Abstract
Objectives
To explore HIV-infected patients’ attitudes about buprenorphine treatment in office-based and opioid treatment program (OTP) settings.
Methods
We conducted in-depth qualitative interviews with 29 patients with co-existing HIV infection and opioid dependence seeking buprenorphine maintenance therapy in office-based and OTP settings. We used thematic analysis of transcribed audiorecorded interviews to identify themes.
Results
Patients voiced a strong preference for office-based treatment. Four themes emerged to explain this preference. First, patients perceived the greater convenience of office-based treatment as improving their ability to address HIV and other healthcare issues. Second, they perceived a strong patient-focused orientation in patient-provider relationships underpinning their preference for office-based care. This was manifest as increased trust, listening, empathy, and respect from office-based staff and providers. Third, they perceived shared power and responsibility in office-based settings. Finally, patients viewed office-based treatment as a more supportive environment for sobriety and relapse prevention. This was partly due to strong therapeutic alliances with office-based staff and providers who prioritized a harm reduction approach, but also due to the perception that the office-based settings were “safer” for sobriety, compared with increased opportunities for purchasing and using illicit opiates in OTP settings.
Conclusions
HIV-infected patients with opioid dependence preferred office-based buprenorphine because they perceived it as offering a more patient-centered approach to care compared with OTP referral. Office-based buprenorphine may facilitate engagement in care for patients with co-existing opioid dependence and HIV infection.
Keywords: patient-centered care, physician-patient relations, buprenorphine, HIV/AIDS, opioid-related disorders
INTRODUCTION
Opioid dependence is a relapsing-remitting chronic condition (McLellan, Lewis, O'Brien, et al., 2000; O'Connor, Samet, 2002) afflicting an estimated 213,000 heroin users and 4.7 million nonmedical analgesic users in the United States (SAMHSA, 2009). Though methadone maintenance treatment with behavioral therapy is effective for treating opioid dependence (National Consensus Development Panel on Effective Medical Treatment of Opiate Addiction, 1998; Amato, Davoli, Perucci, et al., 2005) and decreases HIV risk behaviors and transmission (Camacho, Bartholomew, Joe, et al., 1996; Hartel, Schoenbaum, 1998; Pang, Hao, Mi, et al., 2007), access to treatment remains limited (Friedmann, Lemon, Stein, et al., 2003; SAMHSA, 2009).
Expanding access to treatment for opioid dependence is particularly important in HIV-infected populations, where substance use disorder treatment is associated with increased antiretroviral adherence (Moatti, Carrieri, Spire, et al., 2000; Turner, Laine, Cosler, et al., 2003; Spire, Lucas, Carrieri, 2007), decreased repeated emergency department visits (Turner, Laine, Yang, et al., 2003), increased receipt of primary care (Conover, Whetten-Goldstein, 2002; Messeri, Abramson, Aidala, et al., 2002), decreased hospitalizations (Palepu, Tyndall, Leon, et al., 2001; Turner, Laine, Yang, et al., 2003) and costs (Palepu, Tyndall, Leon, et al., 2001). Substance abuse treatment, however, is underutilized among HIV-infected persons (Burnam, Bing, Morton, et al., 2001; Palepu, Horton, Tibbetts, et al., 2005; Palepu, Tyndall, Joy, et al., 2006). These and other studies led the Institute of Medicine to identify substance abuse treatment as a critical component in preventing the spread of HIV infection (Institute of Medicine, 2001).
The approval of buprenorphine for use by office-based primary care providers offers the potential for increased access to opioid dependence treatment (Fiellin, 2004). Office-based buprenorphine treatment has been demonstrated to be feasible and effective in reducing illicit opioid use (Fiellin, Pantalon, Pakes, et al., 2002; Fudala, Bridge, Herbert, et al., 2003), safe for use in HIV clinical settings (Sullivan, Barry, Moore, et al., 2006), and associated with high patient satisfaction rating (Barry, Moore, Pantalon, et al., 2007). It may also engage more previously untreated opioid-dependent patients compared with methadone maintenance (Sullivan, Chawarski, O'Connor, et al., 2005).
These studies suggest that at least some patients may prefer integration of treatment for opioid dependence and other chronic medical conditions. Little is known, however, about a) why patients might prefer office-based buprenorphine or b) how integrated treatment might affect treatment for HIV infection. Thus, the objective of this study was to investigate HIV-infected patients’ attitudes and perceptions about buprenorphine treatment in integrated settings vs. opioid treatment programs (OTP) and to explore patients’ views of how integrated care might affect substance abuse treatment and HIV care.
METHODS
Research Setting and Participants
We conducted a qualitative study in the context of a randomized trial of two opioid-dependence treatment delivery strategies. Two Ryan White-funded HIV primary care clinics and one federally certified OTP in Portland, Oregon served as demonstration sites for a national Health Research and Services Administration (HRSA) Special Projects of National Significance initiative to promote adoption of buprenorphine in HIV treatment settings. HIV-infected patients ≥ 18 years old, seeking treatment for a Diagnostic and Statistical Manual of Mental Disorders (DSM-IV) diagnosis of opioid dependence were randomized to receive office-based buprenorphine from their HIV provider at an HIV clinic or buprenorphine from an OTP. Patients in the office-based arm of the study received buprenorphine prescriptions from their HIV providers during clinic visits. Patients receiving buprenorphine at an OTP were dispensed buprenorphine according to federal methadone dispensing regulations. All patients received individual substance abuse counseling. Participants were allowed to cross-over after their initial evaluation. The study protocol was approved by the Institutional Review Board of Oregon Health & Science University.
