Abstract
Background
Maternal functional status is important to capture in the 12 months after childbirth, as this period marks a critical window for both mother and child. In most cases, mothers are the primary caregivers and are, therefore, responsible for the majority of the work related to infant care tasks, such as feeding, diaper changes, and doctor's appointments. Additionally, the quality of mother-child interaction in the year after childbirth affects child development. To date, postpartum functioning has exacted scarce coverage, with only one instrument claiming to measure the concept explicitly. This necessitated the development of the Barkin Index of Maternal Functioning (BIMF), which was designed to measure functioning in the year after childbirth.
Methods
Three focus groups comprised of 31 new mothers were held to elicit women's concept of functioning in the first postpartum year. Women were asked to discuss the responsibilities associated with new motherhood as well as the circumstances surrounding high and low functioning periods.
Results
The qualitative data produced by the focus groups were coded by emotive tone and content and translated into item construction for the BIMF, a 20-item self-report measure of functioning intended for use in the year after childbirth. Before implementation into the screening study, the BIMF was critiqued by a panel of experts and cross-checked with the literature to ensure that no major contextual domains were absent. Psychometric testing revealed adequate internal reliability and construct validity, and the BIMF has been implemented successfully in clinical settings.
Conclusions
The high level of patient engagement and psychometric properties associated with the BIMF are indicative of its potential to become a valuable tool for assessing maternal wellness.
Introduction
Maternal functional status is important to capture in the 12 months after birth, as this period marks a critical window for mother and child. In most cases, mothers are the primary caregivers1 and are responsible for the majority of the work related to infant care tasks, such as feeding, diaper changes, and doctor's appointments. The emotional aspect of mothering is equally as important to the child's development. In fact, the quality of mother-child interaction in the year after birth affects infant development.2 In addition to fostering the child's physical and emotional health, a woman must integrate infant care into her existing responsibilities. Although the role of mother can be deeply satisfying, it is also laden with challenges. As with all personal challenges, an individual's level of functioning can prove an asset or a hindrance. High levels of maternal functioning are likely to correlate with positive infant development outcomes. Likewise, impaired functioning in the postpartum period might impede optimal infant development. Proper assessment of postpartum functioning has the potential to provide valuable information about the mother's level of competence in the maternal role.
In a study by Barkin et al.,3 a group of commonly used maternal assessments that measure related constructs such as maternal competence,4 maternal gratification,5,6 infant care tasks,7 feelings about one's baby,8 and subjective evaluation of new motherhood9,10 were evaluated for their coverage of maternal functional status. The analysis revealed that none of the systematically selected assessments were appropriate for measurement of functional status. Maternal adjustment measures, such as the Postpartum Adjustment Questionnaire (PPAQ)11 and the Maternal Adjustment and Maternal Attitudes questionnaire (MAMA),12 as well as the newer, less established instruments, did not meet inclusion criteria at the time of assessment for the Barkin et al. study.3 However, it is possible that these instruments also afford some coverage of maternal functioning.
Despite the substantial number of existing maternal assessments, until recently, the Inventory of Functional Status After Childbirth (IFSAC)13 was the only instrument designed explicitly for the measurement of maternal functional status in the postpartum period.14 However, Aktan stated of the IFSAC, “Although another tool to measure functional status after childbirth does not exist, the use of this tool without refinement may lead to questionable research findings.”14 The premise on which optimal maternal functioning is based represents a limitation of the IFSAC. In order to achieve full functional status, a woman must resume the majority of the roles she possessed before giving birth. Because of the natural reprioritizing that often occurs in the life of a new mother, a return to full functional status (as measured by the IFSAC) can be difficult for many women.15 Additionally, the IFSAC does not account for women's feelings or levels of satisfaction with the changes in their lives since childbirth.13,15 These characteristics may, in part, be a reflection of the methods used to develop the IFSAC. Initial item development for the IFSAC can be traced back to the Sickness Impact Profile16 and from literature related to the postpartum experience. Maternal input seems to have been solicited on a limited basis during the item refinement process. The degree to which the input influenced the content of the instrument is unclear.
