Abstract
The classification of an unexpected infant death as the sudden infant death syndrome (SIDS) depends upon a complete autopsy and death scene investigation to exclude known causes of death. Here we report the death of a four-month-old infant in a tuberculosis endemic area that presented as a sudden unexpected death in infancy (SUDI) with no apparent explanation based on the death scene characteristics. The autopsy, however, revealed progressive primary pulmonary tuberculosis with intrathoracic adenopathy, compression of the tracheobronchial tree and miliary lesions in the liver. This case underscores the clinical difficulties in the diagnosis of infantile tuberculosis, as well as the possibility of sudden death as part of its protean manifestations. The pathology and clinical progression of tuberculosis in infants differs from older children and adults due to the immature immune response in infants. This case dramatically highlights the need for complete autopsies in all sudden and unexpected infant deaths, as well as the public health issues in a sentinel infant tuberculosis diagnosis.
Keywords: Airway obstruction, Tuberculosis, Autopsy, Sudden Infant Death Syndrome (SIDS), Sudden Unexplained Death in Infancy (SUDI), South Africa
Introduction
Sudden unexpected death in infancy (SUDI) remains a global challenge for medicine and society. A complete autopsy and death scene investigation are an essential part of their investigation and have contributed to delineating many unexpected causes of infant deaths. The sudden infant death syndrome (SIDS) accounts for 50-80% of SUDI [1]; it is defined as the sudden death of an infant less than a year old, the cause of which remains unknown after a complete autopsy, death scene investigation and review of medical history [16]. Research efforts span multiple avenues in an attempt to identify pre- and post-natal risk factors with the goal of reducing infant mortality [6]. We are involved in a large (7000 pregnancies), prospective study of SIDS and other adverse pregnancy and infant outcomes (the Safe Passage Study) in the mixed ancestry (Coloured) population of Cape Town, South Africa. In Cape Town, the SIDS incidence is high (3.8/1000 live births) [10] compared to 0.57/1000 in the United States [9]. Mycobacterium tuberculosis infection (TB) is endemic in the Western Cape, with an overall incidence rate of 1037/100,000; the incidence rate among infants is 83.1/100,000 and in HIV-infected infants this rises to 1596/100,000 population [4]. We report a case of an infant with sudden death in Phase 1 of the Safe Passage Study that, on death scene investigation may have suggested SIDS, but in whom TB was diagnosed on autopsy, indicating that sudden and unexpected death should be included in its wide spectrum of infant manifestations.
Case Report
A 4.5-month-old male infant was found dead in bed by his mother. The mother was a 22 year-old G2P2A0 whose first pregnancy was complicated by mild pre-eclampsia but the antenatal course of this pregnancy was uneventful. The mother did not smoke or drink and sought prenatal care at 12 weeks gestation when routine prenatal tests, including those for syphilis and HIV, were negative. Ultrasonography performed at 22 weeks established a gestational age and excluded major congenital abnormalities. Fetal growth as assessed by symphysis pubis-fundus measurements was normal as were the umbilical artery flow velocity waveform and non-stress tests at 29 and 35 gestational weeks. The infant was born at 38 gestational weeks by uncomplicated vaginal delivery, weighing 3440 grams with Apgar scores of 9, 10 and 10 at 1, 5 and 10 minutes, respectively. At birth the hemoglobin of the newborn was 17 g/dL and the glucose 49 mg/dL (2.7 mmol/L). The infant stayed with the mother after delivery and both were discharged from hospital one day post-delivery. Neonatal course and well-baby checks were unremarkable; immunizations were up-to-date, including BCG given before discharge from hospital. At the 2-month follow-up visit, the infant's weight was between the 3rd and 50th centiles for the local population. For the two weeks prior to his death, the infant had mild upper respiratory symptoms with suspected (but not proven) fever, which improved symptomatically upon treatment with home remedies; the mother regarded the illness as trivial and did not think it necessary to attend the nearby hospital. The day of his demise, the infant was “crying and fussy” in the early morning hours but eventually fell asleep. He was found deceased five hours later in a prone position with his head turned to the side.
