Abstract
Objective
To investigate whether acupuncture reduces the duration and intensity of crying in infants with colic.
Patients and methods
90 otherwise healthy infants, 2–8 weeks old, with infantile colic were randomised in this controlled blind study. 81 completed a structured programme consisting of six visits during 3 weeks to an acupuncture clinic in Sweden. Parents blinded to the allocation of their children met a blinded nurse. The infant was subsequently given to another nurse in a separate room, who handled all infants similarly except that infants allocated to receive acupuncture were given minimal, standardised acupuncture for 2 s in LI4.
Results
There was a difference (p=0.034) favouring the acupuncture group in the time which passed from inclusion until the infant no longer met the criteria for colic. The duration of fussing was lower in the acupuncture group the first (74 vs 129 min; p=0.029) and second week (71 vs 102 min; p=0.047) as well as the duration of colicky crying in the second intervention week (9 vs 13 min; p=0.046) was lower in the acupuncture group. The total duration of fussing, crying and colicky crying (TC) was lower in the acupuncture group during the first (193 vs 225 min; p=0.025) and the second intervention week (164 vs 188 min; p=0.016). The relative difference from baseline throughout the intervention weeks showed differences between groups for fussing in the first week (22 vs 6 min; p=0.028), for colicky crying in the second week (92 vs 73 min; p=0.041) and for TC in the second week (44 vs 29 min; p=0.024), demonstrating favour towards the acupuncture group.
Conclusions
Minimal acupuncture shortened the duration and reduced the intensity of crying in infants with colic. Further research using different acupuncture points, needle techniques and intervals between treatments is required.
Introduction
Ten per cent of newborn children in the Western world experience colic.1 2 The aetiology is unclear but gastrointestinal factors and allergy to cow's milk protein have been suggested as possible causes.3 Another suggestion is that colic is a behavioural condition resulting from unfavourable parent–infant interaction.3 In three meta-analyses current medical treatments are evaluated as either inefficient (simethicone) or as having serious side effects like seizures, asphyxia and death3–5 (dicyclomine, presently withheld by the manufacturer). In spite of the good prognosis of infantile colic with full spontaneous recovery,6 colic inhibits optimal family relations7–9 and increases the risk of child abuse.10–12 Acupuncture is widely used and discussed in infantile colic. However, few articles have been published on this subject. Two uncontrolled studies report positive outcomes after acupuncture in children with night crying.13 14 One qualitative study15 and one randomised controlled study16 also indicate that acupuncture has an effect on infants' crying. The objective of this study was to further investigate whether minimal acupuncture reduces the duration and intensity of crying in infants with colic.
Material and methods
A prospective, randomised, controlled, blinded clinical trial was performed at a private acupuncture clinic in Sweden, from November 2005 to February 2007. For the past 15 years this acupuncture clinic has offered acupuncture treatment for adult patients with different symptoms and for infants with colic.
Patients
Infants with colic, 2–8 weeks old, whose parents sought help at either a child health centre, the regional hospital's paediatric clinic or at the acupuncture clinic where the trial was performed, were consecutively preselected by health professionals who were informed of the inclusion criteria: healthy infants, born after gestational week 36, not treated with dicyclomine and fulfilling the modified Wessel criteria for colic: ‘crying/fussing for at least 3 h a day, occurring 3 days or more in the same week’.1 Parents with eligible infants and who were willing to participate reported the extent and degree of their infant's crying and fussing in a diary for at least 3 days. Exclusion of cow's milk from the infant's diet was recommended during the registration period if it had not already been tried. If meeting the criteria, the infant was included in the study and started the structured programme the following Monday or Thursday. Written informed consent was obtained from the parents, and the study was approved by the local research ethics committee (Dnr 583/2005). All infants continued the regular programme at their ordinary child health centre throughout the duration of the study.
Randomisation and blinding
A registered nurse skilled in acupuncture, nurse A, was hired specifically to perform the randomisation, administer the intervention and be the sole person aware of allocation and with access to the records during the study. Nurse A met the infants alone in the treatment room and was only informed of their age and study number. The randomisation procedure divided the infants into an intervention group with a structured programme including acupuncture (acupuncture group) or to the same structured programme not including acupuncture (control group). As we proposed that age was a prognostic variable that might interfere with the result, restricted randomisation was used to achieve a balance between 2–5 weeks old and 6–8 weeks old infants, respectively, in the groups. Two sets of sealed opaque envelopes, marked ‘2–5 weeks old’ and ‘6–8 weeks old’, respectively, had been prepared by nurse A before the study started. The envelopes contained a card with either ‘control group’ or ‘intervention group’, each in equal amounts. The card in the upper envelope in the pile appropriate to the infant's age determined the group to which each infant was assigned. Consequently, all infants had an equal probability of assignment to either group. Each infant remained in the initially allocated group throughout the study.