The Barkin Index of Maternal Functioning (BIMF) was developed as an alternative to the IFSAC in the pursuit of measuring maternal functional status. Despite having a similar goal, the BIMF's development process differed from that of the IFSAC. The BIMF is not tied to a theoretical framework, whereas the IFSAC was based on the role adaptive function of Roy's Adaptation Model.17 Therefore, development of the BIMF was not subject to any predetermined criteria but rather was driven by the perspectives of 31 new mothers revealed during focus group discussions. This grass-roots approach was determined by the study team to be the most efficient method of producing a patient-centered measure of functional status. In addition to providing access to the participants' own meanings of health and illness,18 focus groups are an inexpensive means of both interviewing several people at once19 and becoming familiar with the language of the study population. Assigning this level of significance to the views of the population experiencing the condition of interest (in this case, functioning in the postpartum) also serves to maximize content validity.20
The primary purpose of this article is to describe how qualitative methods were used to develop the BIMF. Researchers wishing to use qualitative data to develop health-related measures may also use this as an example. The role of expert input and the literature is discussed, along with a brief reporting of reliability and validity.
Materials and Methods
Overview of focus group study plan
Planning began in November of 2007, when several logistical and methodological decisions were made about the focus group study. Through this planning process, the study team outlined subject inclusion criteria, a recruiting strategy, and determined that three focus groups were feasible. The most important methodological decision made in the planning stage was the choice of discussion questions, which were constructed with the purpose of understanding the mothers' conceptualizations of postpartum functioning. Details about the content of these questions are discussed in a subsequent section.
Recruitment
Recruitment took place from February 13, 2008, to March 26, 2008, subsequent to approval from the participating university's Institutional Review Board. Recruiting fliers were posted in daycare facilities, university hospitals, and elementary schools located in a large metropolitan area in Western Pennsylvania. Efforts to draw a diverse sample were coordinated with a local university's minority health center. Word of mouth was a force in the recruitment process, as people would often tell friends who had recently given birth about the study. In order to be eligible to participate, women had to (1) have given birth in the year before enrollment and (2) be at least 18 years of age. Once eligibility was confirmed, women chose the focus group that best fit their schedule, constituting a one-time, 2-hour commitment. In total, 33 women enrolled and 31 participated. Two women dropped out because of child care constraints. Attendance was similar across the focus groups, with 11 women participating in the first session, and 10 attending each of the remaining sessions. Women were compensated with gift cards to a local grocery store, which likely contributed to the high rate of participation.
Focus group logistics
The three focus groups were logistically identical, each being held in the evening at a local university's conference center in March of 2008. Dinner and parking were provided as incentives and for the participants' convenience. The environment for focus groups should set the tone for an intimate, productive discussion. Therefore, in order to promote direct communication, the tables were arranged so that women were facing each other.
Before the discussion, women were asked to fill out a short anonymous demographic survey and the Center for Epidemiologic Studies Depression Scale (CES-D).21 The demographic survey comprised 11 items, 7 of which were aimed at characterizing the mother. These 7 variables were age, race, ethnicity, marital status, employment status, education level, and household income. Information about the age of the infant, number of children and adults in the household, and use of daycare services was collected in order to gauge the maternal levels of burden and support.
Opening remarks and confidentiality
The focus groups commenced with prepared dialogue from the facilitator. The opening remarks were meant to both comfort and inform the participants about the importance of their contributions. The facilitator explained that the purpose of the discussion was to better understand women's experiences in the year after birth and that this information would be used to design a measure of maternal functioning. This approach of placing participants' contributions in context was successful in the Portland Men's Study, in which focus groups served as a resource for the development of a survey of health behavior.19
Participants were encouraged to express their views openly, and logistics, such as discussion length and roles of the facilitator and note taker, were reviewed. The facilitator explained that the discussion would be audiotaped and transcribed for purposes of analysis. Therefore, women were instructed to use first names only, which were placed on name tents in front of them to protect their confidentiality. Women were assured that although their statements might be quoted in the development documentation of the measure, specific names would not be connected to the dialogue. Finally, women were given a chance to ask questions or voice concerns. In general, the women appeared comfortable and ready to begin the discussions.
