Abstract
Background: Magnetic resonance angiography (MRA) is supposed to be the new ’gold standard’ in the diagnosis of atherosclerotic disease of the extracranial arteries. Methods: A case report is presented on a patient in whom discordant findings of the status of the left internal carotid artery (ICA) were identified in color-coded duplex-sonography and MRA. Results: Left ICA stenosis was suspected in duplex-sonography, yet not confirmed in contrast-enhanced (CE) MRA reconstruction. Diagnosis was confirmed after surgery and in subsequent analysis of the original CE-MRI data. Conclusions: The analysis of source images must not be missed in MRA examinations. Conventional duplex-sonography may be superior in the estimation of the embolic potential of vascular lesions. Advanced CE techniques may therefore be adequate tools in differentiating patients eligible for carotid endarterectomy (CEA) or carotid stenting, avoiding the risk of peri-interventional iatrogenic complications. It should urgently be further improved and validated.
Keywords: carotid stenosis, color-coded duplex-sonography, plaque morphology, CE-MRA, early carotid endarterectomy
Introduction
Contrast-enhanced magnetic resonance angiography (CE-MRA) achieves the sensitivity and specificity of conventional catheter angiography, long considered the gold standard, for the evaluation of significant cervical carotid stenosis [Anzalone et al. 2006]. Colour-coded duplex-sonography has been shown to have a sensitivity and specificity of 86% and 87%, respectively, compared with digital subtraction angiography [Nederkoorn et al. 2003]. We report a case in which internal carotid artery (ICA) stenosis was suspected in duplex-sonography, yet not confirmed in CE-MRA reconstruction. Carotid endarterectomy (CEA) revealed a thrombus obstructing the vessel at about 55%. Subsequent analysis of the original CE-MRI data revealed an according CE notch on one coronal slice.
Case description
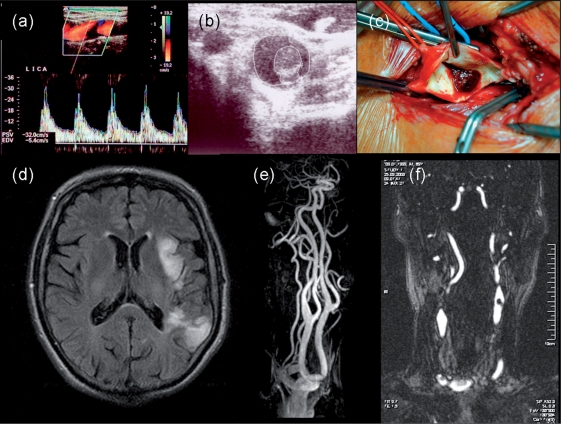
A 69-year-old patient was transferred to our stroke unit from a foreign hospital. Sudden onset of a severe mixed aphasia and mild right-sided sensor-motor hemiparesis 4 days before was reported. Symptoms were slightly regressive in the following days. The patient had well-controlled hypertension treated with perindopril without any other serious medical condi- tions. The MRI showed diffusion-weighted imaging (DWI) and fluid-attenuated inversion recovery (FLAIR) lesions both in the left middle cerebral artery (MCA) dorsal border zone and insular region suggesting a hemodynamic and arterio-arterial-embolic cause (see Figure 1d–f). Treatment with acetylsalicylic acid had been initiated. Duplex-sonography displayed a mixed lesion in the origin of the left ICA with a regional stenosis of about 55%, and no flow acceleration (see Figure 1a and b). The obstructing mass was only sparsely attached to the vessel wall, yet no signs of a free-floating unstable thrombus were seen. Reconstructed CE-MRA did not show any apparent sign of left ICA stenosis, only on the original source images a cauliflower-like notch of contrast agent was seen on one coronal slice.
Figure 1.
(a) Colour-coded duplex- and (b) B-mode sonography displaying the cauliflower-like mixed thrombus in the origin of left ICA leading to a 55% regional stenosis without flow velocity acceleration; (c): intraoperative situs of the left bifurcation with an adhesive thrombus to an ulcerated plaque formation; (d–f): FLAIR, CE-MRA reconstruction, and original CE coronal slice showing infarction signs in the left dorsal border zone and insular region (d) without sign of left ICA stenosis (e) but a cauliflower-like notch of CE in the vessel (f).
A surgical restoration of the left ICA stenosis was recommended, assuming a relevant risk of early embolic recurrence by the mixed thrombus. CEA was conducted 2 days later without any complication, revealing an ulcerated plaque (see Figure 1c). Fourteen days later the neurological condition had markedly improved due to intense speech and occupational therapy. Besides a severe sleep apnea syndrome, no other cardiovascular risk factor was identified.