The study was double blind as neither the parents who registered the infants crying nor the nurse who met the parents (nurse B, the first author) knew to which group the infant belonged. Nurse B enrolled parents of potential patients, informed them of the trial, assessed the infant's eligibility, obtained informed consent and met the parents at the acupuncture clinic. Two closed doors separated the parents from the treatment room and music was always played. Parents were informed that the needle was very thin, usually caused no bleeding or visible marks and that acupuncture does not necessarily provoke crying.
Intervention
The structured programme consisted of a total of six biweekly visits to the acupuncture clinic. The first visit lasted for 30 min, during which the parents met nurse B who repeated information on the study and collected baseline demographic data. During the following five visits, parents met nurse B for 15 min appointments, and were asked standardised questions such as ‘How is it going?’, received standardised oral support such as ‘Hopefully it will be better soon’ and were given time for questions.
At each visit, the infant was carried to the treatment room by nurse B and left there with nurse A. The initial handling of the infants in the treatment room was identical. Nurse A held each infant's hand and spoke soothingly. If starting to cry, the infant was comforted by the nurse in her arms. The infants allocated to have acupuncture subsequently received minimal, standardised acupuncture with a sterilised, disposable acupuncture needle, Vinco MicroClean, 0.20 × 13 mm. The needle was inserted unilaterally and left in place for 2 s at an approximate depth of 2 mm at point LI4 of the hand's first dorsal interossal muscle, a point often used in clinical practice when treating infants with colic and, also used in an earlier randomised controlled trial (RCT) studying acupuncture treatment for colic and known for the generalised analgetic effect.16 Left and right hands were used alternately. After a maximum of 5 min in the treatment room, nurse A carried infants back to their parents. Infants allocated to the two groups went through exactly the same procedure except for the insertion of an acupuncture needle in the acupuncture group.
Assessments and outcomes
Definitions of ‘fussing’ (showing dissatisfaction and whimpering despite being carried), ‘crying’ (screaming loudly) and ‘colicky crying’ (crying hysterically and unconsolably) were communicated to the parents both verbally and in writing. Parents reported infants' fussing, crying and colicky crying in a standardised diary form originally developed and validated by Barr et al17 and modified and tested by Canivet et al.18 The diary form consisted of sheets, each covering 24 h. Parents filled in boxes, each representing 5 min, to indicate when their infant was fussing (marked as F), crying (marked as C) and colicky crying (marked as CC). All marked boxes were counted manually and transferred into a database. Reports were made on at least 3 days during the baseline week preceding possible inclusion and daily during the three intervention weeks, directly following the baseline week. Twice weekly, parents completed a questionnaire modified from Reinthal et al,16 in which they described any adverse effects they considered to be caused by treatment. Duration of crying in the treatment room and bleeding were noted by nurse A. The primary end point was the number of infants who fulfilled the colic criteria during each of the intervention weeks. The secondary end point was the total duration of fussing, crying and colicky crying (TC) during the three intervention weeks as reported by parents in the diary.
Statistical analyses
Based on the assumption that 50% of the infants would go into spontaneous remission without treatment and 75% with acupuncture, 40 patients per group were needed in order to have a 90% chance of detecting a significant difference in remission at a two-sided 5% level. The statistical software SPSS version 17 (SPSS, Chicago, Illinois, USA) was used for calculations. As two parameters were not normally distributed all data were analysed with non-parametric statistics. Kaplan–Meier analysis was performed to assess the time for each infant's crying to fall below 180 min, indicating that the infant no longer fullfilled the criteria for colic. To evaluate differences between intervention and control groups the log rank test was performed. Mann–Whitney U test was used to analyse crying and fussing times, and the relative difference in crying and fussing between the baseline and the intervention weeks was measured as a percentage. p Values <0.05 were considered statistically significant.