Discussion topics
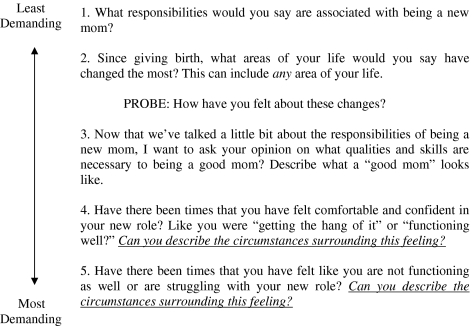
A strength of focus groups as a vehicle for data collection lies in their semistructured nature. Whereas the participants could venture into uncharted topical territories, the discussions were guided by the research questions of interest. The questions chosen for the focus groups and displayed in Figure 1 were selected in accordance with group process, which dictates that the questions progress from easy to more demanding as the participants became more comfortable and prone to self-disclosure. Mothers were initially asked to discuss the responsibilities associated with new motherhood and the changes that occurred since birth. These questions allowed for factual answers, even if the mother chose to reveal more in her response. The third discussion topic: Describe what a “good mom” looks like, was an attempt to access the women's conceptualization of a high-functioning mother. For the last two questions, mothers were asked to describe the circumstances surrounding high-functioning and low-functioning periods. These questions about the functioning spectrum were couched in conversational language for the benefit of the participants.
FIG. 1.
Focus group questions.
Results
Demographics of participants
Survey results indicated that most participants were married (80.7%), non-Hispanic (96.8%), and living with at least one other adult (93.5%). The racial composition of the sample was white (80.6%), black (16.2%), and Asian (3.2%), which is typical of the Pittsburgh community. The participant's mean age was 30.9 years (standard deviation [SD] 4.1), and the infants were 6.6 months (SD 3.6) old on average. In terms of employment status, 40% of women were working part-time, 36.7% were working full-time, and 23.3% were stay-at-home mothers. Additionally, 46.7% of the women had a postgraduate education, 41.9% had a total yearly household income in the $70,001–$100,000 range, 58.1% were primiparous, 54.8% were using daycare to some degree, and 26.7% had high levels of depressive symptoms, according to the CES-D (scored ≥16 on the CES-D).
Participant response
In general, the discussions were robust and flowing, with few periods of silence. The women welcomed the opportunity to commiserate with other new mothers. Lack of self-disclosure was not an issue as women discussed feelings of inadequacy, depression, struggles with body image and breastfeeding, pumping breast milk in the workplace, lack of sex drive, loss of identity, lack of social support, and management of abusive instincts toward their infant. All the prescribed questions were answered, and often the discussion was led into unforeseen territory by the participants. There was a repetition of themes across all three focus groups, which provided evidence of the generalizability of the findings. Many of the themes, such as the importance of self-care, were constant across race and education level. For example, white and black women alike felt that whereas becoming less selfish was necessary to motherhood, tending to oneself (physically and emotionally) was equally important. Women with different levels of education agreed that “managing the worry” associated with infant care was also a key ingredient to functioning. The women felt that pervasive anxiety affected both their quality of life and mother-child interaction. At the conclusion of each focus group, the facilitator and note taker convened separately to discuss the pertinent themes of the discussions as well as their general impressions.
Coding of data and formulation of survey questions
The recorded conversations were transcribed and returned to the study team in the form of text files. Codes were then created to characterize the discussion themes. Each conversation piece was assigned a code based on emotive tone and content. Statements with similar codes were gathered together, and survey items were formed. A total of seven codes that translated into functional areas were identified in the qualitative analysis. Social support, management, mother-child interaction, infant care, self-care, adjustment, and psychological well-being (of mother) served as both analysis codes and domains of maternal functioning.
Social support
As mentioned earlier, the importance of social support was a recurrent theme throughout the discussions:
Participant: To build that confidence… I know my pediatrician, she's almost like a cheerleader.…She just sits there and goes go, go, you're doing great. And I'm like oh my god … I'm doing this right. And then you need your mom or someone else who's gone through it … you need to build like this group of people around you who all say you're doing awesome no matter what. …
This statement (and similarly themed statements) was coded as “social support” and lent itself to the formulation of BIMF item 9: I am getting enough encouragement from other people.
Management
The participants also discussed a substantial increase in their overall level of responsibility:
Participant: I feel like I'm managing everything now. Like, if I want something done, I'm the one that's responsible for delegating that … Well, why am I the one who knows that the baby needs to be fed and … you know, and the trash needs to be taken out?
These types of comments were coded as “management” and translated into BIMF item 17: I am able to take care of my baby and my other responsibilities.
