Abstract
The substantial growth in mobile handheld technologies has heralded the opportunity to provide physicians with access to information, resources, and people at the right time and place. But is this technology delivering the benefits to workflow and patient care promised by increased mobility? The authors conducted a systematic review to examine evidence regarding the impact of mobile handheld technology on hospital physicians' work practices and patient care, focusing on quantification of the espoused virtues of mobile technologies. The authors identified thirteen studies that demonstrated the ability of personal digital assistants (PDAs) to positively impact on areas of rapid response, error prevention, and data management and accessibility. The use of PDAs demonstrates the greatest benefits in contexts where time is a critical factor and a rapid response crucial. However, the extent to which these devices improved outcomes and workflow efficiencies because of their mobility was largely absent from the literature. The paucity of evidence calls for much needed future research that asks explicit questions about the impact the mobility of devices has on work practices and outcomes.
Introduction
Mobility is a central feature of health care delivery. 1 Clinical work, conducted in multiple locations, requires physicians to communicate and collaborate with different individuals and to move between patients, wards, clinics, laboratories, operating theaters, and offices. 2–4 Physicians require information systems which provide access to data, resources, and people where and when they undertake work. 2 Technology can potentially improve information accessibility. 5 Nevertheless, mismatches between system capabilities, and needs and workflows of physicians may hinder realization of intended benefits. 6
Clinical systems have only partly delivered upon the promise of providing the right information, about the right patient, at the right time, in the right place. 2 While desktop computers allow easy storage, searching, retrieval, and sharing of patient information, 7 because they are static, they do not support many aspects of mobile work. 2,8,9 In the absence of bedside terminals, physicians must often search to find an accessible computer at a location away from the patient. 10 Traditional portable paper charts, by contrast, support the mobility of physicians, 8,11 but are limited by inefficient information accessibility and their lack of simultaneous access by multiple users. 2,11
Mobile technologies combine advantages of paper charts and desktop computers in their portability 12 and support for information access anywhere, anytime. 11 Handheld devices, including tablet computers and personal digital assistants (PDAs), are generally small, portable, lightweight computers with wireless network connectivity. 13–15 Since their introduction in the 1990s, their uptake has steadily increased. 12–14,16,17 A review of PDA use by healthcare providers indicated adoption by 45% to 85% of those surveyed, with hospital-based physicians identified as the most likely users. 14
But do handheld devices deliver benefits to workflow and patient care promised by increased mobility? Existing systematic reviews covered the following: uses of handheld devices and their potential roles in medicine; 13,16,18 features and functionality of handheld devices; 13,16 current adoption rates and the primary healthcare users of these devices; 12,14 opinions about the benefits of handheld devices and barriers to their implementation or adoption; 12,17,19 and the perceived outcomes of handheld device use. 12,18,19 The reviews provide considerable evidence regarding uses of handheld devices for: administrative support (e.g., billing and scheduling); professional activities (e.g., patient tracking and electronic prescribing); documentation; decision support (e.g., clinical and drug references); and education and research. Touted benefits of these devices include enhanced productivity, improved information access, improved communication, reduced medical errors, greater mobility, and improved quality of patient care. Paradoxically, few reviewers have examined the extent to which mobile handheld devices produce improved outcomes and work practice efficiencies because of their mobility.
The authors undertook a systematic review of evidence for the impact of mobile handheld technology on hospital physicians' work practices and patient care. The focus went beyond suggestions or conclusions about “potential” impacts of handheld devices to concentrate on quantification of the espoused virtues of mobile technologies. 5,19
Methods
Search Strategy
We based our systematic review on established Cochrane review principles 20 and the Critical Appraisal Checklist for Systematic Reviews of Health Informatics Evaluations (CASP). 21 We conducted the literature search using multiple search strategies to overcome problems associated with inadequate indexing 13,16,22,23 and to ensure a more exhaustive scope. 20,22–25
To explore several databases, our initial search used the Medical Subject Heading (MeSH) “computers, handheld” supplemented by keywords we identified as being synonymous with handheld computers. In some databases, we combined these keywords with the MeSH terms physicians, medical staff, or medicine. Table 1, available as an online data supplement at http://www.jamia.org, outlines the search strategy, conducted in January 2008. We also searched by hand the reference lists from systematic review articles to identify additional relevant studies.
Study Selection
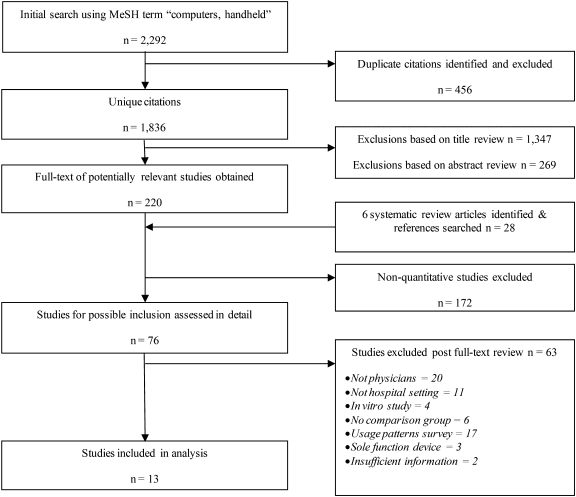
The MeSH search yielded 2,292 results. ▶ illustrates the selection process. The keyword search generated 360 results (Figure 2, available as an online data supplement at http://www.jamia.org). Two reviewers (MP and AG) independently completed title and abstract reviews. In the absence of an abstract, the full-text article was reviewed. Where study information was unclear or additional information was necessary, we contacted the study authors.
Figure 1.
MeSH search and selection process.
The combined search strategies identified 88 full-text articles, which all three authors assessed. Any disagreements were resolved by in-depth discussion and subsequent consensus. Of the 88 articles, 13 met the criteria for inclusion (below); ▶ and 2 list reasons for exclusions.
Inclusion Criteria
The analysis only included articles published between January 2000 and December 2007, available in full-text and in English. While we included experimental, evaluative, and observational studies, we excluded other study designs such as qualitative, beta testing exercises, proof-of-concept research, product descriptions, and usability studies (software- or hardware-oriented). We also excluded surveys of patient opinions, physician usage patterns, and physicians' impressions regarding ease of use. Due to the heterogeneous nature of the studies, formal meta-analysis was not possible.
