Abstract
The natural history for inhalational Bacillus anthracis (Ames strain) exposure in New Zealand white rabbits was investigated to better identify potential, early biomarkers of anthrax. Twelve SPF Bordetella-free rabbits were exposed to 150 LD50 aerosolized B. anthracis spores, and clinical signs, body temperature, complete blood count, bacteremia, and presence of protective antigen in the blood (that is, antigenemia) were examined. The development of antigenemia and bacteremia coincided and preceded both pyrexia and inversion of the heterophil:lymphocyte ratio, an indicator of infection. Antigenemia was determined within 1 h by electrochemiluminescence immunoassay, compared with the 24-h traditional culture needed for bacteremia determination. Rabbits appeared clinically normal until shortly before succumbing to anthrax approximately 47 h after challenge or approximately 22 h after antigenemia, which suggests a relatively narrow therapeutic window of opportunity. To evaluate the therapeutic rabbit model, B. anthracis-exposed rabbits were treated (after determination of antigenemia and later confirmed to be bacteremic) intravenously with the fluoroquinolone antibiotic levofloxacin for 5 d at a total daily dose of 25 or 12.5 mg/kg, resulting in nearly 90% and 70% survival, respectively, to the study end (28 d after challenge). The peak level for 12.5 mg/kg was equivalent to that observed for a 500-mg daily levofloxacin dose in humans. These results suggest that intravenous levofloxacin is an effective therapeutic against inhalational anthrax. Taken together, our findings indicate that antigenemia is a viable and early biomarker for B. anthracis infection that can be used as a treatment trigger to allow for timely intervention against this highly pathogenic disease.
Abbreviations: ECL, electrochemiluminescence; PA, protective antigen
Inhalation is the most lethal route of exposure for spores of the gram-positive bacterium Bacillus anthracis.36,37 Without aggressive prophylaxis or intervention, inhalational anthrax—characterized by extensive bacteremia and toxemia—results in high mortality rates.4,6,7 In humans, inhalational anthrax initially presents with nonspecific to mild influenza-like symptoms (for example, fatigue, myalgia, headache, and nonproductive cough) during a prodromal phase culminating with the onset of a severe, acute fulminant phase marked by high fever, dyspnea, hypotension, shock, and sudden death.18,24,42 Aerosolized B. anthracis is an important biothreat.36,37 The 1979 anthrax outbreak in Sverdlosk, Russia, and the 2001 anthrax attacks in the United States illustrated that inhalational anthrax can be rapidly fatal.21,38,43
In the initial stage of B. anthracis infection, the spores germinate into vegetative cells. The capsule and 2 exotoxins, lethal toxin and edema toxin, secreted from these bacteria are primarily responsible for the symptoms and pathogenesis of anthrax.36,39 Lethal toxin and edema toxin each possess a unique enzymatic active domain—lethal factor and edema factor, respectively—but share a nontoxic cell binding domain known as protective antigen (PA). After the binding of PA to a cellular receptor, PA mediates translocation of lethal and edema factor into the cytosol of host cells. Lethal factor, a zinc metalloprotease, inhibits the intracellular mitogen-activated protease signaling pathway, thereby interfering with numerous biological processes and resulting in the majority of tissue damage.6,10,28,35,36 Edema factor, a calmodulin-dependent adenylyl cyclase, elevates levels of the intracellular second messenger cAMP and induces edema.3,28,35 Ultimately, disease progression leads to vascular injury, with edema, hemorrhage, thrombosis, and shock resulting in death.30,36,47 The central role of PA in anthrax pathogenesis makes this protein a logical target for vaccines and therapeutics6,34 as well as a potential diagnostic tool,24,39 although other diagnostic biomarkers may be used also.39,41
Gaps in our healthcare system were revealed as a direct consequence of the 2001 anthrax attacks, precipitating renewed interest in the development of rapid diagnostic assays and for identifying effective therapeutics strategies against symptomatic anthrax in nonvaccinated persons.4,6,39 Indeed, rapid diagnosis proved to be critical for the successful treatment and survival of victims of the 2001 attacks.19,39 However, early, accurate diagnosis is complicated by nonspecific clinical signs and the lack of a specific biomarker. In addition, anthrax traditionally has been diagnosed through classic 24-h culture and microscopy techniques, which may delay the initiation of treatment in affected persons or fail to distinguish who needs treatment in a timely manner. Therefore, reliable, simple, and fast anthrax diagnosis is needed for successful therapeutic intervention against this highly pathogenic disease.19,38,43,49
Well-characterized animal models are essential for the development of therapeutics directed against anthrax. Rabbits are sensitive to challenge with B. anthracis and, although the disease progresses more rapidly in rabbits than in humans, anthrax-induced pathologic changes are similar in both.13,14,28,37 Moreover, rabbits are predictive of the outcome of inhalational anthrax in nonhuman primates.26,50 Although rabbits are an established animal model for vaccine and postexposure prophylaxis studies against inhalational anthrax,13,26 a detailed natural history study for New Zealand white rabbits exposed to aerosolized B. anthracis is lacking and would be key for successful development of therapeutic intervention after the onset of inhalational anthrax.
In the present investigation, we developed and characterized a natural history study for New Zealand white rabbits exposed to aerosolized B. anthracis to better identify early biomarkers of inhalational anthrax. After anthrax spore exposure, rabbits were monitored for clinical signs and physiologic endpoints, including pyrexia, hematology features, bacteremia, and the presence of PA in the blood (that is, antigenemia). Similar to the African green monkey model of inhalational anthrax,39 an electrochemiluminescence (ECL) immunoassay was used in the present study to determine antigenemia. Furthermore, intravenous treatment with the bactericidal, fluoroquinolone antibiotic levofloxacin significantly increased survival in rabbits affected by inhalational anthrax. Overall, our results identified antigenemia as a suitable early biomarker of infection and superior treatment ‘trigger,’ compared with bacteremia and pyrexia, allowing for timely therapeutic intervention against inhalational anthrax.
Materials and Methods
Animals.