Mother-child interaction
When asked for examples of high-functioning periods, women often cited instances in which they were able to remain focused on their child exclusively:
Participant: I think for me being in a good place means that I can appreciate those little moments where you're just having that happy interaction or you notice the new skill that they just learned and you're able to just sort of soak in that moment.…
This sentiment was common and was the impetus for BIMF item 5: I am able to relax and enjoy time with my baby. This comment was categorized as “mother-child interaction.”
Infant care
Infant care, perhaps the most obvious responsibility of new motherhood, was described by one of the participants:
Participant: Feeding them. Keeping them clean. Changing diapers. Calming temper tantrums. I have more than one, you can tell. Basically that's it. Doctor's appointments.
There were many accounts of the tasks that comprise infant care; this dialogue translated into BIMF item 12: I am taking good care of my baby's physical needs (feedings, changing diapers, doctor's appointments).
Self-care
Women in each of the three groups discussed the need to take care of themselves in order to remain a healthy mother. One aspect of self-care for the mothers was occasionally taking time for themselves. However, this aspect of self-care was often accompanied by feelings of guilt:
Participant: I get such guilt about taking time … taking time for myself. I think, am I in this tub too long? Do I need to get out and go see what's going on? When you're in the middle of it, it's hard to see. And I think that's the most important thing for a mom is just to take care of herself.
Coded as “self-care,” this comment and others resembling it served as the basis for BIMF item 11: I take a little time each week to do something for myself.
Adjustment
Some of the women believed they became acclimated to motherhood as time passed:
Participant 1: I feel like as you get older, as they get older, I think it starts getting slightly easier. And I guess because they start becoming a little bit more independent.
Statements of this genre were coded as “adjustment” and contributed to the development of item 19: As time goes on, I am getting better at taking care of my baby.
Psychological well-being
Perhaps one of the strongest themes throughout the discussions was the connection between the mother's mental and physical health and effective mothering.
Participant: I had a bad case of postpartum depression, and it was all getting a little scary. I was debating about whether to go on medication because I was breastfeeding and the nurse practitioner said to me the most important thing this child needs is a healthy mother. Healthy, happy mother. If you aren't taking care of yourself, you can't take care of this child.
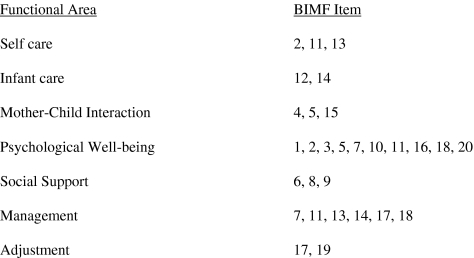
This conversation piece was one of many that were assigned multiple codes because it touches on aspects of infant care, self-care, and psychological well-being. Because of its emotive tone (and content), it was given a primary code of “psychological well-being.” Each of the BIMF's 20 items was associated with at least one of the seven maternal functional domains. Several of the items related to more than one domain. This item-domain mapping is displayed in Figure 2. It is important to note that these are the anticipated item-domain mappings based on information gleaned from the focus group study. These mappings should be confirmed via a rigorous factor analysis.
FIG. 2.
Barkin Index of Maternal Functioning (BIMF) item-domain mapping.
Twenty survey items, constituting the first draft of the BIMF, were generated as a result of this qualitative data analysis process. Each item was derived from the women's personal accounts of their postpartum experiences.
Expert review panel
Upon formulation of the first draft of the instrument, an expert panel was assembled for the purposes of critiquing the instrument. The panel included 11 professionals with expertise in at least one of the following areas: survey design, qualitative data analysis, psychiatry, women's health, and reproductive health. This meeting resulted in a rewording of several survey items and a movement toward a seventh grade reading level. Because of its composition, the panel was mindful of the target population and aided in eliminating complicated item wording. There was also substantial discussion about how this instrument compared with general measures of functioning. This process provided assurance that the relevant domains of functioning were present in the resulting instrument. Additionally, a 2-week time delimiter, intended to make the instrument more viable in clinical settings, was added to the instructions. No survey items were added or removed as a result of this process.