Analysis Framework
We categorized the included studies based on themes from Bates and Gawande 26 regarding use of information technology to support safe healthcare delivery processes. We used these categories as a structured framework to present our results. The categories included use of handheld devices to facilitate: (1) rapid response by allowing physicians to identify patient needs, provide prompt intervention, and improve modes of communication; (2) medication error prevention by providing physicians with point-of-care decision support with accessible reference information and by eliminating illegibility and decreasing transcription errors; and (3) data management and accessibility by enabling physicians to access up-to-date patient information in electronic medical records at the point of care, to assist with monitoring and documentation.
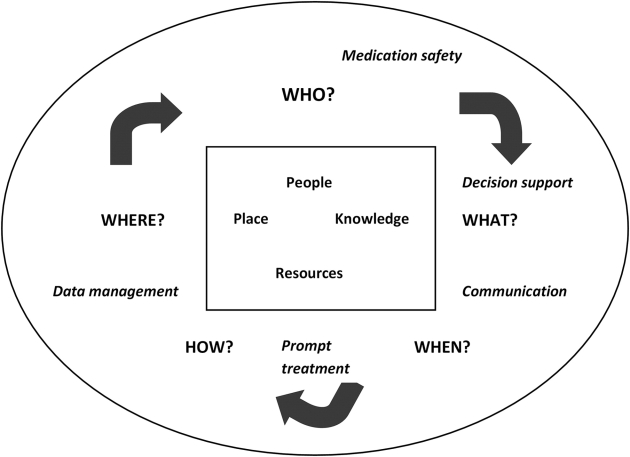
We also assessed the impact of handheld devices on hospital physicians' work practices in terms of changes in: who undertook an activity; what was done or what resources were used in the activity; when the activity happened; where the activity was performed; and how the activity was realized. These were derived from levels of activity (objectives), levels of action (results) and levels of operation (conditions) outlined by Bardram. 27 One author (MP) classified the findings in accordance with the analysis framework and the other two authors validated this.
Results
The thirteen included studies were published between 2000 and 2006, with the largest number originating from the United States (n = 6) and the remaining (n = 7) from the UK, Australia, Canada, Denmark, Finland, Germany, and Hong Kong. The handheld devices used within the studies were all identified as PDAs. Study methodologies included randomized controlled trials (RCTs) (n = 2) and observational studies (n = 11). Five of the thirteen were pilot studies and only one involved more than one study site. Most studies measured the impact of the intervention either immediately after implementation (i.e., within 2 mo) (n = 5) or over/after a longer period (i.e., greater than 6 mo) (n = 5). Only one of the studies stated specifically where within the study site physicians used the handheld device, and four concluded that the mobility of the device had an impact on the study outcomes.
Handheld Devices Facilitating Rapid Response
Four studies evaluated handheld devices that aimed to facilitate physicians' responses to clinical situations in a timely manner (see Table 2, available as an online data supplement at http://www.jamia.org). Of the four, three 28–30 studies examined provision of prompt treatment, and one 31 examined the enhancement of interprofessional communication.
Prompt Treatment
Three emergency medicine studies 28–30 involved the wireless transmission of investigatory images [electrocardiographs (ECGs) or computerized tomography (CT) scans] to physicians' handheld devices to promote faster treatment through earlier notification, assessment, and interpretation. Adams et al. 28 and Clemmensen et al. 29 investigated wireless transmission of prehospital ECGs to a cardiologist's PDA to enable improved door-to-treatment times. Adams et al. 28 compared 17 months of preintervention data, during which 48 patients with acute coronary occlusion were transported to the study site by emergency medical services, with 24 months of intervention data, during which 24 patients with successful prehospital ECG transmission were transported by emergency medical services. In the intervention phase, prehospital ECGs were transmitted to a desktop computer located at the study site. This allowed the Emergency Department (ED) nurses to wirelessly forward the ECG images to a cardiologist's PDA. In nineteen cases, prehospital transmission of ECGs failed, thus this group was used as concurrent controls alongside the 101 patients who self-transported to the ED during the intervention phase. The study findings demonstrated a significantly shorter median door-to-reperfusion time with successful ECG transmission (50 min) compared with: the preintervention time (101 min) (p < 0.0001); those who self-transported (96 min) (p < 0.0001); and those with failed transmission (78 min) (p < 0.0001).
Similar findings were identified by Clemmensen et al. 29 who reported 15 months of data, during which 408 prehospital ECGs were transmitted to a desktop computer at the study site and simultaneously to a cardiologist's PDA. The cardiologist subsequently notified ambulance personnel as to whether the patient needed to be transported to a noninvasive hospital (295 patients) or redirected to a hospital with invasive facilities for primary percutaneous coronary intervention (pPCI) (113 patients). Results showed that redirected patients (pPCI) took significantly longer to arrive at their designated hospital than non-PCI patients [mean time of 17 min compared with 10 min (p = 0.005)]. However, there was a substantial reduction of 54 minutes in door-to-treatment times for pPCI patients compared with historical controls 32 [average time of 40 min compared with 94 min (p < 0.01)].
Reponen et al. 30 explored data accuracy achievable on handheld technology by assessing CT image quality. They rated the suitability for diagnosis of twenty-one CT scans on a PDA by comparing these reports to reference reports based on the original films. During the study, CT images were stored on a teleradiology server from which physicians could download images to a handheld device. The process averaged 90 seconds per image. Image quality was rated as suitable for diagnosis in all cases. Report compatibility showed good agreement with eighteen (86%) handheld image reports identical to the reference reports. Three cases had minor differences, which were of no clinical importance, while in one case an additional diagnosis was noted via the handheld images that had not been documented in the reference reports.
Although all three studies 28–30 demonstrated positive findings using handheld devices, none explicitly discussed the impact that the mobility of the device had on the study outcomes. For example, similar results may have been derived from the transfer of data to fixed computers. The impact of handheld devices in these studies focused on when investigatory images were accessible by the physician, and how these images could be accessed. The studies did not examine how well mobile devices facilitated easier and more frequent access to information from different work locations.
