Abstract
This study examined whether deficits in dealing with daily problems emerge before a depressive episode (i.e., pre-existing vulnerability) or after a depressive episode (i.e., psychosocial scar). Participants completed a 30-day daily diary in which they reported their most negative event of the day, their appraisals of that event, and their mood. Three years later, they completed a structured depression interview. The sample consisted of 350 college students, 24 of whom had a past history of depression and 54 of whom experienced a depressive episode subsequent to dairy completion. Multilevel modeling revealed that students with past depression blamed others more than the never-depressed and those with subsequent depression, which supported the scar hypothesis. In support of the vulnerability hypothesis, as compared to the never-depressed group, participants with past depression demonstrated steeper declines in positive mood on more stressful days but did not significantly differ from the subsequent depression group. Overall, our findings do not provide clear support for either hypothesis; however, this study is the first to use a daily diary design to directly compare individuals with past depression to individuals who would subsequently experience depression.
Daily stressors have been linked to increases in negative mood (Bolger, DeLongis, Kessler, & Schilling, 1989), physical illness (Stone, Reed, & Neale, 1987), and relationship problems (Bodenmann, Pihet, & Kayser, 2006). Moreover, ample research has examined how various personality factors, such as neuroticism, are related to differential exposure and reactivity to daily stressors (e.g., Bolger & Zuckerman, 1995). We know little, however, about whether individuals who have a history of depression, or who are vulnerable to depression, appraise, cope with, and react to stressors in ways that distinguish them from their more resilient peers. In the present study we examined the experience of daily stressful encounters among young adults who have a history of depression, those who are vulnerable to depression (by virtue of experiencing a subsequent depressive episode), and a group of never depressed individuals.
Evidence suggests that a history of major depression affects outcomes in diverse areas. For example, formerly depressed women show an increased risk for coronary heart disease due to a dysfunction in the blood vessels that is not evident among their never depressed counterparts (Wagner, Tennen, Mansoor, & Abott, 2006). Intervention efficacy is also related to history of depression, as Zautra et al. (2008) found that treatment outcomes for adapting to rheumatoid arthritis depended on whether patients had a history of recurrent depression. Further, as compared to people who were never depressed, dysfunctional attitudes and negative attribution styles are elevated after remission from a major depressive episode (Eaves & Rush, 1984; Haeffel et al., 2005). As illustrated here, the effects of a major depressive episode are far-reaching and present even when depressive episodes occurred and resolved years before (e.g., Fifield, Tennen, Reisine, & McQuillan, 1998).
Investigators have recently begun to investigate vulnerability conferred by history of depression using micro-longitudinal research designs – such designs allow for a better understanding of the day to day unfolding of the stress and coping process. For example, Tennen, Affleck, and Zautra (2006) found that fibromyalgia (FM) patients with a history of depression vented emotions more and experienced lower levels of pain coping efficacy on days with increased pain as compared to FM patients who had never been depressed. They also found that mood became less positive on more painful days among patients who had a history of depression and elevated levels of current depressive symptoms, a pattern that was not evidenced among those without a history of depression. The latter findings are consistent with the priming model, also known as the interaction model, which suggests that depressive vulnerability remains latent until it is triggered or primed by a state of elevated distress (Roberts & Kassel, 1996; Tennen et al., 2006). Conner et al. (2006) found a similar pattern among individuals with rheumatoid arthritis.
We are aware of no research that has examined the role of history of depression in the experience of daily negative events or stressors. However, several studies have examined the association between current depressive symptoms and daily negative event exposure, appraisal and reactivity. Gunthert, Cohen, and Armeli (2002) found that individuals with elevated current depressive symptoms reported low levels of coping efficacy, and coping strategies were particularly ineffective in relieving distress when dealing with negative daily events. Also, similar to the pain and mood relationships in studies of history of depression, current depressive symptoms moderated the relationship between stressfulness ratings of daily negative events and positive affect. Gunthert, Cohen, Butler, and Beck (2007) found that among clinic outpatients high in current depressive symptoms, as compared to those low in current symptoms, negative thoughts and negative mood increased to a greater degree on days following a stressful interpersonal encounter as compared to days following a non-interpersonal stressor. Myin-Germeys et al. (2003) found that people with major depressive disorder showed greater increases in negative mood in response to daily stress than did their non-depressed counterparts.
These studies suggest that both mood and appraisals of negative events are affected by current depression status. This is supported by the broader depression literature, which indicates that depressed individuals maintain a negative evaluation bias (Haaga & Beck, 1992) and that depression is characterized by lack of self-efficacy and control, pessimism, hopelessness and maladaptive patterns of blame and coping (Abramson, Metalsky, & Alloy, 1989; Beck, Rush, Shaw, & Emery, 1979). It is unclear, however, whether previously depressed people or those who would experience a depressive episode during the next several years react to negative events less effectively, and whether current levels of depressive symptoms contribute to their stress-related responses.
Although previous research has shown that individuals with prior depression have some deficits when dealing with daily problems (Conner et al., 2006; Tennen et al., 2006), we do not know whether these deficits emerge before or after the depressive episode. Two competing models have been posited to explain deficits among people with a history of depression. The “scar hypothesis” suggests that a depressive episode leaves lasting changes in personality and self-concept that lead a person to be more vulnerable to future mood disturbance (Rohde, Lewinsohn, & Seely, 1990; Zautra et al., 2007). Based on this model one would not anticipate high levels of stress reactivity prior to the experience of the first depressive episode; increased stress reactivity should only occur after the first depressive episode. On the other hand, a vulnerability or “trait marker” hypothesis posits that formerly depressed individuals have preexisting characteristics that make them vulnerable to depression and that persist beyond remission from the depressive episode (Rohde et al., 1990; Tennen et al., 2006). According to this model, increased stress reactivity would be expected both prior to and after experiencing a depressive episode. Distinguishing between the two hypotheses is important in order to refine etiological models of depression and design effective treatment programs that aim to prevent future episodes of depression (Rohde et al., 1990).
