Abstract
The high molecular weight melanoma-associated antigen (HMW-MAA), also known as melanoma chondroitin sulfate proteoglycan, has been used as a target for the immunotherapy of melanoma. This antigen is expressed on the cell surface and has a restricted distribution in normal tissues. Besides its expression in a broad range of transformed cells, this antigen is also found in pericytes, which are important for tumor angiogenesis. We generated a recombinant Listeria monocytogenes (Lm-LLO-HMW-MAA-C) that expresses and secretes a fragment of HMW-MAA (residues 2,160–2,258) fused to the first 441 residues of the listeriolysin O (LLO) protein. Immunization with Lm-LLO-HMW-MAA-C was able to impede the tumor growth of early established B16F10-HMW-MAA tumors in mice and both CD4+ and CD8+ T cells were required for therapeutic efficacy. Immune responses to a known HLA-A2 epitope present in the HMW-MAA2160–2258 fragment was detected in the HLA-A2/Kb transgenic mice immunized with Lm-LLO-HMW-MAA-C. Surprisingly, this vaccine also significantly impaired the in vivo growth of other tumorigenic cell lines, such as melanoma, renal carcinoma, and breast tumors, which were not engineered to express HMW-MAA. One hypothesis is that the vaccine could be targeting pericytes, which are important for tumor angiogenesis. In a breast tumor model, immunization with Lm-LLO-HMW-MAA-C caused CD8+ T-cell infiltration in the tumor stroma and a significant decrease in the number of pericytes in the tumor blood vessels. In conclusion, a Lm-based vaccine against HMW-MAA can trigger cell-mediated immune responses to this antigen that can target not only tumor cells but also pericytes in the tumor vasculature.
Introduction
The human high molecular weight-melanoma associated antigen (HMW-MAA) is a membrane-bound protein of 2322 residues, also known as melanoma chondroitin sulfate proteoglycan, which is overexpressed on over 90% of the surgically removed benign nevi and melanoma lesions (1). Besides tumors of melanocytic origin, HMW-MAA has also been found to be expressed by basal cell carcinoma, tumors of neural crest origin (astrocytomas, gliomas, neuroblastomas and sarcomas), some forms of childhood leukemias and lobular breast carcinoma lesions. In vitro experimental data shows that HMW-MAA is involved in the adhesion, spreading and migration of melanoma cells and may have a role in cell invasion and metastasis (1, 2). Nevertheless, HMW-MAA has a restricted expression in normal tissues, although it is expressed at high levels on both activated pericytes and pericytes in tumor angiogenic vasculature, which are associated with neovascularization in vivo (3, 4). A murine homolog of HMW-MAA, known as AN2, has 80% homology to HMW-MAA, besides a similar expression pattern and function (5).
Because of its cell surface localization, immunotherapies for this antigen have focused on inducing a humoral response against HMW-MAA. In a phase I/II clinical trial, the development of anti-HMW-MAA humoral response elicited by active immunization was associated with prolonged survival of patients with melanoma (6). In contrast, despite the well-established role of cell-mediated immune responses in tumor immunotherapy, limited information is available about the generation of T cell immunity against HMW-MAA. Recently, Peng et al. showed that antigen-specific CTLs against HMW-MAA can be generated in mice in a CD4-dependent manner (7). Nevertheless, the role of cell-mediated immune responses against HMW-MAA in impacting the in vivo growth of tumorigenic cells has not yet been investigated.
Listeria monocytogenes (Lm) is a gram-positive facultative intracellular bacterium that has been extensively used as a vaccine vector for several diseases. Mouse models have shown that recombinant Lm expressing tumor-associated antigens is a potential therapeutic approach able to eradicate established malignant tumors (8–11). Lm is able to infect phagocytic and antigen-presenting cells (APC), such as macrophages and dendritic cells, where it can access the cytosolic compartment after lysing the phagolysosome membrane (12). In the cytosol, the bacterium replicates and spreads to neighboring cells (12). This unusual intracellular life cycle allows antigens secreted by Lm to be processed and presented in the context of both MHC I and II molecules, resulting in strong CD8+ and CD4+ T cell-mediated immune responses (13). The listeriolysin-O (LLO) protein is the major virulence factor of Lm responsible for the lysis of the phagolysosome. LLO, which is highly immunogenic (14), induces maturation of antigen-specific T cells into Th1 cells (15) and interferon-gamma secretion by T cells (16, 17). Our group has previously shown that genetically fusing an antigen to a non-hemolytic form of LLO enhances the immunogenicity of tumor-associated antigens, as compared to the antigen expressed alone in the same system, resulting in a better therapeutic efficacy against established tumors (9, 10, 18, 19).
Here, we describe the therapeutic and immunological properties of a recombinant Lm- based vaccine (Lm-LLO-HMW-MAA-C) that secretes a fragment of the HMW-MAA fused to LLO. We demonstrate that this vaccine is able to eradicate established B16F10 tumors engineered to express HMW-MAA. This therapeutic effect is dependent on both CD4+ and CD8+ T cells. Further, using the HLA-A2/Kb transgenic mouse, we detected HMW-MAA-specific responses induced by the vaccine against an epitope previously shown to be restricted to the HLA-A2 molecule (7). Interestingly, we show that this vaccine can also significantly delay the growth of tumors that do not express the HMW-MAA antigen or its homolog AN2. This impact on tumor growth is associated with infiltration of the tumor stroma by CD8+ T cells and a significant reduction in the pericyte coverage in the tumor vasculature.
Material and methods
Mice
Female C57BL/6, BALB/c and FVB/N mice were purchased from Charles River Laboratories. A breeder pair of HLA-A2/Kb was generously provided by Dr. L. Sherman (The Scripps Research Institute, La Jolla, CA). These mice were maintained and bred in the animal core facility at the University of Pennsylvania. The FVB/N HER-2/neu transgenic mice (20) were housed and bred at the Veterans’ Administration Hospital afiliated with the University of Pennsylvania. Mice were six to eight weeks-old when used at the start of the experiments, which were done in accordance with regulations by the Institutional Animal Care and Use Committee of the University of Pennsylvania.
Antibodies
The anti-HMW-MAA mAb VT80.12 has been previously described (21). Goat anti-mouse IgG-PE, anti-CD8b.2-FITC, anti-IFN-γ-PE, anti-mouse CD31-FITC, anti-mouse CD8α-PE, rat IgG2a and rat IgG2b isotype controls were purchased from BD Biosciences. Anti-α-Smooth Muscle (αSMA)-Cy3 and anti-FLAG M2 monoclonal antibodies were purchased from Sigma. Secondary anti-rabbit Alexa Fluor 488 was purchased from Invitrogen and anti-rat NG2 from Chemicon. The anti-CD4 mAb GK1.5, anti-CD8 mAb 2.43 and anti-CD25 mAb PC61 were purified using protein G sepharose columns (Amersham Biosciences).
Flow cytometry
Cells were harvested, washed in FACS buffer (PBS-2% FBS) and Fc receptors blocked with 2.4G2 hybridoma supernatant. After washing, cells were resuspended in 50 µl of FACS buffer containing the appropriate antibodies and incubated at 4°C in the dark for 30 minutes. Cells were washed twice and when necessary incubated with a secondary antibody. Otherwise, cells were fixed in 2% formaldehyde and analyzed using a FACS Calibur cytometer and CellQuest Pro software (BD Biosciences).
Cell lines
Cell culture media and supplements were purchased from Gibco (Invitrogen). B16F10 cells were maintained in DMEM and RENCA and J774 cells in RPMI 1640. Media was supplemented with 10% FBS, 10 mM HEPES buffer, 2 mM Lglutamine, 0.1 mM non-essential amino acids, 1 mM sodium pyruvate and 50 µg/ml of gentamicin. The NT-2 cell line was maintained in RPMI 1640 supplemented with 20% FBS, 10 mM HEPES buffer, 2 mM L-glutamine, 0.1 mM non-essential amino acids, 1 mM sodium pyruvate, 20 µg/ml of insulin, 100 U/ml of penicillin and 100 µg/ml of streptomycin. All cell cultures were kept at 37°C and 5% CO2. B16F10 cells were transfected with a pcDNA3.1+ plasmid containing the full-length HMW-MAA cDNA sequence (7), using lipofectamine 2000 (Invitrogen), as recommended by the manufacturer. Stable transfected cells were maintained in medium supplemented with 1 mg/ml of G418 and single clones were isolated using limiting dilution. Individual clones were screened for HMW-MAA expression by flow cytometry using the monoclonal antibody VT80.12.
