Abstract
Background
Letter-by-letter readers identify each letter of the word they are reading serially in left to right order before recognizing the word. When their letter naming is also impaired, letter-by-letter reading is inaccurate and can render even single word reading very poor. Tactile and/or kinesthetic strategies have been reported to improve reading in these patients, but only under certain conditions or for a limited set of stimuli.
Aims
The primary aim of the current study was to determine whether a tactile/kinesthetic treatment could significantly improve reading specifically under normal reading conditions, i.e. reading untrained words presented in free vision and read without overt use of the strategy.
Methods & Procedures
Three chronic letter-by-letter readers participated in a tactile/kinesthetic treatment aimed at first improving letter naming accuracy (phase 1) and then letter-by-letter reading speed (phase 2). In a multiple case series design, accuracy and speed of reading untrained words without overt use of the trained tactile/kinesthetic strategy was assessed before phase 1, after phase 1 and again after phase 2.
Outcomes & Results
All three patients significantly improved both their speed and accuracy reading untrained words without overt use of the trained tactile/kinesthetic strategy. All three patients required the additional practice in phase 2 to achieve significant improvement. Treatment did not target sentence level reading, yet two of the three patients became so adept that they could read entire sentences.
Conclusions
This study replicates previous findings on the efficacy of tactile/kinesthetic treatment for letter-by-letter readers with poor letter naming. It further demonstrates that this treatment can alter cognitive processing such that words never specifically trained can be read in free vision without overtly using the trained strategy. The data suggest that an important element in achieving this level of generalization is continuing training beyond the point of initial mastery (i.e. accurate letter naming).
Keywords: aphasia, cognitive rehabilitation, Speech-Language Pathology, pure alexia, letter-by-letter reading, generalization
Patients with pure alexia demonstrate a reading length effect in which shorter words are read more quickly and/or more accurately than are longer ones. These patients often read in letter-by-letter fashion in which they name each letter of a word in left to right order before recognizing the word. Various other orthographic tasks, however, remain intact. Patients with pure alexia are able to recognize words that are spelled aloud to them and they are able to spell words that they cannot read. In cognitive processing terms, this deficit is believed to result from impairment somewhere along the route from visual processing to lexical access, at the letter identification stage (Kay & Hanley, 1991; Bub, Black, & Howell, 1989; Friedman & Hadley, 1992; Arguin, Fiset, & Bub, 2002). The orthographic lexicon itself remains intact. Reading is impaired because it requires access to orthography via the impaired visual route. Other tasks that do not require visual access to orthography, such as spelling words or recognizing words that are spelled aloud, remain well preserved.
Some patients with pure alexia, however, also have impaired letter naming rendering their letter-by-letter reading inaccurate. Previous research has demonstrated that such patients are able to use tactile and/or kinesthetic input to improve their letter naming. For example, patients have been trained to invoke kinesthetic input by copying, then naming, each letter of a word in sequence and then recognizing the word they thereby orally spelled (Goldstein, 1948; Luria, 1970; Stachowiak & Poeck, 1976), or to use a combination of tactile and kinesthetic input by tracing embossed or sandpapered letters (Godwin, 1983; Kreindler & Ionasescu, 1961; LaPointe & Kraemer, 1983). More recently, Sage, Hesketh & Lambon Ralph (2005) reported a solely tactile approach in which a helper traced each letter onto the patient’s hand and said the letter name, which the patient then repeated. Letter naming did not improve for this patient, perhaps suggesting that a kinesthetic component is necessary. Several additional studies in the literature, discussed in the paragraphs that follow, attribute some degree of improved reading to a tactile/kinesthetic treatment for pure alexia. None of these studies, however, has demonstrated a clear generalization of the treatment effect to reading in normal conditions, i.e. reading untrained words presented in free vision without overt use of the particular tactile/kinesthetic strategy that was trained.
Some studies have reported improved reading accuracy, but only with overt use of a tactile/kinesthetic strategy (Lott, Friedman, & Linebaugh, 1994; Maher, Clayton, Barrett, Schober-Peterson, & Gonzalez-Rothi, 1998). Lott et al. (1994) trained a patient with pure alexia to copy each letter onto his left palm with a capped pen and then name it, and then to read words using this letter-by-letter reading method. After approximately five months of treatment, the patient improved his reading of untrained words (i.e. words that were not practiced during training) from 40% to 78% correct. There was no mention of the patient’s reading accuracy when not overtly using the trained tactile/kinesthetic strategy, nor of his reading speed. Maher et al. (1998) trained a patient to trace the shape of each letter on a hard surface with her right index finger until she had traced all letters in the word. The patient reportedly did not need to name the letters aloud. She was trained to use this kinesthetic method reading sentences containing five or six words. Training was conducted four times per week over a period of four weeks. She improved her speed of reading untrained sentences from 19.9 words/min to 44.6 words/min. However, the authors specifically stated that the patient was “no more able to recognize visual letters at the end of the study period than she was at the beginning” (p.645), but rather that she needed to overtly use the trained kinesthetic strategy.
Several other studies have reported improved reading even without overt use of a tactile/kinesthetic strategy, but only for specific stimuli. Kashiwagi and Kashiwagi (1989) reported results for a patient with pure alexia who was trained four times per week over a period of five months to copy Japanese characters and then read them aloud. The patient succeeded in improving his reading of some, but not all, characters without overt use of the trained kinesthetic strategy. The authors suggested that successful reading without overt use of the trained strategy might have been limited to characters having only a few pen strokes. There was no report of reading speed. Seki, Yajima & Sugishita (1995) reported two patients who were trained to read Japanese characters by copying them with the right index finger. After 3 sessions for patient TK and 20 for KS, both patients improved their reading of the trained characters when not overtly using the trained kinesthetic strategy. Reading of some untrained words improved in tachistoscopic reading conditions, however, reading of untrained stimuli in free vision, was not reported.
Lott and Friedman (1999) did report their patient’s performance reading untrained words without a tactile/kinesthetic strategy. The paradigm built upon their 1994 study to include not only tactile-kinesthetic letter naming, but also a second phase of treatment aimed at speeding up letter-by-letter reading. Following the initial letter naming treatment, they observed that although their patient had improved his reading accuracy on untrained words, he remained painfully slow at reading. The rapid letter-by-letter reading treatment targeted his reading speed. Following this second phase of treatment, they directly compared his reading of a list of untrained words presented in free vision under two conditions: when overtly using the trained tactile/kinesthetic strategy and when not allowed to overtly use it (the patient was instructed to sit on his hands). Results showed that patient DL had become both more accurate, and faster, reading untrained words with the trained tactile/kinesthetic strategy than when reading without it. Unfortunately, the word list used to compare his reading with and without that strategy was not administered prior to treatment, so no direct assessment of any improvement in reading untrained words without overt use of that strategy could be made. Nevertheless, it is likely that there was considerable improvement: following treatment his reading without the trained tactile/kinesthetic strategy was 68% accurate and at a rate of 12.5 s/word (low frequency words 4–6 letters in length), while his baseline performance on words of similar length and frequency was 20–40% correct and at a rate of 32–40 s/word. We designed the current study to more carefully evaluate the effects of this treatment on reading without overt use of a tactile/kinesthetic strategy, by assessing the same list of untrained words before treatment, following tactile-kinesthetic letter naming and again following rapid letter-by-letter reading treatment.