Communication
Aziz et al. 31 examined the use of handheld devices to facilitate interprofessional communication. Eight hospital-based physicians received, on alternate weeks during the 6 week study period, either a PDA with mobile phone functionality, or alternatively, a conventional pager. The study compared communication efficiency by measuring call response times for each device for random calls initiated by the researchers. After a 5-minute response interval, it was considered that physicians had failed to respond. The average response times were lower, and failures to respond occurred less often, using the PDA compared with the pager. The authors suggested that the PDA's mobile phone function can improve upon pagers, which require physicians to locate a phone to return a call. As such, the mobility of the handheld device directly impacted on physician work practices, specifically when a physician is able to respond to a call.
Handheld Devices Facilitating Medication Error Prevention
Five studies evaluated how handheld devices could allow hospital-based physicians to prescribe medications more safely and effectively (see Table 3, available as an online data supplement at http://www.jamia.org). Three of the five 33–35 assessed the impact of handheld decision support on prescribing practices, while two 36,37 examined use of handhelds for generating medication lists and prescriptions.
Decision Support
Berner et al., 33 Rudkin et al., 34 and Sintchenko et al. 35 conducted studies where the use of a decision support system (DSS), via a PDA, was designed to improve patient management by reducing unsafe or unnecessary prescribing. In all three studies, the handheld device primarily served as an information and decision support resource for use at the physicians' discretion. Subjects carried out documentation and prescribing separately. Berner et al. 33 evaluated the effectiveness of a DSS on the prescribing safety of nonsteroidal anti-inflammatory drugs (NSAIDs). They conducted an RCT with 31 physicians assigned to the intervention arm and 28 to the control arm. All physicians were given an author-developed, PDA-based DSS, with the intervention group receiving an additional NSAID-related risk assessment with real-time treatment recommendations. Standardized patients, trained to portray clinical conditions that could result in adverse outcomes with inappropriate NSAID prescription, presented to each participant at least once during 6-month baseline data collection, and once during 8 month follow-up. Safe and unsafe prescribing and documentation of key risk factors were determined through chart review by two clinicians blinded to participant group assignment. At baseline, unsafe prescribing was similar for the intervention and control groups [mean proportion of unsafe prescribing cases per physician 0.27 and 0.29 respectively (p > 0.05)]. The intervention rule significantly affected error rates [0.23 in the intervention group compared with 0.45 (p < 0.05)]. However, this was attributed to performance degradation in the control group, rather than a substantial improvement in the intervention group, whose performance remained relatively constant. The authors observed a significant association between obtaining key risk factors and safe prescribing. Intervention physicians who obtained this information provided no unsafe prescriptions.
Rudkin et al. 34 conducted a time-motion study that assessed physicians' accesses to resources and rates of change in patient management. Thirty physicians were observed on two occasions—once while using electronic resources via a PDA and once while using paper text resources. Physicians accessed electronic resources (n = 181) more often than paper resources (n = 131) (OR 1.99; CI 1.41–2.80), with similar average access times (9.3 and 9.4 secs respectively). Access times only reflected the time it took for physicians to find the necessary information within the relevant resource; time required to locate and obtain paper resources was not recorded. Changes in patient management were significantly higher using electronic resources [29.8% compared with 17.6% (OR 2.00; CI 1.11–3.60)], particularly for changes in drug type [21.5% compared with 13.0% (OR 1.84; CI 0.95–3.59)]. This result may reflect differences in information content available electronically versus in paper resources, such as drug interaction information, which was not available in paper format.
Sintchenko et al. 35 assessed the impact of information accessible via a handheld device on patient management. The authors conducted a 6 month prospective study during which twelve physicians received PDAs loaded with locally developed guidelines and site-specific laboratory data. The rate of antibiotic use and outcomes of patients in ICUs during the intervention period were compared with 6 months of historical data, during which no computerized DSS was available. The findings showed that on average the DSS was used four times per day during the study period, primarily to access laboratory data. A significant decrease of antibiotics used occurred. The preintervention consumption rate was 1,925 defined daily doses per 1,000 patient days, and decreased to 1,606 in the intervention period (p = 0.04). The average patient length of stay decreased significantly during DSS use [6.22 bed days compared with 7.15 bed days (p = 0.02)]. Registrars had higher levels of DSS use compared with consultants. Rudkin et al. 34 also noted a similar finding with less experienced physicians accessing information more frequently than their more senior colleagues.
Among these studies, 33–35 handhelds affected hospital physicians' work practices primarily through what information was accessible to them for informed decision making.
Medication Safety
Grasso et al. 36 and Shannon et al. 37 studied the impact of handheld devices on the electronic documentation of medications. Grasso et al. 36 compared error rates when nurses transcribed physicians' handwritten medication orders with those occurring when physicians directly entered medication orders into a PDA to generate patient discharge medications lists. The 110 hand transcribed lists and the 90 electronically generated medication lists were retrospectively reviewed for errors by a pharmacist. The findings showed significantly fewer errors with the electronically generated discharge lists (8%) compared with the hand transcribed lists (22%) (p < 0.05). The errors identified in the handheld-generated lists all involved erroneous exclusion of medications, while transcription errors were eliminated.
Medication error reduction, such as eliminating illegibility, was the impetus for a study by Shannon et al. 37 The authors attempted to increase electronic prescribing among nine emergency physicians by giving them handheld devices that could access the hospital's clinical information system. During the 3 month preintervention phase, handwritten and fixed computer prescribing were available. In the 1-week intervention period the additional method of prescribing via a handheld device was made available. The researchers hypothesized that leaving the patient's bedside to access a fixed computer and enter a prescription was inconvenient and thus hindered electronic prescribing. Seventy-eight preintervention prescriptions and 89 intervention prescriptions were reviewed. Introduction of handhelds significantly increased the average rate of electronic prescribing [64% intervention prescriptions v. 52% preintervention (p = 0.03)]. Half of the electronic prescriptions generated during the intervention period came from handheld devices, and half from the fixed computer. The study found a high degree of variability among individual physicians in the rate of electronic prescribing, ranging from none to all. The authors found that, rather than a preference for handwriting predicting handheld use, a prior preference for electronic prescribing via the fixed computer predicted subsequent handheld prescribing.