Construction of Lm-LLO-HMW-MAA-C vaccine
A fragment corresponding to HMW-MAA residues 2160 to 2258 was amplified by PCR using the primers 5’-TGCTCGAGGCCACTGAGCCTTACAATGCTGCC-3’ (forward primer, XhoI site underlined) and 5’-CCCGGG TTA CTACTTATCGTCGTCATCCTTGTAATCCTGGACGTCATGCTTGCCCG-3’ (reverse primer, XmaI site underlined, stop codon in bold and Flag sequence in italics). The PCR product was ligated into pCR2.1-TOPO plasmid (Invitrogen), confirmed by sequencing and subsequently excised by double digestion with XhoI and XmaI (New England Biolabs). The fragment was ligated into a pGG55-based plasmid downstream and fused to a gene encoding for the first 441 residues of the LLO protein, whose expression is driven by the hly promoter. The construction of the pGG55 has been described in details elsewhere (9). The resultant plasmid was electroporated into the PrfA-defective Lm strain XFL-7 (kindly provided by Hao Shen, University of Pennsylvania, Philadelphia, PA), which is derived from the Lm strain 10403S. Positive clones were selected on Brain Heart Infusion (BHI, Difco) plates supplemented with 34µg/ml of chloramphenicol and 250µg/ml of streptomycin. The resultant strain was named Lm-LLO-HMW-MAA-C, which was subsequently passaged twice in vivo as previously described (22).
Effect of Lm-LLO-HMW-MAA-C on tumor growth
Mice were given s.c. 2 × 105 of B16F10-HMW-MAA, B16F10 or RENCA tumor cells on the flank in 0.2 ml of PBS. On day 3 after tumor inoculation, mice were immunized i.p. with 2.5 × 107 CFU of Lm- LLO-HMW-MAA-C. This dose was determined as one-tenth of the minimum dose observed to have adverse effects on mice and it was used in all experiments. In the NT-2 model, mice were given 1 × 106 tumor cells and immunized 7 days later with Lm-LLO-HMW-MAA-C. The FVB/N HER-2/neu transgenic mice received the first dose of vaccine when x-weeks old. Immunizations were repeated weekly totalizing 3 doses of the vaccine in all experiments. In the control groups, mice received either PBS or an equivalent dose of an irrelevant Lm vaccine (Lm-LLO-E7 or Lm-LLO-NY-ESO-1101–156). Tumors were measured every 2–3 days with calipers and the shortest and longest surface diameters were recorded for each individual tumor. Mice were sacrificed when they developed open wounds or tumors reached 20 mm in diameter. Tumor-free surviving mice challenged with B16F10-HMW-MAA were rechallenged in the opposite flank with the same cell line 7-weeks after the first inoculation.
In vivo cell depletions
For CD4 and CD8 in vivo depletions, 500µg of GK1.5 and 2.43 antibodies, respectively, were given i.p. on days 1, 2, 6 and 9. The control groups received either an anti-β-galactosidase antibody or were left untreated. For CD25 depletion, 500µg of PC61 was given i.p. on days 0 and 2. These antibodies were tested and confirmed to induce depletion of the target cells by flow cytometry (data not shown).
Transfer of anti-tumor immunity (Winn assay)
C57BL/6 mice were injected twice at a one-week interval with Lm-HMW-MAA-C. Control mice were left untreated. One-week after the last immunization, mice were sacrificed and the spleens harvested. CD8+ T cells were enriched from the splenocyte suspension by negative magnetic selection (Dynal® Mouse CD8 Cell Negative Isolation Kit, Invitrogen) and comprised 85% of the total cells as assessed by flow-cytometry. CD8+ T cells either from naïve or Lm-HMW-MAA-C immunized mice were mixed in PBS with B16F10-HMW-MAA at a ratio of 10:1 and 0.2 ml of the cell suspension, containing 2 × 105 tumor cells and 2 × 106 CD8+ T cells, was inoculated s.c. on the flank of naïve mice. Tumors were measured every 2 days with a caliper and the size recorded as the mean tumor diameter.
Synthetic peptide
The HLA-A2-binding synthetic peptide LILPLLFYL, which corresponds to HMW-MAA residues 2238 to 2246, was purchased from EZBiolab.
Murine IFN-γ assays to detect antigen-specific CD8+ T-cells
Spleens from immunized mice were harvested one-week after last immunization. After lysing red blood cells, splenocytes were stimulated with 1 µM of the HMW-MAA2238–2246 peptide and IFN-γ production detected by either ELISpot or intracellular cytokine staining. ELISpots were performed according to the manufacturer instructions (Mabtech) and spot forming cells (SFC) counted using a dissecting microscope. Intracellular cytokine staining for IFN-γ was done as previously described (22). Data was collected using a FACS Calibur cytometer and analyzed using CellQuest Pro software. Cells were gated on CD8high and analyzed for intracellular IFN-γ.
Immunofluorescence
On day 84 post tumor inoculation, mice were sacrificed and the NT-2 tumors were surgically excised, cryopreserved in OCT freezing medium and cryosectioned for 8–10um thick sections. For immunofluorescence, samples were thawed and fixed using 4% formalin. After blocking (2.4G2 conditioned medium / 10% FBS / 5% normal rat serum and normal mouse serum), sections were stained with primary antibodies in blocking solution in a humidified chamber at 37°C for 1 hour. Samples were stained with secondary antibody following the same procedure as for primary staining. DAPI (Invitrogen) staining was performed according to manufacturer instructions. Intracellular stains (αSMA) were done in PBS / 0.1% tween / 1% BSA solution. Slides were coversliped using Biomeda mounting solution (Biomeda) with anti-fading agents, set for 24 hours and kept at 4°C until imaging using Spot Image Software (2006) and BX51 series Olympus fluorescent microscope. Images were merged using Spot Image Software and quantitation was performed after an ROI was gated using Image Pro Software (2006). All images are a merged series of three different channels captured for same exposure time.
Evaluation of possible toxicity associated with inhibition of angiogenesis
Six to eight weeks old FVB/N female mice were immunized three consecutive times weekly with either a control Lm vaccine or Lm-LLO-HMW-MAA-C. On the fourth week safety studies were conducted. For pregnancy and fertility, 5 mice per group were allowed to mate with individual housed males. Coitus was monitored and confirmed by the presence of a vaginal plug. Time to gestation, pup birth weight and total litter size were measured. The wound healing assay utilized in this study was done according to previously described methods used in antiangiogenesis studies (23). Briefly, mice were anesthetized, hair removed and skin-cleaned with an aseptic wipe. Two circular 3mm in diameter wounds were punched from the skin using a sterile skin biopsy tool (Acuderm). Wounds were not treated and no infection was observed. Average time to wound closure was monitored and considered complete when a scar was formed without any visible scab left.
Statistical analysis
Data were analyzed using either the non-parametric Mann-Whitney test or the parametric t test when appropriated. The log-rank test was used for survival data. All statistical analyses were done with the SPSS15.0 software. Statistical significance was based on a value of P ≤ 0.05.
Results
Construction and design of HMW-MAA expressing Lm vaccines
We designed three Lm-based vaccines expressing distinct HMW-MAA fragments based on the position of previously mapped (7) and predicted HLA-A2 epitopes. The fragment A comprised HMW-MAA residues 360 to 554, fragment B residues 701 to 1130 and fragment C residues 2160 to 2258 (Supplementary Fig. S1A). These vaccines were constructed similarly and although fragments A and B were expressed and secreted by Lm (Supplementary Fig. S1B), they had a much lower therapeutic efficacy in mouse models than the Lm-LLO-HMW-MAA-C vaccine. Since the fragments were chosen for the presence of HLA-A2 epitopes, it is possible that the reduced potency of these vaccines is because fragments A and B lack H-2b epitopes. For this reason, only the results obtained with Lm-LLO-HMW-MAA-C are shown and discussed here.
The Lm-LLO-HMW-MMA-C vaccine vector is based on the avirulent Lm XFL-7 strain, which lacks the transcriptional factor PrfA and is derived from the 10403S strain. The Lm XFL-7 was transformed with a plasmid constructed for the expression and secretion of the HMW-MAA2160–2258 fragment fused to the first 441 residues of LLO. This plasmid also contains a copy of the prfA gene that partially restores the virulence of the XFL-7 strain and is necessary for plasmid retention in vivo. To test whether the LLO-HMW-MAA2160–2258 fusion protein was produced and secreted by Lm-LLO-HMW-MAA-C, we analyzed proteins from culture supernatants by Western-Blot. A ~62 KDa band corresponding to the LLO-HMW-MAA2160–2258 fusion protein was detected using a polyclonal anti-LLO antibody (Supplementary Fig. S1B). The secretion of LLO-HMW-MAA2160–2258 was relatively weak likely due to the high hydrophobicity of this fragment, which corresponds to the HMW-MAA transmembrane domain. Despite the expression of the LLO-HMW-MAA2160–2258 fusion protein, Lm-LLO-HMW-MAA-C retained its growth capacity in BHI broth (data not shown) and also intracellularly upon infection of J774 cells, suggesting that this vector retains the ability to escape the vacuole and invade the cytosol of host cells (Supplementary Fig. S1C).