In summary, while several reports in the literature have claimed significant reading improvement following a tactile and/or kinesthetic treatment, it has yet to be demonstrated that those improvements generalized to the reading of untrained words under normal reading conditions and without the use of the trained strategy. Sometimes improvements were demonstrated only with overt use of the trained tactile/kinesthetic strategy or only on specific stimuli, or they were measured only when words were presented very rapidly. The purpose of the current study, therefore, was to determine whether a tactile-kinesthetic treatment can significantly improve reading under normal reading conditions. Specifically, we assessed reading untrained words presented in free vision and read without overt use of a tactile/kinesthetic strategy. Based on results from the first patient, additional testing was administered to the two subsequent patients in order to evaluate a secondary question: whether additional practice naming letters rapidly is sufficient to achieve this level of word reading improvement, or whether subsequent training at the word level is necessary.
Method
Case Histories
Patient 1
LDR is a 61-year-old right-handed male with a bachelor’s degree. He was working as the head of his own general construction and contracting company when he suffered a myocardial infarction, followed by a left CVA during quadruple bypass surgery, two years prior to this study. No CT scans or Neurology reports were in his medical record. Prior to admission into this study LDR’s wife reported that he had retired due to the deficits caused by his stroke, including an inability to see things on his right side or to read even his own name.
Assessment based on the Boston Diagnostic Aphasia Examination (BDAE-3) (Goodglass, Kaplan, & Barresi, 2001) and the Boston Naming Test (BNT-2) (Kaplan, Goodglass, & Weintraub, 2001) revealed a fluent aphasia. Word finding was intact for responsive naming (20/20), conversation and picture description, but mildly impaired for confrontation naming (BNT 45/60). Repetition was intact at the single word (10/10) and sentence levels (10/10). Auditory comprehension was within functional limits (basic word discrimination 36.5/37, commands 14/15, complex ideational material 12/12). Single word oral reading was severely impaired (0/30), with unsuccessful letter-by-letter reading attempted, while spelling was relatively intact (primer words 6/6, regular phonics 4/5, and irregular forms 5/5). See Table 1 for full scores.
Table 1.
Diagnostic BDAE Scores for patients LDR, DBR and IND.
| BDAE Subtest | Patient |
Max Score |
|||
|---|---|---|---|---|---|
| LDR 2 years Post onset |
DBR 2 years Post onset |
IND 13 Months Post onset |
|||
| Severity | 5 | 5 | 5 | 5 | |
| Fluency | |||||
| Phrase Length | 7 | 7 | 7 | 7 | |
| Melodic Line | 7 | 7 | 7 | 7 | |
| Grammatical Form | 7 | 7 | 7 | 7 | |
| Auditory Comprehension | |||||
| Basic word discrimination | 36.5 | 29.5 | 31 | 37 | |
| Commands | 14 | 11 | 15 | 15 | |
| Complex Ideational Material | 12 | 10 | 11 | 12 | |
| Recitation | |||||
| Automatic Sequences | 8 | 8 | 8 | 8 | |
| Repetition | |||||
| Words | 10 | 10 | 9 | 10 | |
| Sentences | 10 | 8 | 10 | 10 | |
| Naming | |||||
| Responsive naming | 20 | 19 | 20 | 20 | |
| Boston Naming Test | 46 | 13 | 6 | 60 | |
| Special categories | 11 | 5 | 9 | 12 | |
| Reading | |||||
| Matching Case & Scripts | 7 | 5 | 6 | 8 | |
| Number Matching | 11 | 10 | 12 | 12 | |
| Word/Picture match | 7 | 6 | 0 | 10 | |
| Lexical Decision | 0 | 3 | 3 | 5 | |
| Homophone Matching | 2 | 2 | 0 | 5 | |
| Free Grammatical Morphemes | 10 | 9 | 0 | 10 | |
| Oral word reading | 0 | 1 | 16 | 15 | |
| Oral sentence reading | 0 | 0 | 0 | 10 | |
| Oral Sentence comprehension | 0 | 0 | 0 | 5 | |
| Sentence/paragraph | 0 | 1 | 0 | 10 | |
| Writing | |||||
| Form | 16 | 13 | 16 | 18 | |
| Letter Choice | 23 | 23 | 23 | 27 | |
| Motor Facility | 17 | 9 | 16 | 18 | |
| Primer Words | 6 | 6 | 6 | 6 | |
| Regular Phonics | 4 | 2 | 5 | 5 | |
| Common Irregular Words | 5 | 5 | 2 | 5 | |
| Written Picture Naming | 6 | 0 | 4 | 12 | |
| Narrative Writing | 0 | 0 | 4 | 11 | |
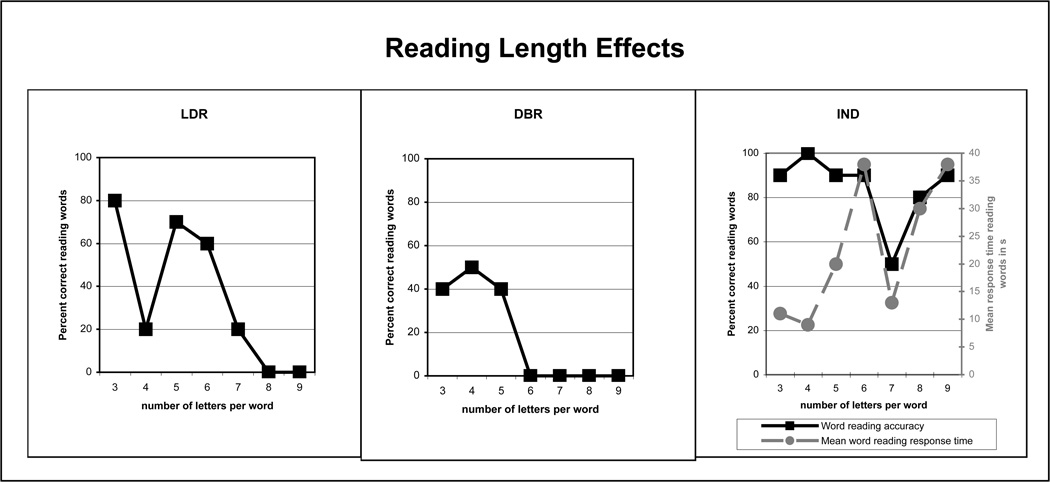
LDR’s reading was further evaluated with a battery of reading and related tests designed to assess his letter knowledge, oral reading and spelling abilities. His letter naming was impaired (20/26 lower case). He demonstrated better performance identifying letters given their names (25/26 lower case), identifying whether letters were presented in their correct or mirror image orientation (51/52) and matching letters across case (47/52). He demonstrated a marked length effect in his reading (see figure 1). He did not have any greater difficulty reading pseudowords than matched, real words (12/20 and 13/20, respectively), and his reading showed no effect of part of speech, although this could have been obscured by a floor effect (nouns 2/8, adjectives 1/8, verbs 1/8, functors 2/8). His spelling and recognition of oral spelling were far superior to his reading (32/32 and 33/40, respectively, compared with 6/32 and 2/40 reading the same lists of words, respectively). Based on his letter-by-letter reading, length and modality effects, LDR was diagnosed with pure alexia.