There is mixed support in the literature regarding these two hypotheses. For example, in a longitudinal, prospective study, Rohde et al. (1990) found support for the scar hypothesis because individuals viewed themselves as less socially skilled after, but not prior to a depressive episode. Similarly, Rohde, Lewsinsohn, and Seeley (1994) reported that a variety “psychosocial scars” (e.g., depressive symptoms, anxiety, emotional reliance on others) were evident among adolescents recovered from a major depressive episode. However, Rohde et al. (1990) also found that participants who became depressed during their study rated their health as poorer than non-depressed controls both before and after the episode, supporting the vulnerability hypothesis. Beevers, Rohde, Stice, and Nolen-Hoeksema (2007) found additional support for the vulnerability hypothesis in their prospective study of female adolescents. They found that the negative effects of a major depressive episode did not persist on a variety of psychological and social outcomes after recovery from that episode as the scar hypothesis would suggest; instead, many factors were elevated both before and after depression onset. Finally, while a recent review found more consistent support for the vulnerability hypothesis, some studies did support the scar hypothesis (Christensen & Kessing, 2006). However, this review focused exclusively on personality traits (e.g., whether personality was altered by a depressive episode), rather than psychosocial functioning.
Importantly, to our knowledge, no study focusing on the daily stress process using a daily process design has compared these models. Although the rigorous prospective studies in this area have made important contributions to our understanding of the psychosocial deficits associated with a history of depression and depression vulnerability, daily process designs can capture deficits as they play out in the context of daily functioning, and in relation to day-to-day changes in life encounters. Psychosocial scars and vulnerability deficits may be difficult to detect in traditional longitudinal or cross-sectional studies if they are manifested only during periods of elevated stress (Rohde et al., 1990); daily studies may be more sensitive to detecting the interplay between current depressive symptoms, elevated daily stressors, and history of depression status.
The Current Study
We combined the virtues of daily process methods and a longer-term longitudinal study design to distinguish between the scar and vulnerability hypotheses. Specifically, a cohort of young adults completed an initial baseline survey and an electronic daily diary each day for 30 days. We then measured history of depression status three years after the baseline and diary assessment. In this way we were able to distinguish participants who had experienced a depressive episode prior to their participation in the study, those who became depressed for the first time subsequent to completing the diary, and those who had never experienced a depressive episode.
The diary portion of the study focused on two aspects of the daily stress process: negative event appraisals (perceived threat, appraised control, coping efficacy, other-blame attributions1) and mood. Negative event appraisals and negative mood have been linked to psychological and biological strain, increased risk of mental and physical health problems, and compromised academic performance (Felsten, 2002; Hojat, Gonnella, Erdmann, & Vogel, 2003; Lazarus & Folkman, 1984).
In line with previous research on history of depression and daily functioning (e.g., Conner et al., 2006), we anticipated that formerly depressed individuals, as compared to those without a history of depression, would report more daily event stress, less event control, less event coping efficacy, more event threat, and more negative mood. We also predicted that on days appraised as more stressful, participants with a history of depression, compared to their never depressed peers, would show greater elevations in negative mood, event threat, and other-blame, as well as greater decreases in event control and event coping efficacy.
Further, in our comparison of formerly depressed versus subsequently depressed participants, the scar hypothesis would be supported if formerly depressed participants showed a more maladaptive pattern of event attributions and mood than subsequently depressed participants. More specifically, the scar hypothesis would predict that participants who had been depressed prior to beginning the diary study, compared to those who became depressed subsequent to their study participation, would show greater deficits in mood and appraisals and would display more pronounced within-person changes in daily mood and appraisals when experiencing greater negative event stress. On the other hand, the vulnerability hypothesis would receive support if participants with past depression and those with subsequent depression show similar patterns of event appraisals and mood on average and when experiencing increased negative event stress. It should be noted that for either hypothesis to be fully supported, never depressed participants should exhibit more adaptive patterns of functioning than individuals with a past history of depression. In tests of each of these questions, we also examined the priming hypothesis by determining whether history of depression status interacted with current depressive symptoms to predict average levels of the daily variables and within-person relations between daily stress and the other daily variables (see Conner et al., 2006 and Tennen et al., 2006).
Method
Participants and Procedure
Participants were recruited from an introductory psychology participant subject pool to take part in a study of daily experience and health-related behaviors. Introductory psychology is a core university course that is the most heavily subscribed (non-required) course at the University. Over 3000 students of diverse majors enroll in this course every academic year. The subject pool participants during recruitment for this study were similar to the overall student body in SAT scores (1167 vs. 1168 campus-wide) and ethnic make-up (14% minority [non Caucasian] vs. 17% campus-wide).
Participants first attended an information session where they provided consent and were given instructions on how to complete an Internet-based initial assessment and daily survey. Within a week of the information session, students completed an initial baseline assessment which included demographic, personality and health measures by logging onto a secure website. Approximately two weeks after completing the initial assessment, participants began the daily diary procedure. They used a secure website to complete a daily survey between 2:30pm and 7:00pm for 30 days which took about 5-minutes. To improve compliance with the daily surveys, participants received daily e-mail reminders. At the end of the 30 days, participants attended an exit session, received compensation, and agreed to be contacted for a future follow-up interview. Participants received course credit and monetary compensation for participation. Approximately three years later, they were contacted via phone or e-mail and invited to participate in the depression phone interview portion of the study. There were separate consent and reimbursement procedures for this portion of the study
Of the 574 participants who enrolled in the larger study, 447 (78%) completed the structured diagnostic interview for depression three years after completing the 30-day electronic diary. Of the 447 participants who completed the diagnostic interview, 17 were excluded because it was determined that they were depressed at the time they completed the diary portion of the study, and 4 were excluded because they reported a depressive episode both prior to the diary and during the subsequent 3 years. Finally, participants (n = 76) were excluded if they completed less than 15 days of the diary data, or had incomplete data from the initial assessment2. This resulted in a final sample of 350 (156 men; 194 women). Participants were mostly White (89%), and at the start of the study were mainly freshmen (59%) with a mean age of 18.65 (SD = .86). The three hundred-fifty participants provided 8869 days of data of out a possible 10,500 daily surveys, which is a compliance rate of 84%.
Measures
Initial assessment
In addition to demographic questions, participants completed the 13-item short form of the Beck Depression Inventory (BDI; Beck & Beck, 1972) to measure current depressive symptoms. BDI scores were summed (α = .83) and ranged from 0 – 20 (M = 4.5, SD = 4.05). Neuroticism was also assessed and served as a control variable, as past research shows that neuroticism is related to depression and stressor appraisals, coping and reactivity (Bolger & Shilling, 1991; Tennen et al., 2006). Neuroticism was measured using the 12-item Neuroticism subscale of the NEO five-factor inventory (Costa & McCrae, 1992). Participants rated the extent to which they agreed with statements measuring neurotic tendencies (e.g., I often feel inferior) from 1 (strongly disagree) to 7 (strongly agree). Items were averaged (α = .86) and scores ranged from 1.08 – 6.33 (M = 3.56, SD = 1).