Data Sources
In-depth interview guides contained open-ended questions about perceptions and attitudes toward current and past drug treatment, impact of drug treatment on HIV care, and organizational factors that influence drug treatment. The interviewer also probed for potential barriers and facilitators of treatment for opioid dependence in office-based and OTP settings. An example interview question was, “Please describe your experience getting drug treatment at this clinic,” with probes: “What services are the most important to you? Can you tell me about any services that you’ve had problems with?”
One-on-one interviews were conducted by a research assistant with experience in qualitative interviews, digitally audio-recorded, and transcribed for later analysis. Interviews were initially conducted 3 and 12 months following study enrollment. Upon preliminary analysis of the first 19 subjects enrolled, a baseline in-depth interview was added for subsequent participants. Participants received a $30 gift card for each completed interview. Interview statements quoted in this manuscript were edited for clarity, as identified by brackets.
Analysis
Audiotaped interviews were transcribed and reviewed for accuracy. We used thematic analysis to analyze our data and chose an inductive approach, seeking themes that emerged from the data rather than themes chosen as part of a theoretical model or literature review (Braun, Clarke, 2006). We analyzed data from a semantic (explicit) perspective using an essentialist/realist paradigm, as opposed to a constructionist paradigm (i.e., we theorized motivations, experience and meaning from what participants said rather than theorize the socio-cultural contexts and structural conditions that enabled the individual narratives). All interview transcripts were circulated to each member of the team for review. Team members met to discuss identified themes and resolve doubts or disagreements based on team discussion in an iterative process. One investigator (WR) then developed an initial coding scheme based on team discussions and reviewed it with the rest of the team which included a medical anthropologist (JG). Transcripts were initially coded by one investigator (WR) using ATLAS.ti software (Muhr, 2004), and then discussed in team meetings with other investigators to review coding and generate additional themes and sub-themes from preliminary codes. Doubts or disagreements were resolved by re-reading the original transcripts until all investigators agreed.
RESULTS
Participants
A total of 32 patients enrolled in the study, 3 of whom withdrew prior to completing a qualitative interview. We collected at least one in-depth qualitative interview for the remaining 29 enrollees, and 79% completed more than 1 interview. Thirteen interviews were conducted at time of enrollment, 25 at 3 months, and 19 at 12 months. The Table presents participant characteristics. The majority of participants were male, white race/ethnicity, injection drug users, and preferred heroin (compared with prescription opiates) as their opiate of choice. Concomitant stimulant use was common with 55% of participants reporting recent cocaine or methamphetamine use. Sixty-two percent of participants had prior treatment experience with methadone maintenance.
Table.
Participant Characteristics (n=29).
| N (%) | |
|---|---|
| Median age in years (range) | 41 (20–58) |
| Male gender | 23 (79) |
| Race/Ethnicity | |
| White | 18 (63) |
| African-American | 3 (10) |
| Native American | 3 (10) |
| Asian | 3 (10) |
| Latino | 2 (7) |
| Opiate of choice | |
| Heroin | 20 (69) |
| Prescription opiate analgesics | 5 (31) |
| Concurrent Drug Use | |
| Cocaine | 12 (41) |
| Methamphetamine | 4 (14) |
| Sedatives | 8 (28) |
| Current IDU | 23 (79) |
| Past Methadone Maintenance | 18 (62) |
Thematic Analysis
Participants voiced an overwhelming preference for office-based care over treatment at an OTP. Most had previously relapsed following treatment with methadone maintenance and said they would not have re-attempted treatment at all if only available in an OTP setting. This view was supported by the fact that 12 of 16 patients randomized to receive buprenorphine from an OTP crossed-over to office-based buprenorphine (75% of whom had been previously experienced methadone maintenance), while none of 16 patients randomized to receive office-based buprenorphine crossed-over to OTP buprenorphine.
“If you put them together [office-based buprenorphine and HIV care], I think it’s better for everybody, way better for everybody.”
Interviewer (I): “So describe your feelings towards being treated with buprenorphine at this clinic to treat your opiate dependence.”
Respondent (R): “Blissful, blissful, blissful.”