Figure 1.
Word reading length effects of the three patients. Patients DBR and LDR demonstrated length effects in their reading accuracy. Patient IND did not demonstrate a typical length effect as measured by his reading accuracy, but did as measured by reading response time (dashed line). Note that IND’s data for 7-letter words show a speed-accuracy trade off.
Patient 2
DBR is an 84-year-old right-handed female with a master’s degree. She was a retired high school English teacher who sustained an intracerebral hemorrhage more than two years prior to this study. Initial CT scan revealed evidence of a left posterior parieto-occipital region hemorrhage. Eight months later she sustained a TIA resulting in slurred speech and confusion that resolved quickly. CT scan from that time showed an old left occipital infarct with extension to both temporo-occipital and parieto-occipital junction and stenosis of the distal left middle cerebral artery with the remainder of the circle of Willis appearing broadly patent. A follow-up CT scan at 14 months post-onset revealed evidence of atrophy and malacia involving the left lateral occipital and posterior temporal region and deficient posterior left MCA branches, all consistent with her original infarct. With no prior history of hypertension or DM, the cause of her hemorrhage was attributed to probable amyloid angiopathy.
Upon admission to the study, DBR’s daughter reported that the patient had minimal reading ability, but that she could write her name and most words.
Assessment based on BDAE-3 (Goodglass et al., 2001) and BNT-2 (Kaplan et al., 2001) revealed a fluent aphasia. Word finding was well preserved in responsive naming (19/20), conversation and picture description, but severely impaired in confrontation naming (BNT 13/60). Repetition was well preserved at the single word (10/10) and sentence levels (8/10). Auditory comprehension was mildly impaired (basic word discrimination 29.5/37, commands 11/15, complex ideational material 10/12). Single word oral reading was severely impaired (1/30) with a letter-by-letter reading strategy noted. Spelling was far superior to reading, breaking down only for more lengthy words [primer words 6/6, common irregular words 5/5, regular phonics 2/5 (errors were on 6–8 letter words)].
DBR’s reading was further evaluated with a battery of reading and related tests designed to further assess her letter knowledge and oral reading abilities. Her naming of individually presented letters was impaired (19/26 lower case), as was her ability to identify individual letters given their names (16/26 lower case). In contrast, she demonstrated better performance identifying whether a letter was presented in its correct or mirror image orientation (47/52) and determining whether or not a pair of upper and lower case letters represented the same letter (48/52). She demonstrated a marked length effect in her reading (see figure 1). Her reading showed no effect of regularity (regular words 5/20; exception words 10/20), nor did it show a typical part-of-speech effect (nouns superior to functors). Her pattern of performance reading words of varying parts of speech was, however, unusual (nouns 3/8, adjectives 8/8, verbs 6/8, functors 2/8). This unusual pattern may be attributable to the fact that DBR had greater difficulty identifying some letters compared with others, and this test was not matched for specific letters across parts of speech. She did not show significantly greater difficulty reading pseudowords than matched, real words (4/20 and 7/20, respectively). Her spelling and recognition of oral spelling were superior to her reading (25/32 and 28/32, respectively vs. 19/32 reading). Based on her letter-by-letter reading, length and modality effects she was diagnosed with pure alexia.
Patient 3
IND is a 68-year-old, right-handed male with a law degree. He was working as an attorney when he sustained a left occipital infarct more than one year prior to this study. CT revealed that he suffered an embolic stroke of the posterior cerebral artery. The resulting occipital lobe lesion extended upward into BA 19/7 and involved the inferior bank of the calcarine fissure. Three years prior to his CVA, IND experienced left sided facial swelling and dizziness; an MRI was conducted at that time and revealed small vessel disease.
Assessment based on BDAE-3 (Goodglass et al., 2001) and BNT-2 (Kaplan et al., 2001) revealed a fluent aphasia. Word finding was preserved in responsive naming (20/20) and conversation, but significantly impaired in confrontation naming (BNT 6/60) and picture description. Repetition was well preserved at both the single word (9/10) and sentence levels (10/10), as was auditory comprehension (basic word discrimination 31/37, commands 15/15, complex ideational material 11/12). Single word oral reading was moderately impaired (16/30), while spelling was intact for regular words, but impaired for irregular forms (primer words 6/6, regular phonics 4/5, and irregular forms 2/5.)
IND’s reading was further evaluated with a battery of reading and related tests designed to assess his letter knowledge, oral reading and spelling abilities. He demonstrated impaired letter naming (20/26 lower case). His ability to identify lower case letters across a variety of tasks, however, was superior to his naming (identifying letters given their names 25/26; identifying whether letters were presented in their correct or mirror image orientation 48/52; and matching letters across case 45/52). A length effect was not readily apparent in his word reading accuracy, as he was quite persistent in working through each word given unlimited time. However, a length effect was clearly evident in his reading response time (see figure 1). His oral reading showed no effects of part of speech (nouns 7/8, adjectives 7/8, verbs 7/8, functors 7/8), nor any greater difficulty reading pseudowords compared with matched, real words (15/20 and 16/20, respectively). He did, however, demonstrate a regularity effect (20/20 regular vs. 12/20 exception). Further, there was some impairment in his spelling (24/32) and his recognition of oral spelling (34/40). It appears, then, that his reading contained characteristics of pure alexia (letter-by-letter reading and consequent length effect in RT) as well as surface alexia and agraphia. These multiple reading impairments are not surprising given IND’s neurologic history. As with the other two patients, his poor letter naming and letter-by-letter reading were the targets of this treatment.
All three participants were seeking reading treatment, and all demonstrated letter-by-letter reading that was ineffective due to their poor letter naming. They were enrolled in the current study to first improve their letter naming accuracy via a tactile-kinesthetic strategy, and then to improve their letter-by-letter word reading speed. The Institutional Review Board of Georgetown University Medical Center approved this study, and signed informed consent was obtained from all participants prior to assessment and treatment.
Stimuli
Training Stimuli
Phase 1 (tactile-kinesthetic letter naming) training stimuli consisted of all 26 lower case letters of the alphabet. Phase 2 (rapid letter-by-letter word reading) training stimuli included all 26 letters, 450 non-pronounceable letter strings and 450 words. Letter strings and words were 4–8 letters in length. The set of words was composed of pairs that were matched for orthographic similarity (starting with the same first three letters and containing the same total number of letters, e.g. straight-strength, pound-pouch), to eliminate the potential for guessing the word after identifying only the first few letters. The letters in the words were scrambled in order to create the non-pronounceable letter strings (e.g. gihtasrt). All training stimuli were presented in lower case, arial font.
Testing Stimuli
Internal Test Measures
To assess improvement within Phase 1(tactile-kinesthetic letter naming), all 26 letters of the alphabet were presented for oral naming. To assess improvement within Phase 2 (rapid letter-by-letter word reading), 50 of the training letter strings were presented for letter naming and 50 of the training words were presented for oral reading. The 50 letter strings and 50 words each consisted of ten items of each letter length (four to eight letters).