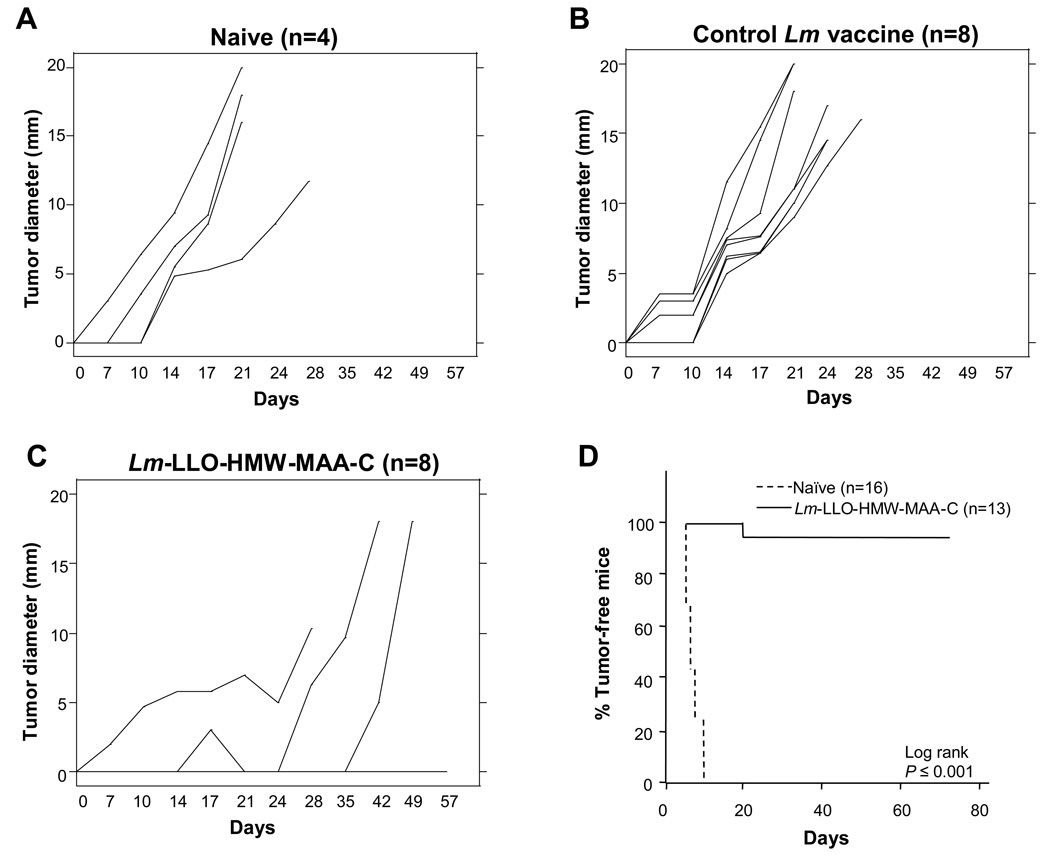
Therapeutic efficacy of Lm-LLO-HMW-MAA-C in a tumor model expressing HMW-MAA
The B16F10 melanoma was chosen as a mouse tumor model to test the therapeutic efficacy of the Lm-LLO-HMW-MAA-C vaccine because HMW-MAA is expressed in a high proportion of melanoma lesions in humans. The B16F10 cell line, which does not express the mouse HMW-MAA homolog AN2, was transfected with the full-length HMW-MAA gene. A stable clone expressing HMW-MAA was selected (Supplementary Fig. S1D), whose in vivo growth characteristics were similar to the parental B16F10 cell line (Supplementary Fig. S2). To verify the impact of Lm-LLO-HMW-MAA-C vaccination on tumor growth, mice were inoculated with B16F10-HMW-MAA cells and immunized 3 days later with the Lm-LLO-HMW-MAA-C vaccine. In the control groups, mice were immunized with either an irrelevant Lm or left untreated and no significant difference in the growth of B16F10-HMW-MAA was observed between these groups (Fig. 1A and B). On the other hand, in the group immunized with the Lm-LLO-HMW-MAA-C vaccine, 5 out of 8 mice (62.5%) were tumor-free on day 56 after tumor challenge (Fig. 1C). This difference was highly significant when compared to the Lm control group (P ≤ 0.05). This finding was reproducible and early treatment with Lm-LLO-HMW-MAA-C led to tumor regression in 37.5% to 62.5% of mice in three independent experiments. Importantly, no mice given the parental B16F10 cell line remained tumor-free upon immunization with Lm-LLO-HMW-MAA-C, suggesting that the vaccine is specifically targeting the HMW-MAA protein. However, as discussed below, Lm-LLO-HMW-MAA-C vaccination did slow down the growth of the parental B16F10 tumor (Fig. 4A).
Figure 1.
Vaccination with Lm-HMW-MAA-C induces regression of B16F10-HMW-MAA tumors and confers long-term protection. In this experiment, 20 C57BL/6 mice were inoculated s.c. with B16F10-HMW-MAA cells on the left flank. Mice were left untreated (n=4) (A) or immunized i.p. with either a control Lm vaccine (n=8) (B) or Lm-HMW-MAA-C (n=8) (C) on days 3, 10 and 17. Tumor sizes were measured for each individual tumor and the values expressed as the mean diameter in millimeters. Each line in A, B and C represents an individual mouse. D, mice treated with Lm-HMW-MAA-C that rejected the B16F10-HMW-MAA were challenged a second time with the same cell line 7 weeks after the first challenge. Data were pooled from independent experiments and the proportion of mice that remained tumor-free after the second challenge is plotted against time expressed in days of follow-up.
Figure 4.
Vaccination of mice with Lm-HMW-MAA-C impairs the growth of HMW-MAA/AN2-negative tumors. A, C57Bl/6 mice were inoculated s.c. with B16F10 cells and either immunized i.p. on days 3, 10 and 17 with Lm-HMW-MAA-C (n=8) or left untreated (n=7).B, BALB/c mice were inoculated s.c. with RENCA cells and immunized i.p. on days 3, 10 and 17 with either Lm-HMW-MAA-C (n=8) or an equivalent dose of a control Lm vaccine. C, FVB/N mice were inoculated s.c. with NT-2 tumor cells and immunized i.p. on days 7, 14 and 21 with either Lm-HMW-MAA-C (n=5) or an equivalent dose of a control Lm vaccine (n=8). Tumor sizes were measured for each individual tumor and the values expressed as the mean diameter in millimeters ± SEM. *, P ≤ 0.05, Mann-Whitney test. D, 8-week old FVB/N HER-2/neu transgenic mice were immunized i.p. followed by two additional doses at one week intervals with either Lm-HMW-MAA-C (n=20) or an equivalent dose of a control Lm vaccine (n=14).
We also tested the long-term immunity to HMW-MAA by giving a second lethal dose of the B16F10-HMW-MAA tumor cell line to those mice that remained tumor-free 7 to 8 weeks after the first challenge. Whereas all the naïve mice developed palpable tumors within the first 10 days after injection, more than 90% of the mice in the group treated with Lm-LLO-HMW-MAA-C rejected this tumor cell line after the second challenge (P ≤ 0.05) (Fig. 1D).