Reasons for Preferring office-based care
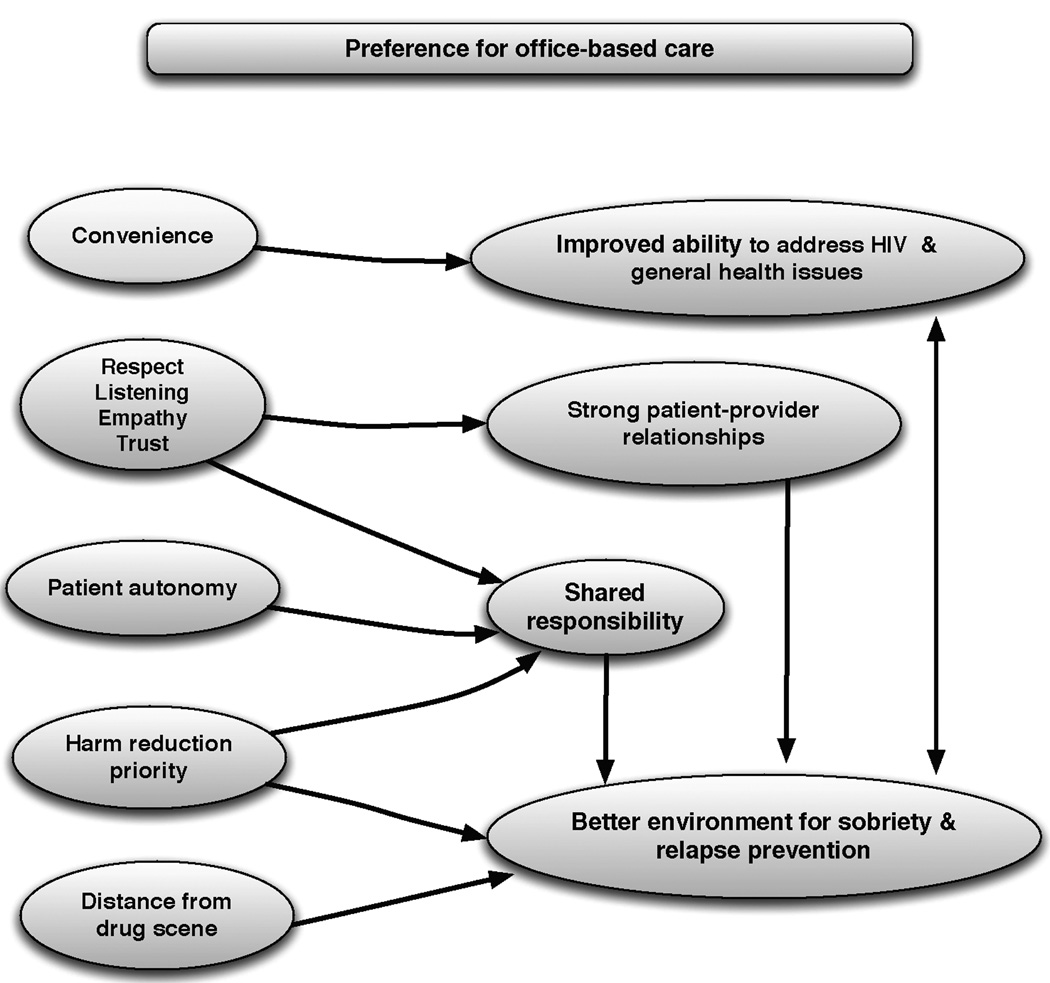
We identified four major themes illuminating why patients preferred office-based treatment (Figure). They felt that office-based care provided: 1) Greater convenience, which in turn improved HIV and overall care, 2) Respect, trust, and empathy from providers, which fostered strong patient-provider relationships, 3) Increased autonomy, which led to shared power and responsibility, and 4) a harm reduction priority and distance from the drug scene, which, in combination with these other factors, led to a supportive environment for sobriety.
Figure 1.
Preferences for Office-Based Care
Theme 1: Greater Convenience Improves Overall Care
Patients repeatedly cited the greater convenience of office-based care as a primary reason for preferring integrated care. They believed the increased convenience of receiving all their care in an office-based setting improved their ability to address both HIV and general healthcare issues. Participants specifically cited improved access for treatment of acute and chronic conditions and greater appointment and antiretroviral adherence as benefits of this increased convenience.
“I think [office-based care] is absolutely great. The fact that I don’t have to go to a methadone situation and be dosed every day, and all that stuff.”
“[Office-based buprenorphine] helps me stay sober so I take my [HIV] medicine.”
“I think the more exposure I have to a clinical setting…the better my care is. I mean, if I’m here and something is going on, I’ll hang out and go run up and ask [my provider]…if I’m scared.”
“[Office-based care] makes me show up for my appointments more frequently.”
“Going through my primary care doctor [lets me] kill two birds with one stone, because I’ve got to get back on my psych meds too.”
One participant, however, voiced a notable exception to this theme, suggesting that for him the additional structure and routine of treatment in an OTP setting may have been preferable for helping him adhere to opiate replacement therapy.
“At first I thought [office-based buprenorphine] would be perfect, because I’ve been through so many methadone clinics…and I really don’t like coming in every day. But then when I got the bup…I just didn’t take it. I’m thinking maybe…the whole idea of a [methadone] clinic and going in there every day… maybe I’m used to that more than just having to do it myself every day.”
Theme 2: Strong Patient-Provider Relationships
Patients perceived office-based settings as preferable due to strong interpersonal relationships with HIV clinic staff, counselors, and providers. Patients gravitated to these therapeutic relationships because of a greater perception of trust, listening, empathy, and mutual respect with office-based staff, counselors and providers. Participants repeatedly linked these patient-centered provider characteristics to their preference for office-based care:
I: “What’s it like getting your buprenorphine treatment here at the clinic with your doctor?”