Results
Participants and progress throughout the trial
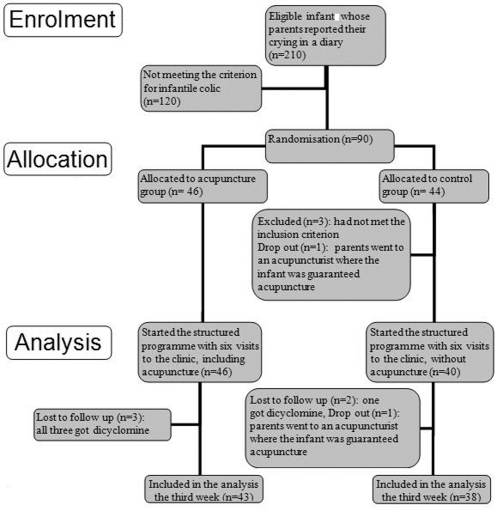
Of the 210 infants who between November 2005 and February 2007 were suspected to have colic, 90 fulfilled the colic criteria after completing the diary. Three infants randomised to the control group did not meet the criteria and were excluded, and the procedures for analysing the diaries before randomisation were changed (figure 1). Two infants in the acupuncture group who only came to the clinic five times as the symptoms disappeared are counted as fulfillers as their parents continued to complete the diary. Background data were analysed for infants starting the structured programme (n=86) and for infants who completed the three intervention weeks (n=81) (table 1). Outcomes from the intervention weeks are based on the infants' remaining in the study each week and drop outs are reported as missing values. Infants were stratified by age and age at inclusion was similar in both groups (table 1). However, owing to small numbers in the subgroups, age groups were analysed together.
Figure 1.
Flow chart of infants through the trial.
Table 1.
Baseline data for infants
| Infants starting the intervention (N=86) | Infants completing 3 weeks (N=81) | |||
|---|---|---|---|---|
| Background characteristics | Acupuncture group (n= 46) | Control group (n=40) | Acupuncture group (n= 43) | Control group (n=38) |
| Firstborn, n (%) | 22 (48) | 22 (55) | 21 (49) | 21 (55) |
| Gender, female, n (%) | 22 (48) | 19 (48) | 21 (49) | 19 (50) |
| Gestational age, weeks, mean (SD) | 39.2 (1.5) | 39.5 (1.3) | 39.3 (1.4) | 39.5 (1.3) |
| Age when colic started, weeks, mean (SD) | 1.9 (1.3) | 1.5 (1.0) | 2 (1.3) | 1.5 (1) |
| Age at inclusion, weeks, mean (SD) | 5.0 (1.9) | 5.3 (1.7) | 5.1 (1.9) | 5.2 (1.6) |
| Solely breastfed, n (%) | 35 (76) | 26 (65) | 32 (74) | 25 (66) |
| Having a parent and/or sibling with food intolerance/allergy, n (%) | 17 (37) | 18 (45) | 15 (35) | 17 (45) |
| Having a parent and/or sibling who had had infantile colic, n (%) | 29 (63) | 23 (58) | 25 (58) | 20 (53) |
Baseline data
There were no significant differences between the groups for background characteristics such as parents being born in Sweden, educational level, smoking and mother's complications during pregnancy or delivery; nor were there differences between their baseline levels of fussing and crying (tables 1 and 2).
Table 2.
Baseline data for fussing, crying, colicky crying and the total duration of fussing, crying and colicky crying (TC)
| Infants starting the intervention (N=86) | Infants completing 3 weeks (N=81) | |||||
|---|---|---|---|---|---|---|
| Categories of fussing and crying, min/day | Acupuncture group (n=46) | Control group (n= 40) | p Value | Acupuncture group (n=43) | Control group (n= 38) | p Value |
| Fussing, median (q1–q2) | 113 (57–178) | 146 (66–188) | 0.255 | 112 (57–161) | 148 (70–188) | 0.173 |
| Crying, median (q1–q2) | 86 (55–123) | 72 (36–119) | 0.170 | 85 (53–121) | 72 (34–119) | 0.228 |
| Colicky crying, median (q1–q2) | 37 (17–127) | 57 (21–96) | 0.515 | 37 (17–124) | 56 (20–92) | 0.418 |
| TC, median (q1–q2) | 260 (218–351) | 277 (231–370) | 0.286 | 251 (213–315) | 277 (230–368) | 0.187 |
Outcome measures
Rate of infants fulfilling the colic criterion in each of the intervention weeks
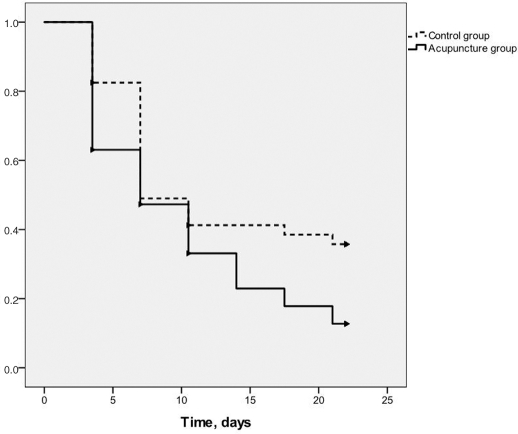
There was a difference (p=0.034) between groups in the time which passed from inclusion until the infant had a mean value for TC of <180 min/day for the first time, indicating that the infant no longer met the criteria for colic. Figure 2demonstrates this difference by showing the proportion of infants with a mean TC <180 min/day for each of the six treatment periods consisting of 3 or 4 days depending on whether treatment was given on a Monday or a Thursday. Median time until criteria for colic were no longer fulfilled was 7 days in both groups.