The case was referred for forensic autopsy and the parents gave permission for additional tissue procurement for research in the Safe Passage Study. A death scene investigation was performed within 14 days of death by the authors according to the SUDI/SIDS protocols of the Center for Disease Control, Atlanta, GA, USA [1]. At the time of death, the infant was bed sharing with his parents and two other children in a double bed, typical of the family sleeping arrangements. The bedding was firm with no pillows or heavy blankets. There was no evidence or history of wedging, asphyxial positioning or overlay by any of the bed occupants
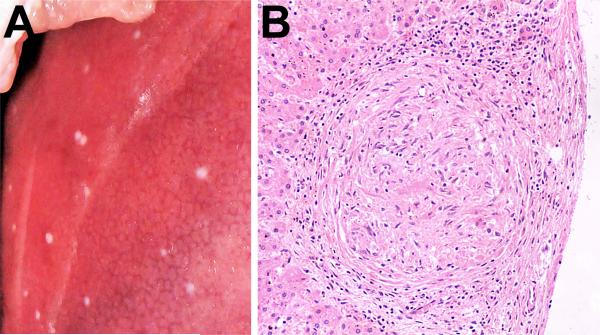
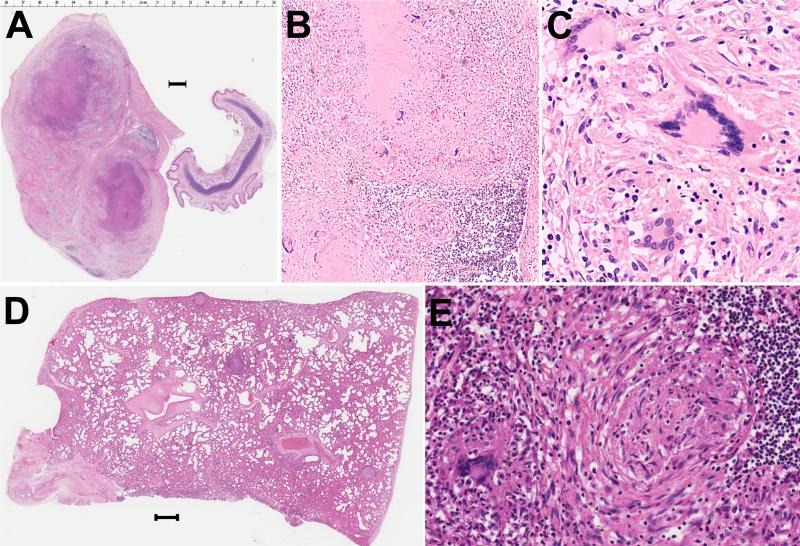
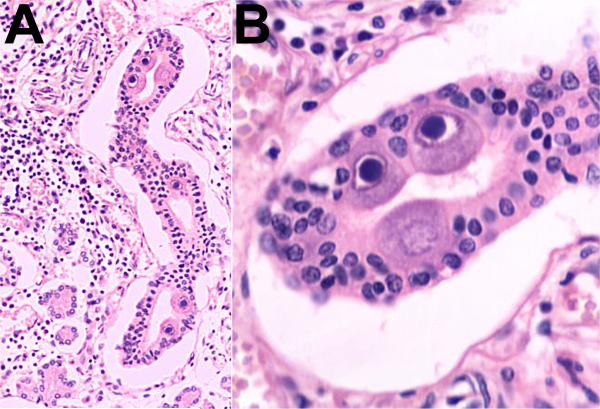
Pediatric autopsy was performed on a male infant, length 65.5 cm (60 -66 cm), weighing 6.0 kg (5.8-7.8 kg). The surface of the liver demonstrated numerous white nodules, 1 mm or less (Figure 1a) which microscopically showed non-caseating granulomas (Figure 1b). A 2.5 cm caseating mass with cavitation was present in the upper lobe of the right lung, with large, matted hilar and tracheobronchial nodes which appeared to partially occlude the airway (Figure 2). Histology of the lung and nodes confirmed granulomatous inflammation with amorphous necrosis and giant cells (Figure 2); Ziehl – Neelsen stains were positive for acid fast bacilli consistent with TB. The parotid gland showed evidence of cytomegalovirus (CMV) infection (Figure 3) but there was no evidence of systemic CMV infection. The examination of the brain and spinal cord was negative for TB meningitis. The death scene, historical, and autopsy findings were reviewed by all authors and a consensus diagnosis reached of progressive primary pulmonary tuberculosis with caseation and cavitation, complicated by intrathoracic adenopathy, compression of the airway, and miliary spread to the liver. Testing for HIV was negative. Investigation of family and contacts excluded TB in the father and mother but identified TB in a cousin, a close contact of the deceased infant.
Figure 1.
A) Liver at autopsy showing numerous 1 mm white nodules involving the capsule. B) Histology of the liver nodule demonstrating non-caseating granulomas. 100 x, H&E.
Figure 2.
A) One of the large tracheal-bronchial lymph nodes with caseation necrosis and the smaller trachea for comparison. Bar is 1 mm. 1 x, H&E. B) Histology of hilar lymph node showing amorphous necrosis. 100 x, H&E. C) Giant cells within the granulomas of the hilar lymph node, 400 x, H&E.. D) Lung with multiple granulomas throughout the parenchyma and at pleural surface. Bar is 1 mm. 1x, H&E. E. Histology of lung granuloma. 200x, H&E.
Figure 3.
A) Histology of parotid gland demonstrating CMV infection 100 x, H&E. B) High power of salivary gland ductal epithelial cells with CMV inclusions, 400 x, H&E.