R: “I think it’s better, because I have a good rapport with my doctor. And…my doctor, you know, knows all about my history, so it’s not like I can B.S. her or anything.”
“I would rather come here [to the HIV clinic] because…you have that kinship like with the staff.”
“She [my HIV provider] was real encouraging. I mean, especially because she sat and she listened, you know, until I was finished.”
In contrast, patients considered the OTP to be less a personal setting for treatment.
“I think it’s better working with your doctor …because there is a kind of a more personal level. At the [OTP] clinics you just go to the dosing window and the attitude”
In several cases, patients attributed perceived lack of respect particularly to their co-existing HIV infection, and voiced concerns about confidentiality in OTP settings.
“I didn’t want anybody to know [I was HIV positive]. If it was up to them they’d stone me to death. You know, a lot of HIV people were outcasts.”
Theme 3:Shared power and responsibility
Patients perceived greater patient autonomy and control of their treatment in office-based settings compared with experiences in OTP settings. They reported this sense of shared responsibility made it easier to stay sober.
“I think it’s…for a lot of people that are opiate dependent, they have to go every day and get their medicine. And for the fact that they trust me to do it for a month and give me the pills in advance, and I don’t have to bring the pills in and have them counted. And they trust me, so therefore, yeah…it’s nice.”
“He’s [my HIV provider] real open to my concept of things…[so that] in the long run I’m not getting strung out again.”
Patients greatly disliked what can be seen as a more external locus of control over their treatment in OTPs.
“One thing, you’re five minutes late they’ll shut the door right in your face.”
“And if I don't go to certain groups, then they don't give you take-outs and…you know, it's just a pain in the butt.”
Theme 4: Supportive Environment for Sobriety
Patients perceived the HIV clinic setting as offering a more welcoming environment to support sobriety. This included both interpersonal and structural characteristics. Patients described open discussions of substance use with office-based providers who prioritized harm reduction. They perceived their providers as having an unconditional commitment to providing care to them.
“…we [my doctor and I] have a real open dialogue about my drug use, which helps her and helps, you know, gauge where I am, why my body is changing and what all is going on.”
“I’m more…I’ll open more to him, the [HIV clinic] doctor that takes care of drug treatment. And, I don’t know, I’m just more comfortable talking about the drugs and my HIV problems with him.”
This alliance for sobriety extended to relapse prevention. Patients perceived office-based treatment to prioritize harm reduction (e.g., acknowledgement of reduced overall drug use over time as improvement in the face of relapse) over complete abstinence as leading to a more supportive community environment for sobriety and relapse prevention.
“I remember being told at the very beginning, you know, that this was not about succeed or not succeed. That if I did have problems that they were gonna work with me. I wasn't gonna get thrown out, or anything.”
“And she's [my HIV provider] made me feel really comfortable knowing that if I…were to get off it and relapse, or whatever, that she could…you know, that she could start giving it to me again.”
Open dialogues about relapse were perceived as limited in some OTP settings.
“I got used to being with one case manager there and I relapsed a couple of times. And…she just dropped me like a dirty rag. You know. And…it kinda left a bad taste in my mouth.”
While patients also reported strong therapeutic alliances with counselors in OTPs, relapse prevention at those centers was complicated by environmental factors that increased opportunities to purchase illicit opiates in those settings.
“…It’s dope central. I mean, you go to any city in the United States and you want to know where to score big for dope, or something, just go to the methadone clinic.”
“Watching the people who aren’t really there for recovery…and the buying and selling of things…It’s just a cycle to watch people who really don’t want to go in there, and getting it and then selling it and walking right across the street and buying the illegal part of it …it’s just…ugly.”
DISCUSSION
Patients with co-existing HIV infection and opioid dependence in this study voiced a strong preference for office-based treatment compared with OTP referral. Though we did not intentionally construct our interviews to probe for elements of patient-centered care, the reasons participants gave for their preference echoed four key dimensions of patient-centeredness described by Mead and Bower: 1) Biopsychosocial perspective—incorporating medical, mental health, behavioral, and social aspects of a patient’s existence, 2) Viewing the “patient as a person,” 3) Promoting shared power and responsibility between patients and health care providers, and 4) Developing a therapeutic alliance between patients and providers with the common goal of improving health (Mead, Bower, 2000).
Participants in our study perceived the greater convenience of having addiction treatment and HIV care delivered under one roof as improving the overall quality of their healthcare – a finding consistent with the biopsychosocial dimension of patient-centered care. Our patients’ perception of improved care is paralleled by studies showing improved clinical outcomes with integrated care. For example, patients with substance abuse-related medical conditions (e.g., Hepatitis C) randomized to receive chemical dependence treatment in a primary care setting were more likely to achieve abstinence than those treated in an addiction clinic (Weisner, Mertens, Parthasarathy, et al., 2001). HIV-infected patients may be even more likely to benefit from integrated treatment (McLellan, Lewis, O'Brien, et al., 2000).