Bordetella-free SPF male and female New Zealand white rabbits (2.2 to 3.5 kg) were acquired from Charles River Laboratories (Pointe-Claire, Quebec, Canada). Animals were housed in individual cages and were acclimated to a 12:12-h light:dark cycle in a temperature- and humidity-controlled, SPF environment. Rabbits were maintained according to facility standard operating procedures, with food and water provided ad libitum. All rabbits were acclimated to the facility for at least 7 d before surgical implantation of a venous access port (Solomon Scientific, San Antonio, TX) to facilitate frequent phlebotomy sampling. In addition, rabbits used in the natural history study were implanted with a radiotelemetry device (model TA10TA-D70; Data Sciences International, St Paul, MN) to measure body temperature. Before inclusion in any study, rabbits were allowed to recover from surgery for 1 wk and were determined to be clinically healthy.
Research was conducted in compliance with the Animal Welfare Act2 and other applicable federal statutes and regulations related to animals and experiments involving animals and conformed to the guidelines for humane treatment set by the Guide for the Care and Use of Laboratory Animals.20 The United States Army Medical Research Institute of Infectious Disease facility is fully AAALAC-accredited. All research was conducted under approved protocols by the Institutional Animal Care and Use Committee at the United States Army Medical Research Institute of Infectious Disease.
Telemetry data analysis.
Body temperature was recorded every 15 min by radiotelemetry (DataQuest A.R.T.3.1 system, Data System International, Overland Park, KS). To establish the temperature baseline, data were collected at least 24 h before challenge with B. anthracis. Data collection continued until the animals succumbed or were euthanized. Pyrexia was defined as a body temperature above 40 °C for at least 3 sequential time points.1,40,45
Spore preparation.
As described previously,39 in a Biologic Safety Level 3 laboratory, B. anthracis (Ames strain) spores were produced in flask cultures containing Leighton and Doi medium.27 After centrifugation, the spore pellet was washed in sterile water and purified on gradients of 60% Hypaque-76 (GE Healthcare, Piscataway, NJ). Spores were stored in 1% phenol at 4 °C until use. Phenol was removed before aerosolization and spores were resuspended in sterile water and heat-shocked at 60 °C for 45 min.
Aerosol exposure.
Immediately before challenge, whole-body plethysmography (Buxco Research Systems, Wilmington, NC) was performed on each rabbit to determine respiratory capacity.26 Rabbits subsequently were challenged in a head-only chamber for approximately 10 min to an aerosol of B. anthracis spores created by a 3-jet collision nebulizer (BGI, Waltham, MA) and controlled by automated bioaerosol exposure system.16,26 The concentration of aerosolized B. anthracis in the chamber was determined through constant sampling by using an all-glass impinger (Ace Glass, Vineland, NJ) containing sterile water. Spore concentration was determined by plating on tryptic soy agar (Remel, Lenexa, KS). Rabbits were exposed to 150 times the median lethal dose (LD50; 1 LD50 = 105,000 cfu) of aerosolized B. anthracis spores, well above the aerosol LD99 for B. anthracis in rabbits.50 Aerosols mimic the route of infection expected for future bioterrorism attacks6,30,43 and result in diffuse bronchopneumonia.5,15 Aerosolized B. anthracis challenges occurred in a class III biological safety cabinet situated within an approved, restricted access Biological Safety Level 3 laboratory at the United States Army Medical Research Institute of Infectious Disease.
Natural history study.
Starting at 9 h after B. anthracis challenge and continuing at 3- or 6-h intervals thereafter, blood was collected by means of the vascular access port until either 96 h after exposure or the rabbit had succumbed to the disease or became moribund and was euthanized. Each blood sample was subdivided for CBC, bacteremia, and antigenemia analysis. Body temperature was monitored continuously and clinical observations made until B. anthracis-challenged rabbits succumbed or were euthanized.
Clinical observations.
After challenge, rabbits were observed and scored at least twice daily for changes in appearance (for example, coat condition, respiration, and body posture), natural behavior (for example, mobility, alertness, food intake, and vocalization), and provoked behavior (for example, response to handling). Each category was ranked on an ascending numerical order from 0 (normal) to 2 (listless, abdominal or open mouth breathing) for the appearance category; 0 (normal) to 3 (vocalization, decreased mobility and alertness) for natural behavior; and 0 (normal) to 3 (unresponsive when stimulated, weak, precomatose) for provoked behavior category. These categorical scores were summed to obtain the total clinical score. When a clinical score was 4 to 6, the frequency of daily observations increased to carefully monitor disease progression and animal welfare. Rabbits meeting the predetermined clinical score of 7 to 8 were deemed moribund and euthanized.
CBC.
Blood was collected in an EDTA-treated tube and processed on an AC-T diff hematology analyzer (Beckman Coulter, Fullerton, CA). Differential blood cell counts were done manually. CBC analysis included WBC, RBC, heterophils, lymphocytes, monocytes, platelets, hematocrit, and hemoglobin.
Bacteremia.
Whole-blood samples were collected in Wampole isolator microbial tubes (Inverness Medical, Princeton, NJ) and cultured on tryptic soy agar. Plates (in duplicate) were incubated for 18 to 24 h at 37 °C and evaluated for colonies at 24 h after sampling.
Antigenemia.
PA was determined qualitatively from whole blood by ECL immunoassay (Bioveris M-Series M1M System Analyzer; Bioveris, Gaithersburg, MD), as previously described.39 Three PA-specific monoclonal antibodies were used as a capture-antibody mix.11,29,39 All samples were analyzed in duplicate. Positive controls consisted of naïve rabbit whole blood spiked with PA (Critical Reagents Program, Aberdeen Proving Grounds Edgewood Area, Chesterton, MD), whereas negative matrix controls consisted of whole blood only. Samples were considered ECL positive, and thereby antigenemic, if the signal:noise ratio was ≥ 1.2 times the average of the negative matrix controls. The ECL limit of detection for PA-spiked whole blood was less than 2 ng/mL. Antigenemia results by ECL assay were determined within 1 h of blood collection.
Levofloxacin efficacy.
Starting 15 h after challenge with B. anthracis and continuing at 3-h intervals thereafter, blood was collected from the vascular access port until rabbits were determined to be antigenemic by ECL immunoassay or 30 h after exposure. Blood was collected every 24 h thereafter. Blood samples were subdivided for antigenemia and bacteremia analysis. After antigenemia determination, B. anthracis-challenged rabbits intravenously received either saline vehicle (control) or levofloxacin (total daily dose, 12.5 or 25 mg/kg; Ortho Pharmaceutical, Raritan, NJ). Vehicle or levofloxacin was administered twice daily, in half-total daily doses at 12-h intervals. Efficacy end-point was survival time, defined as the time from B. anthracis challenge to 28 d after challenge. Clinical observations were made at least twice daily until the rabbit succumbed to the disease or was euthanized.