External Test Measures
A different set of words, Word List 2, was used to assess improvement across both Phase 1 and Phase 2 in reading untrained words without the overt use of the tactile-kinesthetic strategy. Word List 2 contained 40 six-letter, 2-syllable, low frequency [<50 based on Francis and Kucera (1982)] words with a regular spelling-to-sound correspondence. The words in Word List 2 were never trained at any point in the study. The BNT-2 (Kaplan et al., 2001) was used to rule out spontaneous recovery by evaluating visual confrontation naming. Visual confrontation naming is a non-reading language skill that was impaired in all patients, but that was not expected to improve as a result of this treatment. Patients LDR and IND were further tested reading sentences from the BDAE-3 Oral Sentence Reading subtest (Goodglass et al., 2001), and twenty additional sentences, each of which contained five, predominantly high frequency words.
Design
Phase 1
Phase 1 training consisted of tactile-kinesthetic letter naming treatment, intended to improve letter naming accuracy. Improvement in Phase 1 was assessed by the internal test measure of letter naming accuracy administered before and after Phase 1 (see Table 2 for a summary of the design).
Table 2.
Treatment Design
| Time Point | ||||||||
|---|---|---|---|---|---|---|---|---|
| Assessment Measure | Testing 1 | Treatment Phase 1 |
Testing 2 | Treatment Phase 2a |
Testing 3 | Treatment Phase 2b |
Testing 4 | |
|
Internal Measures |
Letter Naming accuracy |
X | X | |||||
| Letter Naming accuracy and speed |
X | X | X | |||||
| Word Reading accuracy and speed |
X | X | X | |||||
|
External measures |
Word Reading accuracy and speed (Word List 2) |
X | X | X * | X | |||
| BNT-2 | X | X | ||||||
| BDAE-3 Oral Sentence Reading |
X | X* | X* | |||||
| Sentence Reading accuracy and speed |
X* | X* | ||||||
Internal Measures assessed improvement within each training phase. External measures assessed performance across both training phases, on untrained items/tasks.
indicates tests administered to only 2 of the 3 patients.
Phase 2
Phase 2 training consisted of rapid letter-by-letter word reading treatment divided into two stages: Phase 2a trained rapid letter naming, while Phase 2b trained rapid letter-by-letter word reading. The goal of Phase 2 was to improve letter-by-letter word reading by first making letter naming as efficient as possible. Improvement across Phase 2 was assessed by the internal test measures of letter naming and word reading accuracy and speed (before Phase 2a, after Phase 2a, and after Phase 2b).
External test measures administered across Phases 1 and 2
The goal of the study was to assess whether the treatment effect generalized to reading untrained words without overt use of the strategy. This was assessed across both training phases by the external measure of word reading, Word List 2 (at baseline, following Phase 1, and following Phase 2b; two of the three patients were administered this test a fourth time, following Phase 2a). In order to specifically attribute any reading improvement to the treatment provided, rather than to any spontaneous language recovery, visual confrontation naming was assessed before and after the entire course of treatment by the BNT-2 (Kaplan et al., 2001) (at baseline and after Phase 2b). Patients LDR and IND were further assessed across both treatment phases by external measures of sentence reading (at baseline, following Phase 1 and following Phase 2b).
Procedure
Internal Test Measures
At baseline, all 26 letters were presented for naming. The letters were presented one at a time and in random order on a computer screen via the SuperLab program (Abboud, 1991). Accuracy was recorded. To ensure performance stability, testing was done on three separate occasions over a period of two weeks (all other baseline measures were assessed once). Letter naming was reassessed following Phase 1. Prior to Phase 2, the training letter strings were presented for naming and the training words were presented for oral reading. Items were blocked and presented one at a time and in random order on a computer screen, also via SuperLab (Abboud, 1991). The patient was instructed to name each letter in the letter strings, or to read aloud each word, as quickly and accurately as possible. No direction regarding use or non-use of the strategy was provided. Both accuracy and response times were recorded. Retesting after Phase 2a and after Phase 2b were conducted in the same manner.
External Test Measures
At baseline, Word List 2, the list of words that would never be trained, was presented for oral reading. Words were presented in free vision, one at a time, and in random order on a computer screen via Superlab (Abboud, 1991). Accuracy and response times were recorded. On retesting (following Phase 1and following Phase 2b; and following Phase 2a for two of the three patients), patients were instructed to not use the tactile-kinesthetic strategy, and were asked to sit on their hands to prevent inadvertent use of the strategy. At baseline, the BNT-2 (Kaplan et al., 2001) was administered in standardized fashion. It was re-administered after Phase 2b. At baseline, the BDAE-2 Oral Reading subtest (Goodglass et al., 2001) was also administered in standardized fashion. Response times were measured with a stopwatch from an audiotape of the testing. The subtest was re-administered before and after Phase 2. Before Phase 2, the additional 20 sentences were presented one at a time and in random order on a computer screen via Superlab (Abboud, 1991). The patients were instructed to read each sentence as quickly and accurately as possible. Accuracy and response times were recorded. The sentences were re-administered after Phase 2. No direction regarding use or non-use of the strategy was provided for either sentence reading test. All testing was conducted under baseline conditions in which no feedback regarding accuracy or response time was provided.
Phase 1 Treatment
Treatment sessions were conducted for one hour three times per week. In Phase 1, the tactile-kinesthetic letter naming technique was trained through a hierarchy of stages. Treatment at each stage continued until the patient demonstrated 90% accuracy on the task currently being trained as measured on two consecutive probe tests. Probe tests were conducted at the beginning of each session (any treatment stage for which the patient was at least 90% accurate on the initial probe was omitted). The stages were as follows: 1) tracing of each two-inch high letter presented on an index card with arrows indicating correct pen strokes; 2) tracing of each two-inch high letter presented on an index card without arrows; 3) copying onto the left palm of each two-inch high letter presented on an index card; 4) copying onto the left palm of each two-inch high letter presented on an index card and then accurately naming it; and 5) copying onto the left palm of each standard size letter (18 point) presented on an index card and then accurately naming it. Once criterion was achieved on this final training stage, the internal test measure of letter naming accuracy was re-administered. Note that while criterion for advancing through the training stages was based on probe tests, overall improvement in Phase 1 was assessed by this internal test measure. Note also that this Phase of therapy only included letter naming; word reading was not introduced until Phase 2.
If the patient made an error on a training trial, cues were provided as necessary until the correct response was elicited (response contingent cues). If the patient failed to trace/copy the letter prior to naming it, s/he was reminded to do so; if the pen strokes were incorrect, s/he was cued to look at the card with the arrows.