Interview narratives also yielded strong positive expressions of patients’ relationships with clinic staff and providers as a major reason for preferring office-based buprenorphine treatment. The underlying components of these relationships were the trust, respect, listening, and empathy central to the patient-centered dimension of viewing the “patient as a person.” This finding echoes a recent patient satisfaction survey among patients receiving office-based buprenorphine in a primary care clinic which showed high satisfaction scores for perceptions of physician concern about “you as a patient” and “being treated like a patient instead of a drug addict” (Barry, Moore, Pantalon, et al., 2007). This dimension of patient-centeredness has also been associated with improved outcomes. In a national survey of U.S. adults, patients who reported their provider treated them with dignity had higher patient satisfaction, medication adherence, and optimal preventive care (Beach, Sugarman, Johnson, et al., 2005). Among patients attending an urban medical center HIV clinic, those who reported their provider “knows them as a person” reported greater receipt of antiretroviral therapy, adherence, and HIV viral suppression (Beach, Keruly, Moore, 2006). Patients reporting drug or alcohol use in this study, however, were less likely to report that their provider “knows them as a person.” Little is known about the relationship between viewing “the patient as a person” in OTP settings or its relationship to substance use outcomes. The current study raises new research questions about the capacity of providers – both in office-based and OTP settings – to foster patient-provider relationships where the patient feels viewed “as a person,” and whether these relationships might be associated with improved substance use outcomes.
Furthermore, patients in our study perceived themselves as having greater autonomy in the office-based setting that evoked a sense of shared power and responsibility for health care with their provider, the third dimension in Mead’s definition of patient-centered care and one highly associated with patient satisfaction. In a survey of patients receiving primary care in an urban setting, patient satisfaction was highly associated with their physicians having a greater participatory decision-making style (Cooper-Patrick, Gallo, Gonzales, et al., 1999). Likewise, Beach et al. demonstrated that a national sample of U.S. patients who reported their provider regularly involved them in decisions about their care reported both greater satisfaction and medication adherence (Beach, Sugarman, Johnson, et al., 2005). Among patients attending an urban HIV clinic, 63% preferred to share decisions with their doctor, and they were more likely to adhere to antiretroviral medications and achieve HIV viral suppression (Beach, Duggan, Moore, 2007). Mutual mistrust between physicians and drug-using patients, however, impedes attainment of this ideal among drug users hospitalized for medical issues (Merrill, Rhodes, Deyo, et al., 2002) and likely in other healthcare settings, as well. The current study suggests that interventions to improve patient autonomy and participatory decision making around substance use issues may foster improved engagement in substance use disorder treatment, offering fertile ground for additional research.
Finally, patients in this study perceived the office-based setting as a supportive community environment for treatment and recovery due to therapeutic alliances that prioritized harm reduction and environmental features. The concept of client-provider therapeutic alliance was originally developed to describe the partnership between client and counselor in moving toward the goals of psychotherapy. It has since been emphasized in substance use disorder treatment settings where early therapeutic alliance is associated with improved treatment retention and substance use outcomes (Diamond, Liddle, Wintersteen, et al., 2006; Ilgen, Tiet, Finney, et al., 2006; Meier, Donmall, McElduff, et al., 2006). Empiric evidence evaluating the role of therapeutic alliance in treatment of opioid dependence in primary care settings is lacking, but patients in this study indicated HIV clinic providers and staff were strongly aligned with the goal of sobriety and pragmatic in the event of relapse.
Creating a supportive environment for recovery, though, exceeded the bounds of interpersonal relationship to include a sense of the clinic as a safe place for recovery – indicating these patients perceived the physical environment and culture of office-based settings to be as important to their recovery as interpersonal therapeutic alliance with their providers. Patients in this study particularly valued the relative anonymity of the office-based settings with regard to other addicts. In contrast, they perceived greater opportunities to purchase illicit drugs and relapse in the environs surrounding OTPs. This finding raises further research questions of the role of therapeutic alliance in primary settings, and how organizational structures, cultures, and environments may influence treatment engagement and relapse prevention. The Network for the Improvement of Addiction Treatment (NIATx), for example, uses process improvement strategies to enhance engagement and retention (Capoccia, Cotter, Gustafson, et al., 2007; McCarty, Gustafson, Wisdom, et al., 2007; Hoffman, Ford, Choi, et al., 2008). Organizational change strategies appear to be a useful intervention for improvements in patient-centered care (McCarty, Gustafson, Capoccia, et al., 2009).
This study’s findings should be interpreted in the context of several limitations. First, the study population was limited to HIV-infected patients enrolled in a buprenorphine integration demonstration initiative, most of whom had previously relapsed following methadone maintenance treatment. We are cautious in interpreting our participant’s criticisms of OTP. Methadone maintenance is clearly effective in improving both substance use and behavioral outcomes (National Consensus Development Panel on Effective Medical Treatment of Opiate Addiction, 1998; Amato, Davoli, Perucci, et al., 2005). Opioid-dependent patients ranked methadone as preferable to buprenorphine in one study (Luty, 2004), and one of our study participants identified the additional structure of OTP with increased likelihood of adherence to opiate replacement therapy. Nearly two thirds of patients in our study, however, had already failed prior attempts at methadone maintenance, indicating that office-based buprenorphine may offer a means of engaging persons in care who have not responded to other evidence-based treatment modalities. Patients successfully treated with office-based buprenorphine may represent a different patient population compared with those who enroll in methadone maintenance (Sullivan, Chawarski, O'Connor, et al., 2005). Additional research is required to identify patients more likely to benefit from office-based vs. OTP treatment approaches.