Figure 2.
Proportion of infants with a mean total duration of fussing, crying and colicky crying (TC) under 180 min/day for each of the six treatments.
Duration of fussing, crying and colicky crying
The duration of fussing was shorter in the acupuncture group during the first (p=0.029) and second (p=0.047) intervention weeks. The duration of colicky crying was shorter (p=0.046) in the acupuncture group during the second intervention week. However, TC was lower in the acupuncture group than in the control group as early as the first intervention week (p=0.025) and in the following intervention week (p=0.016) (table 3). A subanalysis showed TC to already be lower (p=0.005) in the acupuncture group after the first treatment. The relative difference between groups, measured as the percentage decrease of crying and fussing from baseline to intervention weeks 1, 2 and 3 showed differences between groups for fussing the first week (p=0.028), for colicky crying the second week (p=0.041) and for TC the second week (p=0.024) (table 4).
Table 3.
Fussing, crying, colicky crying and total duration of fussing, crying and colicky crying (TC) during the three intervention weeks for the infants still remaining in the trial at each of the intervention weeks
| First intervention week | Second intervention week | Third intervention week | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Categories of fussing and crying, min/day | Acupuncture group (n=46) | Control group (n=40) | p Value | Acupuncture group (n=44) | Control group (n=39) | p Value | Acupuncture group (n=43) | Control group (n=38) | p Value |
| Fussing, median (q1–q3) | 74 (53–154) | 129 (80–183) | 0.029 | 71 (41–123) | 102 (60–148) | 0.047 | 69 (36–109) | 85 (63–151) | 0.119 |
| Crying, median (q1–q3) | 76 (45–103) | 61 (30–102) | 0.428 | 52 (27–88) | 55 (24–73) | 0.964 | 54 (21–87) | 46 (22–98) | 0.846 |
| Colicky crying, median (q1–q3) | 20 (6–53) | 26 (9–48) | 0.634 | 9 (0–27) | 13 (4–49) | 0.046 | 3 (0–18) | 9 (0–18) | 0.087 |
| TC/day, median (q1–q3) | 193 (143–253) | 225 (178–316) | 0.025 | 164 (103–201) | 188 (149–273) | 0.016 | 149 (92–193) | 169 (119–267) | 0.062 |
Table 4.
Relative difference in fussing, crying, colicky crying and total duration of fussing, crying and colicky crying (TC) between the baseline week and the first, second and third intervention weeks, respectively
| Difference baseline – first intervention week | Difference baseline – second intervention week | Difference baseline – third intervention week | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Categories of crying and fussing, median min/day | Acupuncture group (n=46) | Control group (n=40) | p Value | Acupuncture group (n=44) | Control group (n=39) | p Value | Acupuncture group (n=43) | Control group (n=38) | p Value |
| Fussing, difference in % (min−max in %) | 22 (−956, 84) | 6 (−1614, 57) | 0.028 | 30 (−210, 98) | 26 (−2071, 89) | 0.158 | 43 (−317, 100) | 30 (−2242, 98) | 0.291 |
| Crying, difference in % (min−max in %) | 12 (−219, 100) | 13 (−786, 89) | 0.726 | 34 (−217, 100) | 30 (−486, 95) | 0.784 | 39 (−107, 100) | 44 (−543, 100) | 0.936 |
| Colicky crying, difference in % (min−max in %) | 57 (−443, 100) | 57 (−1050, 100) | 0.921 | 92 (−700, 100) | 73 (−191, 100) | 0.041 | 92 (8, 100) | 81 (−600, 100) | 0.062 |
| TC, difference in % (min−max in %) | 27 (−59, 69) | 16 (−59, 75) | 0.060 | 44 (−25, 92) | 29 (−67, 84) | 0.024 | 48 (−23, 86) | 42 (−71, 90) | 0.219 |
Adverse events
Slight bleeding (one drop) was detected after needling in one of the 256 acupuncture treatments administered. Thirty-two infants (74%) in the acupuncture group cried for more than 10 s during one to four interventions in the treatment room compared with 14 infants (37%) in the control group (p = 0.009) (table 5). Crying lasted more than a minute in 37 out of 256 needling occasions (14%). No infant cried for more than 2 min. No other adverse events were reported.