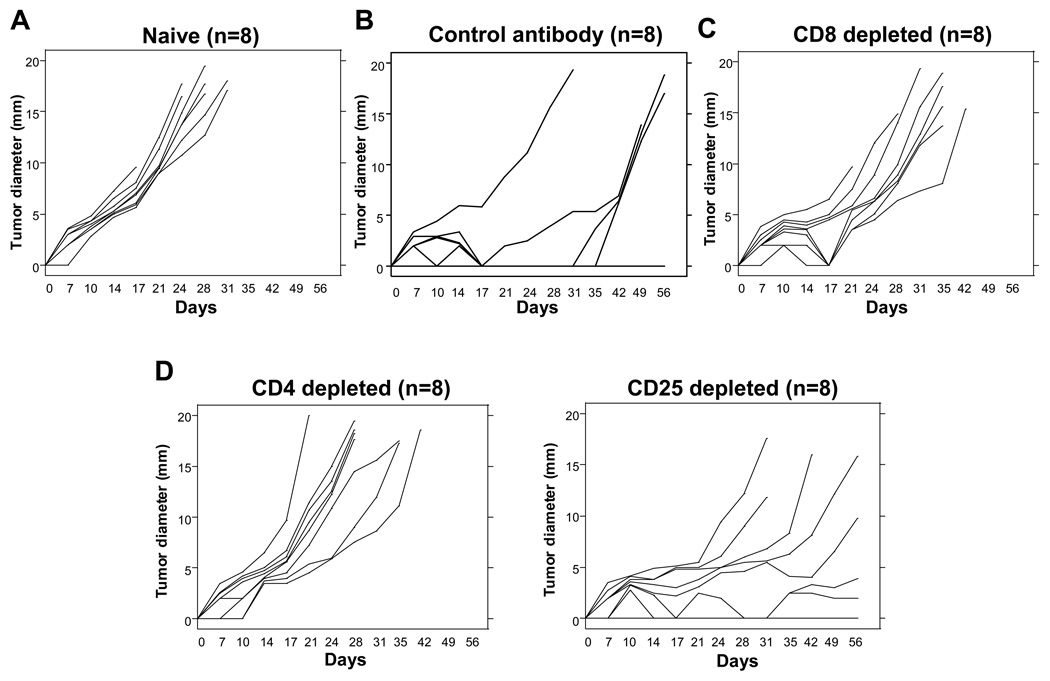
Depletion of either CD8+ or CD4+ cells abrogates the effect of Lm-LLO-HMW-MAA-C on tumor growth
To evaluate the role of different cell types in the efficacy of Lm-LLO-HMW-MAA-C, we depleted in vivo CD8+, CD4+ and CD25+ cells by antibody administration before and during the treatment course. In the non-immunized control group, all mice developed tumors (Fig. 2A), whereas 50% of the mice immunized with Lm-LLO-HMW-MAA-C and given a control antibody remained tumor-free for at least 56 days after tumor-challenge (Fig. 2B). On the other hand, none of the mice receiving either the anti-CD8 or anti-CD4 antibodies could control the tumor growth, showing that both cells types play an important role in the anti-tumor immunity generated by the Lm-LLO-HMW-MAA-C vaccine (Fig. 2C and D). However, administration of the anti-CD25 antibody did not improve the efficacy of the Lm-LLO-HMW-MAA-C vaccine, suggesting that the subset of CD4+CD25+ T regulatory cells does not have a significant influence in this model (Fig 2D).
Figure 2.
In vivo depletion of either CD4+ or CD8+ cells abrogates the efficacy of Lm-HMW-MAA-C vaccine. In this experiment, 40 C57BL/6 mice were inoculated s.c. with B16F10-HMW-MAA cells on the left flank and either left untreated (n=8) (A) or immunized i.p. with Lm-HMW-MAA-C (n=32) on days 3, 10 and 17 (B, C and D). For CD8, CD4 and CD25 in vivo cell depletions, mice were treated with 2.43 (anti-CD8) (C), GK1.5 (anti-CD4) (D, left) or PC61 (anti-CD25) (D, right) antibodies. An anti-β-galactosidase antibody was given to mice in the control group (B). Tumor sizes were measured for each individual tumor and the values expressed as the mean diameter in millimeters. Each line in A, B, C and D represents an individual mouse.
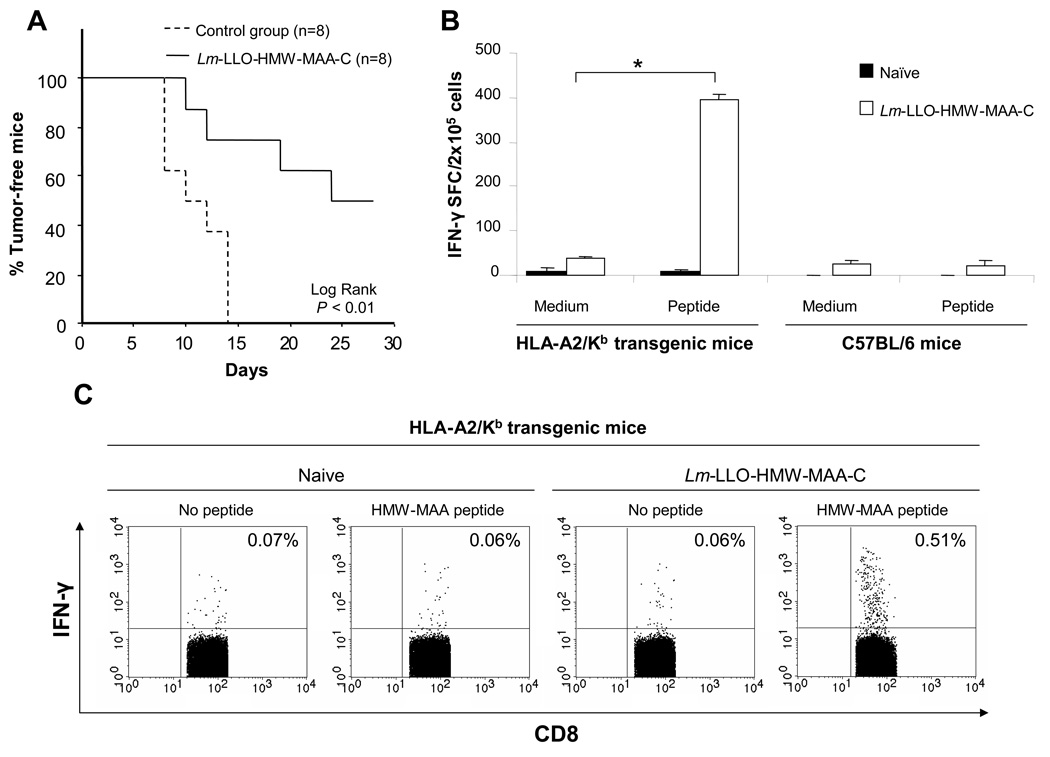
Transfer of CD8+ T cells from Lm-LLO-HMW-MAA-C immunized mice confers anti-tumor immunity against B16F10-HMW-MAA tumor cells
Lm vectors are recognized for their ability to generated strong CD8+ T cell responses, which are important for tumor rejection. To verify if the CD8+ T cells generated upon immunization with Lm-LLO-HMW-MAA-C had anti-tumor activity against the B16F10-HMW-MAA cell line, we inoculated tumor cells mixed with CD8+ T cells from either immunized or non-immunized mice and followed the tumor growth for four weeks. When mixed with CD8+ T cells from mice immunized with Lm-LLO-HMW-MAA-C, 50% of the naïve animals did not develop tumors in four weeks, as compared to none in the control group (P ≤ 0.05) (Fig. 3A). This result indicates that vaccination with Lm-LLO-HMW-MAA-C induces CD8+ T cells able to inhibit the in vivo growth of the B16F10-HMW-MAA cell line.
Figure 3.
Immunization with Lm-HMW-MAA-C induces effector CD8+ T cells in C57Bl/6 and HLA-A2/Kb transgenic mice. A, CD8+ T cells from C57Bl/6 mice vaccinated with Lm-HMW-MAA-C inhibit the growth of B16F10-HMW-MAA tumors in vivo. CD8+ T cells were purified from the spleen of either naïve or Lm-HMW-MAA-C immunized mice and mixed to B16F10-HMW-MAA tumor cells at a 10:1 effector to target ratio. The mixed cells were injected subcutaneously in mice (8 per group), which were followed-up for 28 days and examined every 2 days for tumor growth. B, vaccination of HLA-A2/Kb transgenic mice with Lm-HMW-MAA-C induces a CD8+ immune response against the HLA-A2-restricted HMW-MAA2238–2246 epitope. C57BL/6 and HLA-A2/Kb transgenic mice were either immunized twice at one-week interval with Lm-LLO-HMW-MAA-C or left untreated. One-week later the spleens were harvested and analyzed for IFN-γ secretion upon stimulation with the HMW-MAA2238–2246 peptide (LILPLLFYL). Values are expressed as spot-forming cells (SFC) ± SEM. C, HLA-A2/Kb transgenic mice were immunized once with Lm-HMW-MAA-C. Spleens were harvested 9 days later and IFN-γ production by CD8+ T cells was analyzed upon stimulation with the HMW-MAA2238–2246 peptide for 5 hours in the presence of monensin. Cells were gated on CD8high and analyzed for intracellular IFN-γ. *, P ≤ 0.05, Mann-Whitney test.