Levofloxacin pharmacokinetics.
Sera were collected 5 min after levofloxacin treatment (first and third) and just before levofloxacin treatment (second and fourth) from B. anthracis-challenged rabbits to determine levofloxacin peak and trough levels, respectively. To facilitate serum sample removal for pharmacokinetic analysis from a Biologic Safety Level 3 laboratory, all samples were irradiated with 5 × 106 rads in a model 484R 60CO Irradiator (JL Shepherd and Associates, San Fernando, CA) to destroy B. anthracis spores and then a portion safety tested on tryptic soy agar plates. Irradiation did not degrade serum levofloxacin levels (data not shown). Serum levofloxacin levels were analyzed quantitatively by HPLC (1200 Series, Waldbronn, Germany). The fluorescence excitation and emission wavelengths were 296 and 498 nm, respectively. Samples were resolved on a phase column (4.6 × 150 mm, 3.5 µm; Zorbax Eclipse Plus C18, Agilent Technologies) equipped with an analytical guard column (4.6 × 12.5 mm, 5 µm; Zorbax Eclipse Plus C18, Agilent Technologies). The mobile phase was an 83:17 (v/v) mixture of 25 mM potassium phosphate buffer (with 1% triethyl amine, pH 3.0) and acetonitrile. All standards and samples were extracted using perchloric acid and then further diluted in mobile-phase buffer before HPLC analysis.
Statistical analysis.
Sigmaplot, version 11.0 (Systat Software, Chicago, IL) was used. Results are expressed as mean ± SEM. Data expressed as percentages were subject to arcsine square root transformations prior to analysis. Bacteremia load and ECL signal:noise values were correlated by using Spearman rank-order correlation. All other correlations were analyzed by using Pearson product-moment correlations. Data for single comparison were analyzed by Student t test. Multiple comparisons of homogeneous data were analyzed by one-way ANOVA, and group means were compared by using the Student Newman–Keuls post hoc test. Fisher exact tests with step-down Bonferroni adjustment for multiple comparisons were used to compare the survival rates in the levofloxacin-treated groups with those of the vehicle control group at day 28. Survival curves between these groups were analyzed by log-rank test with the Holm–Sidak method for multiple comparisons. The criterion for significance was P ≤ 0.05 for all comparisons.
Results
Natural history study of rabbits challenged with aerosolized B. anthracis.
New Zealand white rabbits (male = 6, female = 6) were challenged with 150 LD50 B. anthracis (Ames strain) spores. Rabbits were exposed to an actual presented dose of 155.6 ± 23.1 LD50, ranging from 51.1 to 313.8 LD50 for individual rabbits (Table 1). The mean survival time after B. anthracis exposure was 46.9 ± 3.3 h (range, 29 to 61 h). Postchallenge survival times did not differ between male and female rabbits. Moreover, no correlation was observed between the presented dose of B. anthracis spores and postchallenge survival time.
Table 1.
Disease course for rabbits challenged with aerosolized B. anthracis
| After challenge with B. anthracis |
|||||||||
| Rabbit no. | Sex | Weight (kg) | Dose (LD50) | Antigenemia (h) | Bacteremia (h) | Pyrexia (h) | Inversion of heterophil: lymphocyte ratio (h) | Survival after challenge (h) | Survival after antigenemia (h) |
| 1 | M | 3.0 | 183.0 | 27 | 27 | 32.75 | 33 | 43 | 16 |
| 2 | M | 3.0 | 313.8 | 21 | 27 | 27.75 | 27 | 35 | 14 |
| 3 | F | 3.0 | 237.7 | 27 | 27 | 30.0 | 33 | 37 | 10 |
| 4 | F | 3.0 | 51.1 | 21 | 21 | 26.0 | 27 | 29 | 8 |
| 5 | F | 3.0 | 189.0 | 21 | 21 | 26.25 | 33 | 46 | 25 |
| 6 | F | 3.0 | 88.5 | 27 | 27 | 30.25 | 33 | 35 | 8 |
| 7 | M | 2.2 | 70.8 | 30 | 27 | 31.75 | 44 | 56 | 26 |
| 8 | M | 2.4 | 73.7 | 30 | 24 | 29.0 | 30 | 57 | 27 |
| 9 | M | 3.1 | 110.0 | 24 | 15 | 25.5 | 18 | 46 | 22 |
| 10 | F | 3.0 | 171.0 | 30 | 30 | 30.5 | 21 | 61 | 31 |
| 11 | M | 3.0 | 226.6 | 15 | 15 | ND | ND | 57 | 45 |
| 12 | F | 3.2 | 151.9 | 21 | ND | ND | ND | 61 | 40 |
| Mean ± SEM | 155.6 ± 23.1 | 24.5 ± 1.4 | 23.1 ± 0.2 | 29.0 ± 0.8 | 29.9 ± 2.3 | 46.9 ± 3.3 | 22.7 ± 3.5 | ||
ND, not determined
The resultant pathology for rabbits succumbing to inhalational anthrax infection was similar to that described previously.50 All rabbits exhibited typical histopathologic lesions associated with inhalational anthrax. In particular, lungs, lymph nodes draining the lung, and spleen exhibited moderate to severe fibrinous inflammation and necrosis. In addition, marked congestion, edema, fibrin, and bacilli were present in the lamina propria and submucosa of the trachea.
Development of antigenemia and bacteremia in B. anthracis-challenged rabbits.
Both antigenemia and bacteremia developed before the occurrence of pyrexia and inversion of the heterophil:lymphocyte ratio (Table 1 and Figure 1). Heterophil:lymphocyte inversion is an indicator of infection.46 The presence of PA in rabbit blood (that is, antigenemia) was detected starting 24.5 ± 1.4 h (range, 15 to 30 h) after B. anthracis challenge. PA detection by ECL immunoassay was simple and reproducible,39 with results obtained within 1 h of blood collection. Similar to antigenemia, bacteremia developed between 15 and 30 h after B. anthracis challenge, for a mean occurrence time of 23.1 ± 0.2 h. However, bacteremia determination by culture was considerably more time-intensive than was antigenemia detection, with bacteremia results obtained within 18 to 24 h of blood collection. Qualitative ECL signal:noise values positively correlated with bacterial load (r = 0.923, P < 0.0000002). The ECL signal:noise level and bacterial load remained elevated until B. anthracis-challenged animals succumbed to inhalational anthrax (data not shown). Interestingly, neither the development of antigenemia nor bacteremia correlated with either the presented dose or postchallenge survival time. Although both antigenemia and bacteremia positively correlated with the occurrence of pyrexia (r = 0.757, P = 0.0112 and r = 0.806, P = 0.00866, respectively), only bacteremia correlated with inversion of the heterophil:lymphocyte ratio (r = 0.712, P = 0.0315). No sex-associated differences were observed in the development of antigenemia or bacteremia after challenge.