Table 5.
Infants who cried more than 10 s in the treatment room during the intervention
| Infants who cried more than 10 s during … | Acupuncture group (n=43) | Control group (n=38) | Total |
|---|---|---|---|
| … None of the treatments, n (%) | 11 (26) | 24 (63) | 35 (43) |
| … 1 Treatment, n (%) | 17 (40) | 10 (26) | 27 (33) |
| … 2 Treatments, n (%) | 8 (19) | 3 (8) | 11 (14) |
| … 3 Treatments, n (%) | 4 (9) | 1 (3) | 5 (6) |
| … 4 Treatments, n (%) | 3 (7) | 0 (0) | 3 (4) |
| … 5 or 6 Treatments, n (%) | 0 (0) | 0 (0) | 0 (0) |
Discussion
In this study where both acupuncture and control groups were allotted six visits with support and counselling as an intervention beside their ordinary child health centre visits, there was an expected decrease in TC in both groups.19 However, the decrease was slightly faster in the acupuncture group as shown by measuring both absolute and relative differences between groups. There was a small but significant difference between groups already after the first treatment and in the duration until the infants no longer fullfilled the colic criterion. Spontaneous healing might explain the lack of difference between groups during the third intervention week. The results of this study are in agreement with the only RCT on acupuncture in infantile colic published,16 in which 40 infants were included, of whom 20 were needled in LI4 bilaterally for 20 s. Spontaneous remission was more likely to occur in that study as some of the infants were older than 8 weeks. Furthermore, the parents were blinded but not the nurse meeting the parents and administering the acupuncture.
Strengths and limitations of this study
The strengths of our study are the randomisation, the blinding of the parents, the small number of drop-outs and strict protocol, including an extensive diary validated in several studies.18 20 21 Furthermore, the infants were included before their eighth week in order to minimise the risk of spontaneous healing during the study period, and infants recovering after a 5-day period excluding cow's milk were not included.
Blinding patient and practitioner and finding an inert control are considerable methodological problems in acupuncture research.22–27 As parents could easily be influenced by the acupuncturist's enthusiasm, an advantage of this study was that the nurse they met was blinded to the infants' allocation. The structured programme, ensuring equal support and advice to all participating families influenced both groups equally, is a strength. Infants in both groups lacked expectations and had limited communication skills, thereby eliminating any difference in placebo effect in them and in their blinded parents.
No test of blinding was done after the three intervention weeks, which is a limitation. More infants in the acupuncture group than in the control group started to cry in the treatment room. Parents might have heard the infants cry and thus suspected that the infant had received acupuncture. However the fussing/crying lasted for <10 s in most cases. On one occasion one infant cried for more than a minute after the acupuncture treatment but none cried for more than 2 min, indicating that this light acupuncture treatment was well tolerated by the infants.
The safety of acupuncture is a major concern, particularly during early infancy when responses are difficult to evaluate. In a review, acupuncture was considered a safe modality for paediatric patients, but the authors advised that fewer needles should be used when treating children.28 In accordance with this our study used one single point with light stimulation. As different acupuncture points result in different effects29–32 55 the option of choosing points individually after analysing all symptoms presented in an ordinary clinical setting may increase efficacy of future acupuncture treatment of colic. The six treatments in this study may be more than needed.
Possible mechanisms and explanations
Most basic acupuncture research is conducted with electroacupuncture on animals, and cannot be generalised to manual acupuncture in infants. However, it is known that acupuncture in animals inhibits somatic33–36 and visceral pain37 38 and has an effect on the autonomous system.25–27 39–44 Stimulating LI4 bilaterally resulted in more immediate effect than unilateral stimulation.39 The motility in the intestinal tract and the gastric acid secretion increased or decreased depending on which points were needled.29 30 32 45 46 In human adults47–49 and children50 acupuncture had a beneficial effect on visceral symptoms like nausea. Acupuncture increased bowel movement in children,51 altered gastric motility52 and affected gastric emptying in adults with motility disorders53 but caused no effect on gastric motility in healthy individuals.54 Manual acupuncture applied to LI4 induced an increase in the sympathetic and parasympathetic nervous systems in 12 healthy individuals.55
It is possible that infantile colic derives from distension of the intestines and activation of the autonomic nervous system and that acupuncture can influence both visceral pain and the autonomic nervous system. Thus it is plausible that even modest stimulation of LI4, as performed in this study, can influence either or both mechanisms and thereby alleviate infantile colic.