Patients were instructed to carry out home practice three times per day. To accomplish this, they were provided with index cards containing the letters in the format currently being trained, and a logbook for recording each time they ran through the alphabet. At the beginning of each session, the examiner checked the logbook to ensure compliance with the home practice schedule. In order to increase the likelihood that home practice would be conducted accurately, it was not initiated until after the patient had demonstrated consistently correct pen strokes during treatment sessions (stage 2),
Phase 2 Treatment
Treatment sessions in Phase 2 were also conducted for one hour three times per week. All training stimuli in Phase 2 were presented via SuperLab (Abboud, 1991) in order to record response times. In Phase 2, rapid letter-by-letter word reading was trained, again through a hierarchy of stages. In Phase 2a (rapid letter naming) letter naming continued to be practiced, first in isolation and then within unrelated letter strings. The task was to name each letter as quickly and accurately as possible. Letter strings were included to highlight the need to name every letter when reading a word, and to not just make an educated guess based on only the first few letters. In Phase 2b rapid letter-by-letter word reading was trained. Words were presented one at a time. The patient was instructed to name each letter in the word and then say the word, as quickly and accurately as possible. For Phases 2a and 2b, criterion was based on response time rather than accuracy, and therefore we chose to monitor progress based on performance on training trials rather than on probe tests. Three blocks of 25 strings or words each were presented each session. The corpus of training stimuli was made large enough that no letter string or word would be repeated over a two-week period. This was done in order to reduce the likelihood that improvement might be due to familiarity with the stimuli and to foster generalization to untrained stimuli. Training continued within each stage until performance on training trials reaching asymptote. Asymptote was defined as when the linear trend line of the daily average response time no longer revealed a negative slope over six consecutive sessions. To prevent inducing the patients to increase their speed at the cost of accuracy, response times were calculated only for training blocks in which accuracy was at least 90%, and for correct responses only. Once asymptote was reached in Phase 2a and, again in Phase 2b, the internal test measures of letter naming and word reading accuracy and speed were re-administered at the beginning of the next session, conducted under baseline conditions. Note that while criterion for advancement was based on training trial response times, overall improvement in Phase 2 was assessed by these internal test measures.
During training, response contingent cues were provided as needed depending on the nature of the error. If a letter was misidentified, the patient was either reminded to use the tactile-kinesthetic method or to view the card for the correct pen strokes. For speed, the patient was told his/her average response times after the time for each block was computed, and the patient was encouraged to beat his/her time on the next block. Since this stage focused on reading speed, there was no home practice during this phase of treatment because feedback regarding speed could not be given.
Results
All statistics on accuracy were computed with McNemar or binomial test. All statistics on changes in response times were computed with paired t-tests.
Internal Test Measures
Phase 1 (tactile-kinesthetic treatment)
In training trials, the patients rarely made pen stroke errors after stage 2. Despite using correct pen strokes in subsequent training stages, occasional naming errors were made. Patient LDR reached criterion level performance in letter naming accuracy in 12 sessions, DBR in 5 sessions and IND in 4 sessions. Post Phase 1 testing on the internal test measure of letter naming accuracy demonstrated that all three patients improved to greater than 90% accuracy: LDR from 82% to 96%, DBR from 85% to 100%, and IND from 83% to 92%.
Phase 2 (speeded treatment)
Phase 2a (rapid letter naming)
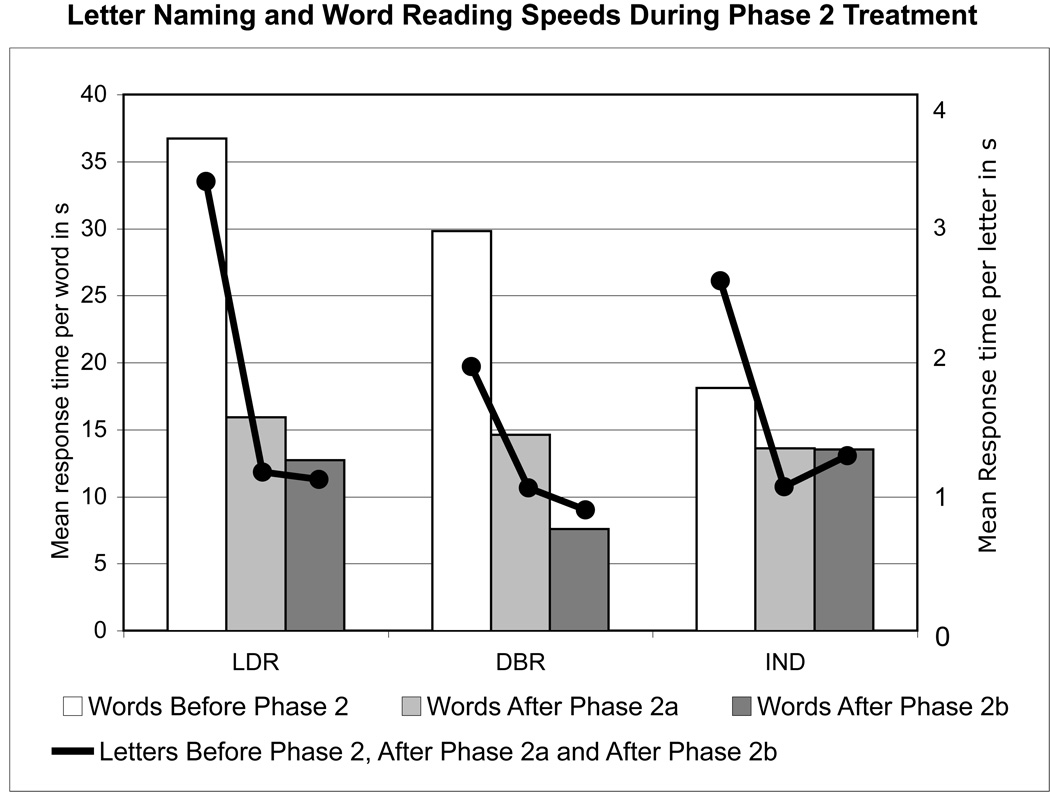
Patient LDR reached plateau in his letter naming speed on training trials after 30 sessions, DBR after 38 sessions and IND after 39 sessions. On the internal test measure of letter naming, all three patients significantly improved their speed [LDR t (27) = 14.036, p < .001; DBR t (28) = 5.413, p < .001; IND t (33) = 8.297, p < .001]. On the internal test measure of word reading, no patient had yet made any significant improvement in accuracy. On the words they could read accurately, however, all three became faster [LDR t (33) = 7.642, p < .001; DBR t (27) = 2.873, p = .008; IND t (19) = 2.871, p = .01]. See figure 2 for mean response times naming letters (line graphs) and reading words (bar graphs). It is important to note that at this point in treatment, word reading had not yet been trained.
Figure 2.
Mean response times for naming letters (line graph) and reading words (bar graph) throughout Phase 2 treatment. Changes in response times for word reading were significant for each time interval, with the exception of IND's change from After Phase 2a to After Phase 2b.
Phase 2b (rapid letter-by-letter word reading)
LDR reached plateau on his letter-by-letter word reading speed on training trials after 21 sessions, DBR after 25 sessions and IND after 20 sessions. On the internal test measure of word reading, this additional practice at the word level yielded even greater word reading speed for two of the three patients [LDR t (36) = 7.642, p = .029; DBR t (32) = 4.716, p < .001; IND t (27) = .883, p = .385] (again see figure 2 for response times). The internal test measure of word reading also demonstrated that all three patients now read words with significantly greater accuracy than they did prior to Phase 2 training (LDR 76% to 94%, binomial test: p = .012; DBR 66% to 88%, binomial test: p = .007; IND 52% to 80%, binomial test: p = .003).