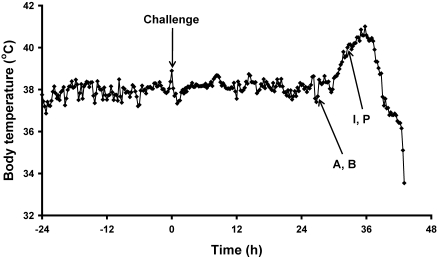
Figure 1.
Representative body temperature time course for a B. anthracis-challenged rabbit. Temperature data were collected by radiotelemetry 24 h before B. anthracis challenge and continued until the rabbit succumbed to inhalational anthrax. Both antigenemia (A) and bacteremia (B) preceded the occurrence of pyrexia (P) and heterophil:lymphocyte inversion (I). No temperature data were collected during actual aerosol challenge with B. anthracis.
Clinical observations and pyrexia in B. anthracis-challenged rabbits.
Clinical observations for B. anthracis-challenged rabbits were similar to those reported previously.50 After B. anthracis challenge, rabbits appeared clinically normal until shortly before succumbing to inhalational anthrax. At that time, moribund rabbits appeared lethargic and weak and exhibited respiratory distress (as characterized by abdominal and open-mouth breathing), sometimes accompanied by convulsions. However, no clear, consistent pattern in the overall clinical observations for B. anthracis-challenged rabbits could be elucidated as a predictor for infection or state of pathogenesis (data not shown).
Pyrexia developed in rabbits approximately 29 ± 0.8 h (range, 25 to 33 h) after B. anthracis challenge, consistently after the appearance of both antigenemia and bacteremia (Table 1 and Figure 1). After pyrexia, body temperature decreased (save for short-term reversals in some animals) until rabbits succumbed to inhalational anthrax or were euthanized. No correlation was observed between either development of pyrexia and the presented dose or postchallenge survival time.
Hematology in B. anthracis-challenged rabbits.
Lymphocyte levels exceeded that of heterophils before B. anthracis exposure (data not shown). After challenge, lymphocyte levels gradually decreased and heterophil levels increased. Heterophil:lymphocyte inversion (Table 1) for individual B. anthracis-challenged rabbits occurred between 18 and 44 h after challenge. The mean time of occurrence for heterophil:lymphocyte inversion was 29.9 ± 2.3 h, appearing at approximately the same time as pyrexia and consistently after the development of antigenemia and bacteremia (Table 1 and Figure 1). No correlation was observed between time of heterophil:lymphocyte inversion and the presented dose or postchallenge survival time.
No statistically significant differences were observed in WBC, RBC, monocytes, hemoglobin, hematocit, or platelet concentrations after challenge (data not shown). However, a trend (P = 0.077) toward an increase in WBC concentrations started 9 h after challenge and remained throughout. WBC levels for some individual B. anthracis-challenged rabbits at later time points exceeded the normal expected WBC range for New Zealand white rabbits.17,45 Conversely, a trend (P = 0.085) toward a decrease in monocytes was observed by 33 h after challenge. Overall, although occasional individual hematologic parameters were outside of the normal hematologic range for rabbits,17,45 the vast majority were not.
Therapeutic window for B. anthracis-challenged rabbits.
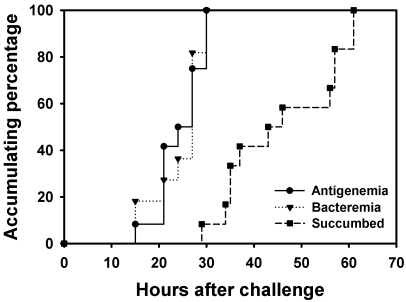
Given antigenemia as the biomarker of systemic infection for treatment initiation, postantigenemia survival time in B. anthracis-challenged rabbits was approximately 22.7 ± 3.5 h, ranging from 8 to 40 h after antigenemia (Table 1 and Figure 2). This result suggests a relatively narrow window of opportunity for treatment.
Figure 2.
Inhalational anthrax progression in rabbits challenged with aerosolized B. anthracis spores. The pattern for disease development was defined by the appearance of antigenemia and bacteremia, as well as rabbits succumbing to disease.
Therapeutic efficacy of intravenous levofloxacin in B. anthracis-challenged rabbits.
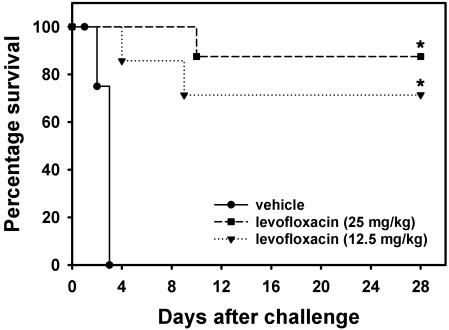
To evaluate New Zealand white rabbits as a therapeutic model, a levofloxacin efficacy study was conducted in rabbits challenged with 150 LD50 of aerosolized B. anthracis spores (Table 2). As seen in the natural history study, antigenemia and bacteremia occurred at similar times. Antigenemia determination was the trigger for treatment initiation, and animals were confirmed later as bacteremic at time of treatment. Levofloxacin was administered intravenously for 5 d at half total-daily dose every 12 h to accommodate the higher metabolic rate of rabbits compared with humans.23,31 B. anthracis-challenged rabbits treated with levofloxacin at either 25 or 12.5 mg/kg had significantly (P < 0.001) improved survival (87.5% and 71.4%, respectively) compared with that of vehicle-treated rabbits (0%) at study end at 28 d after challenge (Figure 3). Survival did not differ between the 2 levofloxacin-treated groups throughout the study. Although bacterial load was abrogated after the first day of levofloxacin treatment, the ECL signal:noise value remained elevated until the fourth day of treatment. By the final levofloxacin treatment, both bacteremia and antigenemia were absent in B. anthracis-challenged rabbits that survived to the study endpoint (data not shown). The peak levofloxacin level in rabbits given the 25-mg/kg dose exceeded that in humans given a 500-mg daily dose,23 whereas the peak level for rabbits that received 12.5 mg/kg was equivalent to that in humans. The trough concentration of the 25-mg/kg dose exceeded the levofloxacin minimal inhibitory concentration for the Ames strain of B. anthracis (that is, 0.12 µg/mL),23 but the 12.5 mg/kg daily dose was below the minimal inhibitory concentration (Table 2). All B. anthracis-challenged rabbits that succumbed prior to study end exhibited pathology consistent with inhalational anthrax infection.50 However, no significant pathological findings were observed in B. anthracis-challenged rabbits treated with levofloxacin that survived to the study end.