Generalisability
This study includes infants with eczema, a rash from a Von Rosen splint, a temperature, a hand burned by boiling water and infants whose mothers had a high level of anxiety or depression. In this aspect the participants represent clinical reality, and these afflictions were equally distributed among the groups. Parents who were negative about exposing their children to acupuncture or who lacked the ability to complete the diaries did not participate and infants born prematurely were excluded. This leaves the included sample and the results of this study as reasonably representative of the general population.
Clinical implications
Parents have described colic as a strain on the family.7–9 As no safe and effective cure is known we assume that even a short reduction of the colicky period can make a difference. Of the 210 infants estimated by the parents to have colic, only 90 fulfilled the criteria after registration of their symptoms in the diary. This indicates that parents have a tendency to overestimate the crying, and a diary in which parents note their infant's crying could be a valuable diagnostic tool. Another explanation may be that the definition of colic does not reflect the parent's experience of what they consider to be colic.
Conclusion
Standardised, light stimulation of the acupuncture point LI4 twice a week for 3 weeks reduced the duration and intensity of crying more quickly in the acupuncture group than in the control group. No serious side effects were reported. Future research is needed to validate the results and to investigate the efficacy of other acupuncture points and modes of stimulation for the treatment of infantile colic.
Summary points.
-
▶
Previous reports suggested acupuncture might reduce infantile colic.
-
▶
We conducted a randomised controlled trial in 90 infants.
-
▶
Acupuncture showed a small but significant effect on some outcomes.
Acknowledgments
Thanks to Margareta Normark for providing acupuncture, to Per Nyberg for statistical support.
Footnotes
Funding The authors thank Ekhagastiftelsen, Magn Bergvalls Stiftelse, General Maternity Hospital Foundation, Pampers and Baby Bag for funding.
Competing interests None.
Ethics approval This study was conducted with the approval of the Lund University, Research Ethics Committee (Dnr 583/2005).
Provenance and peer review Not commissioned; externally peer reviewed.
References
- 1.Canivet C. Infantile Colic. Risk Factors in Pregnancy, Maternal Reports and Outcome at 4 Years of Age. Thesis. Lund University, 2002
- 2.Canivet C, Jakobsson I, Hagander B. Colicky infants according to maternal reports in telephone interviews and diaries: a large Scandinavian study. J Dev Behav Pediatr 2002;23:1–8 [DOI] [PubMed] [Google Scholar]
- 3.Lucassen PL, Assendelft WJ, Gubbels JW, et al. Effectiveness of treatments for infantile colic: systematic review. BMJ 1998;316:1563–9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wade S, Kilgour T. Extracts from “clinical evidence”: Infantile colic. BMJ 2001;323:437–40 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Garrison MM, Christakis DA. A systematic review of treatments for infant colic. Pediatrics 2000;106:184–90 [PubMed] [Google Scholar]
- 6.Hiscock H. The crying baby. Aust Fam Physician 2006;35:680–4 [PubMed] [Google Scholar]
- 7.Keefe MR, Froese-Fretz A. Living with an irritable infant: maternal perspectives. MCN Am J Matern Child Nurs 1991;16:255–9 [DOI] [PubMed] [Google Scholar]
- 8.Keefe MR, Kajrlsen KA, Lobo ML, et al. Reducing parenting stress in families with irritable infants. Nurs Res 2006;55:198–205 [DOI] [PubMed] [Google Scholar]
- 9.Wade K, Black A, Ward-Smith P. How mothers respond to their crying infant. J Pediatr Health Care 2005;19:347–53 [DOI] [PubMed] [Google Scholar]
- 10.Reijneveld SA. Re: Age-related incidence curve of hospitalized Shaken Baby Syndrome cases: convergent evidence for crying as a trigger to shaking (Barr, Trent, & Cross, 2006). Child Abuse Negl 2007;31:601–2 [DOI] [PubMed] [Google Scholar]
- 11.Reijneveld SA, van der Wal MF, Brugman E, et al. Infant crying and abuse. Lancet 2004;364:1340–2 [DOI] [PubMed] [Google Scholar]