Daily mood, negative event stress, and negative event appraisals
Participants described their current daily mood by rating adjectives on a scale from 1 (not at all) to 5 (extremely). A “pleasant mood” scale (α = .88)3 was created by averaging daily scores for “happy” and “cheerful.” Unpleasant mood (α = .73) was created by averaging daily scores for “sad” and “dejected.” Items were drawn from Larsen and Diener’s (1992) mood complex, and similar to Tennen et al. (2006), only the pure pleasant and unpleasant mood states were retained. Participants were then asked to think about their most negative experience that day, provide a brief description of it, and rate how stressful and threatening this event was, how much they felt they could control the event’s outcome, how well they felt they could deal with the event, and if this event was someone else’s’ fault. These questions were rated on a scale of 1 (not at all) to 7 (extremely). Participants listed a variety of negative events, with academic being the most common (33%), and the remaining interpersonal (e.g., friendship issues; 15%), health (e.g., trouble sleeping; 25%), or other (e.g., the weather; 27%) events4.
History of depression status
The mood episode module of the Structured Clinical Interview for the DSM-IV (SCID-I; First, Spitzer, Gibbon, & Williams, 2002) was used to classify participants’ history of depression status. This interview occurred three years after the diary portion of the study. The SCID-I requires that a mood disturbance created significant impairment to life at the time of the depressive episode. Interviews were conducted by research associates who were trained in the administration and coding of the SCID-I by a clinical psychologist, also a trained SCID evaluator. SCID depression interviews were conducted by phone, which have been shown to be comparable with face-to-face protocols (Rohde, Lewinsohn, & Seeley, 1997; Simon, Revicki, & Von Korff, 1993). To qualify for a diagnosis of lifetime major depression, a participant needed to endorse a time in which he or she experienced depressed mood or loss of interest every day or nearly every day for at least two weeks and that these changes in mood/interest significantly impaired his/her functioning at that time. During this period, the participant also needed to report having experienced at least four of the following symptoms: Changes in appetite or weight; sleep disturbance; fatigue or lack of energy; diminished self-worth; motor agitation or slowing; and suicidal thoughts. The depressive episode could not be due to normal bereavement, injury, illness, alcohol/drugs, or medication. During these interviews participants reported both past and current depressive episodes. Prior research indicates that people can accurately recall the occurrence of a previous depressive episode (Thompson, Bogner, Coyne, Gallo, & Eaton, 2004).
Participants were classified into three depression groups: Past depression, (i.e., a major depressive episode prior to the diary portion of the study; n = 24), subsequent depression, (i.e., a first major depressive episode during the three years following the beginning of the study; n = 54), and never depressed (n = 272). The mean age of depression episode was 20.88 (SD = 1.09) for participants in the subsequent depression group and 15.74 (SD = 2.25) for those in the past depression group. See Table 1 for descriptive statistics for each depression group on the personality measures, diary outcomes, and negative events reported.
Table 1.
Descriptive statistics based on depression history status
| Subsequent Depression Group | Never Depressed Group | Past Depression Group | |
|---|---|---|---|
| M (SD) or % | M (SD) or % | M (SD) or % | |
| Age | 18.57(.69) | 18.63(.83) | 19.13(1.26) |
| BDI | 6.13(4.58) | 4.11(3.92) | 5.25(3.27) |
| N | 3.93(.98) | 3.45(.97) | 3.94(1.13) |
| Academic Events | 28.2 | 34.4% | 26.7 |
| Interpersonal Events | 17.9 | 13.9% | 19.6 |
| Health Events | 24.9 | 24.9% | 25.8 |
| Other Events | 27.9 | 26.7% | 26.5 |
| Negative Event Stress | 4.52(.66) | 4.05(1.05) | 4.47(.68) |
| Negative Event Threat | 3.05(1.57) | 2.76(1.08) | 3.04(.98) |
| Negative Event Control | 3.74(.98) | 3.88(.93) | 3.91(.96) |
| Negative Event Ability to Deal | 4.76(.96) | 4.72(1.01) | 4.79(.74) |
| Negative Event Other Blame | 2.91(.82) | 2.65(.93) | 3.50(.91) |
| Pleasant Mood | 2.45(.70) | 2.71(.74) | 2.67(.59) |
| Unpleasant Mood | 1.38(.40) | 1.33(.40) | 1.40(.39) |
One-way ANOVAs and Tukey’s post-hoc tests indicated that participants with past depression were slightly older at the beginning of the study than those who were never depressed and those who went on to become depressed subsequent to diary participation (F(2,347) = 4.07, p < .05). There were also mean differences between groups on the BDI and Neuroticism measures. The subsequent depression group had the highest BDI scores, and scored significantly higher than participants in the never depressed group; participants with past depression did not differ from the other two groups on the BDI (F(2,347) = 6.21, p < .01). Never depressed participants had the lowest Neuroticism scores, and their Neuroticism scores were significantly lower than those in the subsequent depression and past depression groups (F(2,347) = 7.33, p < .01). Chi-square analyses indicated there were no significant differences between the depression groups on gender, race, and dating status.
Statistical analysis
The daily diary data had a nested structure in which the 30 repeated daily assessments (level 1) were nested within people (level 2; Raudenbush & Bryk, 2002). Therefore, multilevel modeling using Hierarchical Linear Modeling software (v. 6.06; Raudenbush, Bryk, & Congdon, 2008) was used to investigate the hypotheses. In all analyses, continuous level 1 variables were person-mean centered and continuous level 2 variables were grand mean-centered. The history of depression status variable was dummy-coded such that the past depression group was compared to the no depression and the subsequent depression groups.
Results
History of Depression Status and Average Mood and Negative Event Appraisals
Intercept-only models were constructed to determine whether history of depression status was associated with average levels of mood and event appraisals; current depressive symptoms (BDI), neuroticism and age were also included in all models. Age and neuroticism were included as control variables because they differed based on history of depression status. In addition, to test the priming hypothesis, a product term derived from the history of depression status and current depressive symptoms predictors was included to test for their interactive effect (e.g., Fifield et al., 1998). Using the pleasant mood outcome as an example, the multilevel equations are as follows:
Level 1
Level 2
In these equations, we were interested in the significance of G01, and G02 as these indicate the unique effects of history of depression status (at average levels of BDI) on average pleasant mood. The G06 and G07 terms were also of interest because they indicate whether history of depression status and current depression interact to affect average mood in these models. These interaction terms were dropped from the model if they were not significant to ease interpretation of the lower order BDI effect.