Table 2.
Levofloxacin efficacy against inhalational anthrax in rabbits
| After challenge with B. anthracis |
||||||||||
| Group ID | No. of rabbits | LD50 | Treatment | Antigenemia (h) | Bacteremia (h) | First peak levofloxacin concentration (µg/mL) | First trough levofloxacin concentration (µg/mL) | Second peak levofloxacin concentration (µg/mL) | Second trough levofloxacin concentration (µg/mL) | % Survival 28 d after challenge |
| Vehicle | 8 (4 male, 4 female) | 143.0 ± 19.3 | Saline | 23.6 ± 2.1 | 20.0 ± 2.0 | 0 | 0 | 0 | 0 | 0 |
| 25-Levofloxacin | 8 (5 male, 3 female) | 135.5 ± 23.6 | Levofloxacin (25 mg/kg) | 20.0 ± 1.2 | 12.03 ± 1.47 | 0.17 ± 0.046 | 10.00 ± 2.21 | 0.15 ± 0.025 | 87.5 | |
| 12.5-Levofloxacin | 7 (2 male, 5 female) | 101.3 ± 20.9 | Levofloxacin (12.5 mg/kg) | 18.9 ± 1.4 | 19.1 ± 1.4 | ND | 0.069 ± 0.018 | 5.33 ± 1.16 | 0.079 ± 0.011 | 71.4 |
ND, not determined
Figure 3.
Percentage survival for B. anthracis-challenged rabbits treated with vehicle or levofloxacin. Rabbits were challenged with approximately 150 LD50 of aerosolized B. anthracis spores. After antigenemia determination, animals were treated with either vehicle or levofloxacin (either 25 or 12.5 mg/kg) twice daily, at half total dose, for 5 d and survival monitored to the study end at 28 d after challenge. n = 7 or 8 per group (see Table 2). *, Significantly (P < 0.05) different from vehicle-treated B. anthracis-challenged rabbits.
Discussion
Diverse therapeutic models are crucial for the development of successful medical interventions against inhalational anthrax. A detailed natural history study of aerosolized B. anthracis (Ames strain) exposure in African green monkeys demonstrated the suitability of this animal model for therapeutic efficacy studies.39 Moreover, cynomolgus macaques were recently used in a raxibacumab (that is, anti-PA) efficacy study against inhalational anthrax.34 However because of their greater availability and ease of handling, species lower on the phylogenic scale than nonhuman primates are better suited for initial therapeutic efficacy studies.13,26 In the present work, a detailed study of the natural history of aerosolized B. anthracis (Ames strain) in New Zealand white rabbits was performed to characterize the disease and assess early biomarkers of infection. Disease progression studies have been conducted previously in rabbits, but those experiments differ from the present work in that intranasal exposure,24,25 Dutch belted dwarf rabbits,25 Vollum strain of B. anthracis,24 and different biomarkers were assessed.24,25
In the current study, the mean survival time for rabbits after challenge with B. anthracis (Table 1) was 46.9 ± 3.3 h, with the resultant pathology in each animal consistent with succumbing to inhalational anthrax. Survival time was similar to that in previous studies in which rabbits were exposed to a lethal dose of aerosolized Ames strain B. anthracis spores.34,50 Consistent with a previous report by Zaucha and colleages,50 no correlation was observed between the presented dose of aerosolized B. anthracis spores and postchallenge survival time (Table 1).
Antigenemia and bacteremia development preceded the occurrence of pyrexia and heterophil:lymphocyte inversion (Table 1) in rabbits challenged with aerosolized B. anthracis. Bacteremia is considered the ‘gold standard’ for diagnosis of systemic infection. However, recent studies involving inhalational anthrax have determined that the detection of PA is a comparable, reliable biomarker of systemic infection in rabbits and nonhuman primates.24,32,34,39 Bacterial load in the present study positively correlated with antigenemia, supporting the premise that antigenemia may be used as a surrogate for bacteremia to estimate severity of disease.24 Despite the development of bacteremia and antigenemia at relatively the same time after B. anthracis challenge, antigenemia determination by ECL immunoassay is considerably more rapid (that is, within approximately 1 h) than the traditional 18- to 24-h culture needed to determine bacteremia. ECL immunoassay therefore allows for timely, appropriate therapeutic intervention. Hence, antigenemia serves an early biomarker of systemic infection.