The Grasso et al. 36 and Shannon et al. 37 studies showed positive effects for use of handheld devices, with the impact of the handheld devices on hospital physicians' work practices focusing on how medications could be documented or prescribed to prevent errors and who performs these tasks.
Handheld Devices Facilitating Data Management and Accessibility
Four studies evaluated how handheld devices could facilitate hospital-based physicians in improving documentation of, and accessibility to, patient data during daily clinical routines (see Table 4, available as an online data supplement at http://www.jamia.org). Stengel et al., 38 Carroll et al., 39 Chan et al., 40 and VanDenKerkhof et al. 41 conducted studies in inpatient settings that compared standard paper documentation with electronic documentation via a handheld device. Two of the studies 38,39 investigated the impact of handheld devices on the quality of patient data documentation, while two 40,41 assessed the use of handheld devices for managing patient information.
Documentation and Information Access
Stengel et al. 38 conducted an RCT to determine whether handheld devices could beneficially impact the quantity and quality of documentation and coding of patient diagnoses. During the study, four physicians performed either conventional paper documentation or electronic documentation via a PDA for patients' history, clinical findings and treatments. Documented diagnoses were translated into standardized codes, manually for paper documentation but automated with electronic documentation. Thirty-nine patients were randomized to conventional paper documentation, and 38 to electronic documentation. Documentation via the handheld device recorded significantly more diagnoses per patient (median diagnoses = 9) compared with paper documentation (median = 4) (p < 0.0001). However, the rate of false or redundant codes was also higher with handhelds (11.7 vs. 4.5%). The findings remained significant even after the false codes were removed (p < 0.0001). Documentation quality was rated based on: regularly performed data entry; detailed depiction of clinical findings; and correct assessment of patients' progress and translation into standardized codes. The handheld device was rated as significantly better than conventional paper documentation on all aspects of data quality (respectively p = 0.004; p = 0.0045; and p = 0.0026).
Carroll et al. 39 conducted a before and after trial in a neonatal intensive care unit to determine whether a handheld-based patient record and charting system could reduce the prevalence of documentation discrepancies in daily progress notes. The authors analyzed 339 paper progress notes and 432 handheld-generated progress notes. They examined information about patients' weights, medications and vascular lines. A documentation discrepancy occurred when the information documented on the progress note did not match the information noted in the nursing flow sheet, assessment sheet or pharmacy medication administration record. Documentation via the handheld device resulted in significantly fewer documentation discrepancies of patient weight [14.4% compared with 4.4% (OR 0.29; CI 0.15–0.56)]. However, there were no significant changes in the number of progress notes with medication discrepancies [27.7% compared with 17.1% (OR 0.63; CI 0.35–1.13)] or vascular line discrepancies [33.6% compared with 36.1% (OR 1.11; CI 0.66–1.87)].
Chan et al. 40 and VanDenKerkhof et al. 41 assessed the use of handheld devices to document and access patient information during ward rounds in acute pain service settings. They compared duration of rounds pre- and post-implementation of electronic documentation. Chan et al. 40 provided one PDA for use among a clinical team. The device replaced the paper process, where physicians recorded demographic and clinical data on a form that was subsequently transcribed into a computer database. The PDA was synchronized daily with a fixed computer to transfer information to and from the database. The electronic data collection forms included prompts to ensure all mandatory data were entered. The study compared 60 paper documented visits to 68 electronically documented visits during a 3 month study period. No significant change occurred in the average duration of patient encounters [7.0 min for handhelds, compared with 8.8 min for paper processes (p = 0.151)].
Unlike Carroll et al. 39 and Chan et al., 40 who compared structured paper forms with structured electronic forms, VanDenKerkhof et al. 41 assessed the use of structured pain assessment forms on a handheld device and compared the encounter time and the comprehensiveness of the documentation with the standard unstructured paper process. Throughout the 3 week study period one physician performed 100 assessments on 44 patients using paper, where documentation was completed outside the patients' rooms. A further 94 assessments on 30 patients were performed using a PDA, during which documentation was completed at the patient's bedside. Completeness of documentation was assessed using the frequency of recorded pain variables (characterization, location and duration of pain) and the ten most common medication side effects. The median encounter time for each patient was significantly shorter with handheld documentation (227 secs, vs. 301 secs for paper) (p < 0.001). The frequency of documented side effects ranged from 5 to 100% for paper charting and 98% to 100% for recording via the handheld device. Pain variables were also more frequently documented via handhelds. The authors suggested that the difference in the comprehensiveness of the documentation might have occurred due to the location of the recording and the structure of the forms.
Although all four studies 38–41 demonstrated positive findings using handheld devices for documentation during daily clinical routines, only VanDenKerkhof et al. 41 explicitly stated that the mobility of the handheld device contributed to the study outcomes. The impact of handheld devices on hospital physicians' work practices in the VanDenKerkhof, et al 41 study focused on where documentation of patient data were completed. Stengel et al., 38 Carroll et al., 39 and Chan et al. 40 focused on how documentation could be performed to improve data quality.
Technical Features of Handheld Devices
Details about handheld devices provided in the studies varied widely (see Table 5, available as an online data supplement at http://www.jamia.org). Reported device manufacturers included: Nokia (n = 2); Palm (n = 2); Handspring (n = 1); Sony (n = 1); Psion (n = 1); Compaq (n = 1); and Handera (n = 1). Seven studies used devices that ran on the Palm Operating System (Palm OS), while three reported using Windows Embedded Compact (Windows CE) systems. Data transfer speeds showed substantial improvements over the 6-year period, from 9600 bit/sec in 200030 to 2 MB/sec in 2006. 37
Study authors developed the tested handheld software (or modified existing software) in seven of the 13 studies. The majority (n = 8) of studies documented technical difficulties, including: failed transmissions (n = 3); battery issues (n = 2); synchronization problems (n = 1); hospital network failure (n = 1); and device breakdown (n = 1). Touchscreen techniques (including stylus handwriting recognition capabilities, onscreen keyboard, drop down menus and check boxes) were the only type of data entry methods reported (n = 7). Some form of user training was provided in seven studies, including one study 37 where participants were only provided with brief instructions on device use.