Immunization with Lm-LLO-HMW-MAA-C induces CD8+ T cells specific for HMW-MAA in HLA-A2/Kb mice
The HMW-MAA fragment expressed and secreted by the Lm-LLO-HMW-MAA-C vaccine contains the HLA-A2-restricted epitope2238LILPLLFYL2246 (7). To test whether immunization with Lm-LLO-HMW-MAA-C was able to induce immune responses against this epitope, we vaccinated either HLA-A2/Kb transgenic mice or C57BL/6 mice with Lm-LLO-HMW-MAA-C and analyzed the production of IFN-γ by ELISpot after stimulation with HMW-MAA2238–2246 peptide. Following two immunizations, a significantly higher number of SFC was detected in splenocytes from the HLA-A2/Kb transgenic mice, but not in the C57BL/6 mice (Fig. 3B). Similar results were obtained using intracellular staining for IFN-γ. After one immunization with Lm-LLO-HMW-MAA-C, IFN-γ production was detected in 0.51% of the CD8+ T cells from the HLA-A2/Kb transgenic mice stimulated with the HMW-MAA2238–2246 peptide, compared to 0.06% in the absence of the peptide (Fig. 3C). No responses could be detected in non-transgenic C57Bl/6 mice (data not shown). These results show that immunization with the Lm-LLO-HMW-MAA-C vaccine can induce CD8+ T cell responses against a HMW-MAA epitope restricted to the HLA-A2 molecule.
Effect of Lm-LLO-HMW-MAA-C immunization on the growth of tumors not engineered to express HMW-MAA
Interestingly, we also observed that immunization of mice with Lm-LLO-HMW-MAA-C could impact the growth of several different tumors that were not engineered to express HMW-MAA, such as the parental B16F10, RENCA and NT-2 tumors, which were derived from distinct mouse strains. In the RENCA, which is a spontaneous renal carcinoma cell line derived from the BALB/c mouse, and B16F10 models, mice were immunized weekly with Lm-LLO-HMW-MAA-C three times, starting 3 days after tumor challenge. Immunization with Lm-LLO-HMW-MAA-C significantly delayed the growth of these tumors (Fig. 4A and B). In the NT-2 tumor model, which is a mammary carcinoma cell line expressing the rat HER-2/neu protein and is derived from the FVB/N HER-2/neu transgenic mice (24), immunization with Lm-LLO-HMW-MAA-C 7 days after tumor inoculation not only impaired tumor growth but also induced regression of the tumor in 1 out of 5 mice (Fig. 4C). Furthermore, these results could not be attributed to a non-specific Lm effect since a control Lm vaccine strain did not impact on the growth of B16F10 (Supplementary Fig. S3), RENCA (Fig. 4B) or NT-2 tumors (Fig. 4C). We also evaluated the effect of Lm-LLO-HMW-MAA-C immunization in a spontaneous tumor model using the FVB/N HER-2/neu transgenic mouse. These mice express the rat HER-2/neu proto-oncogene under the control of the mouse mammary tumor virus (MMTV) promoter (20). In this transgenic mouse strain, over 90% of the females develop focal mammary tumors after a latency of about 4–6 months. Immunization with Lm-LLO-HMW-MAA-C significantly delayed the median time for the onset of mammary tumors in these mice (39 weeks), as compared to a control Lm vaccine (25 weeks) (Figure 4D).
Immunization of mice with the Lm-HMW-MAA-C vaccine induces infiltration of the tumor by CD8+ T lymphocytes and decreases the number of pericyte-positive tumor vessels
Although NT-2 cells do not express the HMW-MAA homolog AN2, immunization of FVB/N mice with Lm-LLO-HMW-MAA-C significantly impaired the growth of NT-2 tumors and eventually led to tumor regression (Fig. 4C). One hypothesis is that activated pericytes present in tumor blood vessels, which express the AN2/HMW-MAA marker, could be a potential target for HMW-MAA vaccines. Because the more pronounced effect of Lm-LLO-HMW-MAA-C vaccination in NT-2 tumors, we used this tumor model to evaluate CD8+ T cells and pericytes in the tumor site by immunofluorescence. Staining of NT-2 tumor sections for CD8 showed infiltration of CD8+ T cells into the tumors and around blood vessels in mice immunized with the Lm-LLO-HMW-MAA-C vaccine, but not in mice immunized with the control vaccine (Fig. 5A). We also analyzed pericytes in NT-2 tumors by double staining with αSMA and NG2 antibodies. The NG2 protein is the rat homolog of HMW-MAA and the NG2 antibody used in this study has been shown to cross-react with the mouse homolog AN2. Data analysis from 3 independent NT-2 tumors showed a significant decrease in the number of pericytes in mice immunized with Lm-LLO-HMW-MAA-C, as compared to control (P ≤ 0.05) (Fig. 5B). Similar results were obtained when the analysis was restricted to cells stained for αSMA, which is not targeted by the vaccine (data not shown). This finding is in agreement with the hypothesis that Lm-LLO-HMW-MAA-C vaccination might potentially impact blood vessel formation in the tumor site by targeting pericytes.
Figure 5.
Immunization with Lm-HMW-MAA-C promotes tumor infiltration by CD8+ cells and decreases the number of pericytes in blood vessels. A, NT-2 tumors were removed and sectioned for immunofluorescence. Staining groups are numbered (1–3) and each stain is indicated on the left. Sequential tissues were either stained with the pan-vessel marker anti-CD31 or the anti-NG2 antibody for the HMW-MAA mouse homolog AN2, in conjuction with anti-CD8α for possible TILs. Group 3 shows isotype controls for the above antibodies and DAPI staining used as a nuclear marker. A total of 5 tumors were analyzed and a single representative image from each group is shown. CD8+ cells around blood vessels are indicated by arrows. B, sequential sections were stained for pericytes by using the anti-NG2 and anti-alpha-smooth-muscle-cell-actin (αSMA) antibodies. Double staining/colocalization of these two antibodies (yellow in merge image) are indicative of pericyte staining (top). Pericyte colocalization was quantitated using Image Pro Software and the number of colocalized objects is shown in the graph (bottom). A total of 3 tumors were analyzed and a single representative image from each group is shown. *, P ≤ 0.05, Mann-Whitney test. Graph shows mean ± SEM.
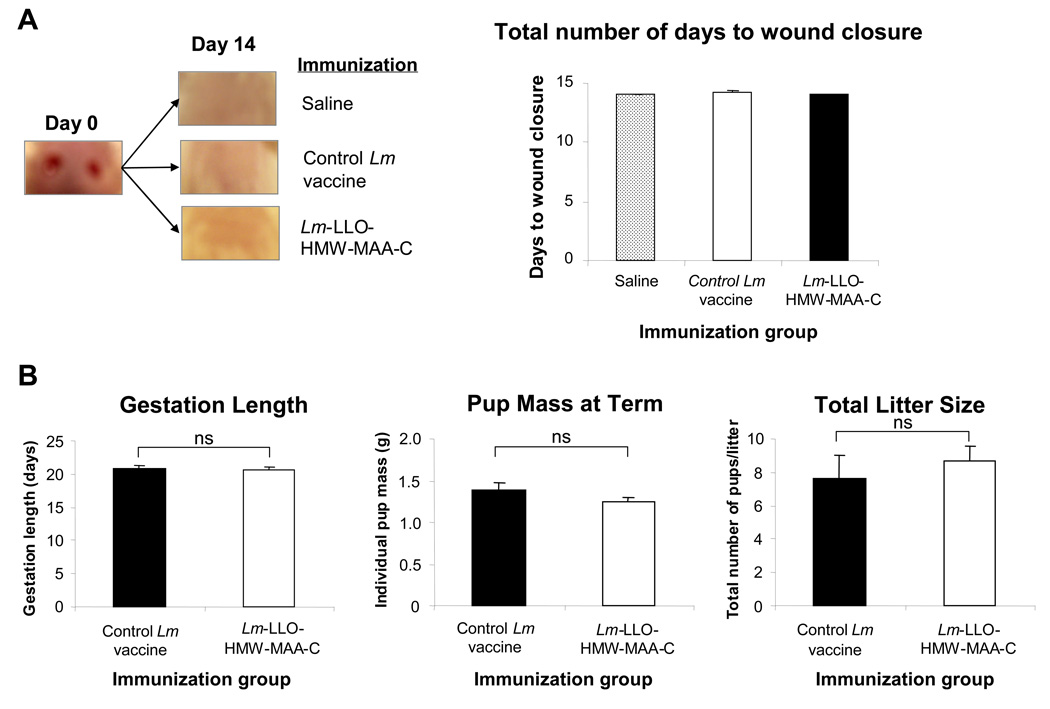
Immunization with HMW-MAA-C has no impact on wound healing, pregnancy and fertility in mice
To evaluate whether Lm-LLO-HMW-MAA-C causes toxicity that is associated with angiogenesis inhibition, we studied wound healing, pregnancy and fertility in immunized mice. No significant difference was observed in the time required for wound closure in mice immunized with Lm-LLO-HMW-MAA-C as compared to a control Lm vaccine or saline injection (Fig. 6A). Similarly, Lm-LLO-HMW-MAA-C immunization had no impact on fertility, gestation length and pup mass at birth (Fig. 6B).