Implications for clinical care
This case pinpoints two well-known and important aspects of the diagnostic procedure for the extracranial vasculature. First, reconstructed MRA should always be complemented by the analysis of the original source images. Second, for the estimation of the emboligenic potential of a vessel narrowing, duplex-sonography as a morphological non-contrast agent-based method seems to be equipollent to MRA and probably to CT angiography (CTA) as well. It can be pondered whether CTA under these circumstances might have been more sensible in the detection of the intraluminal clot.
It is recommended that duplex-sonography should be conducted in all patients with known alterations of the carotid arteries or any kind of stroke symptoms (http://www.eso-stroke.org/). Likewise, duplex-sonography is used as a standard tool for the estimation of atherosclerotic vessel disease. Substantial improvements of image quality of atherosclerotic changes have been reported in recent years [U-King-Im et al. 2007; Spence, 2006]. Ultrasound techniques may be considered as more cost effective and easier to apply than MRI in this setting. However, it is our experience that even today many interventional procedures of the carotid artery are undertaken without previous ultrasound examination. If, for any reason, an interventional procedure based on the sole MRI examination had been conducted in our patient, there would have been a very likely risk for peri-interventional complications due to flaking of thrombotic debris by the catheter causing an iatrogenic embolism [Skjelland et al. 2009]. This, of course, can be reduced to a certain extent by the use of a distal protection device.
We think that advanced duplex-sonography may be an adequate tool in differentiating patients eligible for CEA or carotid stenting. Therefore, duplex-sonography should be utilized as an obligatory screening tool before any interventional procedure to improve procedure safety. However, grade of stenosis alone does not seem to be sufficient in defining the risk of upcoming clinical events. Thus, there is a need for redefining imaging risk factors for stroke, such as neovascularization or contrast enhancement [Coli et al. 2008]. In our case the early CEA was a safe procedure in order to minimize the risk of early re-embolism. This is in the best accordance with the recent trend to carry out CEA early in symptomatic ICA stenosis; that is, within the first 48 hours to 2 weeks [Ballotta et al. 2008; Aleksic et al. 2006].
Acknowledgements
The authors would like to thank Ms Olga Koutoula from the Department of Neurology, AHEPA Hospital, Aristotle University Thessaloniki, Greece for collaboration with this patient.
Conflict of interest statement
None declared.
References
- Aleksic M., Rueger M.A., Lehnhardt F.G., Sobesky J., Matoussevitch V., Neveling M., et al. (2006) Primary stroke unit treatment followed by very early carotid endarterectomy for carotid artery stenosis after acute stroke. Cerebrovasc Dis 22: 276–281 [DOI] [PubMed] [Google Scholar]
- Anzalone N., Scotti R., Iadanza A. (2006) MR angiography of the carotid arteries and intracranial circulation: advantage of a high relaxivity contrast agent. Neuroradiology 48(Suppl. 1): 9–17 [DOI] [PubMed] [Google Scholar]
- Ballotta E., Meneghetti G., Da Giau G., Manara R., Saladini M., Baracchini C. (2008) Carotid endarterectomy within 2 weeks of minor ischemic stroke: a prospective study. J Vasc Surg 48: 595–600 [DOI] [PubMed] [Google Scholar]
- Coli S., Magnoni M., Sangiorgi G., Marrocco-Trischitta M.M., Melisurgo G., Mauriello A., et al. (2008) Contrast-enhanced ultrasound imaging of intraplaque neovascularization in carotid arteries: correlation with histology and plaque echogenicity. J Am Coll Cardiol 52: 223–230 [DOI] [PubMed] [Google Scholar]
- Nederkoorn P.J., van der Graaf Y., Hunink M.G. (2003) Duplex ultrasound and magnetic resonance angiography compared with digital subtraction angiography in carotid artery stenosis; a systematic review. Stroke 34: 1324–1331 [DOI] [PubMed] [Google Scholar]
- Skjelland M., Krohg-Sørensen K., Tennøe B., Bakke S.J., Brucher R., Russell D. (2009) Cerebral microemboli and brain injury during carotid artery endarterectomy and stenting. Stroke 40: 230–234 [DOI] [PubMed] [Google Scholar]
- Spence J.D. (2006) Technology insight: ultrasound measurement of carotid plaque - patient management, genetic research, and therapy evaluation. Nat Clin Pract Neurol 2: 611–619 [DOI] [PubMed] [Google Scholar]
- U-King-Im J.M., Tang T., Moustafa R.R., Baron J.C., Warburton E.A., Gillard J.H. (2007) Imaging the cellular biology of the carotid plaque. Int J Stroke 2: 85–96 [DOI] [PubMed] [Google Scholar]