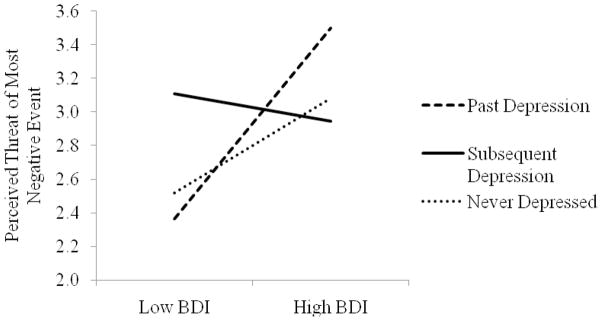
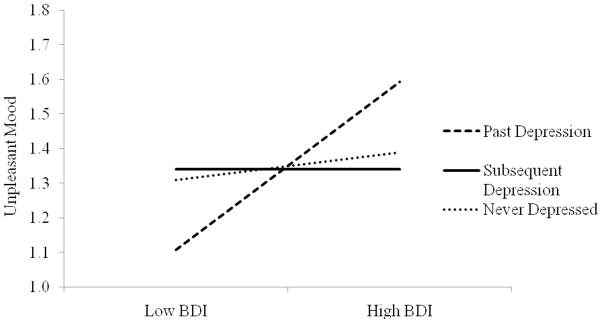
As Table 2 indicates, individuals with past depression were more likely to blame others for a negative event than were the never depressed and subsequently depressed groups. Also, there were two significant interactions between history of depression status and current symptoms indicating a priming effect. As illustrated in Figure 1, individuals in the past depression group had the strongest relationship between current symptoms and perceived threat, while those with subsequent depression had the weakest. As Table 2 indicates, these slopes differed significantly between the subsequent and past depression groups. The slopes did not differ between the past and never depressed groups. Figure 2 shows a similar pattern, such those with past depression had the strongest relationship between current symptoms and unpleasant mood, with the past depression group slope significantly differing from the subsequent depression group’s slope. There was also a trend with marginal significance that the never depressed group differed from the past depression group’s slope.
Table 2.
The association between depression history status and current depression symptoms and average diary measures
| Outcome Measure | Unstandardized coefficients | ||||
|---|---|---|---|---|---|
| Subsequent Depression Group1 | Never Depressed Group1 | BDI | BDI × Subsequent Depression | BDI × Never Depressed | |
| Negative Event Stress | −0.07 | −0.37 | 0.05** | -- | -- |
| Negative Event Threat | 0.10 | −0.13 | 0.14* | −.16* | −.07 |
| Negative Event Control | −0.19 | −0.06 | 0.02 | -- | -- |
| Negative Event Ability to Deal | −0.05 | −0.24 | −0.01 | -- | -- |
| Negative Event Other Blame | −0.58** | −0.84*** | −0.001 | -- | -- |
| Pleasant Mood | −0.22 | −0.15 | −0.04** | -- | -- |
| Unpleasant Mood | −0.01 | −0.001 | 0.06** | −.06* | −.05† |
Note. Neuroticism and age were controlled for in all models. Interaction terms were dropped from the model if they were not significant.
= as compared to past depression group;
p < .06;
p < .05;
p < .01;
p < .001
Figure 1.
Perceived threat of negative event as a function of current depressive symptoms and history of depression status.
Figure 2.
Unpleasant mood as a function of current depressive symptoms and history of depression status.
History of Depression Status and the Relationship between Negative Event Stress, Mood, and Appraisals
We determined whether history of depression status was related to differences in the within-person daily associations between negative event stress and mood and appraisals using a series of slope-as-outcomes models in HLM. Using pleasant mood as an example, the multilevel equations are as follows:
Level 1
Level 2
In these models we focused upon the significance tests of G11 and G12 as these represent the association between history of depression status and the within-person relation between negative event stress and pleasant mood (while controlling for current depression, age and Neuroticism). In addition, the G16 and G17 terms indicate if history of depression status and current depression interact in predicting the relationship between daily negative event stress and mood. Again, if the BDI × history of depression status interaction was not significant, it was removed from the model to ease interpretation of the lower order terms.
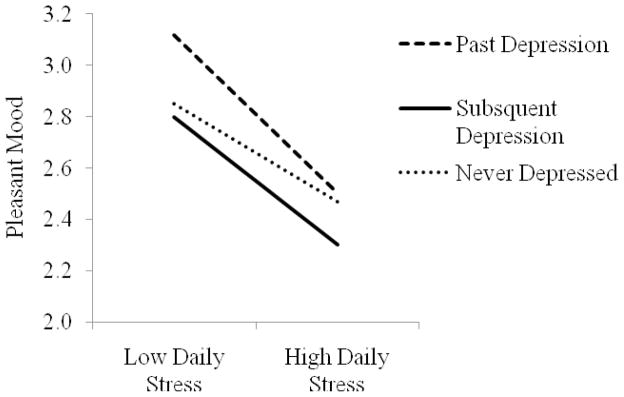
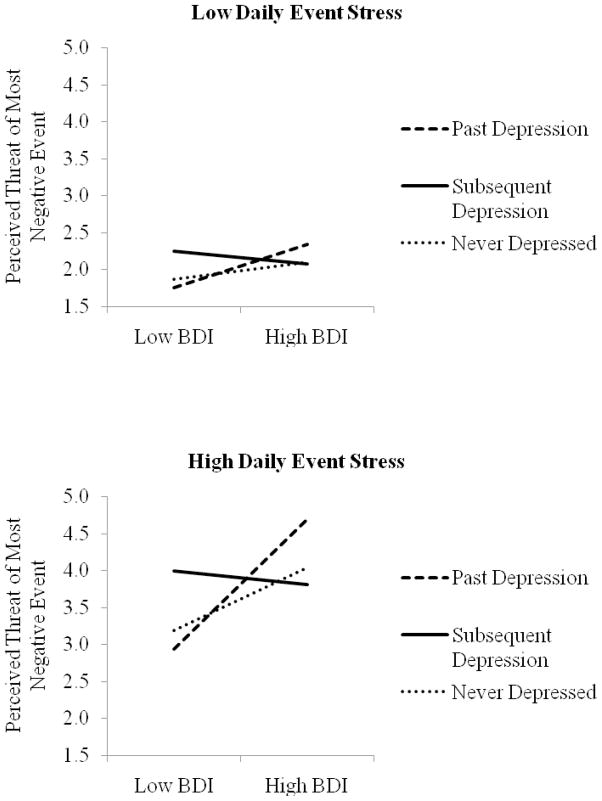
As noted in Table 3, deviations from one’s mean level of negative event stress was related to perceiving events as more threatening, feeling less able to deal with the event, greater other-blame for the event, less pleasant mood and more unpleasant mood. In addition, history of depression status affected the relationship between negative event stress and pleasant mood. As shown in Figure 3, as daily negative event stress increased, daily pleasant mood declined most sharply among those with past depression, as compared to those with no depression history and subsequent depression; however the difference in slopes was significant only between the past and never depressed groups. We also found a three-way interaction between current symptoms, history of depression status (subsequent depression vs. past depression) and daily stress in predicting daily negative event threat. Figure 4 illustrates that the there was a stronger moderating effect of depression status on the relationship between BDI scores and daily perceived event threat on high stress days versus low stress days. Specifically, among past depressed individuals, but not subsequently depressed individuals, current symptoms show a stronger relationship with daily threat perceptions on high versus low stress days.