Discussion
The Impact of Mobile Handheld Technology on Hospital Physicians' Work Practices and Patient Care
This systematic review reveals that the handheld technology may be beneficial in supporting hospital physicians' work practices and patient care through facilitation of (a) rapid response, (b) medication error prevention, and (c) data management and accessibility. Many of the benefits reported could also occur when desktop workstations are available.
In the area of rapid response, over half of the studies were conducted in emergency or critical care settings, where time delays can constrain treatment options and impact on patients' chances of recovery or even survival. 27,42 The studies showed that wireless transmission of investigatory patient data to the relevant physicians' handheld device was feasible for diagnosis 30 and could expedite treatment by allowing earlier notification, resource preparation and mobilization of staff. 28,29 Similar efficiency gains may be realized through the facilitation of interprofessional communication using handheld devices. The mobile phone functionality and multidirectional nature of PDAs overcame limitations of pagers. 31 Given the mobile and collaborative nature of medical work, 6,43–45 PDAs can help to improve accessibility to coworkers 31 and thus coordination of patient care.
The literature also showed improvements in patient management decisions through the use of electronic resources on handheld devices. Physicians accessed electronic resources more often than paper resources, possibly because physicians are limited in the types of paper resources they can feasibly carry. 33,34 A handheld device offers greater portability and provides a greater scope of up-to-date information, including drug interaction information, that may be more rapidly accessed from any location. 13–15,33,34 Thus, by providing information and decision support access at the point-of-need, which supports informed treatment decisions, 33,34 improved patient outcomes may be achieved. 35
The findings also indicated that medication error prevention could be facilitated by addressing problems of drug order illegibility and errors in transcription. 36,37 Direct input of medications onto a handheld device reduced errors in medication documentation and eliminated transcription errors. 36,37 Although similar results could be achieved through the direct input of medications onto a fixed computer they are generally not located near the patient's bedside. Researchers suggest that the inconvenience of leaving the bedside to locate an available computer hinders a physician's decision to use direct input via a desktop computer. 5,36,37 However, when provided with a choice of input method—paper, fixed computer, or handheld device—some physicians preferred to use a fixed desktop computer located away from the patients bedside rather than using a handheld device at the point of care. 36,37 Evidence showing that entering data onto a PDA via a stylus is slower, more erroneous and less satisfactory for users than entering data via a QWERTY keyboard 46 may explain this preference.
Nonetheless, in the area of data management and accessibility, the evidence showed the use of handheld devices to be at least as effective and efficient as paper processes. 38–41 The studies demonstrated improvements in documentation quality with an increased recording of diagnoses 38 and a reduction in documentation discrepancies. 39 As most patient information is obtained at the bedside 3,8,11,47 providing physicians with devices that allow data entry at the point of care can promote more complete documentation 41 and decrease the length of patient encounters. 40,41 These findings are important given that decision-making may be compromised not only by incorrect data, but also data not entered in a timely fashion. 5 Therefore, having portable, complete, accurate and up-to-date patient specific information could facilitate more complete, accurate and timely patient management. 48,49
Ability of Handheld Devices to Support Mobile Work Practices
In 2003, Fischer et al. 16 sought to raise physician awareness of handheld computers in medicine, but also noted the lack of substantial evidence about the use of these devices and their impact on health care delivery. 16 The continuing paucity of evidence in this area was identified in three subsequent reviews. 12,50,51 The current review is the first to focus on evidence of the role of handheld devices in supporting the mobile work practices of hospital physicians. We identified only four of 13 studies where the role of device mobility was directly commented upon by researchers. Thus, we adopted a broad analysis framework to carefully examine and identify contextual factors (either implicit or explicit) impacting on physician mobile work practices that can improve understanding of the areas that mobile technology affects. 52,53 We used the definition of Badram et al. 3 of mobility as the “work needed to achieve the right configuration of people, resources, knowledge and place” as a prism through which to examine and identify domains of physician work mobility (i.e., what is being done, when is it occurring, how is it being done and where is it happening).
Hospitals are complex and busy places involving constant shifts and movement of people and things (resources, information) that are distributed within different areas at different times for diverse requirements. 2 ▶ illustrates the interconnectedness of these factors, recognized as important to clinical workflow, 54 and identifies their relationship with key themes uncovered in this review. The studies that focused on prompt treatment of patients within the ED, addressed issues related to the impact of handheld technology on the timing or availability (when) of accessible images with a corresponding focus on the available resources (how) that allowed these images to be accessible. 28–30 The Aziz et al. 31 study, which concentrated on the use of PDAs to accentuate interprofessional communication, dealt with issues related to the availability (when) of a given resource. Conversely, decision support facets of handheld technology primarily addressed issues related to the accessibility of knowledge (what) resources 33–35 and medication safety elements were related to medication documentation processes (how) and responsibility (who). 36,37 The studies that addressed data management focused either on issues related to the location (where) documentation occurred 41 or the method (how) of documentation. 38–41 Using this framework it is interesting (and somewhat ironic) that only one of the included studies 41 expressly observed where handheld device use occurred and addressed the subsequent impact the location had on the study outcomes.
Figure 3.
Key areas of handheld technology impact as they relate to issues of mobility in the clinical workplace.
Although many studies alluded to the mobility of the handheld device for “point-of-care”, 33,39 “bedside”, 34,37 or “just in time” 35 use, none of these studies specifically measured whether the devices were used in this manner. The extent to which handheld devices support mobile work processes was often not clearly portrayed. Many studies also failed to distinguish the benefits of providing physicians with a mobile handheld device over a desktop computer platform, with less than one third of studies explicitly stating that the mobility of the handheld device contributed to the study outcomes. Sintchenko et al. 35 adequately summarize the shortcomings of many studies on handheld devices when referring to their own inability “to identify the specific contributions of using a handheld platform over [a] fixed platform to the study results.”
The Status of Handheld Devices in Clinical Practice
Handheld devices possess the advantages of being portable 12 and allowing access to information anywhere and at any time. 11 But does this mobility of information and resources lead to improved outcomes, and if so when and in what context? The available evidence suggests that mobile handheld devices demonstrate the greatest benefits in contexts where time is a critical factor and a rapid response is crucial, for example prehospital notification of vital patient data. 28,29 They are also beneficial in connecting spatially distributed coworkers. Health care work is highly interconnected and health care practitioners are dependent on their coworkers skills, knowledge, and expertise. 54 Thus, improving communication with and accessibility to coworkers allows physicians to deliver “faster, more efficient patient care” 31 with potential benefits to patient outcomes.