Rabbits appeared clinically normal until shortly before succumbing to inhalational anthrax. No clear, consistent pattern in the clinical observations arose that could be discerned as an early, reliable predictor for the onset of infection or the outcome. Difficulties in determining predictors based on observations after exposure to aerosolized B. anthracis have been noted in New Zealand white50 and Dutch-belted dwarf rabbits,25 rhesus macaques, and African green monkeys.39,48 Early diagnosis in humans is problematic due to the spectrum of nonspecific symptoms during the prodromal phase of inhalational anthrax.19
Both pyrexia and modest hematologic changes occurred during the course of B. anthracis infection (Table 1). Although development of pyrexia was inconsistent in African green monkeys challenged with aerosolized B. anthracis,39 similar to that observed in humans,18,22 pyrexia developed in all infected rabbits (Table 1 and Figure 1). However, pyrexia was not a suitable trigger for treatment initiation, because both antigenemia and bacteremia preceded development of pyrexia. In the present study, before and shortly after exposure of rabbits to aerosolized B. anthracis, lymphocytes predominated over heterophils. Lymphocyte levels decreased and heterophil levels increased as the disease progressed. Heterophil:lymphocyte inversion occurred at 29.9 ± 2.3 h postchallenge (Table 1), at about the time of development of pyrexia. Interestingly, WBC levels did not increase significantly during the course of infection, consistent with findings for B. anthracis-challenged African green monkeys39 but different from those of other inhalational anthrax studies involving cynomolgus macaques32 and Dutch belted rabbits.25 Because a trend toward an increase in WBC was observed throughout the infection, it cannot be excluded that a significant increase occurred between analyzed time points. Similar to results from a study with African green monkeys,39 no other significant hematologic changes in rabbits were apparent after B. anthracis challenge. Early biomarkers in human cases of inhalational anthrax have not been fully discerned as biomarkers and other clinical parameters have usually been determined after the onset of symptoms. However, as described in the current work, inhalational anthrax in rabbits is similar to human cases in that pyrexia develops along with increased numbers of heterophils (the equivalent to human neutrophils) and PA levels.19,21
A relatively narrow therapeutic window of opportunity (that is, 22.7 ± 3.5 h; Table 1 and Figure 2) exists between antigenemia development and death in rabbits with inhalational anthrax. This therapeutic window is generally within the time required for bacteremia culture, indicating that most B. anthracis-challenged rabbits would have succumbed to the disease before bacteremia-based treatment would be initiated. Because treatment effectiveness is based on rapid diagnosis (as with the ECL immunoassay), time-intensive or complex diagnostic assays (such as, bacteremia culture and PCR analysis of PA levels) may be better suited for confirmation of B. anthracis than to indicate treatment initiation.24,30
To verify New Zealand white rabbits as an appropriate therapeutic animal model for aerosolized B. anthracis, antigenemic rabbits were treated intravenously with levofloxacin (Table 2). All rabbits were confirmed to be bacteremic at the time of initial treatment, thereby verifying the therapeutic model. Levofloxacin is a fluoroquinolone that has a minimal inhibitory concentration similar to that for ciprofloxacin when tested against B. anthracis isolates8,23 and has been approved by the US Food and Drug Administration for inhalational anthrax postexposure prophylaxis in adults.9,12,44 In the present study, intravenous levofloxacin was administered at a ‘humanized dose’ (that is, half total-daily dose every 12 h) to accommodate the higher metabolic rate of rabbits to generate a pharmacokinetic profile similar to that in humans.23,31 This levofloxacin dosing regimen (25 or 12.5 mg/kg) proved to be therapeutically efficacious against aerosolized B. anthracis-challenged rabbits, eliminating bacterial load after the first treatment day. Survival in levofloxacin-treated animals was significantly higher throughout the study and at study end than in vehicle-treated rabbits challenged with B. anthracis (Figure 3). The peak for the 25-mg/kg dose proved to be higher than the peak concentration for levofloxacin in humans given a 500-mg daily dose (11 µg/mL compared with 5.7 µg/mL, respectively). However, trough concentrations for the 25-mg/kg dose were greater than the minimal inhibitory concentration for levofloxacin (that is, 0.12 µg/mL) but approximately 3-fold below that in humans given a 500-mg daily levofloxacin dose (that is, 0.5 µg/mL).23 When a 12.5-mg/kg dose of levofloxacin was administered to B. anthracis-challenged rabbits, peak levels were equivalent to that for a 500-mg daily dose in humans, whereas trough concentration was half of the minimal inhibitory concentration for levofloxacin and approximately 10-fold less than the levofloxacin dose in humans. Overall, intravenous levofloxacin administered at the time of antigenemia was effective in preventing morbidity and mortality from inhalational anthrax in rabbits. Early treatment initiation may be essential to therapeutic effectiveness, as decreased survival was associated with increasing treatment delay after antigenemia in an oral levofloxacin treatment model for aerosolized B. anthracis-exposed New Zealand white rabbits.33 Further optimization of the intravenous levofloxacin dosing regimen, as well as comprehensive pharmacokinetic analysis, are needed to better evaluate the therapeutic efficacy of this antimicrobial for its intended use in humans as a treatment for inhalational anthrax.
In summary, the present study provides a comprehensive natural history study of aerosolized Ames strain B. anthracis exposure in New Zealand white rabbits. Antigenemia is a viable, early biomarker for systemic B. anthracis infection that can be used as a treatment trigger to allow for timely therapeutic intervention against this highly pathogenic disease. This study demonstrates the potential of New Zealand white rabbits as a therapeutic model for the testing of pharmaceuticals against inhalational anthrax.
Acknowledgments
This research was sponsored through an interagency agreement between the National Institute of Allergy and Infectious Diseases, Bethesda (Y1-AI-6129-04) and USAMRIID (A 120-B-10.3). The views, opinions, and/or findings contained herein are those of the authors, and should not be construed as an official Department of Army position, policy, or decision unless so designated by other documentation. The authors do not have a commercial or other association that would pose a conflict of interest.
The authors are grateful to the staff of the Center for Aerobiological Sciences (USAMRIID) for providing aerosol challenge expertise. The authors also thank Joshua Moore and the Veterinary Medicine (USAMRIID) technicians for expert animal care and veterinary assistance. Finally, the authors are grateful to Sarah Norris of the Research Support Division (USAMRIID) for statistical advice and to MAJ Carl Shaia, DACVP (USAMRIID), LTC Thomas Steinbach, DACVP (Walter Reed Army Institute of Research), and the Pathology Division (USAMRIID) for expert pathology.
References
- 1.Anderson IE, Buxton D, Campbell I, Russell G, Davis WC, Hamilton MJ, Haig DM. 2007. Immunohistochemical study of experimental malignant catarrhal fever in rabbits. J Comp Pathol 136:156–166 [DOI] [PubMed] [Google Scholar]
- 2.Animal Welfare Act as Amended. 2007. 7 USC §2131-2159.