Table 3.
The within-person association between depression history status, current depression symptoms, negative event stress and diary measures
| Outcome Measure | Unstandardized coefficients | |||||
|---|---|---|---|---|---|---|
| Daily event stress | Subsequent Depression Group × Daily stress | Never Depressed Group × Daily stress | BDI × Daily stress | BDI × Subsequent Depression × Daily stress | BDI × Never Depressed × Daily stress | |
| Negative Event Threat | 0.54*** | −0.01 | −0.04 | 0.04* | −.04* | −.03 |
| Negative Event Control | 0.05 | −0.01 | −0.01 | −0.004 | -- | -- |
| Negative Event Ability to Deal | −0.27*** | −0.02 | 0.09 | −0.01 | -- | -- |
| Negative Event Other Blame | 0.18** | −0.06 | 0.01 | −0.003 | -- | -- |
| Pleasant Mood | −0.16*** | 0.03 | 0.06* | 0.001 | -- | -- |
| Unpleasant Mood | 0.09*** | −0.02 | −0.03 | 0.001 | -- | -- |
Note. Neuroticism and age were controlled for in all models. The interaction terms involving depression history group and BDI were dropped from the model if they were not significant.
p < .05;
p < .01;
p < .001
Figure 3.
Pleasant mood as a function of negative event stress and history of depression status.
Figure 4.
Perceived threat of negative event as a function of perception of negative event stress, current depressive symptoms and history of depression status.
Discussion
We predicted that formerly depressed individuals, as compared to those without a history of depression, would appraise daily events more negatively. In support of this prediction, we found that compared to participants who had never been depressed, those who had experienced a depressive episode prior to study participation were more inclined to blame others for the negative events they encountered during the diary period. While blaming the self for negative events is often considered maladaptive and has been emphasized in the literature, blaming others is also associated with poor psychological adjustment because it may interfere with adaptive coping, lower sense of control over events, or hinder social support (Hall, French, & Marteau, 2003; Tennen & Affleck, 1990). Therefore, our findings suggest that depression researchers pay closer attention to other-blame among formerly depressed individuals.
We also predicted that on days with a more stressful event, individuals with a history of depression would report greater increases in maladaptive event-related appraisals, and more negative and less positive mood as compared to never depressed individuals. Echoing Conner et al. (2006), we found that participants who had been depressed prior to study participation demonstrated steeper declines in positive mood on more stressful days. Similar to Tennen et al. (2006) we did not find this pattern for negative affect. It is possible that because there was less variability in negative mood than positive mood, this effect was harder to capture. Future research will be needed to determine why in some cases positive affect is affected but negative affect is not. In any case, declines in positive affect are important even without increases in negative affect. For example, according to the ‘broaden and build’ theory (Fredrickson, 2001), positive emotions increase emotional well-being by broadening people’s attention and cognitive resources and should facilitate coping with stress (Fredrickson & Joiner, 2002). The declines in positive mood seen in this study among the formerly depressed on high stress days indicate that these individuals may have difficulty finding meaning in everyday negative events, which could continue their cycle of lower positive affect and pessimistic thinking (Fredrickson & Joiner, 2002).
Our findings indicate that people with a history of depression do have deficits on some of the outcomes in this study as compared to those who have never been depressed, suggesting that either psychosocial scars or preexisting vulnerabilities may be responsible. In this study, we found support for both explanations. Full support for the scar hypothesis would be provided if the past depression group significantly differed from both the future and the never depressed group by reporting greater deficits in functioning. The strongest support for this hypothesis comes from the finding that individuals with a history of depression blamed others for negative events more, on average, compared to those who would subsequently become depressed and who were never depressed. Additional support for the scar hypothesis, albeit less strong, comes from a priming effect. Participants with past depression, who also had high current depressive symptoms, reported higher daily levels of unpleasant mood as compared to participants in the subsequent depression and never depressed groups. However, full support for the scar hypothesis was dampened due to the marginal nature of the difference between the never depressed and past depression groups’ slopes; a significant difference between these groups would be required for full support. An additional priming effect suggested that among individuals with greater current depressive symptoms, the past depression group perceived events to be more threatening than the subsequent depression group, especially on high negative event stress days, providing initial support for the scar hypothesis. However this finding did not provide full support because the past and never depressed groups did not significantly differ from each other. While tentative, the findings reported here in support of the scar hypothesis raise concerns regarding individuals with a history of depression because other-blame, negative mood and appraising events as threatening has been related to poorer psychological adjustment among a variety of populations (e.g., Chandler, Kennedy, & Sandhu, 2007; Felsten, 2002; Pakenham, 1999; Pakenham & Rinaldis, 2001).
As noted, several of these findings occurred as a result of a priming effect, which suggests that vulnerabilities from depressive episodes are triggered or “primed” by a state of elevated distress (e.g., high current depressive symptoms; Roberts & Kassel, 1996). This indicates that in some cases, deficits due to “psychosocial scars” may only be evident in day to day functioning at times when symptoms are elevated. Therefore, in addition to collecting information about past depressive episodes, researchers should also measure current symptoms and determine their interactive affect on the stress reactivity process.
We also found evidence for the vulnerability hypothesis, with the strongest support coming from our finding that as compared to the never depressed group, participants who had been depressed prior to study participation demonstrated steeper declines in positive mood on more stressful days and they did not significantly differ from the subsequent depression group. Similar support for the vulnerability hypothesis is seen in the lack of differences between the past depression and subsequent depression groups on four of the seven outcomes, indicating that these two groups have similar cognitive patterns in some areas both prior to and after depressive episodes. However, due to a host of factors (especially the small sample sizes), these null findings should be interpreted with caution.