Figure 6.
Lm-LLO-HMW-MAA-C vaccine does not reduce wound healing ability of immunized mice nor affect pregnancy or fertility. A, FVB/N female 8 week old, age-matched mice were immunized three times, one week apart with a control Lm vaccine or Lm-LLO-HMW-MAA-C or saline alone. On the fourth week mice were shaved and 3mm punctures through the skin were done on the upper back of anesthetized mice. A total of 5 mice were tested per group and a representative mouse from each group is shown on day 0 and 14 days later. B, FVB/N female mice were immunized three times, one week apart with either a control Lm vaccine (n=4) or Lm-LLO-HMW-MAA-C (n=3) and then mated with syngeneic males. Vaginal plug denoted time of coitus and the gestation length, individual pup mass, and total pup number per litter were measured. Graphs show mean±SEM. ns, P>0.05, t test.
Discussion
HMW-MAA is a potential antigen for cancer immunotherapy that is expressed in a wide range of tumors and also in pericytes found in tumor angiogenic vasculature. Additionally, HMW-MAA may play a role in cell invasion and metastasis (1, 2). In this study, we generated a recombinant Lm that expresses and secretes a fragment of the HMW-MAA protein fused to a non-hemolytic form of the Listeriolysin-O (LLO) protein, despite the high hydrophobicity of the LLO-HMW-MAA2238–2246 fragment. Additionally, Lm-LLO-HMW-MAA-C retains its ability to replicate in the cytosol of host cells. It is believed that secretion of the LLO-antigen fusion protein and cytosol invasion are important features of a Lm-based vaccine, because antigens secreted at this stage would potentially be targeted to the MHC-class I processing pathway, consequently leading to activation of antigen-specific CD8+ T cells (11). In fact, most of the Lm epitopes presented by MHC class I molecules to CD8+ T cells are derived from proteins secreted by the bacteria in the cytosol (13, 25, 26). Besides, invasion of the cytosol by Lm has been shown to enhance the maturation of murine dendritic cells, generate higher number of functional CD8+ T cells (27) and protective immunity (28, 29).
Recombinant live-attenuated Lm has been extensively investigated as a potential vector to deliver and elicit cellular immunity against tumor-associated antigens. As a bacterial vector, Lm induces a potent innate immune response with activation of immune cells and production of several chemokines and cytokines such as IL-6, IL-12, IL-18, INF-γ, and TNF-α, which are important to generate effector T cells (13). As a vaccine vector, Lm has the ability to activate and deliver antigens into the intracellular environment of professional APCs such as macrophages and dendritic cells, resulting in strong cellular immune responses against these antigens, while raising minimum humoral responses against the bacterium itself (30). This is an advantage over live viral vaccine vectors, which induce strong humoral responses against the vector upon primary immunization, limiting their use in subsequent immunizations. Additionally, Lm does not integrate its genetic material into the host genome and unlike viral vectors, it can be eliminated quickly by a whole range of antibiotics, without compromising its efficacy (31).
In previous studies, we demonstrated that vaccination of mice with Lm recombinant vectors induced regression of established tumors expressing target antigens such as HPV16 E7 and HER-2/neu (9, 10). These studies also show that fusion of the antigen to a non-functional LLO increases the immunogenicity of the target antigen and the efficacy of the cancer immunotherapy (9, 10, 32). In agreement with these studies, Lm-LLO-HMW-MAA-C was able to specifically impede the growth of recently established B16F10 tumors expressing HMW-MAA, besides conferring a long-term immunity against this tumor.
T cells are known to play an essential role in tumor immunotherapy. In our model, we showed that CD4+ or CD8+ T cells are essential for the therapeutic efficacy of Lm-HMW-MAA-C. The importance of CD8+ T cells in the tumor rejection upon Lm-based immunotherapy has been previously shown and it is consistent with our findings (9, 10). As expected, CD8+ T cells from mice immunized with Lm-HMW-MAA-C could inhibit the growth of these tumors in vivo, in contrast to CD8+ T cells from non-immunized mice. Also, in the HLA-A2/Kb transgenic mouse, vaccination with Lm-HMW-MAA-C induced CD8+ T cell immunity against a HMW-MAA epitope restricted to the HLA-A2 molecule, which had been previously mapped (7). Together, these results suggest that vaccination with Lm-HMW-MAA-C induces CD8+ T cell responses against HMW-MAA that are important to the therapeutic effect of this vaccine.
In contrast to CD8+ T cell immunity, the role of CD4+ T cells in anti-tumoral immunity is less well characterized and may differ depending on the tumor model and vaccine strategy used. In the B16F10-HMW-MAA model and Lm-HMW-MAA-C vaccine, CD4+ cells were essential to control tumor growth. Although Lm infection is capable of activating CD8+ T cells even in the absence of CD4 help (33), several studies have reported that CD4+ T cells play an important role in antitumor immunity in B16F0 and B16F10 melanomas and other tumors (34–37). Interestingly, depletion of CD25+ cells did not improve the efficacy of the Lm-HMW-MAA-C vaccine against the B16F10-HMW-MAA tumor. CD25 is constitutively expressed by regulatory T cells and anti-CD25 antibody is commonly used to deplete these cells in vivo. However, CD25 is also expressed by recently activated effector CD4+ T cells and the elimination of CD25+ T cells, although may predominantly reduce regulatory CD25+CD4+ T cells, it may also impair the responses by reducing effector T cells (38). On the other hand, we and others have shown that fusion of the target antigen to LLO might be the major factor in modulating regulatory T cells (9, 39, 40) and also broadening the regions of an antigen recognizable as targets by CTLs (10). These results support the strategy of fusing tumor antigens to LLO to enhance the immunogenicity of such antigens and improve the therapeutic efficacy of Lm-based cancer vaccines (9, 10, 18, 32).
Systemic injection of Lm can nonspecifically impair the growth of some tumors, an effect that is dependent on NK cells (41). Besides tumor killing properties, NK cells are also a major primary source of IFN-γ during infection with Lm, probably contributing to the antitumor and antiangiogenic effects of Lm vaccination (42, 43). However, Lm-HMW-MAA-C vaccine can impact the growth of different transplantable tumors, which were not engineered to express HMW-MAA, more efficiently than other Lm vectors expressing irrelevant antigens. This effect was observed with RENCA, NT-2 and B16F10 tumors. Additionally, the Lm-HMW-MAA-C vaccine also significantly delayed the onset of mammary tumors in the FVB/N HER-2/neu transgenic mice. Although these tumor cells could express the AN2 protein at very low levels, an attractive hypothesis to explain this property of Lm-HMW-MAA-C is that vaccination against HMW-MAA targets pericytes in the tumor angiogenic vasculature, thus impairing the blood vessel formation in the tumor site. The AN2/HMW-MAA molecule is expressed at high levels in activated pericytes such as in wound healings and pericytes in the tumor stroma (44), which are important cells in vascular development, stabilization, maturation and remodeling (3, 4). Immunofluorescence staining showed a significant reduction in the number of pericytes expressing both αSMA and AN2 markers in NT-2 tumors from mice immunized with Lm-HMW-MAA-C, as compared to tumors from mice immunized with a control Lm vaccine. This finding suggests that vaccination with Lm-HMW-MAA-C can indeed target pericytes in the tumor vasculature, which might contribute to the improved efficacy of this vaccine in slowing down the tumor growth. Additionally, we observed an infiltration of CD8+ T cells around blood vessels and in the stroma of tumors from mice immunized with Lm-HMW-MAA-C, but not in tumors from the control group. This is an essential characteristic in a vaccine, because the presence of tumor infiltrating lymphocytes has been correlated with clinical responses in cancer immunotherapy (45). Noteworthy, we did not observe possible toxicity associated with blood vessel damage in mice immunized with Lm-HMW-MAA-C, such as wound healing, pregnancy or fertility problems.