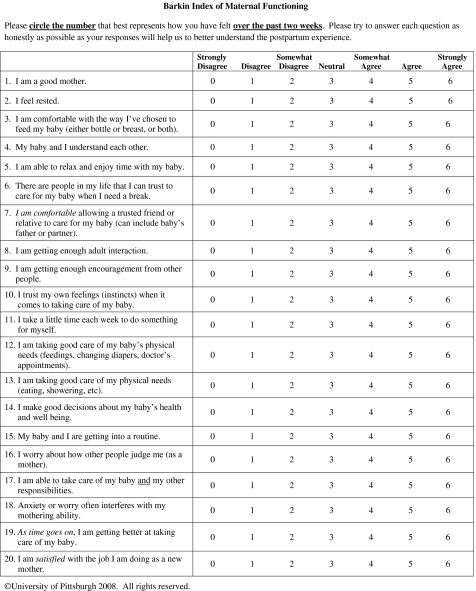
Scoring of the BIMF
A total score is generated from summing the 20 items (after the reverse-coding of items 16 and 18) and ranges from 0 to 120. Higher total scores are associated with greater levels of functioning. The measure takes approximately 5–10 minutes to complete and is shown in Figure 3.
FIG. 3.
Barkin Index of Maternal Functioning. The copyright for the BIMF is owned by the University of Pittsburgh; the BIMF may be reprinted without charge only for noncommercial research and educational purposes. You may not make changes or modifications to the BIMF without prior written permission from the University of Pittsburgh. If you would like to use this instrument for commercial purposes or for commercially sponsored research, please contact the Office of Technology Management at the University of Pittsburgh at 412-648-2206 for licensing information. Questions about the development of the BIMF may be directed to Jennifer L. Barkin, Ph.D. E-mail: barkinj@gmail.com
Role of the literature
Whereas focus groups are being used more frequently as a method for constructing health-related surveys, many existing instruments were developed using a top-down approach.20 Typically, the research literature and clinician input determined much of the instruments' framework and content. The danger inherent in this approach lies in its neglect of patient experience, which poses a threat to content validity.20 However, the research literature can serve as a valuable benchmark for information gleaned from focus groups. The focus group work in this article resulted in a novel way of measuring maternal functional status, and there was some conceptual overlap with the literature. Logsdon et al.1 define the key components of mothering as (1) maternal-infant interaction, (2) caretaking of infant, (3) providing healthcare for the child, and (4) finding gratification in the mothering role. Components 1 and 4 are analogous to the mother-child interaction domain presented in this article, and components 2 and 3 are related to the infant care domain. Fawcett et al. described maternal functional status as “a multidimensional concept encompassing the mother's readiness to assume infant care responsibilities and resume self-care, household, social and community, and occupational activities.”13 Infant care, self-care, and social aspects are also measured by the BIMF, albeit via a different approach (Table 1). Specific household and occupational activities are not addressed by the BIMF. However, women are asked to rate their own level of resource management by item 17: I am able to take care of my baby and my other responsibilities. This focus on the ability to achieve balance rather than execution of specific household/occupational tasks reflects the themes of the focus groups. Although the two definitions of maternal functional status have similarities in terms of domain names, the coverage of those domains remained distinct. Nevertheless, the postpartum literature provided a basis of comparison for the focus group data. In short, there were no major contextual domains discussed in the literature that were absent from the focus group discussions. The BIMF is the beneficiary of the thorough study of functioning represented by the focus groups.
Table 1.
Overlap Among Barkin et al.'s Domains of Maternal Functioning, Logsdon et al.'s Key Components of Motherhood, and Fawcett et al.'s Five Dimensions of Functional Status
| Barkin et al. Domains of Maternal Functioning | Logsdon et al. analog | Fawcett et al. analog |
|---|---|---|
| Self-care | Self-care | |
| Infant care | Caretaking of infant, Providing healthcare for the child | Infant care |
| Mother-child interaction | Maternal-infant interaction, finding gratification in the maternal role | |
| Psychological well-being | ||
| Social support | Social and community | |
| Management | ||
| Adjustment |
Reliability and validity of BIMF
Content validity was achieved for the BIMF via the focus groups and expert critique. In order to further develop the BIMF's psychometric portfolio, the BIMF was administered to all women receiving a baseline assessment as part of the Identification and Therapy of Postpartum Depression Study (screening study) (R01 MH071825, K Wisner, PI) from October 1, 2008, to March 27, 2009. All the women had previously scored ≥10 on the Edinburgh Postnatal Depression Scale (EPDS),22 which indicated depressive symptomatology. The 6 months of data collection yielded 109 complete BIMF assessments, and the psychometric analysis was based on this sample. On average, the women in the baseline sample were 29 years old, primarily white (72.5%), and non-Hispanic (97.3%). Infants were 6.6 weeks old, on average, at the time of the baseline assessment. The mean BIMF total score for the 109 women was 81.4 (SD 17.1).