While we add to the mixed findings on the scar vs. vulnerability hypothesis debate, the findings of this study are noteworthy because we provided a stringent test of the hypotheses by comparing previously depressed individuals to both never depressed and subsequently depressed individuals using a daily dairy method. To our knowledge, this is the first such test of these hypotheses.
Strengths and Limitations
This study had several distinct strengths and offers some insight into the role of major depression in daily functioning. We combined a daily process and longitudinal study design and this method differs from the cross-sectional and prospective designs that have previously been used to investigate the scar versus the vulnerability hypothesis. This study is the first to use such a design to directly compare individuals who had previously experienced a depressive episode to individuals who would subsequently experience a depressive episode several years later allowing for a clear comparison of the two hypotheses. Our study methods also allowed us to examine the influence of individual differences in history of depression status on daily within-person slopes (e.g., when-then contingencies or behavioral signatures; Shoda, Mischel & Wright, 1994; Tennen, Affleck, Armeli, & Carney, 2000), rather than utilizing nomothetic methods which at times have not detected deficiencies in functioning before and after depressive episodes (see Haeffel et al., 2005).
Despite these notable strengths, there are limitations which must be mentioned. First, the past depression group was relatively small, which limits the power of our analyses. Second, although we used a well-validated method to measure history of depression status (i.e., SCID interviews), we nonetheless had to rely on participants’ recollections of the timing of their previous depression. Although the SCID has been shown to be valid for recall of previous episodes (Thompson et al., 2004), this method in not as precise as prospective assessment methods (e.g., Alloy et al., 1999). This study offered a unique glimpse into everyday psychosocial functioning among individuals who would subsequently become depressed; however, a diary study embedded within a fully prospective longitudinal design will be an important next step. In addition, a more comprehensive (e.g., multiple daily assessments) study of daily stress, appraisals, coping, and mood might provide more reliable assessments of these processes.
Although we followed participants for three years after they completed the diary, the students in our study had not yet reached the normative age of highest risk for the onset of a first major depressive episode (Zisook et al., 2004). Therefore, there are students in the never depressed group who may go on to experience a depressive episode perhaps leading us to understate the observed associations and miss others. Even longer follow-up periods will be required to fully answer the questions posed in this study. In addition, because the average age of first onset of major depression is in the mid-twenties, this study may reflect outcomes specific to those with early-onset/adolescent depression. As compared to adult-onset, pre-adulthood onset is associated with greater clinical (e.g., more irritability) and psychosocial (e.g., lower educational attainment) deficits; therefore, future research may need to determine whether similar outcomes are found among those with adult-onset depression (e.g., Kessler, Foster, Saunders, & Stang, 1994; Zisook et al., 2004). We did not assess whether participants had received a depression diagnosis, or whether they had received treatment; therefore, it is unknown how this may have affected the results. In the future, diagnostic and treatment history should be gathered and perhaps used as a control in statistical analyses. Finally, our sample was predominantly White and consisted of college students. This is a strength because previous history of depression diary studies have focused on clinical populations and this study extends findings to a more normative population; however, we do not know whether these findings generalize to more diverse populations in terms of race, age, education, and socioeconomic status. We did, however, document that our study participants reflected the broader student population on campus.
Implications
This study has implications for depression theory and research. It is important to understand why differences in functioning are present between the formerly depressed and never depressed in order to better understand the progression and treatment of depression. Theoretically, we found some support for the scar hypothesis, though several other studies have found limited to no support for it. It is possible that other studies did not support the scar hypothesis because of the nature of the outcomes measured (e.g., non stress-related outcomes), or the method used. As we mentioned previously, daily process methods appear to be particularly well suited to testing the scar and vulnerability hypotheses and future investigations should consider using such methods.
Methodologically, this study suggests that typical control groups used in depression research may need to be reconsidered. Although all of our study participants would be considered non-depressed in most studies, and thus would be eligible to be included in a control group in a depression study, our previously depressed participants showed some depression-related appraisal and mood reactivity patterns. Although investigators cannot identify who will go on to experience a depressive episode, they can reliably determine depression history.
Future Directions
We know little about whether individuals who have a history of depression or who are vulnerable to depression are exposed to more daily stressors than their never-depressed counterparts; however, our methods in the current study did not allow us to examine differential stress generation and exposure processes between the depression groups. While research indicates that depressed individuals appear to generate stressful interpersonal events (Hammen, 1991), future research should examine whether history of depression status and the appraisal processes investigated in this study affect the generation of stressful events.
In the current study, some outcomes supported the vulnerability hypothesis, while others supported the scar hypothesis. It is not clear why this occurred, however it could be because we asked participants to report only on the most negative event of their day rather than allowing them to report on an unlimited amount of daily negative events. In addition, much less is known about how positive events are perceived among depressed individuals. Future research should investigate whether some types of appraisals may be particularly prone to deficits related to depression, and should expand the type and amount of negative events reported, as well as investigate positive events. Finally, it is possible that both hypotheses may be true in some cases, as this and other research indicates that both scars and preexisting vulnerabilities contribute to deficits in functioning.
In conclusion, previous daily diary research has consistently suggested that past depressive episodes negatively affect individuals’ appraisals, coping and mood. However, these studies did not determine why such vulnerabilities existed. In this study, we offer the first examination of the scar versus the vulnerability hypotheses using daily process methods in addition to extending previous findings on the history of depression and daily life. Overall, our findings do not provide clear support for either the scar hypothesis or the vulnerability hypothesis, with the past depression and subsequent depression groups differing on several of the outcome measures, but not on others. However, this study is an important first step to understanding why people who experienced depression in the past are sometimes less able to maintain their well-being in the face of daily challenges.
Acknowledgments
This research was supported by grants T32-AA007290 and P50-AA03510 from the National Institute on Alcohol Abuse and Alcoholism.
Footnotes
A variety of negative event attributions (see Abramson et al., 1989; Tennen & Affleck, 1990) have been linked to depression, including the perception of how stable and global the event cause is, and blaming the self or others for the event. In the current study we only assessed other-blame. We considered assessing other types of attributions but felt other-blame was important because it has received little attention in the literature and including other attribution types would have required many additional diary items.
Analyses indicated that excluded students (M = 18.95, SD = 1.34) were slightly older than included students (M = 18.65, SD = .86), t(572) = −3.23, p < .01, and differed by race and gender in that a larger proportion of males and students who identified as Hispanic/Latino or Other were excluded, X2(4) = 15.56, p < .01.
Alpha reliabilities for composite measures were computed at the daily level (across all individuals and all days).