Second, HIV clinic providers and staff participating in this demonstration project received substantial training and expert support in implementation of office-based buprenorphine – both identified as important barriers to widespread implementation of buprenorphine treatment in primary care (Turner, Laine, Lin, et al., 2005). With regard to both of these limitations, however, we used a qualitative approach to generate new research questions and hypotheses for future study rather than achieve a generalizable sample (Crabtree, Miller, 1999). Finally, our findings lack biologic substance use outcome data, which may not correlate with patients’ attitudes and perceptions about their treatment. Twelve-month retention rates, however, were high among our participants (60%), suggesting that larger studies of patients who have relapsed following methadone maintenance may demonstrate improved outcomes with more patient-centered approaches to treatment of opioid dependence.
CONCLUSIONS
Patient-centeredness – focusing health care on the patient’s experience of illness and promoting systems that meet an individual patient’s needs – is one of the Institute of Medicine’s key aims for improving the quality of U.S. health care. Patients in this study preferred office-based buprenorphine treatment because they perceived it be a more patient-centered alternative to OTP referral. The current study’s findings suggest that additional work may be required to realize the Institute of Medicine’s call to improve patient-centered substance abuse treatment (Institute of Medicine, 2006). To the extent that office-based buprenorphine maintenance remains patient-centered, it may offer an attractive alternative for engaging patients with co-existing opioid dependence and HIV in treatment. These findings generate many questions for further research including whether dimensions of patient-centeredness are associated with HIV and substance use outcomes, how to improve patient-centered care in both office-based and OTP settings, and whether interventions to improve the interpersonal and structural aspects of patient-centeredness might lead to improved outcomes.
ACKNOWLEDGEMENTS
Supported by the Health Research and Services Administration, Special Projects of National Significance (1-H97-HA03782-01), and the National Institutes of Health, National Institute on Drug Abuse (K23DA019808 and R01DA016341). Dr. Gregg’s time was supported by the Oregon Clinical and Translational Research Institute (OCTRI), grant number UL1 RR024140 from the National Center for Research Resources (NCRR), a component of the National Institutes of Health (NIH), and NIH Roadmap for Medical Research. Dr. Nicolaidis’ time was supported by the National Institute of Mental Health (K23MH073008). The authors wish to thank Sarann Bielavitz for her assistance with manuscript preparation.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Disclaimer: The views expressed in this paper are those of the authors. No official endorsement by DHHS, HRSA, the National Institutes of Health, or NIDA is intended or should be inferred.
REFERENCES
- Amato L, Davoli M, Perucci CA, Ferri M, Faggiano F, Mattick RP. An overview of systematic reviews of the effectiveness of opiate maintenance therapies: available evidence to inform clinical practice and research. J Subst Abuse Treat. 2005;28(4):321–329. doi: 10.1016/j.jsat.2005.02.007. [DOI] [PubMed] [Google Scholar]
- Barry DT, Moore BA, Pantalon MV, et al. Patient satisfaction with primary care office-based buprenorphine/naloxone treatment. J Gen Intern Med. 2007;22(2):242–245. doi: 10.1007/s11606-006-0050-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beach MC, Duggan PS, Moore RD. Is patients' preferred involvement in health decisions related to outcomes for patients with HIV? J Gen Intern Med. 2007;22(8):1119–1124. doi: 10.1007/s11606-007-0241-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beach MC, Keruly J, Moore RD. Is the quality of the patient-provider relationship associated with better adherence and health outcomes for patients with HIV? J Gen Intern Med. 2006;21(6):661–665. doi: 10.1111/j.1525-1497.2006.00399.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beach MC, Sugarman J, Johnson RL, Arbelaez JJ, Duggan PS, Cooper LA. Do patients treated with dignity report higher satisfaction, adherence, and receipt of preventive care? Annals of Family Medicine. 2005;3(4):331–338. doi: 10.1370/afm.328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Braun V, Clarke V. Using thematic analysis in psychology. Qualitative Research in Psychology. 2006;3(2):77–101. [Google Scholar]