Mobile handheld devices are also effective for overcoming difficulties created by inadequate numbers of available of fixed desktop computers. Fixed computers provide access to electronic information systems but, due to the highly mobile nature of hospital work, physicians are limited in their ability to regularly check information only available on fixed computers. Electronic messages or decision support alerts will be ineffective if physicians do not receive them. 54 Additionally, fixed computers located away from patients' bedsides may result in workflow interruptions, 54 additional work such as duplicate documentation (first on paper then on the computer) 40,54 or less comprehensive data collection. 41 Mobile handheld devices potentially provide a solution allowing both direct input and viewing of data at the point of care, increasing the opportunities for physicians to gain value from electronic information systems. However, as this review has demonstrated, there is little evidence to confirm that mobile devices will be used at this location and in the ways expected. A recent observational study of physicians' use of tablet computers during ward rounds demonstrated that while the tablet computers provided the ability to access and document information at a patient's bedside, physicians chose to complete most computer tasks on the tablet in the corridor of the ward. 55 Such results challenge assumptions about how physicians will use mobile technologies in situ.
Mobile handheld devices have some limitations. Their smaller screens are designed for individual use 56,57 which can make collaboration difficult 3,11 and they present challenges in easily viewing and entering data. 46,55 The limitations and potentially error-inducing features of computer screens, which may include limiting a full overview of patient information, or hiding important information behind menus, 58 will be exacerbated on a PDA screen. Nonetheless, available evidence suggests that handheld devices have some advantages over both paper and fixed computers in supporting physician hospital work practice in situations when: rapid information exchange is required and will influence patient care decisions; where physicians are undertaking highly mobile work which reduces their ability to spend periods in a fixed place where they can access electronic resources via fixed computers; and where data entry or access is required at the point of care and that the absence of these capabilities will reduce the efficiency or effectiveness of care delivery.
Mobile technology is still an emerging and rapidly developing area of study. 12 Existing literature has a tendency to view the mobility of any device as inherently beneficial without clear evidence demonstrating how, why or in what circumstances this mobility provides value. What is required is a more evidence-based approach to the use and evaluation of mobile technologies to understand if, and when, they are useful in supporting clinical practice and improvements in care delivery. The framework that we used to examine and identify domains of physician work mobility provides a useful lens by which to assess the role of mobile technology in supporting improved health care delivery and understanding what will work, for whom, where, and in what circumstances. 59 The results from this review contribute to providing a foundation upon which to refocus future studies of mobile technologies.
Those seeking to implement mobile handheld technologies in a hospital setting should consider questions of why and how the mobile device is expected to improve care delivery because of its core “mobility” asset. Further, how handheld devices might compare with other mobile devices, such as laptops or computers on wheels, should be considered. It is likely that securing the integration of the “right” combination of mobile, fixed and paper information sources is required to achieve the best outcomes for both health care staff and their patients. 3,8,11,47 This requires understanding and acknowledging both the advantages and disadvantages of various technologies, how they are used in real-work clinical situations, and the contextual factors which determine their use.
Technical Features of Handheld Devices
The outcomes associated with the implementation of ICT systems within the context of one institution may not always be applicable to another healthcare setting. 5 To address such issues studies assessing ICT systems should aim to clearly describe the IT artifact being evaluated. 60 The level of detail regarding the handheld devices used within the included studies varied considerably. Information regarding intended and actual use, functionality, and infrastructure was limited across the studies, however most provided software and hardware details, and information about the number of users, their experience and training. The benefits of handheld devices to hospital physicians will be influenced by the extent to which they are stand alone, connected to the Internet or to the hospital's electronic information systems. Few studies in the review revealed such details, but such information is important to allow comparisons of the impact of different devices or features.
Limitations
Despite a comprehensive search only a limited number of quantitative articles which investigated the impact of handheld devices on hospital physicians' work practices and patient care were identified. We sought to include tablet computers in the review but found no studies investigating this mobile handheld technology that met the review criteria, further demonstrating the dearth of research on this topic. We did not exclude articles based on an assessment of their quality and thus the limitations associated with the literature included in this review may impede the conclusions drawn. The heterogeneity of the outcome measures assessed within the included literature made synthesis difficult and precluded the use of meta-analysis techniques. Despite the rapidly evolving nature of handheld technology the central themes identified in this review, in particular the need to more specifically address how any new handheld device actually delivers upon its goal of supporting mobile health care work, remain current.
Conclusions
This review identified evidence about the ability of mobile handheld technology to positively impact rapid response, error prevention, information accessibility, and data management in healthcare settings. The study findings support claims of the potential beneficial impact of this technology on aspects of healthcare delivery. However, the extent to which handheld devices provide benefits due to their mobility has been significantly underinvestigated. The mobility framework applied in this review is grounded in the reality of everyday clinical practice where people are involved in the constant pursuit of achieving the optimal mix of individuals, resources, and knowledge, at the desired time. 2 We believe this framework provides a useful lens by which to assess the role of handheld device use in supporting improved healthcare delivery and better patient outcomes. Prior to widespread adoption of mobile technologies in hospitals, implementers and adopters should address explicit questions about why and how the mobility of these devices is expected to improve care delivery. Pilot observational studies should test assumptions about how mobile technologies will be used in practice to support the work of physicians.
Footnotes
This work was supported by an ARC Linkage grant LP0989144. MP is supported by an APA scholarship. The authors thank the JAMIA editorial office for its helpful suggestions and advice.