Additional multilevel analyses (available from the first author) were performed to investigate whether event type interacted with depression group to affect appraisals and mood. Results indicated that the relationship between event type (e.g., academic, interpersonal, health) and the outcomes variables did not differ across depression groups except for the pleasant mood outcome. For this outcome, the past depression group’s positive mood decreased on days when a negative event was non-academic, as compared to an academic event. The other two group’s moods were not affected by whether the event was academic or non-academic.
References
- Abramson LY, Metalsky GI, Alloy LB. Hopelessness depression: A theory-based subtype of depression. Psychological Review. 1989;96:358–372. [Google Scholar]
- Alloy LB, Abramson LY, Whitehouse WG, Hogan ME, Tashman NA, Steinberg DL, et al. Depressogenic cognitive styles: predictive validity, information processing and personality characteristics, and developmental origins. Behaviour Research and Therapy. 1999;37:503–531. doi: 10.1016/s0005-7967(98)00157-0. [DOI] [PubMed] [Google Scholar]
- Beck AT, Beck RW. Screening depressed patients in family practice: A rapid technique. Postgraduate Medicine. 1972;52:81–85. doi: 10.1080/00325481.1972.11713319. [DOI] [PubMed] [Google Scholar]
- Beck AT, Rush AJ, Shaw BF, Emery G. Cognitive therapy of depression. New York: Guilford; 1979. [Google Scholar]
- Beevers CG, Rohde P, Stice E, Nolen-Hoeksema S. Recovery from major depressive disorder among female adolescents: A prospective test of the scar hypothesis. Journal of Consulting and Clinical Psychology. 2007;75:888–900. doi: 10.1037/0022-006X.75.6.888. [DOI] [PubMed] [Google Scholar]
- Bodenmann G, Pihet S, Kayser K. The relationship between dyadic coping and marital quality: A 2-year longitudinal study. Journal of Family Psychology. 2006;20:485–493. doi: 10.1037/0893-3200.20.3.485. [DOI] [PubMed] [Google Scholar]
- Bolger N, DeLongis A, Kessler RC, Schilling EA. Effects of daily stress on negative mood. Journal of Personality and Social Psychology. 1989;57:808–818. doi: 10.1037//0022-3514.57.5.808. [DOI] [PubMed] [Google Scholar]
- Bolger N, Shilling EA. Personality and the problems of everyday life: The role of neuroticism in exposure and reactivity to daily stressors. Journal of Personality. 1991;59:355–386. doi: 10.1111/j.1467-6494.1991.tb00253.x. [DOI] [PubMed] [Google Scholar]
- Bolger N, Zuckerman A. A framework for studying personality in the stress process. Journal of Personality and Social Psychology. 1995;69:890–902. doi: 10.1037//0022-3514.69.5.890. [DOI] [PubMed] [Google Scholar]
- Chandler M, Kennedy P, Sandhu N. The association between threat appraisals and psychological adjustment in partners of people with spinal cord injuries. Rehabilitation Psychology. 2007;52:470–477. [Google Scholar]
- Christensen MV, Kessing LV. Do personality traits predict first onset in depressive and bipolar disorder? Nordic Journal of Psychiatry. 2006;60:79–88. doi: 10.1080/08039480600600300. [DOI] [PubMed] [Google Scholar]
- Conner TS, Tennen H, Zautra AJ, Affleck G, Armeli S, Fifield J. Coping with rheumatoid arthritis pain in daily life: Within-person analyses reveal hidden vulnerability for the formerly depressed. Pain. 2006;126:198–209. doi: 10.1016/j.pain.2006.06.033. [DOI] [PubMed] [Google Scholar]
- Costa PT, McCrae RR. NEO PI-R. Professional Manual. Revised NEO Personality Inventory (NEO PI-R) and NEO Five-Factor Inventory (NEO-FFI) Odessa, FL: Psychological Assessment Resources, Inc; 1992. [Google Scholar]
- Eaves G, Rush AJ. Cognitive patterns in symptomatic and remitted unipolar major depression. Journal of Abnormal Psychology. 1984;93:31–40. doi: 10.1037//0021-843x.93.1.31. [DOI] [PubMed] [Google Scholar]
- Felsten G. Minor stressors and depressed mood: Reactivity is more strongly correlated than total stress. Stress and Health. 2002;18:75–81. [Google Scholar]
- Fifield J, Tennen H, Reisine S, McQuillan J. Depression and the long-term risk of pain, fatigue, and disability in patients with rheumatoid arthritis. Arthritis and Rheumatism. 1998;41:1851–1857. doi: 10.1002/1529-0131(199810)41:10<1851::AID-ART18>3.0.CO;2-I. [DOI] [PubMed] [Google Scholar]
- First MB, Spitzer RL, Gibbon M, Williams JBW. Structured clinical interview for DSM-IV TR Axis I disorders, research version, non-patient edition (SCID-I/NP) New York: Biometrics Research, New York State Psychiatric Institute; 2002. [Google Scholar]
- Fredrickson BL. The role of positive emotions in positive psychology: The broaden and build theory of positive emotions. American Psychologist. 2001;56:218–226. doi: 10.1037//0003-066x.56.3.218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fredrickson BL, Joiner T. Positive emotions trigger and upward spiral toward emotional well-being. Psychological Science. 13:172–175. doi: 10.1111/1467-9280.00431. [DOI] [PubMed] [Google Scholar]
- Gunthert KC, Cohen LH, Armeli S. Unique effects of depressive and anxious symptomatology on daily stress and coping. Journal of Social and Clinical Psychology. 2002;21:583–609. [Google Scholar]
- Gunthert KC, Cohen L, Butler AC, Beck JS. Depression and next-day spillover of negative mood and depressive cognitions following interpersonal stress. Cognitive Research and Therapy. 2007;31:521–532. [Google Scholar]
- Haaga D, Beck AT. Cognitive therapy. In: Paykel ES, editor. Handbook of affective disorders. 2. New York: The Guilford Press; 1992. pp. 511–523. [Google Scholar]
- Haeffel GJ, Abramson LY, Voelz ZR, Metalsky GI, Halberstadt L, Dykman BM, et al. Negative cognitive styles, dysfunctional attitudes, and the remitted depressive paradigm: A search for the elusive cognitive vulnerability to depression factor among remitted depressives. Emotion. 2005;5:343–348. doi: 10.1037/1528-3542.5.3.343. [DOI] [PubMed] [Google Scholar]