An interesting possibility is to target HMW-MAA in combination with metronomic therapies to reduce tumor angiogenesis. It has been previously reported in a pre-clinical mouse model that inhibition of PDGFR signaling, which reduces pericytes counts, enhances the therapeutic efficacy of metronomic chemotherapy or VEGFR inhibition (46). Additionally, targeting pericytes in the tumor stroma might cause a certain degree of vasculitis that could promote the infiltration of the tumor by specific T cells to tumor-associated antigens and improve the efficacy of cancer immunotherapies. In this study, we did not investigate a possible role of antibodies against HMW-MAA that could be generated during the immunotherapy since antibodies are not thought to play a role in tumor immunotherapy using recombinant Lm as a vaccine vector (8, 47), as we previously demonstrated using a HER-2/neu tumor model (48). Thus enhanced efficacy might be achieved by combining Lm-HMW-MAA-C with active antibody-mediated therapies also targeting HMW-MAA. In a previous study, melanoma patients had prolonged survival upon immunization with an anti-idiotypic monoclonal antibody that mimics the determinant defined by an anti-HMW-MAA antibody (6).
In summary, these results indicate that immunization with Lm-HMW-MAA-C can induce cell-mediate immune responses against HMW-MAA that can impact the in vivo growth of a melanoma tumor expressing this antigen. This vaccine has shown not only potential to target tumors expressing HMW-MAA, but also other tumors, likely due to its effects in reducing the number of pericytes in the tumor vasculature. This characteristic makes this antigen suitable to be used as a universal antigen in cancer immunotherapy. In addition, even if the vaccine is not powerful enough to cause complete regression of all tumor lesions, it could be combined with other antigens and therapies to improve the efficacy of the therapeutic regimen.
Supplementary Material
Acknowledgements
Grant support: RO1CA109253 (Y.P.). Matthew Seavey is supported by training grant “The immunobiology of normal and neoplastic lymphocytes” T32CA09140.
We thank Russell Delgiacco at the Wistar Institute and Dan Martinez at the Children's Hospital of Philadelphia (CHOP) Research Pathology Core for their excellent technical assistance with all the histology and fluorescent microscopy.
Footnotes
Disclosure: Yvonne Paterson and Paulo Maciag wish to disclose that they have a financial interest in Advaxis, Inc., a vaccine and therapeutic company that has licensed or has an option to license all patents from the University of Pennsylvania that concern the use of Listeria monocytogenes or listerial products as vaccines.
References
- 1.Campoli MR, Chang CC, Kageshita T, Wang X, McCarthy JB, Ferrone S. Human high molecular weight-melanoma-associated antigen (HMW-MAA): a melanoma cell surface chondroitin sulfate proteoglycan (MSCP) with biological and clinical significance. Crit Rev Immunol. 2004;24:267–296. doi: 10.1615/critrevimmunol.v24.i4.40. [DOI] [PubMed] [Google Scholar]
- 2.Chang CC, Campoli M, Luo W, Zhao W, Zaenker KS, Ferrone S. Immunotherapy of melanoma targeting human high molecular weight melanoma-associated antigen: potential role of nonimmunological mechanisms. Ann N Y Acad Sci. 2004;1028:340–350. doi: 10.1196/annals.1322.040. [DOI] [PubMed] [Google Scholar]
- 3.Baluk P, Hashizume H, McDonald DM. Cellular abnormalities of blood vessels as targets in cancer. Curr Opin Genet Dev. 2005;15:102–111. doi: 10.1016/j.gde.2004.12.005. [DOI] [PubMed] [Google Scholar]
- 4.von Tell D, Armulik A, Betsholtz C. Pericytes and vascular stability. Exp Cell Res. 2006;312:623–629. doi: 10.1016/j.yexcr.2005.10.019. [DOI] [PubMed] [Google Scholar]
- 5.Schneider S, Bosse F, D'Urso D, et al. The AN2 protein is a novel marker for the Schwann cell lineage expressed by immature and nonmyelinating Schwann cells. J Neurosci. 2001;21:920–933. doi: 10.1523/JNEUROSCI.21-03-00920.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mittelman A, Chen ZJ, Yang H, Wong GY, Ferrone S. Human high molecular weight melanoma-associated antigen (HMW-MAA) mimicry by mouse anti-idiotypic monoclonal antibody MK2-23: induction of humoral anti-HMW-MAA immunity and prolongation of survival in patients with stage IV melanoma. Proc Natl Acad Sci U S A. 1992;89:466–470. doi: 10.1073/pnas.89.2.466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Peng L, Ko E, Luo W, Wang X, Shrikant PA, Ferrone S. CD4-dependent potentiation of a high molecular weight-melanoma-associated antigen-specific CTL response elicited in HLA-A2/Kb transgenic mice. J Immunol. 2006;176:2307–2315. doi: 10.4049/jimmunol.176.4.2307. [DOI] [PubMed] [Google Scholar]
- 8.Pan ZK, Ikonomidis G, Lazenby A, Pardoll D, Paterson Y. A recombinant Listeria monocytogenes vaccine expressing a model tumour antigen protects mice against lethal tumour cell challenge and causes regression of established tumours. Nat Med. 1995;1:471–477. doi: 10.1038/nm0595-471. [DOI] [PubMed] [Google Scholar]
- 9.Gunn GR, Zubair A, Peters C, Pan ZK, Wu TC, Paterson Y. Two Listeria monocytogenes vaccine vectors that express different molecular forms of human papilloma virus-16 (HPV-16) E7 induce qualitatively different T cell immunity that correlates with their ability to induce regression of established tumors immortalized by HPV-16. J Immunol. 2001;167:6471–6479. doi: 10.4049/jimmunol.167.11.6471. [DOI] [PubMed] [Google Scholar]
- 10.Singh R, Dominiecki ME, Jaffee EM, Paterson Y. Fusion to Listeriolysin O and delivery by Listeria monocytogenes enhances the immunogenicity of HER-2/neu and reveals subdominant epitopes in the FVB/N mouse. J Immunol. 2005;175:3663–3673. doi: 10.4049/jimmunol.175.6.3663. [DOI] [PubMed] [Google Scholar]
- 11.Paterson Y, Maciag PC. Listeria-based vaccines for cancer treatment. Curr Opin Mol Ther. 2005;7:454–460. [PubMed] [Google Scholar]
- 12.Portnoy DA, Auerbuch V, Glomski IJ. The cell biology of Listeria monocytogenes infection: the intersection of bacterial pathogenesis and cell-mediated immunity. J Cell Biol. 2002;158:409–414. doi: 10.1083/jcb.200205009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Pamer EG. Immune responses to Listeria monocytogenes. Nat Rev. 2004;4:812–823. doi: 10.1038/nri1461. [DOI] [PubMed] [Google Scholar]
- 14.Dietrich G, Hess J, Gentschev I, Knapp B, Kaufmann SH, Goebel W. From evil to good: a cytolysin in vaccine development. Trends Microbiol. 2001;9:23–28. doi: 10.1016/s0966-842x(00)01893-x. [DOI] [PubMed] [Google Scholar]
- 15.Yamamoto K, Kawamura I, Tominaga T, et al. Listeriolysin O, a cytolysin derived from Listeria monocytogenes, inhibits generation of ovalbumin-specific Th2 immune response by skewing maturation of antigen-specific T cells into Th1 cells. Clin Exp Immunol. 2005;142:268–274. doi: 10.1111/j.1365-2249.2005.02922.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kohda C, Kawamura I, Baba H, et al. Dissociated linkage of cytokine-inducing activity and cytotoxicity to different domains of listeriolysin O from Listeria monocytogenes. Infect Immun. 2002;70:1334–1341. doi: 10.1128/IAI.70.3.1334-1341.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kimoto T, Kawamura I, Kohda C, et al. Differences in gamma interferon production induced by listeriolysin O and ivanolysin O result in different levels of protective immunity in mice infected with Listeria monocytogenes and Listeria ivanovii. Infect Immun. 2003;71:2447–2454. doi: 10.1128/IAI.71.5.2447-2454.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Sewell DA, Shahabi V, Gunn GR, 3rd, Pan ZK, Dominiecki ME, Paterson Y. Recombinant Listeria vaccines containing PEST sequences are potent immune adjuvants for the tumor-associated antigen human papillomavirus-16 E7. Cancer Res. (3rd) 2004;64:8821–8825. doi: 10.1158/0008-5472.CAN-04-1958. [DOI] [PubMed] [Google Scholar]