External Test Measures
Reading Word List 2 Without Overt Use of the Strategy
Phase 1 (tactile-kinesthetic treatment)
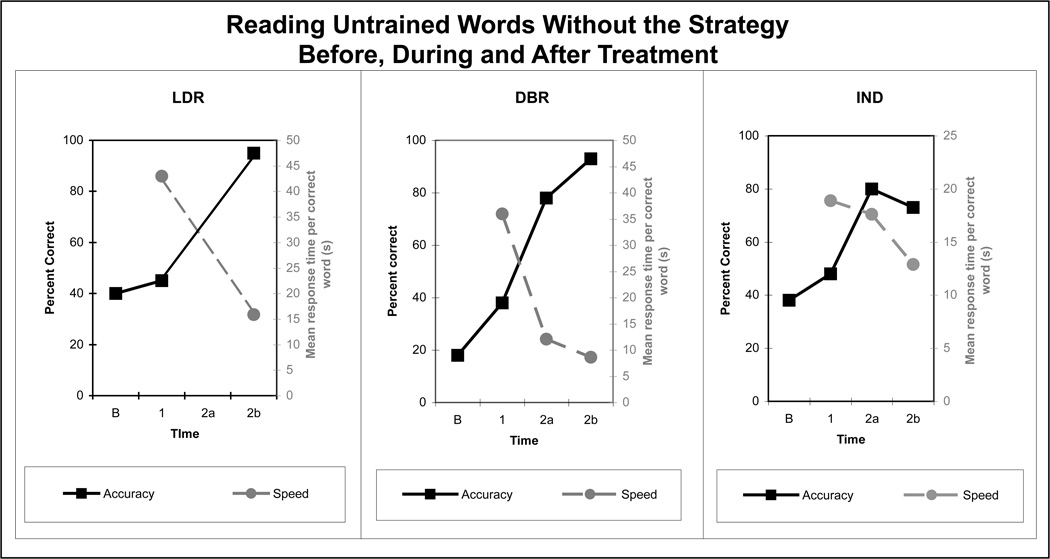
As can be seen in figure 3, two of the three patients showed some improvement in accuracy when reading without overt use of the strategy. However, these changes were not statistically significant, nor clinically meaningful as accuracy remained quite poor (LDR 40% to 45%, binomial test: p = 1.0; DBR 18% to 38%, binomial test: p = .08; IND 38% to 48%, binomial test: p = .45).
Figure 3.
Accuracy and speed reading untrained words without overt use of the strategy throughout the treatment phases. Data were collected at baseline (B), following Phase 1 (1), following Phase 2a (2a) and following Phase 2b (2b). No patient significantly improved following Phase 1. All patients significantly improved both accuracy and speed following Phase 2b. Only patients DBR and IND were tested following Phase 2a; both patients had already achieved significant gains in accuracy and speed by this point in treatment.
Phase 2 (speeded treatment)
Phase 2a (rapid letter naming)
Two of the three patients were tested following Phase 2a. As can be seen in figure 3, by this time point both were significantly more accurate (DBR, χ2 = 20.3, p < .001; IND, binomial test: p < .001) and faster [DBR t (5) = 6.54, p = .001; IND t (14) = 3.129, p = .007] than they were at baseline.
Phase 2b (rapid letter-by-letter word reading)
As can be seen in figure 3, all three patients were now significantly more accurate (LDR binomial test: p = .001; DBR χ2 = 28.0, p < .001; IND binomial test: p = .003) and faster [LDR t (7) = 2.874, p = .024; DBR t (6) = 7.327, p < .001; IND t (11) = 2.21, p = .049] than they were at baseline. Patients DBR and IND were also tested on Word List 2 following Phase 2a. This additional testing enabled us to evaluate whether any improvement was gained specifically from the word level training in Phase 2b. Patient DBR demonstrated some additional improvement following Phase 2b treatment. She was significantly faster [t (29) = 2.817, p = .009], and tended to be more accurate (78% to 93%, binomial test: p = .07) than she was following Phase 2a.
Sentence Reading
LDR and IND were further evaluated reading entire sentences. Before treatment, neither was able to correctly read any of the sentences on the BDAE-3 Oral Sentence Reading subtest (Goodglass et al., 2001). Following Phase 2, both were able to complete the entire subtest. With no direction regarding use or non-use of the strategy provided, LDR read sentences without overt use of the strategy, while IND used it only occasionally. LDR accurately read 9/10 sentences, and he correctly answered 2/5 of the comprehension questions. IND read 8/10 sentences and correctly answered 3/5 comprehension questions. Prior to Phase 2, reading of the additional set of 20 sentences was assessed. IND was unable to read any of the sentences at that time. Following Phase 2, he correctly read six of them. LDR, on the other hand, had already become quite accurate with these short sentences by the beginning of Phase 2, and made little further improvement by the end of Phase 2 (from 15/20 to 16/20). His average time to read these sentences, however, improved dramatically, from 154.0 to 41.7 s/sentence [t (7) = 2.495, p = .041].
Non-reading language skills
Prior to treatment, all three patients were impaired at visual confrontation naming as measured by the BNT-2 (Kaplan et al., 2001). They were reassessed following treatment. LDR’s naming remained at the 75th percentile (46/60 to 49/60) while IND’s naming remained at the 20th percentile (6/60 to 8/60). The stability of their naming suggests that LDR and IND did not spontaneously recover language skills over the course of this study. DBR’s naming improved slightly, from the 25th to 30th percentile (13/60 to 20/60). Her auditory comprehension, however, as measured by the BDAE-3 (Goodglass et al., 2001) composite auditory comprehension score, showed no improvement. She scored at the 45th percentile before treatment and at the 40th percentile on follow-up testing (Basic Word Discrimination 29.5/37 to 29/37, Commands 11/15 to 12/15, Complex Ideational Material 10/12 to 9/12). Although DBR’s performance on the BNT-2 (Kaplan et al., 2001) improved slightly over the course of the treatment, her other impaired language skill, auditory comprehension, did not improve. The stability of her auditory comprehension score suggests that she also did not spontaneously recover general language function.
Summary of results
All three patients significantly improved both their accuracy and speed of word reading under normal reading conditions following a two-phase tactile-kinesthetic treatment. Improving letter-naming accuracy alone (Phase 1) was not sufficient for any of the three patients to significantly improve their reading; continued practice (Phase 2) was required for all three patients. Additional testing administered to two of the three patients revealed that continued practice naming letters rapidly (Phase 2a) was sufficient to achieve significant improvement in word reading accuracy and speed; training at the word level (Phase 2b) was not necessary to achieve significant improvement, although it did confer some additional benefit. While treatment did not target sentence level reading, two of the three patients were additionally tested reading sentences and demonstrated notable gains at this level.