- 3.Arora N, Leppla SH. 1993. Residues 1–254 anthrax lethal factor are sufficient to cause cellular uptake of fused polypeptides. J Biol Chem 268:3334–3341 [PubMed] [Google Scholar]
- 4.Baillie LW. 2006. Past, imminent, and future human medical countermeasures for anthrax. J Appl Microbiol 101:594–606 [DOI] [PubMed] [Google Scholar]
- 5.Bakker-Woudenberg IAJM. 2003. Experimental model of pulmonary infection. J Microbiol Methods 54:295–313 [DOI] [PubMed] [Google Scholar]
- 6.Bouzianas DG. 2007. Potential biological targets of Bacillus anthracis in antiinfective approaches against the threat of bioterrorism. Expert Rev Anti Infect Ther 5:665–684 [DOI] [PubMed] [Google Scholar]
- 7.Brachman PS. 1980. Inhalation anthrax. Ann N Y Acad Sci 353:83–93 [DOI] [PubMed] [Google Scholar]
- 8.Cavallo JD, Ramisse F, Giradet M, Vassaire J, Mock M, Hernandez E. 2002. Antibiotic susceptibilities of 96 isolates of Bacillus anthracis in France between 1994 and 2000. Antimicrob Agents Chemother 46:2307–2309 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Deziel MR, Heine H, Louie A, Kao M, Byrne WR, Basset J, Miller L, Bush K, Kelly M, Drusano GL. 2005. Effective antimicrobial regimens for use in humans for therapy of Bacillus anthracis infections and postexposure prophylaxis. Antimicrob Agents Chemother 49:5099–5106 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Duesbery NS, Webb CP, Leppla SH, Gordon VM, Klimpel KR, Copeland TD, Ahn NG, Oskarsson MK, Fukasawa K, Paull KD, Vande Woude GF. 1998. Proteolytic inactivation of MAP kinase–kinase by anthrax lethal factor. Science 280:734–737 [DOI] [PubMed] [Google Scholar]
- 11.Ezzell JW, Abshire TG, Brown C. 1990. Analysis of Bacillus anthracis vegetative cell surface antigens and of serum protease cleavage of protective antigen, p 43–33. : Proceedings of the International Workshop on Anthrax. Wiltshire (UK): Salisbury Printing [Google Scholar]
- 12.Fish DN. 2003. Levofloxacin: update and perspectives on one of the original ‘respiratory quinones.’ Expert Rev Anti Infect Ther 1:371–387 [DOI] [PubMed] [Google Scholar]
- 13.Goossens PL. 2009. Animal models of human anthrax: the quest for the Holy Grail. Mol Aspects Med 30:467–480 [DOI] [PubMed] [Google Scholar]
- 14.Grinberg LM, Abramova FA, Yampolskaya OV, Walker DH, Smith JH. 2001. Quantitative pathology of inhalational anthrax I: quantitative microscopic findings. Mol Pathol 14:482–495 [DOI] [PubMed] [Google Scholar]
- 15.Halperin SA, Heifetz SA, Kasina A. 1988. Experimental respiratory infection with Bordetella pertusis in mice: comparison of two methods. Clin Invest Med 11:297–303 [PubMed] [Google Scholar]
- 16.Hartings JM, Roy CJ. 2004. The automated bioaerosol exposure system: preclinical development and a respiratory dosimetry application with nonhuman primates. J Pharmacol Toxicol Methods 49:39–55 [DOI] [PubMed] [Google Scholar]
- 17.Hewitt CD, Innes DJ, Savory J, Willis MR. 1989. Normal biochemical and hematological values in New Zealand white rabbits. Clin Chem 35:1777–1779 [PubMed] [Google Scholar]
- 18.Holty JE, Bravata DM, Liu H, Olshen RA, McDonald KM, Owens DK. 2006. Systematic review: a century of inhalational anthrax cases from 1900 to 2005. Ann Intern Med 144:270–280 [DOI] [PubMed] [Google Scholar]
- 19.Inglesby TV, O'Toole T, Henderson DA, Bartlett JG, Ascher MS, Eitzen E, Friedlander AM, Gerberding J, Hauer J, Hughes J, McDade J, Osterholm MT, Parker G, Perl TM, Russell PK, Tonat K. 2002. Anthrax as a biological weapon, 2002: updated recommendations for management. J Am Med Assoc 287:2236–2252 [DOI] [PubMed] [Google Scholar]
- 20.Institute for Laboratory Animal Research 1996. Guide for the care and use of laboratory animals. Washington (DC): National Academies Press; [PubMed] [Google Scholar]
- 21.Jernigan DB, Raghunathan PL, Bell BP, Brechner R, Bresnitz EA, Butler JC, Cetron M, Cohen M, Doyle T, Fischer M, Greene C, Griffith KS, Guarner J, Hadler JL, Hayslett JA, Meyer R, Petersen LR, Phillips M, Pinner R, Popovic T, Quinn CP, Reefhius J, Reissman D, Rosenstein N, Schuchat A, Sheih WJ, Siegal L, Swerdlow DL, Tenover FC, Traeger M, Ward JW, Weisfuse I, Yeskey K, Zachi S, Ashford DA, Perkins BA, Ostroff S, Hughes J, Fleming D, Koplan JP, Gerberding JL; National Anthrax Epidemiology Investigation Team 2002. Investigation of bioterrorism-related anthrax, United States, 2001: epidemiological findings. Emerg Infect Dis 8:1019–1028 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Jernigan JA, Stephens DS, Ashford DA, Omencaca C, Topiel MS, Galbraith M, Tapper M, Fisk TL, Zaki S, Popovic T, Meyer RF, Quinn CP, Harper SA, Fridkin SK, Sejvar JJ, Shepard CW, McConnell M, Guarner J, Shieh WJ, Malecki JM, Gerberding JL, Hughes JM, Perkins BA; Anthrax Bioterrorism Investigation Team 2001. Bioterrorism-related inhalational anthrax: the first 10 cases reported in the United States. Emerg Infect Dis 7:933–944 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kao LM, Bush K, Barnewall R, Thalacker FW, Olson PH, Drusano GL, Minton N, Chien S, Hemeryck A, Kelley MF. 2006. Pharmacokinetic considerations and efficacy of levofloxacin in an inhalational anthrax (postexposure) rhesus monkey model. Antimicrob Agents Chemother 50:3535–3542 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kobiler D, Weiss S, Levy H, Fisher M, Mechaly A, Pass A, Zeev A. 2006. Protective antigen as a correlative marker for anthrax in animal models. Infect Immun 74:5871–5876 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Lawrence WS, Hardcastle JM, Brining DL, Weaver LE, Ponce C, Whorton EB, Peterson JW. 2009. The physiologic response of Dutch belted rabbits infected with inhalational anthrax. Comp Med 59:257–265 [PMC free article] [PubMed] [Google Scholar]