References
- 1.Bardram JE. Activity-based computing: Support for mobility and collaboration in ubiquitous computing Pers Ubiquit Comput 2005;9(5):312-322. [Google Scholar]
- 2.Bardram JE, Bossen C. Mobility work: The spatial dimension of collaboration at a hospital Comput Support Coop Work 2005;14(2):131-160. [Google Scholar]
- 3.Ammenwerth E, Buchauer A, Bludau B, Haux R. Mobile information and communication tools in the hospital Int J Med Inform 2000;57(1):21-40. [DOI] [PubMed] [Google Scholar]
- 4.Banitsas KA, Georgiadis P, Tachakra S, Cavouras D. Using handheld devices for real-time wireless teleconsultation Conf Proc IEEE Eng Med Biol Soc 2004;4:3105-3108. [DOI] [PubMed] [Google Scholar]
- 5.Baldwin LP, Low PH, Picton C, Young T. The use of mobile devices for information sharing in a technology-supported model of care in AE Int J Electron Healthc 2006;3(1):90-106. [DOI] [PubMed] [Google Scholar]
- 6.Reddy MC, McDonald DW, Pratt W, Shabot MM. Technology, work, and information flows: Lessons from the implementation of a wireless alert pager system J Biomed Inform 2005;38(3):229-238. [DOI] [PubMed] [Google Scholar]
- 7.Sellen AJ, Harper RHR. The Myth of the Paperless Office. Cambridge, MA: MIT Press; 2002.
- 8.Luff P, Heath C. Mobility in collaboration Proceedings of the 1998 ACM Conference on Computer Supported Cooperative Works: Seattle, WA 1998:305-314.
- 9.Bardram JE, Bossen C. Moving to get ahead: Local mobility and collaborative work Proceedings of the 8th European Conference on Computer Supported Cooperative Works: Helsinki, Finland 2003:355-374.
- 10.McCord G, Smucker WD, Selius BA, et al. Answering questions at the point of care: Do residents practice EBM or manage information sources? Acad Med 2007;82(3):298-303. [DOI] [PubMed] [Google Scholar]
- 11.Dahl Y, Svanaes D, Nytro O. Designing pervasive computing for hospitals: Learning from the media affordances of paper-based medication charts Pervasive Health Conference and Workshops 2006:1-10.
- 12.Kuziemsky CE, Laul F, Leung RC. A review on diffusion of personal digital assistants in healthcare J Med Syst 2005;29(4):335-342. [DOI] [PubMed] [Google Scholar]
- 13.Baumgart DC. Personal digital assistants in health care: Experienced clinicians in the palm of your hand? Lancet 2005;366(9492):1210-1222. [DOI] [PubMed] [Google Scholar]
- 14.Garritty C, El Emam K. Who's using PDAs?. Estimates of PDA use by health care providers: A systematic review of surveys. J Med Internet Res 2006;8(2):7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Cole E, Pisano ED, Clary GJ, et al. A comparative study of mobile electronic data entry systems for clinical trials data collection Int J Med Inform 2006;75(10–11):722-729. [DOI] [PubMed] [Google Scholar]
- 16.Fischer S, Stewart TE, Mehta S, Wax R, Lapinsky SE. Handheld computing in medicine J Am Med Inform Assoc 2003;10(2):139-149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lu YC, Xiao Y, Sears A, Jacko JA. A review and a framework of handheld computer adoption in healthcare Int J Med Inform 2005;74(5):409-422. [DOI] [PubMed] [Google Scholar]
- 18.Lindquist MA, Johansson EP, Petersson IG, Saveman BI, Nilsson CG. The use of the personal digital assistant (PDA) among personnel and students in health care: A review J Med Internet Res 2008;10(4):31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Martins HMG, Jones MR. What's so different about mobile information communication technologies (MICTs) for clinical work practices?. A review of selected pilot studies. Health Inform J 2005;11(2):123-134. [Google Scholar]
- 20.Jackson N, Waters E. Criteria for the systematic review of health promotion and public health interventions Health Promot Int 2005;20(4):367-374. [DOI] [PubMed] [Google Scholar]
- 21.Car J, Black A, Anandan C, et al. The impact of eHealth on the quality and safety of healthcare: A systematic overview and synthesis of the literature, LondonUniversity of Edinburgh and the Imperial College London; 2008.
- 22.Counsell C. Formulating questions and locating primary studies for inclusion in systematic reviews Ann Intern Med 1997;127(5):380-387. [DOI] [PubMed] [Google Scholar]
- 23.Whittemore R, Knafl K. The integrative review: Updated methodology J Adv Nurs 2005;52(5):546-553. [DOI] [PubMed] [Google Scholar]
- 24.Crowther MA, Cook DJ. Trials and tribulations of systematic reviews and meta-analyses Hematology 2007 2007;1:493-497. [DOI] [PubMed] [Google Scholar]
- 25.Greenhalgh T. How to read a paper: Papers that summarise other papers (systematic reviews and meta-analyses) BMJ 1997;315(7109):672-675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Bates DW, Gawande AA. Improving safety with information technology N Engl J Med 2003;348(25):2526-2534. [DOI] [PubMed] [Google Scholar]
- 27.Bardram JEIL. The system—I just don't use it!Proceedings of the International ACM SIGGROUP Conference on Supporting Group WorkPhoenix, AZ: The Integration Challenges; 1997. pp. 251-260.