Discussion
We report three patients who significantly improved their speed and accuracy reading untrained words following a two-phase tactile/kinesthetic treatment. What is most striking about these findings is that all three patients were able to do so without overtly using the tactile/kinesthetic strategy. This improvement is not likely attributable to spontaneous recovery. Spontaneous recovery of letter naming has been reported in the literature, but it tends to happen very acutely, during the first weeks following the stroke (Beeson, Magloire, & Robey, 2005). Beeson et al. (2005) reported that their patient demonstrated 100% letter naming by 15 weeks post-onset, and they cited two additional cases in the literature that also fully regained their letter naming during the acute stages of recovery. Our patients were chronic and demonstrated stable letter naming performance over repeated baseline measures. Furthermore, if improvement were due to spontaneous recovery, one would expect their other language impairment, naming (and auditory comprehension in the case of DBR), to also improve. None of the patients demonstrated this.
The patients in the current study had relatively mild letter naming deficits (ranging from 73% to 77% accuracy). Lott et al. (1994) and Lott and Friedman (1999) have shown that the tactile-kinesthetic approach also successfully improves word reading in patients who demonstrate more severe letter naming deficits (49% and 62% accuracy, respectively). It remains to be seen whether these more severely impaired patients could progress to reading without overt use of the strategy, as did the more mildly impaired patients in the current study.
One might predict that once letter naming became highly accurate, then letter-by-letter word reading accuracy would follow suit. This was not the case. In order to significantly improve reading without overt use of strategy, all patients required the additional practice in Phase 2 treatment. In fact, Phase 1 was not even sufficient to significantly improve reading with overt use of the strategy. Two of the patients were additionally tested following Phase 1 reading words with overt use of the strategy; neither had improved significantly in this condition either (LDR 40% to 50%, binomial test: p = 1.0; IND 38% to 55%, binomial test: p = .143).
One possible explanation for the improvement seen following Phase 2 is that letter naming became more efficient as a result of being repeatedly practiced. As in the Lott and Friedman (1999) study, letter naming reached criterion in the first treatment phase, and was then repeatedly practiced in the second training phase. The second phase, however, contained multiple components: additional practice naming letters but also practice reading letter-by-letter at the word level. Results from the additional testing administered to two of the three patients in the current study allow us to disambiguate the contributions of these two components. Both patients were already significantly more accurate and faster reading words following rapid letter naming treatment (Phase 2a). This suggests that repeated practice with letter naming was sufficient to achieve significant improvement; subsequent training at the word level (Phase 2b) was not necessary. It should be noted, however, that this study did not control for the order of training rapid letter naming versus rapid word reading. It has been suggested that the training of complex grammatical structures results in generalization to less complex structures that rely on common processes (Thompson, Shapiro, Kiran and Sobecks, 2003). Based on this Complexity Account of Treatment Efficacy (CATE) it is possible that the complex, rapid word training phase may have produced the same generalization effects had it been administered prior to the less complex, rapid letter naming treatment phase. Regardless, the data clearly suggest that additional practice beyond the point of initial letter naming mastery is beneficial, and that doing so only within the context of letters can result in significant word reading improvement.
Why should additional practice with letter naming be sufficient to improve word reading? One possible explanation is that it is the result of repeatedly practicing the naming of individual letters. Several speech and language treatment studies have attributed successful outcome to the use of some type of repeated practice, or overlearning, in their paradigm (Dworkin, Abkarian and Johns, 1988; McNeil, Clayton, Barrett, Schober-Peterson, & Gonzalez-Rothi, 1998; Wambaugh, Martinez, McNeil & Rogers, 1999). McNeil et al. (1998), referring to the classic work of Schneider and Shiffrin (Schneider, Dumais, & Shiffrin, 1984; Schneider & Shiffrin, 1977; Shiffrin & Schneider, 1977), suggested that additional practice on a newly learned task is necessary before it can reach some basic level of automaticity, even if that task was learned to a high level of accuracy. They further suggested that automaticity may be very beneficial for people with aphasia by freeing up cognitive resources which can then be devoted to other language tasks. In this tactile-kinesthetic treatment, improving the efficiency of the serial letter identification process frees up additional cognitive resources to focus on the other skills needed to read words letter-by-letter, such as retaining all the letters identities and then recognizing the word they spell. Since the additional letter naming practice included naming letters presented within letter strings as well as presented in isolation, an alternative explanation is that improvement may be attributable to practice identifying letters in a sequence rather than simply overlearning individual letter names. To evaluate this alternative hypothesis, one patient, IND, was administered additional testing following practice naming letters individually, but prior to naming letters in strings. Following letter naming in isolation, his accuracy reading untrained words without the strategy had already improved significantly over baseline performance (from 38% to 65%, binomial test: p = .027). Following practice naming letters in letter strings, his accuracy further improved, though not significantly so (to 80%, binomial test: p = .18). This pattern suggests that the improvement seen following Phase 2a, at least for patient IND, cannot be wholly attributed to the effects of practice identifying letters in a sequence, but rather that the overlearning of naming letters in isolation was sufficient to significantly improve reading of untrained words without overt use of the trained strategy.
While significant improvement was demonstrated prior to word training, some additional gains were made following the word level training. This further improvement may simply be the result of the additional letter naming practice afforded by letter-by-letter word reading practice, or it may suggest that the additional cognitive components of letter-by-letter reading (e.g. retaining letter identities and recognizing the word they spell) also respond to remediation. The relationship between the patterns of change in letter naming and word reading speed depicted in Figure 2 suggest that the answer is patient specific. After Phase 2a in which only letter naming was trained, all three significantly improved letter naming speed and this generalized to improved word reading speed. After Phase 2b in which word reading was trained, the changes in patient DBR’s and IND’s word reading speed continued to parallel their changes in letter naming speed, although in opposite directions: DBR continued to make significant gains in word reading speed and also in letter naming speed, while IND did not make any further gains in his word reading speed nor in his letter naming speed. These patterns are consistent with the first hypothesis that treatment at the word level simply provides additional practice with letter naming; further improvement in word reading speed depended upon whether or not letter naming speed continued to improve. Patient LDR, however, showed a different pattern. He continued to improve his word reading speed after Phase 2b but not his letter naming speed. This pattern suggests that his improvement in word reading speed was not simply the result of additional practice naming letters, but rather of improving the other cognitive components of letter-by-letter word reading.
It remains unclear exactly how these patients processed orthography after treatment. Kashiwagi and Kashiwagi (1989) claimed that their patient, although not overtly using kinesthetic information when reading, was activating kinesthetic images. This was based on the finding that their patient made more reading errors when concurrently drawing triangles with his left index finger (requiring a kinesthetic image of a triangle) than when repetitively tapping the finger (not requiring a kinesthetic image). Patients with aphasia, but not pure alexia, did not show this interference. Did our patients also internalize the treatment such that they were activating kinesthetic images when they read visually? Did they regain the ability to recognize letters purely visually? fMRI may help us elucidate how these behavioral changes are instantiated in the brain. For example, Puttemans, Wenderoth, & Swinnen (2005) demonstrated changes in patterns of neural activation with the automatization of a motor task. All of our patients had pacemakers and therefore were, unfortunately, not magnet compatible. We plan to use imaging when possible with future patients to evaluate how the behavioral outcome of this treatment may be instantiated in the brain. While we can’t speculate on whether or not our patients imaged kinesthetic movements when they read, they did continue to demonstrate length effects in their reading, suggesting that they continued to read in letter-by-letter fashion .