- 19.Hussain SF, Paterson Y. What is needed for effective antitumor immunotherapy? Lessons learned using Listeria monocytogenes as a live vector for HPV-associated tumors. Cancer Immunol Immunother. 2005;54:577–586. doi: 10.1007/s00262-004-0600-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Muller WJ. Expression of activated oncogenes in the murine mammary gland: transgenic models for human breast cancer. Cancer Metastasis Rev. 1991;10:217–227. doi: 10.1007/BF00050793. [DOI] [PubMed] [Google Scholar]
- 21.Chen ZJ, Ferrone S. Comparison of the binding parameters to melanoma cells of antihuman high molecular weight-melanoma associated antigen (HMW-MAA) monoclonal antibodies (mAb) and syngeneic anti-anti-idiotypic (anti-anti-id) mAb. Ann N Y Acad Sci. 1993;690:398–401. doi: 10.1111/j.1749-6632.1993.tb44043.x. [DOI] [PubMed] [Google Scholar]
- 22.Peters C, Paterson Y. Enhancing the immunogenicity of bioengineered Listeria monocytogenes by passaging through live animal hosts. Vaccine. 2003;21:1187–1194. doi: 10.1016/s0264-410x(02)00554-6. [DOI] [PubMed] [Google Scholar]
- 23.Niethammer AG, Xiang R, Becker JC, et al. A DNA vaccine against VEGF receptor 2 prevents effective angiogenesis and inhibits tumor growth. Nat Med. 2002;8:1369–1375. doi: 10.1038/nm1202-794. [DOI] [PubMed] [Google Scholar]
- 24.Reilly RT, Gottlieb MB, Ercolini AM, et al. HER-2/neu is a tumor rejection target in tolerized HER-2/neu transgenic mice. Cancer Res. 2000;60:3569–3576. [PubMed] [Google Scholar]
- 25.Geginat G, Schenk S, Skoberne M, Goebel W, Hof H. A novel approach of direct ex vivo epitope mapping identifies dominant and subdominant CD4 and CD8 T cell epitopes from Listeria monocytogenes. J Immunol. 2001;166:1877–1884. doi: 10.4049/jimmunol.166.3.1877. [DOI] [PubMed] [Google Scholar]
- 26.Kamm C, Skoberne M, Geginat G. CD8 T cell immunome analysis of Listeria monocytogenes. FEMS Immunol Med Microbiol. 2003;35:235–242. doi: 10.1016/S0928-8244(02)00450-9. [DOI] [PubMed] [Google Scholar]
- 27.Brzoza KL, Rockel AB, Hiltbold EM. Cytoplasmic entry of Listeria monocytogenes enhances dendritic cell maturation and T cell differentiation and function. J Immunol. 2004;173:2641–2651. doi: 10.4049/jimmunol.173.4.2641. [DOI] [PubMed] [Google Scholar]
- 28.Berche P, Gaillard JL, Sansonetti PJ. Intracellular growth of Listeria monocytogenes as a prerequisite for in vivo induction of T cell-mediated immunity. J Immunol. 1987;138:2266–2271. [PubMed] [Google Scholar]
- 29.Bahjat KS, Liu W, Lemmens EE, et al. Cytosolic entry controls CD8+-T-cell potency during bacterial infection. Infect Immun. 2006;74:6387–6397. doi: 10.1128/IAI.01088-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Schafer R, Portnoy DA, Brassell SA, Paterson Y. Induction of a cellular immune response to a foreign antigen by a recombinant Listeria monocytogenes vaccine. J Immunol. 1992;149:53–59. [PubMed] [Google Scholar]
- 31.Corbin GA, Harty JT. Duration of infection and antigen display have minimal influence on the kinetics of the CD4+ T cell response to Listeria monocytogenes infection. J Immunol. 2004;173:5679–5687. doi: 10.4049/jimmunol.173.9.5679. [DOI] [PubMed] [Google Scholar]
- 32.Lamikanra A, Pan ZK, Isaacs SN, Wu TC, Paterson Y. Regression of established human papillomavirus type 16 (HPV-16) immortalized tumors in vivo by vaccinia viruses expressing different forms of HPV-16 E7 correlates with enhanced CD8(+) T-cell responses that home to the tumor site. J Virol. 2001;75:9654–9664. doi: 10.1128/JVI.75.20.9654-9664.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Shedlock DJ, Whitmire JK, Tan J, MacDonald AS, Ahmed R, Shen H. Role of CD4 T cell help and costimulation in CD8 T cell responses during Listeria monocytogenes infection. J Immunol. 2003;170:2053–2063. doi: 10.4049/jimmunol.170.4.2053. [DOI] [PubMed] [Google Scholar]
- 34.Ossendorp F, Toes RE, Offringa R, van der Burg SH, Melief CJ. Importance of CD4(+) T helper cell responses in tumor immunity. Immunol Lett. 2000;74:75–79. doi: 10.1016/s0165-2478(00)00252-2. [DOI] [PubMed] [Google Scholar]
- 35.Wu TY, Fleischmann WR., Jr. Murine B16 melanoma vaccination-induced tumor immunity: identification of specific immune cells and functions involved. J Interferon Cytokine Res. 2001;21:1117–1127. doi: 10.1089/107999001317205259. [DOI] [PubMed] [Google Scholar]
- 36.Goldszmid RS, Idoyaga J, Bravo AI, Steinman R, Mordoh J, Wainstok R. Dendritic cells charged with apoptotic tumor cells induce long-lived protective CD4+ and CD8+ T cell immunity against B16 melanoma. J Immunol. 2003;171:5940–5947. doi: 10.4049/jimmunol.171.11.5940. [DOI] [PubMed] [Google Scholar]
- 37.Knutson KL, Disis ML. Tumor antigen-specific T helper cells in cancer immunity and immunotherapy. Cancer Immunol Immunother. 2005;54:721–728. doi: 10.1007/s00262-004-0653-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Yamaguchi T, Sakaguchi S. Regulatory T cells in immune surveillance and treatment of cancer. Semin Cancer Biol. 2006;16:115–123. doi: 10.1016/j.semcancer.2005.11.005. [DOI] [PubMed] [Google Scholar]
- 39.Nitcheu-Tefit J, Dai MS, Critchley-Thorne RJ, et al. Listeriolysin O expressed in a bacterial vaccine suppresses CD4+CD25high regulatory T cell function in vivo. J Immunol. 2007;179:1532–1541. doi: 10.4049/jimmunol.179.3.1532. [DOI] [PubMed] [Google Scholar]
- 40.Hussain SF, Paterson Y. CD4+CD25+ regulatory T cells that secrete TGFbeta and IL-10 are preferentially induced by a vaccine vector. J Immunother. 2004;27:339–346. doi: 10.1097/00002371-200409000-00002. (1997) [DOI] [PubMed] [Google Scholar]
- 41.Huang B, Zhao J, Shen S, et al. Listeria monocytogenes promotes tumor growth via tumor cell toll-like receptor 2 signaling. Cancer Res. 2007;67:4346–4352. doi: 10.1158/0008-5472.CAN-06-4067. [DOI] [PubMed] [Google Scholar]
- 42.Thale C, Kiderlen AF. Sources of interferon-gamma (IFN-gamma) in early immune response to Listeria monocytogenes. Immunobiology. 2005;210:673–683. doi: 10.1016/j.imbio.2005.07.003. [DOI] [PubMed] [Google Scholar]
- 43.Yao L, Sgadari C, Furuke K, Bloom ET, Teruya-Feldstein J, Tosato G. Contribution of natural killer cells to inhibition of angiogenesis by interleukin-12. Blood. 1999;93:1612–1621. [PubMed] [Google Scholar]
- 44.Schlingemann RO, Rietveld FJ, de Waal RM, Ferrone S, Ruiter DJ. Expression of the high molecular weight melanoma-associated antigen by pericytes during angiogenesis in tumors and in healing wounds. Am J Pathol. 1990;136:1393–1405. [PMC free article] [PubMed] [Google Scholar]
- 45.Haanen JB, Baars A, Gomez R, et al. Melanoma-specific tumor-infiltrating lymphocytes but not circulating melanoma-specific T cells may predict survival in resected advanced-stage melanoma patients. Cancer Immunol Immunother. 2006;55:451–458. doi: 10.1007/s00262-005-0018-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Pietras K, Hanahan D. A multitargeted, metronomic, and maximum-tolerated dose ”chemo-switch” regimen is antiangiogenic, producing objective responses and survival benefit in a mouse model of cancer. J Clin Oncol. 2005;23:939–952. doi: 10.1200/JCO.2005.07.093. [DOI] [PubMed] [Google Scholar]
- 47.Starks H, Bruhn KW, Shen H, et al. Listeria monocytogenes as a vaccine vector: virulence attenuation or existing antivector immunity does not diminish therapeutic efficacy. J Immunol. 2004;173:420–427. doi: 10.4049/jimmunol.173.1.420. [DOI] [PubMed] [Google Scholar]
- 48.Singh R, Paterson Y. In the FVB/N HER-2/neu transgenic mouse both peripheral and central tolerance limit the immune response targeting HER-2/neu induced by Listeria monocytogenes-based vaccines. Cancer Immunol Immunother. 2007;56:927–938. doi: 10.1007/s00262-006-0237-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.