- Hall S, French DP, Marteau TM. Causal attributions following serious unexpected negative events: A systematic review. Journal of Social & Clinical Psychology. 2003;22:515–536. [Google Scholar]
- Hojat M, Gonnella JS, Erdmann JB, Vogel WH. Medical students’ cognitive appraisal of stressful life events as related to personality, physical well-being, and academic performance: A longitudinal study. Personality and Individual Differences. 2003;35:219–235. [Google Scholar]
- Hammen C. Generation of stress in the course of unipolar depression. Journal of Abnormal Psychology. 1991;100:555–561. doi: 10.1037//0021-843x.100.4.555. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Foster CL, Saunders WB, Stang PE. The social consequences of psychiatric disorders: I. Educational attainment. American Journal of Psychiatry. 1995;152:1026–1032. doi: 10.1176/ajp.152.7.1026. [DOI] [PubMed] [Google Scholar]
- Larsen RJ, Diener E. Promises and problems with the circumplex model of emotion. In: Clark MS, editor. Review of personality and social psychology. Newbury Park: Sage; 1992. pp. 25–59. [Google Scholar]
- Lazarus RS, Folkman S. Stress, appraisal, and coping. New York: Springer; 1984. [Google Scholar]
- Myin-Germeys I, Peeters F, Havermans R, Nicolson NA, deVries MW, Delespaul P, et al. Emotional reactivity to daily life stress in psychosis and affective disorder: An experience sampling study. Acta Psychiatrica Scandinavica. 2003;107:124–131. doi: 10.1034/j.1600-0447.2003.02025.x. [DOI] [PubMed] [Google Scholar]
- Pakenham KI. Adjustment to multiple sclerosis: Application of a stress and coping model. Health Psychology. 1999;18:383–392. doi: 10.1037//0278-6133.18.4.383. [DOI] [PubMed] [Google Scholar]
- Pakenham KI, Rinaldis M. The role of illness, resources, appraisal and coping strategies in adjustment to HIV/AIDS: The direct and buffering effects. Journal of Behavioral Medicine. 2001;24:259–279. doi: 10.1023/a:1010718823753. [DOI] [PubMed] [Google Scholar]
- Raudenbush SW, Bryk AS. Hierarchical linear models: Applications and data analysis methods. London: Sage; 2002. [Google Scholar]
- Raudenbush SW, Bryk AS, Congdon R. HLM 6 hierarchical linear and nonlinear modeling. Scientific Software International Inc; 2008. [Google Scholar]
- Roberts JE, Kassel JD. Mood-state dependence in cognitive vulnerability to depression: The roles of positive and negative affect. Cognitive Therapy and Research. 1996;20:1–12. [Google Scholar]
- Rohde P, Lewinsohn PM, Seeley JR. Are people changed by the experience of having an episode of depression? A further test of the scar hypothesis. Journal of Abnormal Psychology. 1990;99:264–271. doi: 10.1037//0021-843x.99.3.264. [DOI] [PubMed] [Google Scholar]
- Rohde P, Lewinsohn PM, Seeley JR. Are adolescents changed by an episode of major depression? Journal of the American Academy of Child & Adolescent Psychiatry. 1994;33:1289–1298. doi: 10.1097/00004583-199411000-00010. [DOI] [PubMed] [Google Scholar]
- Rohde P, Lewinsohn PM, Seeley JR. Comparability of telephone and face-to-face interviews assessing Axis I and II disorders. American Journal of Psychiatry. 1997;154:1593–1598. doi: 10.1176/ajp.154.11.1593. [DOI] [PubMed] [Google Scholar]
- Shoda Y, Mischel W, Wright J. Intraindividual stability in the organization and patterning of behavior: Incorporating psychological situations into the idiographic analysis of personality. Journal of Personality and Social Psychology. 1994;67:674–687. doi: 10.1037//0022-3514.67.4.674. [DOI] [PubMed] [Google Scholar]
- Simon GE, Revicki D, Von Korff M. Telephone assessment of depression severity. Journal of Psychiatric Research. 1993;27:247–252. doi: 10.1016/0022-3956(93)90035-z. [DOI] [PubMed] [Google Scholar]
- Stone AA, Reed BR, Neale JM. Changes in daily event frequency precede episodes of physical symptoms. Journal of Human Stress. 1987;13:70–74. doi: 10.1080/0097840X.1987.9936797. [DOI] [PubMed] [Google Scholar]
- Tennen H, Affleck G. Blaming others for threatening events. Psychological Bulletin. 1990;108:209–232. [Google Scholar]
- Tennen H, Affleck G, Armeli S, Carney MA. A daily process approach to coping: Linking theory, research, and practice. American Psychologist. 2000;55:626–636. doi: 10.1037//0003-066x.55.6.626. [DOI] [PubMed] [Google Scholar]
- Tennen H, Affleck G, Zautra A. Depression history and coping with chronic pain: A daily process analysis. Health Psychology. 2006;25:370–379. doi: 10.1037/0278-6133.25.3.370. [DOI] [PubMed] [Google Scholar]
- Thompson R, Bogner HR, Coyne JC, Gallo JJ, Eaton WW. Personal characteristics associated with consistency of recall of depressed or anhedonic mood in the 13-year follow-up of the Baltimore Epidemiologic Catchment Area Survey. Acta Psychiatrica Scandinavica. 2004;109:345–354. doi: 10.1111/j.1600-0447.2003.00284.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wagner JA, Tennen H, Mansoor GA, Abbott G. History of depressive disorder and endothelial function in postmenopausal women. Psychosomatic Medicine. 2006;68:80–86. doi: 10.1097/01.psy.0000195868.68122.9e. [DOI] [PubMed] [Google Scholar]
- Zautra AJ, Parrish BP, Van Puymbroeck CM, Tennen H, Davis MC, Reich JW, et al. Depression history, stress, and pain in rheumatoid arthritis patients. Journal of Behavioral Medicine. 2007;30:187–197. doi: 10.1007/s10865-007-9097-4. [DOI] [PubMed] [Google Scholar]
- Zautra AJ, Davis MC, Reich JW, Nicassio P, Tennen H, Finan P, et al. Comparison of cognitive behavioral and mindfulness meditation interventions on adaptation to rheumatoid arthritis for patients with and without history of recurrent depression. Journal of Consulting and Clinical Psychology. 2008;76:408–421. doi: 10.1037/0022-006X.76.3.408. [DOI] [PubMed] [Google Scholar]
- Zisook S, Rush AJ, Albala A, Alpert J, Balasubramani GK, Fava M, et al. Factors that differentiate early vs. later onset of major depression disorder. Psychiatry Research. 2004;129:127–140. doi: 10.1016/j.psychres.2004.07.004. [DOI] [PubMed] [Google Scholar]