This study has important implications both theoretically and clinically. First, it provides additional evidence on the efficacy of using a tactile-kinesthetic approach to improve letter naming in patients with letter-by-letter reading. Secondly, it demonstrates that learning a tactile/kinesthetic mediating strategy can alter cognitive processing such that words never specifically trained can be read in free vision without overtly using the mediating strategy. While it remains unclear exactly what mechanism underlies this processing shift, the data suggest that an important element in achieving this level of generalization is continuing training beyond the point of initially mastering letter naming accuracy.
Acknowledgements
This research was supported by NIH grants HD036019 and DC007169 to the last author. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NICHD, NIDCD, or NIH. The authors would like to thank patients LDR, DBR and IND for their dedication to this project.
REFERENCES
- Abboud H. Superlab. [computer software] Cedrus; 1991. [Google Scholar]
- Arguin M, Fiset D, Bub D. Sequential and parallel letter processing in letter-by-letter dyslexia. Cognitive Neuropsychology. 2002;19(6):535–555. doi: 10.1080/02643290244000040. [DOI] [PubMed] [Google Scholar]
- Beeson PM, Magloire JG, Robey RR. Letter-by-letter reading: natural recovery and response to treatment. Behavioral Neurology. 2005;16(4):191–202. doi: 10.1155/2005/413962. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bub DN, Black S, Howell J. Word recognition and orthographic context effects in a letter-by-letter reader. Brain and Language. 1989;36(3):357–376. doi: 10.1016/0093-934x(89)90073-4. [DOI] [PubMed] [Google Scholar]
- Dworkin JP, Abkarian GG, Johns DF. Apraxia of speech: The effectiveness of a treatment regimen. Journal of Speech and Hearing Disorders. 1988;53:280–294. doi: 10.1044/jshd.5303.280. [DOI] [PubMed] [Google Scholar]
- Francis WN, Kucera H. Frequency Analysis of English Usage: Lexicon and Grammar. Boston: Houghton Mifflin Co; 1982. [Google Scholar]
- Friedman RB, Hadley JA. Letter by letter surface alexia. Cognitive Neuropsychology. 1992;9(3):185–208. [Google Scholar]
- Godwin R. The treatment of pure alexia. In: Code C, Muller DJ, editors. Aphasia Therapy. London: Edward Arnold; 1983. pp. 146–156. [Google Scholar]
- Goldstein K. Language and Language Disturbances. New York: Grune-Stratton; 1948. [Google Scholar]
- Goodglass H, Kaplan E, Barresi B. Boston Diagnostic Aphasia Examination. 3rd ed. Baltimore: Lippincott Williams & Wilkins; 2001. [Google Scholar]
- Kaplan E, Goodglass H, Weintraub S. Boston Naming Test. 2nd ed. Austin, TX: PRO-ED, Inc; 2001. [Google Scholar]
- Kashiwagi T, Kashiwagi A. Recovery process of a Japanese alexic without agraphia. Aphasiology. 1989;3(1):75–91. [Google Scholar]
- Kay J, Hanley R. Simultaneous Form Perception and Serial Letter Recognition in a Case of Letter-by-Letter Reading. Cognitive Neuropsychology. 1991;8(3–4):249–273. [Google Scholar]
- Kreindler A, Ionasescu U. A case of "pure" word blindness. Journal of Neurology, Neurosurgery and Psychiatry. 1961;24:275–280. doi: 10.1136/jnnp.24.3.275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- LaPointe LL, Kraemer IT. Treatment of alexia without agraphia. In: Perkins WH, editor. Current Therapy of Communication Disorders: Language Handicaps in Adults. New York: Thieme-Stratton, Inc; 1983. pp. 77–85. [Google Scholar]
- Lott SN, Friedman RB. Can treatment for pure alexia improve letter-by-letter reading speed without sacrificing accuracy? Brain and Language. 1999;67(3):188–201. doi: 10.1006/brln.1999.2054. [DOI] [PubMed] [Google Scholar]
- Lott SN, Friedman RB, Linebaugh C. Rationale and efficacy of a tactile-kinaesthetic treatment for alexia. Aphasiology. 1994;8(2):181–195. [Google Scholar]
- Luria AR. Traumatic Aphasia: Its Syndromes, Psychology and Treatment. The Hague: Mouton; 1970. [Google Scholar]
- Maher LM, Clayton MC, Barrett AM, Schober-Peterson D, Gonzalez-Rothi LJ. Rehabilitation of a case of pure alexia: Exploiting residual abilities. Journal of the International Neuropsychological Society. 1998;4:636–647. doi: 10.1017/s1355617798466128. [DOI] [PubMed] [Google Scholar]
- McNeil MR, Doyle PJ, Spencer K, Goda AJ, Flores D, Small S. Effects of training multiple form classes on acquisition, generalization and maintenance of word retrieval in a single subject. Aphasiology. 1998;12(7):575–585. [Google Scholar]
- Puttemans V, Wenderoth N, Swinnen SP. Changes in brain activation during the acquisition of a multifrequency bimanual coordination task: From the cognitive stage to advanced levels of automaticity. The Journal of Neuroscience. 2005;25(17):4270–4278. doi: 10.1523/JNEUROSCI.3866-04.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sage K, Hesketh A, Ralph MA. Using errorless learning to treat letter-by-letter reading: contrasting word versus letter-based therapy. Neuropsychological Rehabilitation. 2005;15(5):619–642. doi: 10.1080/09602010443000155. [DOI] [PubMed] [Google Scholar]
- Schneider W, Dumais ST, Shiffrin RM. Automatic and control processing and attention. In: Parasuraman R, Davies DR, editors. Varieties of Attention. New York: Academic Press; 1984. [Google Scholar]
- Schneider W, Shiffrin RM. Controlled and automatic human information processing: 1. Detection, search and attention. Psychological Review. 1977;84:1–66. [Google Scholar]
- Seki K, Yajima M, Sugishita M. The efficacy of kinesthetic reading treatment for pure alexia. Neuropsychologia. 1995;33(5):595–609. doi: 10.1016/0028-3932(94)00138-f. [DOI] [PubMed] [Google Scholar]
- Shiffrin RM, Schneider W. Controlled and automatic human information processing: II. Perceptual learning, automatic attending and a general theory. Psychological Review. 1977;84:127–190. [Google Scholar]
- Stachowiak FJ, Poeck K. Functional disconnection in pure alexia and color naming deficit demonstrated by facilitation methods. Brain and Language. 1976;3(1):135–143. doi: 10.1016/0093-934x(76)90010-9. [DOI] [PubMed] [Google Scholar]
- Thompson CK, Shapiro LP, Kiran S, Sobecks J. The role of syntactic complexity in treatment of sentence deficits in agrammatic aphasia: the complexity account of treatment efficacy (CATE) Journal of Speech Language and Hearing Research. 2003;46(3):591–607. doi: 10.1044/1092-4388(2003/047). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wambaugh JL, Martinez AL, McNeil MR, Rogers MA. Sound production treatment for apraxia of speech: Overgeneralization and maintenance effects. Aphasiology. 1999;13:821–827. [Google Scholar]