- 28.Adams GL, Campbell PT, Adams JM, et al. Effectiveness of prehospital wireless transmission of electrocardiograms to a cardiologist via hand-held device for patients with acute myocardial infarction (from the timely intervention in myocardial emergency, northeast experience (TIME-NE)) Am J Cardiol 2006;98(9):1160-1164. [DOI] [PubMed] [Google Scholar]
- 29.Clemmensen P, Sejersten M, Sillesen M, et al. Diversion of ST-elevation myocardial infarction patients for primary angioplasty based on wireless prehospital 12-lead electrocardiographic transmission directly to the cardiologist's handheld computer: A progress report J Electrocardiol 2005;38(4):194-198(Suppl). [DOI] [PubMed] [Google Scholar]
- 30.Reponen J, Ilkko E, Jyrkinen L, et al. Initial experience with a wireless personal digital assistant as a teleradiology terminal for reporting emergency computerized tomography scans J Telemed Telecare 2000;6(1):45-49. [DOI] [PubMed] [Google Scholar]
- 31.Aziz O, Panesar SS, Netuveli G, et al. Computers and the 21st century surgical team: A pilot study BMC Med Inform Decis Mak 2005;5:28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Andersen HR, Nielsen TT, Rasmussen K, et al. A comparison of coronary angioplasty with fibrinolytic therapy in acute myocardial infarction N Engl J Med 2003;349(8):733-742. [DOI] [PubMed] [Google Scholar]
- 33.Berner ES, Houston TK, Ray MN, et al. Improving ambulatory prescribing safety with a handheld decision support system: A randomized controlled trial J Am Med Inform Assoc 2006;13(2):171-179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Rudkin SE, Langdorf MI, Macias D, Oman JA, Kazzi AA. Personal digital assistants change management more often than paper texts and foster patient confidence Eur J Emerg Med 2006;13(2):92-96. [DOI] [PubMed] [Google Scholar]
- 35.Sintchenko V, Iredell JR, Gilbert GL, Coiera E. Handheld computer-based decision support reduces patient length of stay and antibiotic prescribing in critical care J Am Med Inform Assoc 2005;12(4):398-402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Grasso BC, Genest R, Yung K, Arnold C. Reducing errors in discharge medication lists by using personal digital assistants Psychiatr Serv 2002;53(10):1325-1326. [DOI] [PubMed] [Google Scholar]
- 37.Shannon T, Feied C, Smith M, Handler J, Gillam M. Wireless handheld computers and voluntary utilization of computerized prescribing systems in the emergency department J Emerg Med 2006;31(3):309-315. [DOI] [PubMed] [Google Scholar]
- 38.Stengel D, Bauwens K, Walter M, Kopfer T, Ekkernkamp A. Comparison of handheld computer-assisted and conventional paper chart documentation of medical records: A randomized controlled trial J Bone Joint Surg 2004;86(3):553-560. [DOI] [PubMed] [Google Scholar]
- 39.Carroll AE, Tarczy-Hornoch P, O'Reilly E, Christakis DA. Resident documentation discrepancies in a neonatal intensive care unit Pediatrics 2003;111(5):976-980. [DOI] [PubMed] [Google Scholar]
- 40.Chan SS, Chu CP, Cheng BC, Chen PP. Data management using the personal digital assistant in an acute pain service Anaesthesiol Intens Care 2004;32(1):81-86. [DOI] [PubMed] [Google Scholar]
- 41.VanDenKerkhof EG, Goldstein DH, Lane J, Rimmer MJ, Van Dijk JP. Using a personal digital assistant enhances gathering of patient data on an acute pain management service: A pilot study Can J Anesth 2003;50(4):368-375. [DOI] [PubMed] [Google Scholar]
- 42.Ikeya N. Practical management of mobility: The case of the emergency medical system Environ Plann A 2003;35(9):1547-1564. [Google Scholar]
- 43.Coiera E, Tombs V. Communication behaviours in a hospital setting: An observational study BMJ 1998;316(7132):673-676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Eisenstadt S, Wagner M, Hogan W, et al. Mobile workers in healthcare and their information needs: Are 2-way pagers the answer? AMIA Annu Symp Proc 1998:135-139. [PMC free article] [PubMed]
- 45.Reddy MC, Pratt W, McDonald DW, Shabot MM. Challenges to physicians' use of a wireless alert pager AMIA Annu Symp Proc 2003:544-548. [PMC free article] [PubMed]
- 46.Haller G, Haller DM, Courvoisier DS, Lovis C. Handheld versus laptop computers for electronic data collection in clinical research: A cross-over randomized trial J Am Med Inform Assoc. . JAMIA PrePrint. 30June2009. doi: 10.1197/jamia.M3041. [DOI] [PMC free article] [PubMed]
- 47.Moran EB, Tentori M, Gonzalez V, et al. Mobility in hospital work: Towards a pervasive computing hospital environment Int J Electron Healthc 2006;3(1):72-89. [DOI] [PubMed] [Google Scholar]
- 48.Lau F, Yang J, Pereira J, Daeninck P, Aherne M. A survey of PDA use by palliative medicine practitioners J Palliat Care 2006;22(4):267-274. [PubMed] [Google Scholar]
- 49.Criswell DF, Parchman ML. Handheld computer use in US family practice residency programs J Am Med Inform Assoc 2002;9(1):80-86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Kho A, Henderson LE, Dressler DD, Kripalani S. Use of handheld computers in medical education: A systematic review J Gen Intern Med 2006;21(5):531-537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Mendonça EA, Chen ES, Stetson PD, et al. Approach to mobile information and communication for health care Int J Med Inform 2004;73(7–8):631-638. [DOI] [PubMed] [Google Scholar]
- 52.Pawson R, Greenhalgh T, Harvey G, Walshe K. Realist review—A new method of systematic review designed for complex policy interventions J Health Serv Res Policy 2005;10(Suppl 1):21-34. [DOI] [PubMed] [Google Scholar]
- 53.Greenhalgh T, Kristjansson E, Robinson V. Realist review to understand the efficacy of school feeding programmes BMJ 2007;335(7625):858-861. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Niazkhani Z, Pirnejad H, Berg M, Aarts J. The impact of computerized provider order entry systems on inpatient clinical workflow: A literature review J Am Med Inform Assoc 2009;16(4):539-549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Andersen P, Lindgaard A-M, Prgomet M, Creswick N, Westbrook J. Is selection of hardware device related to clinical task?. A multi-method study of mobile and fixed computer use by doctors and nurses on hospital wards. J Med Internet Res 2009;11(3):e32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Gurses AP, Xiao Y. A systematic review of the literature on multidisciplinary rounds to design information technology J Am Med Inform Assoc 2006;13(3):267-276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Dryer DC, Eisbach C, Ark WS. At what cost pervasive?. A social computing view of mobile computing systems. IBM Syst J 1999;38(4):652-676. [Google Scholar]
- 58.Koppel R, Wetterneck T, Telles J, Karsh B. Workarounds to barcode medication administration systems: Their occurrences, causes, and threats to patient safety J Am Med Inform Assoc 2008;15(4):408-423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Pawson R, Tilley N. Realistic Evaluation. London: Sage Publications; 1997.
- 60.Ammenwerth E, Graber S, Herrmann G, Burkle T, Konig J. Evaluation of health information systems—Problems and challenges Int J Med Inform 2003;71(3):125-135. [DOI] [PubMed] [Google Scholar]