The Cronbach's alpha23 for the BIMF was 0.87, indicating a strong interitem agreement. In order to establish construct validity, it is important to observe how the BIMF relates to other relevant measures. Pearson correlation coefficients were generated to examine the BIMF's associations with the Gratification Checklist (GRAT),5,6 the 17-item Hamilton Rating Scale for Depression (HRSD-17),24 and the 12-item Short-Form Health Survey Mental Functioning Component (SF-12 Mental).25 The GRAT, HRSD-17, and SF-12 Mental Component capture gratification in the maternal role, depression, and mental functioning, respectively. As hypothesized, maternal functioning (as measured by the BIMF) was positively and significantly associated with maternal gratification (r = 0.56, p < 0.0001) and mental functioning (0.39, p < 0.0001). Also as expected, maternal functioning (BIMF) was significantly and inversely related to depression (r =−0.21, p = 0.0326). The significance, direction, and strength (or lack thereof) of the relationship between the BIMF and these variables provide evidence of construct validity.
Discussion
The BIMF is one of two instruments designed with the explicit purpose of measuring maternal functional status. Currently, the most common method of assessing postpartum health is through evaluation for depression. Although depression assessment captures mood elements, such as sadness, lack of enjoyment, and anxiety, it does not address functioning in the maternal role. Ware et al. state that, “the goal of medical care for most patients today is to obtain a more ‘effective life’ and to preserve functioning and well-being.”25 Therefore, it is important to have appropriate tools for measuring the construct.
The BIMF was developed from information garnered during three focus group discussions, one expert review panel, and the literature. The focus groups collectively consisted of 6 hours of conversation and were intended to collect and assimilate women's thoughts on functioning in new motherhood, which was defined as the 12 months after childbirth. Changes in the mother's role set since childbirth, individual conceptualizations of a “good mother,” and circumstances surrounding high-functioning and low-functioning periods were the main research topics of interest. These three focus groups were successful according to several key parameters. The major research questions were covered extensively in each of the three discussions, and there was an overwhelming willingness to disclose personal details, which may have been a reflection of the women's need to share their frustrations (and joys) with other mothers. In general, facilitators are trained to handle groups that are less forthcoming with conversation and to gently encourage participation from timid group members. These skills were rarely needed in the new mother focus groups. Often, focus group members will speak exclusively to the facilitator rather than communicating directly with the other participants. However, this is not ideal, as interactions between participants provide valuable information and are what distinguish focus groups from one-to-one interviews.18,26,27 Again, this did not apply to the new mothers, where direct communication between participants was the standard. The attendance was also excellent, with 31 of 33 enrolled women participating. The focus groups produced rich discussion that served as the basis for the 20-item BIMF.
Although qualitative data analysis was the primary source for the initial item development, the BIMF was the beneficiary of extensive expert input. Additionally, the research literature was reviewed to ensure that no major contextual domains were missing from the new instrument. The focus group work captured the major themes in the literature.
The BIMF provides an attractive alternative to the IFSAC for measuring maternal functional status. The instrument reflects the new mother's conceptualization of functioning in motherhood and is not based on a clinical construct of the concept. This unique approach of allowing new mothers to define maternal functional status is also a flexible one that allows for changes in women's roles since giving birth. It also measures personal satisfaction in the mothering role (item 20). Although the BIMF includes items that gauge social support, it does not specifically address spousal support. This was intentional, as the BIMF is meant as a measure of functioning for all women regardless of marital status. Social support can be present in a woman's life in a variety of forms, and this instrument targets the adequacy and availability of that support rather than its source.
The BIMF covers a broad range of functional areas (self-care, infant care, mother-child interaction, psychological well-being of mother, social support, management, adjustment) that emerged as a result of the discussions. This new application of maternal functional status is a robust construct where the physical and mental health of the mother is essential to optimal functioning. It is important to note that despite its breadth, the BIMF does not measure any one of the functional areas in great depth. For example, there are instruments dedicated exclusively to the measurement of infant care or mother-child interaction.