- Burnam MA, Bing EG, Morton SC, et al. Use of mental health and substance abuse treatment services among adults with HIV in the United States. Arch Gen Psychiatry. 2001;58(8):729–736. doi: 10.1001/archpsyc.58.8.729. [DOI] [PubMed] [Google Scholar]
- Camacho LM, Bartholomew NG, Joe GW, Cloud MA, Simpson DD. Gender, cocaine and during-treatment HIV risk reduction among injection opioid users in methadone maintenance. Drug Alcohol Depend. 1996;41(1):1–7. doi: 10.1016/0376-8716(96)01235-5. [DOI] [PubMed] [Google Scholar]
- Capoccia VA, Cotter F, Gustafson DH, et al. Making "stone soup": improvements in clinic access and retention in addiction treatment. Joint Commission Journal on Quality & Patient Safety. 2007;33(2):95–103. doi: 10.1016/s1553-7250(07)33011-0. [DOI] [PubMed] [Google Scholar]
- Conover CJ, Whetten-Goldstein K. The impact of ancillary services on primary care use and outcomes for HIV/AIDS patients with public insurance coverage. AIDS Care. 2002;14(1) doi: 10.1080/09540120220149957. [DOI] [PubMed] [Google Scholar]
- Cooper-Patrick L, Gallo JJ, Gonzales JJ, et al. Race, gender, and partnership in the patient-physician relationship. Journal of the American Medical Association. 1999;282(6):583–589. doi: 10.1001/jama.282.6.583. [DOI] [PubMed] [Google Scholar]
- Crabtree B, Miller W. Doing Qualitative Research. 2nd ed. London: Sage; 1999. [Google Scholar]
- Diamond GS, Liddle HA, Wintersteen MB, Dennis ML, Godley SH, Tims F. Early therapeutic alliance as a predictor of treatment outcome for adolescent cannabis users in outpatient treatment. Am J Addict. 2006;15 Suppl 1:26–33. doi: 10.1080/10550490601003664. [DOI] [PubMed] [Google Scholar]
- Fiellin DA. Substance use of disorders in HIV-infected patients: impact and new treatment strategies. Topics in HIV Medicine. 2004;12(3):77–82. [PubMed] [Google Scholar]
- Fiellin DA, Pantalon MV, Pakes JP, O'Connor PG, Chawarski M, Schottenfeld RS. Treatment of heroin dependence with buprenorphine in primary care. Am J Drug Alcohol Abuse. 2002;28(2):231–241. doi: 10.1081/ada-120002972. [DOI] [PubMed] [Google Scholar]
- Friedmann PD, Lemon SC, Stein MD, D'Aunno TA. Accessibility of addiction treatment: results from a national survey of outpatient substance abuse treatment organizations. Health Serv Res. 2003;38(3):887–903. doi: 10.1111/1475-6773.00151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fudala PJ, Bridge TP, Herbert S, et al. Office-based treatment of opiate addiction with a sublingual-tablet formulation of buprenorphine and naloxone. N Engl J Med. 2003;349(10):949–958. doi: 10.1056/NEJMoa022164. [see comment] [DOI] [PubMed] [Google Scholar]
- Hartel DM, Schoenbaum EE. Methadone treatment protects against HIV infection: two decades of experience in the Bronx, New York City. Public Health Rep. 1998;1:107–115. [PMC free article] [PubMed] [Google Scholar]
- Hoffman KA, Ford JH, 2nd, Choi D, Gustafson DH, McCarty D. Replication and sustainability of improved access and retention within the Network for the Improvement of Addiction Treatment. Drug Alcohol Depend. 2008;98(1–2):63–69. doi: 10.1016/j.drugalcdep.2008.04.016. [comment] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ilgen M, Tiet Q, Finney J, Moos RH. Self-efficacy, therapeutic alliance, and alcohol-use disorder treatment outcomes. J Stud Alcohol. 2006;67(3):465–472. doi: 10.15288/jsa.2006.67.465. [DOI] [PubMed] [Google Scholar]
- No time to lose: Getting more from HIV prevention. Washington, D.C: National Academy Press; 2001. Institute of Medicine. [PubMed] [Google Scholar]
- Improving the Quality of Health Care for Mental and Substance-Use Conditions: Quality Chasm Series. Washington, D.C: The National Academies Press; 2006. Institute of Medicine. [PubMed] [Google Scholar]
- Luty J. Treatment preferences of opiate-dependent patients. Psychiatric Bulletin. 2004;28(2):47–50. [Google Scholar]
- McCarty D, Gustafson D, Capoccia VA, Cotter F. Improving care for the treatment of alcohol and drug disorders. J Behav Health Serv Res. 2009;36(1):52–60. doi: 10.1007/s11414-008-9108-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCarty D, Gustafson DH, Wisdom JP, et al. The Network for the Improvement of Addiction Treatment (NIATx): enhancing access and retention. Drug Alcohol Depend. 2007;88(2–3):138–145. doi: 10.1016/j.drugalcdep.2006.10.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McLellan AT, Lewis DC, O'Brien CP, Kleber HD. Drug dependence, a chronic medical illness: implications for treatment, insurance, and outcomes evaluation. Journal of the American Medical Association. 2000;284(13):1689–1695. doi: 10.1001/jama.284.13.1689. [see comment] [DOI] [PubMed] [Google Scholar]
- Mead N, Bower P. Patient-centredness: a conceptual framework and review of the empirical literature. Soc Sci Med. 2000;51(7):1087–1110. doi: 10.1016/s0277-9536(00)00098-8. [DOI] [PubMed] [Google Scholar]