- 12.van der Wal MF, van den Boom DC, Pauw-Plomp H, et al. Mothers' reports of infant crying and soothing in a multicultural population. Arch Dis Child 1998;79:312–17 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Liu HR. Night crying in infants treated by acupuncture. J Chin Med 1994;46:38 [Google Scholar]
- 14.Zhao B. Treatment of infantile morbid night crying by acupuncture at Zhongchong point in 100 cases. J Tradit Chin Med 2002;22:11. [PubMed] [Google Scholar]
- 15.Landgren K, Hallström I. Akupunkturbehandling vid spädbarnskolik – föräldrars upplevelser av barnets beteende före och efter behandling. Vård i Norden 2005;1:26–31 [Google Scholar]
- 16.Reinthal M, Andersson S, Gustafsson M, et al. Effects of minimal acupuncture in children with infantile colic - a prospective, quasi-randomised single blind controlled trial. Acupunct Med 2008;26:171–82 [DOI] [PubMed] [Google Scholar]
- 17.Barr RG, Trent RB, Cross J. Age-related incidence curve of hospitalized Shaken Baby Syndrome cases: convergent evidence for crying as a trigger to shaking. Child Abuse Negl 2006;30:7–16 [DOI] [PubMed] [Google Scholar]
- 18.Canivet C, Hagander B, Jakobsson I, et al. Infantile colic–less common than previously estimated? Acta Paediatr 1996;85:454–8 [DOI] [PubMed] [Google Scholar]
- 19.Olafsdottir E, Forshei S, Fluge G, et al. Randomised controlled trial of infantile colic treated with chiropractic spinal manipulation. Arch Dis Child 2001;84:138–41 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Barr RG, Kramer MS, Boisjoly C, et al. Parental diary of infant cry and fuss behaviour. Arch Dis Child 1988;63:380–7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.St James-Roberts I, Plewis I. Individual differences, daily fluctuations, and developmental changes in amounts of infant waking, fussing, crying, feeding, and sleeping. Child Dev 1996;67:2527–40 [PubMed] [Google Scholar]
- 22.Cao X. Scientific bases of acupuncture analgesia. Acupunct Electrother Res 2002;27:1–14 [DOI] [PubMed] [Google Scholar]
- 23.NIH Consensus Conference Acupuncture. JAMA 1998;280:1518–24 [PubMed] [Google Scholar]
- 24.Birch S. Clinical research on acupuncture. Part 2. Controlled clinical trials, an overview of their methods. J Altern Complement Med 2004;10:481–98 [DOI] [PubMed] [Google Scholar]
- 25.Birch S. A review and analysis of placebo treatments, placebo effects, and placebo controls in trials of medical procedures when sham is not inert. J Altern Complement Med 2006;12:303–10 [DOI] [PubMed] [Google Scholar]
- 26.Birch S, Hesselink JK, Jonkman FA, et al. Clinical research on acupuncture. Part 1. What have reviews of the efficacy and safety of acupuncture told us so far? J Altern Complement Med 2004;10:468–80 [DOI] [PubMed] [Google Scholar]
- 27.Madsen MV, Gøtzsche PC, Hróbjartsson A. Acupuncture treatment for pain: systematic review of randomised clinical trials with acupuncture, placebo acupuncture, and no acupuncture groups. BMJ 2009;338:a3115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Jindal V, Ge A, Mansky PJ. Safety and efficacy of acupuncture in children: a review of the evidence. J Pediatr Hematol Oncol 2008;30:431–42 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Noguchi E, Ohsawa H, Tanaka H, et al. Electro-acupuncture stimulation effects on duodenal motility in anesthetized rats. Jpn J Physiol 2003;53:1–7 [DOI] [PubMed] [Google Scholar]
- 30.Sato A, Sato Y, Suzuki A, et al. Neural mechanisms of the reflex inhibition and excitation of gastric motility elicited by acupuncture-like stimulation in anesthetized rats. Neurosci Res 1993;18:53–62 [DOI] [PubMed] [Google Scholar]
- 31.Li YQ, Zhu B, Rong PJ, et al. Effective regularity in modulation on gastric motility induced by different acupoint stimulation. World J Gastroenterol 2006;12:7642–8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Li YQ, Zhu B, Rong PJ, et al. Neural mechanism of acupuncture-modulated gastric motility. World J Gastroenterol 2007;13:709–16 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Rong PJ, Zhu B, Huang QF, et al. Acupuncture inhibition on neuronal activity of spinal dorsal horn induced by noxious colorectal distention in rat. World J Gastroenterol 2005;11:1011–17 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Newberg AB, Lariccia PJ, Lee BY, et al. Cerebral blood flow effects of pain and acupuncture: a preliminary single-photon emission computed tomography imaging study. J Neuroimaging 2005;15:43–9 [DOI] [PubMed] [Google Scholar]