A potential limitation in the design of the maternal focus groups was their heterogeneity across race and depression status, which are factors that might influence women's postpartum experience. In general, homogeneity within a focus group promotes open discussion. Ideally, focus group planners should try to anticipate factors that could inhibit discussion. For example, HIV status (among other factors) was considered when researchers from the Portland Men's Study were constructing focus groups.19 Researchers received information from key informants in the gay male community about HIV-seropositive men. Their assertion was that these men might feel more comfortable sharing their experiences with other seropositive men. Initial plans for the maternal focus groups included a finer separation of women based on race and depression status, but these plans were thwarted by practical and ethical concerns. In general, however, this limitation did not suppress conversation in the three discussions. In fact, some of the most vocal participants were women who admitted to having postpartum depression. Additionally, although the majority of the study population comprised educated white women (72.5% white), the themes that the BIMF was based on were common across race and education level.
The BIMF was developed based on the experiences of a sample in which 26.7% of participants had high depressive symptom levels. However, the psychometric analysis was based on a population in which all women scored ≥10 on the Edinburgh Postnatal Depression Scale,22 indicating depressive symptomatology. There are limitations associated with testing in a depressed population. Certain variables, such as maternal functioning and depression, are likely to have a restricted range in a depressed population. This restriction, if present, could affect the correlation observed between functioning and depression or between functioning and other affected variables. Similar to most prevalent health assessments, which are validated in a variety of research study settings, the BIMF's psychometric properties should be retested. Although the BIMF displayed good internal consistency and construct validity, further study should include testing in a population without established depressive symptomatology.
Data collection through the Identification and Therapy of Postpartum Depression Study (screening study) allowed for an initial evaluation of the BIMF's psychometric properties. It also provided evidence that the BIMF is appropriate for use in clinical trials. Many instruments present significant patient burden and do not engage the respondent. However, the psychiatric assessors who have had the opportunity to administer the BIMF in different study settings report a high level of patient receptivity. Of the 112 BIMFs collected via self-report over 6 months, 109 were without missing data. One potential reason for this impressive completion rate is that the women related to the survey questions, a hypothesis that is consistent with the opinions of the psychiatric assessors.
Conclusions
The BIMF represents a valuable tool for assessing postpartum wellness. Evidence of internal reliability, content validity, and construct validity is provided, and the BIMF has been successfully administered in clinical trial settings. The BIMF has the potential to be particularly valuable in cases where screening for functional status, which can be more conceptually appealing and less stigmatizing than depression screening, is preferred for postpartum women. Ideally, depression and functional status should be assessed simultaneously in order to provide a more comprehensive characterization of maternal health. Additionally, the BIMF will afford researchers the means to study the relationship between postpartum maternal functioning and developmental outcomes in infants and children. Future research regarding the BIMF should include the development of a threshold that indicates poor maternal functioning. Development of such a threshold will promote clinical relevancy and will allow healthcare providers to identify patients in need of intervention.
Acknowledgments
This work was supported by an internal development fund at the University of Pittsburgh and the Identification and Therapy of Postpartum Depression Study (R01 MH071825, K. Wisner, PI).
Disclosure Statement
No competing financial interests exist.
References
- 1.Logsdon MC. Wisner KL. Pinto-Foltz MD. The impact of postpartum depression on mothering. J Obstet Gynecol Neonatal Nurs. 2006;35:652–658. doi: 10.1111/j.1552-6909.2006.00087.x. [DOI] [PubMed] [Google Scholar]