- Meier PS, Donmall MC, McElduff P, Barrowclough C, Heller RF. The role of the early therapeutic alliance in predicting drug treatment dropout. Drug Alcohol Depend. 2006;83(1):57–64. doi: 10.1016/j.drugalcdep.2005.10.010. [DOI] [PubMed] [Google Scholar]
- Merrill JO, Rhodes LA, Deyo RA, Marlatt GA, Bradley KA. Mutual mistrust in the medical care of drug users: the keys to the "narc" cabinet. J Gen Intern Med. 2002;17(5):327–333. doi: 10.1046/j.1525-1497.2002.10625.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Messeri PA, Abramson DM, Aidala AA, Lee F, Lee G. The impact of ancillary HIV services on engagement in medical care in New York City. AIDS Care. 2002;14(1) doi: 10.1080/09540120220149948. [DOI] [PubMed] [Google Scholar]
- Moatti JP, Carrieri MP, Spire B, Gastaut JA, Cassuto JP, Moreau J The Manif 2000 study group. Adherence to HAART in French HIV-infected injecting drug users: the contribution of buprenorphine drug maintenance treatment. AIDS. 2000;14(2):151–155. doi: 10.1097/00002030-200001280-00010. [DOI] [PubMed] [Google Scholar]
- Muhr T. User's Manual for ATLAS.ti 5.0. Berlin: ATLAS.ti Scientific Software Development GmbH; 2004. [Google Scholar]
- National Consensus Development Panel on Effective Medical Treatment of Opiate Addiction. Effective medical treatment of opiate addiction. JAMA. 1998;280(22):1936–1943. [PubMed] [Google Scholar]
- O'Connor PG, Samet JH. Substance abuse: the expanding role of general internal medicine. J Gen Intern Med. 2002;17(5):398–399. doi: 10.1046/j.1525-1497.2002.20212.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Palepu A, Horton NJ, Tibbetts N, Meli S, Samet JH. Substance abuse treatment and hospitalization among a cohort of HIV-infected individuals with alcohol problems. Alcoholism: Clinical & Experimental Research. 2005;29(3):389–394. doi: 10.1097/01.alc.0000156101.84780.45. [DOI] [PubMed] [Google Scholar]
- Palepu A, Tyndall MW, Joy R, et al. Antiretroviral adherence and HIV treatment outcomes among HIV/HCV co-infected injection drug users: the role of methadone maintenance therapy. Drug Alcohol Depend. 2006;84(2):188–194. doi: 10.1016/j.drugalcdep.2006.02.003. [DOI] [PubMed] [Google Scholar]
- Palepu A, Tyndall MW, Leon H, et al. Hospital utilization and costs in a cohort of injection drug users. Can Med Assoc J. 2001;165(4):415–420. [PMC free article] [PubMed] [Google Scholar]
- Pang L, Hao Y, Mi G, et al. Effectiveness of first eight methadone maintenance treatment clinics in China. AIDS. 2007;21 Suppl 8:S103–S107. doi: 10.1097/01.aids.0000304704.71917.64. [DOI] [PubMed] [Google Scholar]
- SAMHSA. Results from the 2008 National Survey on Drug Use and Health: National Findings. Rockville, MD: Office of Applied Studies; 2009. [Google Scholar]
- Spire B, Lucas GM, Carrieri MP. Adherence to HIV treatment among IDUs and the role of opioid substitution treatment (OST) International Journal of Drug Policy. 2007;18(4):262–270. doi: 10.1016/j.drugpo.2006.12.014. [DOI] [PubMed] [Google Scholar]
- Sullivan LE, Barry D, Moore BA, et al. A trial of integrated buprenorphine/naloxone and HIV clinical care. Clin Infect Dis. 2006;43 Suppl 4:S184–S190. doi: 10.1086/508182. [DOI] [PubMed] [Google Scholar]
- Sullivan LE, Chawarski M, O'Connor PG, Schottenfeld RS, Fiellin DA. The practice of office-based buprenorphine treatment of opioid dependence: is it associated with new patients entering into treatment? Drug Alcohol Depend. 2005;79(1):113–116. doi: 10.1016/j.drugalcdep.2004.12.008. [DOI] [PubMed] [Google Scholar]
- Turner BJ, Laine C, Cosler L, Hauck WW. Relationship of gender, depression, and health care delivery with antiretroviral adherence in HIV-infected drug users. J Gen Intern Med. 2003;18(4):248–257. doi: 10.1046/j.1525-1497.2003.20122.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Turner BJ, Laine C, Lin Y-T, Lynch K. Barriers and facilitators to primary care or human immunodeficiency virus clinics providing methadone or buprenorphine for the management of opioid dependence. Arch Intern Med. 2005;165(15):1769–1776. doi: 10.1001/archinte.165.15.1769. [DOI] [PubMed] [Google Scholar]
- Turner BJ, Laine C, Yang CP, Hauck WW. Effects of long-term, medically supervised, drug-free treatment and methadone maintenance treatment on drug users' emergency department use and hospitalization. Clin Infect Dis. 2003;37(5):15. doi: 10.1086/377558. [DOI] [PubMed] [Google Scholar]
- Weisner C, Mertens J, Parthasarathy S, Moore C, Lu Y. Integrating primary medical care with addiction treatment: a randomized controlled trial. Journal of the American Medical Association. 2001;286(14):1715–1723. doi: 10.1001/jama.286.14.1715. [DOI] [PMC free article] [PubMed] [Google Scholar]