- 35.Qin W, Tian J, Bai L, et al. FMRI connectivity analysis of acupuncture effects on an amygdala-associated brain network. Mol Pain 2008;4:55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Sakai S, Hori E, Umeno K, et al. Specific acupuncture sensation correlates with EEGs and autonomic changes in human subjects. Auton Neurosci 2007;133:158–69 [DOI] [PubMed] [Google Scholar]
- 37.Cui KM, Li WM, Gao X, et al. Electro-acupuncture relieves chronic visceral hyperalgesia in rats. Neurosci Lett 2005;376:20–3 [DOI] [PubMed] [Google Scholar]
- 38.Zhou EH, Liu HR, Wu HG, et al. Suspended moxibustion relieves chronic visceral hyperalgesia via serotonin pathway in the colon. Neurosci Lett 2009;451:144–7 [DOI] [PubMed] [Google Scholar]
- 39.Lin TB, Fu TC. Effect of electroacupuncture on blood pressure and adrenal nerve activity in anesthetized rats. Neurosci Lett 2000;285:37–40 [DOI] [PubMed] [Google Scholar]
- 40.Lin TB, Fu TC, Chen CF, et al. Low and high frequency electroacupuncture at Hoku elicits a distinct mechanism to activate sympathetic nervous system in anesthetized rats. Neurosci Lett 1998;247:155–8 [DOI] [PubMed] [Google Scholar]
- 41.Ting H, Liao JM, Lin CF, et al. Pressor effect on blood pressure and renal nerve activity elicited by electroacupuncture in intact and acute hemorrhage rats. Neurosci Lett 2002;327:5–8 [DOI] [PubMed] [Google Scholar]
- 42.Iwa M, Matsushima M, Nakade Y, et al. Electroacupuncture at ST-36 accelerates colonic motility and transit in freely moving conscious rats. Am J Physiol Gastrointest Liver Physiol 2006;290:G285–92 [DOI] [PubMed] [Google Scholar]
- 43.Luo D, Liu S, Xie X, et al. Electroacupuncture at acupoint ST-36 promotes contractility of distal colon via a cholinergic pathway in conscious rats. Dig Dis Sci 2008;53:689–93 [DOI] [PubMed] [Google Scholar]
- 44.Liao JM, Lin CF, Ting H, et al. Electroacupuncture at Hoku elicits dual effect on autonomic nervous system in anesthetized rats. Neurosci Res 2002;42:15–20 [DOI] [PubMed] [Google Scholar]
- 45.Noguchi E, Hayashi H. Increases in gastric acidity in response to electroacupuncture stimulation of the hindlimb of anesthetized rats. Jpn J Physiol 1996;46:53–8 [DOI] [PubMed] [Google Scholar]
- 46.Jin HO, Zhou L, Lee KY, et al. Inhibition of acid secretion by electrical acupuncture is mediated via beta-endorphin and somatostatin. Am J Physiol 1996;271:G524–30 [DOI] [PubMed] [Google Scholar]
- 47.Ezzo J, Streitberger K, Schneider A. Cochrane systematic reviews examine P6 acupuncture-point stimulation for nausea and vomiting. J Altern Complement Med 2006;12:489–95 [DOI] [PubMed] [Google Scholar]
- 48.Ezzo JM, Richardson MA, Vickers A, et al. Acupuncture-point stimulation for chemotherapy-induced nausea or vomiting. Cochrane Database Syst Rev 2006;2:CD002285 [DOI] [PubMed] [Google Scholar]
- 49.Lee A, Fan LT. Stimulation of the wrist acupuncture point P6 for preventing postoperative nausea and vomiting. Cochrane Database Syst Rev 2009;2:CD003281 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Dune LS, Shiao SY. Metaanalysis of acustimulation effects on postoperative nausea and vomiting in children. Explore (NY) 2006;2:314–20 [DOI] [PubMed] [Google Scholar]
- 51.Broide E, Pintov S, Portnoy S, et al. Effectiveness of acupuncture for treatment of childhood constipation. Dig Dis Sci 2001;46:1270–5 [DOI] [PubMed] [Google Scholar]
- 52.Chang CS, Chou JW, Ko CW, et al. Cutaneous electrical stimulation of acupuncture points may enhance gastric myoelectrical regularity. Digestion 2002;66:106–11 [DOI] [PubMed] [Google Scholar]
- 53.Takahashi T. Acupuncture for functional gastrointestinal disorders. J Gastroenterol 2006;41:408–17 [DOI] [PubMed] [Google Scholar]
- 54.Yim YK, Kang WC, Cho JH, et al. Crossover clinical trial to determine the effect of manual acupuncture at Siguan points (bilateral LI4 and LR3) on intestinal motility in healthy subjects. Am J Chin Med 2007;35:209–18 [DOI] [PubMed] [Google Scholar]
- 55.Haker E, Egekvist H, Bjerring P. Effect of sensory stimulation (acupuncture) on sympathetic and parasympathetic activities in healthy subjects. J Auton Nerv Syst 2000;79:52–9 [DOI] [PubMed] [Google Scholar]