- 26.Leffel EK, Pitt LM. 2006. Anthrax, p 77–94. : Swearengen JR. Biodefense: research methodology and animal models. Boca Raton (FL): CRC Press [Google Scholar]
- 27.Leighton TJ, Doi RH. 1971. The stability of messenger ribonucleic acid during sporulation in Bacillus subtilis. J Biol Chem 246:3189–3195 [PubMed] [Google Scholar]
- 28.Little SF, Ivins BE. 1999. Molecular pathogenesis of Bacillus anthracis infection. Microbes Infect 1:131–139 [DOI] [PubMed] [Google Scholar]
- 29.Little SF, Leppla SH, Cora E. 1988. Production and characterization of monoclonal antibodies to the protective antigen component of Bacillus anthracis toxin. Infect Immun 56:1807–1813 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Loving CL, Kennett M, Lee GM, Grippe VK, Merkel TJ. 2007. Murine aerosol challenge model of anthrax. Infect Immun 75:2689–2698 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.McDuffie RS, Jr, Eskens JL, Gibbs RS. 1998. Oral quinolone in the treatment of experimental polymicrobial puerperal infection in rabbits. Obstet Gynecol 92:28–30 [PubMed] [Google Scholar]
- 32.Meister G, Simmons A, Schmidt J, Herr-Calomeni P, Stark G, Lubert E, Clement K, Sivko G, Mott J. 2009 Development of an inhalational B. anthracis exposure therapeutic model in cynomolgous macaques, abstract 132(D), p 84. Bacillus–ACT 2009, 30 Aug–3 Sep 2009, Sante Fe, NM. [Google Scholar]
- 33.Meister GT, Henning LN, McGuiness EE, Olson PH, Edwards M, Sivko GS, Mott JM. 2010. Assessing the efficacy of combination therapy following exposure to Bacillus anthracis in NZW rabbits, abstract 097(G). Eighth ASM Biodefense and Emerging Disease Research Meeting, 21–24 Feb 2010, Baltimore, MD [Google Scholar]
- 34.Migone TS, Subramanian GM, Zhong J, Healey LM, Corey A, Devalaraja M, Lo L, Ullrich S, Zimmerman J, Chen A, Lewis M, Meister G, Gillum K, Sanford D, Mott J, Bolmer SM. 2009. Raxibacumab for the treatment of inhalational anthrax. N Engl J Med 361:135–144 [DOI] [PubMed] [Google Scholar]
- 35.Mourez M. 2004. Anthrax toxins. Rev Physiol Biochem Pharmacol 152:135–164 [DOI] [PubMed] [Google Scholar]
- 36.Passalacqua KD, Bergman NH. 2006. Bacillus anthracis: interactions with the host and establishment of inhalational anthrax. Future Microbiol 1:397–415 [DOI] [PubMed] [Google Scholar]
- 37.Phipps AJ, Premanandan C, Barnewall RE, Lairmore MD. 2004. Rabbits and nonhuman primate models of toxin-targeting human anthrax vaccines. Microbiol Mol Biol Rev 68:617–629 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Purcell BK, Worsham PL, Friedlander AM. 2007. Anthrax, p 69–90. : Dembek ZF. Medical aspects of biological warfare. Washington (DC): Borden Institute [Google Scholar]
- 39.Rossi CA, Ulrich M, Norris S, Reed DS, Pitt LM, Leffel EK. 2008. Identification of a surrogate marker for infection in the African green monkey model of inhalation anthrax. Infect Immun 76:5790–5801 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Sande MA, Sande ER, Woolwine JD, Hackbarth CJ, Small PM. 1987. The influence of fever on the development of experimental Streptococcus pneumoniae meningitis. J Infect Dis 156:849–850 [DOI] [PubMed] [Google Scholar]
- 41.Sela-Abramovich S, Chitlaru T, Gat O, Grosfeld H, Cohen O, Shafferman A. 2009. Novel and unique diagnostic biomarkers for Bacillus anthracis infection. Appl Environ Microbiol 75:6157–6167 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Sloat BR, Cui Z. 2006. Strong mucosal and systemic immunities induced by nasal immunization with anthrax protective antigen protein incorporated in liposome–protamine–DNA particles. Pharm Res 23:262–269 [DOI] [PubMed] [Google Scholar]
- 43.Spencer RC. 2003. Bacillus anthracis. J Clin Pathol 56:182–187 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Stern EJ, Uhde KB, Shadomy SV, Messonnier N. 2008. Conference report on public health and clinical guidelines for anthrax. Emerg Infect Dis 14:pii:07–0969 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Suckow MA, Brammer DW, Rush HG, Chrisp CE. 2002. Biology and diseases of rabbits. : Fox JG, Anderson LC, Loew FM, Quimby FW. Laboratory animal medicine, 2nd ed. London (UK): Academic Press [Google Scholar]
- 46.Toth LA, Krueger JM. 1989. Hematologic effects of exposure to three infective agents in rabbits. J Am Vet Med Assoc 195:981–986 [PubMed] [Google Scholar]
- 47.Tournier JN, Quesnel-Hellman A, Cleret A, Vidal DR. 2007. Contributions of toxins to the pathogenesis of inhalational anthrax. Cell Microbiol 9:555–565 [DOI] [PubMed] [Google Scholar]
- 48.Twenhafel NA, Leffel E, Pitt ML. 2007. Pathology of inhalational anthrax infection in the African green monkey. Vet Pathol 44:716–721 [DOI] [PubMed] [Google Scholar]
- 49.Walsh JJ, Pesik N, Quinn CP, Urdaneta V, Dykewicz CA, Boyer AE, Guarner J, Wilkins P, Norville KJ, Barr JR, Zaki SR, Patel JB, Reagan SP, Pirkle JL, Treadwell TA, Messonnier NR, Rotz LD, Meyer RF, Stephens DS. 2007. A case of naturally acquired inhalation anthrax: clinical care and analyses of anti-protective antigen immunoglobulin G and Lethal factor. Clin Infect Dis 44:968–971 [DOI] [PubMed] [Google Scholar]
- 50.Zaucha GM, Pitt MLM, Estep J, Ivins BE, Friedlander AM. 1998. The pathology of experimental anthrax in rabbits exposed by inhalation and subcutaneous inoculation. Arch Pathol Lab Med 122:982–992 [PubMed] [Google Scholar]