] [PubMed] [Google Scholar]
- 40.WHO. European charter on counteracting obesity. Istanbul. 2006 Available from: http://www.euro.who.int/Document/E89567.pdf [cited 2 December 2009]