- 2.Fowles ER. Horowitz JA. Clinical assessment of mothering during infancy. J Obstet Gynecol Neonatal Nurs. 2006;35:662–670. doi: 10.1111/j.1552-6909.2006.00090.x. [DOI] [PubMed] [Google Scholar]
- 3.Barkin JL. Wisner KL. Bromberger JT. Beach SR. Wisniewski SR. Assessment of functioning in new mothers. J Womens Health. 2010;19:1493–1499. doi: 10.1089/jwh.2009.1864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gibaud-Wallston J. Wandersman LP. Development and utility of the Parenting Sense of Competence Scale. Paper presented at American Psychological Assocation Meeting; Toronto, Canada. 1978. [Google Scholar]
- 5.Mercer RT. The process of maternal role attainment over the first year. Nurs Res. 1985;34:198–204. [PubMed] [Google Scholar]
- 6.Russell CS. Transition to parenthood: Problems and gratifications. J Marriage Fam. 1974;36:294–302. [Google Scholar]
- 7.Froman RD. Owen SV. Infant care self-efficacy. Sch Inq Nurs Pract. 1989;3:199–211. [PubMed] [Google Scholar]
- 8.Leifer M. Psychological changes accompanying pregnancy and motherhood. Genet Psychol Monogr. 1977;95:55–96. [PubMed] [Google Scholar]
- 9.Pridham KF. Chang AS. Parents' beliefs about themselves as parents of a new infant: Instrument development. Res Nurs Health. 1985;8:19–29. doi: 10.1002/nur.4770080106. [DOI] [PubMed] [Google Scholar]
- 10.Walker LO. Crain H. Thompson E. Maternal role attainment and identity in the postpartum period: Stability and change. Nurs Res. 1986;35:68–71. [PubMed] [Google Scholar]
- 11.O'Hara MW. Hoffman JG. Phillips HC. Wright EJ. Adjustment in childbearing women: The Postpartum Adjustment Questionnaire. Psychological Assessment. 1992;4:160–169. [Google Scholar]
- 12.Kumar R. Robson KM. Smith AMR. Development of a self-administered questionnaire to measure maternal adjustment and maternal attitudes during pregnancy and after delivery. J Psychosom Res. 1984;28:43–51. doi: 10.1016/0022-3999(84)90039-4. [DOI] [PubMed] [Google Scholar]
- 13.Fawcett J. Tulman L. Myers ST. Development of the Inventory of Functional Status After Childbirth. J Nurse Midwifery. 1988;33:252–260. doi: 10.1016/0091-2182(88)90080-8. [DOI] [PubMed] [Google Scholar]
- 14.Aktan NM. Functional status after childbirth: A review of the literature. Clin Nurs Res. 2007;16:195–211. doi: 10.1177/1054773807303075. [DOI] [PubMed] [Google Scholar]
- 15.McVeigh C. Functional status after childbirth in an Australian sample. J Obstet Gynecol Neonatal Nurs. 1998;27:402–409. doi: 10.1111/j.1552-6909.1998.tb02664.x. [DOI] [PubMed] [Google Scholar]
- 16.Gilson BS. Gilson JS. Bergner M, et al. The Sickness Impact Profile. Development of an outcome measure of health care. Am J Public Health. 1975;65:1304–1310. doi: 10.2105/ajph.65.12.1304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Roy C. An Adaptation Model. 2nd. Englewood Cliffs, NJ: Prentice-Hall; 1984. Introduction to nursing. [Google Scholar]
- 18.Wilkinson S. Focus groups in health research. Exploring the meanings of health and illness. J Health Psychol. 1998;3:329–348. doi: 10.1177/135910539800300304. [DOI] [PubMed] [Google Scholar]
- 19.O'Brien K. Using focus groups to develop health surveys: An example from research on social relationships and AIDS-preventive behavior. Health Educ Q. 1993;20:361–372. doi: 10.1177/109019819302000307. [DOI] [PubMed] [Google Scholar]
- 20.Fayers P. Hays R. Assessing quality of life in clinical trials. 2nd. Oxford, England: Oxford University Press; 2005. [Google Scholar]
- 21.Radloff LS. Center for Epidemiological Studies-Depression Scale. Appl Psychol Meas. 1997;1:38. [Google Scholar]
- 22.Cox JL. Holden JM. Sagovsky R. Detection of postnatal depression. Development of the 10-item Edinburgh Postnatal Depression Scale. Br J Psychiatry. 1987;150:782–786. doi: 10.1192/bjp.150.6.782. [DOI] [PubMed] [Google Scholar]
- 23.Cronbach LJ. Coefficient alpha and the internal structure of tests. Psychometrika. 1951;16:297–334. [Google Scholar]
- 24.Hamilton M. A rating scale for depression. J Neurol Neurosurg Psychiatry. 1960;23:56–62. doi: 10.1136/jnnp.23.1.56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ware JE., Jr Kosinski M. Keller SD. A 12-item Short-Form Health Survey: Construction of scales and preliminary test of reliability and validity. Med Care. 1996;34:220–233. doi: 10.1097/00005650-199603000-00003. [DOI] [PubMed] [Google Scholar]
- 26.Kitzinger J. The methodology of focus groups: The importance of interaction between research participants. Sociol Health Illness. 1994;16:103–121. [Google Scholar]
- 27.Morgan D. Sage University Papers, Qualitative Research Methods Series No. 16. London: Sage; 1988. Focus groups as qualitative research. [Google Scholar]