Discussion
There are few categories of death in medicine with a broader range of diagnoses than SUDI in both manner and cause of death. Within the SIDS differential, many entities have profound ramifications in public health, such as contagious diseases or hazardous environments, in family health with unsuspected genetic and metabolic disease, or in legal arenas with infant homicide, poisoning or neglect. The case reported here dramatically illustrates the importance of autopsy findings in identifying a communicable disease within a family and community. It also highlights the difficulty of diagnosing TB in infants and the difference in the clinical presentation of TB among infants, older children, and adults.
Neonates (and infants) can acquire TB either prenatally from infected mothers (congenital TB) or postnatally from respiratory exposure (neonatal TB). Infants have a 50% risk of disease following exposure and a high rate of miliary or CNS involvement (10-20%) [12, 2] compared to less than a 5% risk of disease and 0.5 – 2.5 rate of miliary/CNS disease in older children and 10 – 20% risk of disease and <0.5% miliary / CNS involvement in adults following primary exposure to TB [2]. In TB endemic areas such as South Africa, BCG vaccination is given within days of birth which confers limited immunity but does protect against disseminated tuberculosis, particularly TB meningitis [11, 5]. Determination of the source of exposure for infants is important for public health assessment; however, both congenital and neonatal TB are similar in clinical presentation and course. Congenital tuberculosis is rare and results from in utero exposure by: (1) hematogenous infection via the umbilical vein; (2) exposure to infected amniotic fluid, including aspiration and/or swallowing; and/or (3) contact with maternal genital lesions during birth. A diagnosis of congenital TB is based on evidence of TB in the infant and at least one of the following: 1) lesions in the first week of life; (2) a primary hepatic complex (3) documented tuberculosis infection of the endometrium or placenta; or (4) exclusion of post-natal sources of mycobacterial infection [14]. By all criteria, the progressive primary tuberculosis in this infant was from post-natal exposure and not congenitally acquired.
The clinical diagnosis of TB in an infant is challenging. Infants may present with non-specific findings such as reduced playfulness, fatigue, wheezing, non-remitting cough, failure-to-thrive or hepatosplenomegaly [15]. In infants who are more acutely ill, TB may be suspected when they are not responsive to first line antibiotics [8]. Skin tests, the hallmark screening test for older children and adults, are not reliable in infants due to their immature immune response. In our case, mild respiratory symptoms and fever were present after birth, but were considered nonspecific, particularly in light of appropriate growth and development. The pathology of TB in infants differs from older children and adults; progressive primary disease is more frequently seen in young infants while pleural effusions are uncommon [2]. Miliary spread and meningitis are more common in infants than any other age group (10-20%), as are complications due to enlarging lymph nodes and small airways [8]. Children under three have a high mortality rate due in part to the diagnostic difficulty of TB in infants and small children, as well as the increased rate of progressive disease and CNS involvement [8, 13]. Co-infection with HIV increases the infection rate and mortality of children with TB [13, 7]. Microscopically, granulomas may be poorly formed in infants with TB, and the inflammatory response may be sparse and necrosis present [3].
Finally there are several important forensic implications of this case. Investigation of sudden deaths in infancy is clearly within responsibilities of the forensic death systems worldwide. These investigations serve as a gatekeeper to the entire medical-legal enterprise; triggering responses that may include police investigation, arrest, and/or child protective service involvement. Through prompt recognition of a natural disease process, justice is served by avoiding prosecutorial actions toward parents / caregiver as well as preserving community, law-enforcement and legal resources. Communicable diseases and public health implications are also an important part of forensic pathology practice; prompt recognition of this entity enabled identification of TB within this family unit.
Conclusions
In summary, we report a case of progressive primary pulmonary TB in an infant with sudden unexpected death that some investigators may have suspected was due to SIDS. Although mild, non-specific upper respiratory symptoms were present in the days before death, these symptoms are common in infants of this age, they responded to home remedies and on the day of death only a “crying and fussiness” occurred. The autopsy confirmed pulmonary parenchymal TB with caseation and cavitation complicated by intrathoracic adenopathy, compression of the airway and miliary spread to the liver, emphasizing the need for complete autopsy and death scene assessment in all infant deaths. Without a complete autopsy, this death may have been attributed to unspecified natural causes, resulting in continued TB exposure of other family members and community, or the death may have been investigated as unnatural, wasting forensic resources and potentially resulting in a miscarriage of justice. This death was sentinel in identifying TB in a family member, congruent with the public health ramifications of pediatric autopsies.
Acknowledgments
This research was funded by the following grants from the National Institute on Alcohol Abuse and Alcoholism and the Eunice Kennedy Shriver National Institute of Child Health and Human Development: U01 HD055154, U01 HD045935, U01 HD055155, U01 HD045991, and U01 AA016501.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Center for Disease Control (CDC) Atlanta, GA, USA [January 2, 2010];Sudden Infant Death Syndrome (SIDS) and Sudden Unexpected Infant Death (SUID): Sudden, Unexpected Infant Death (SUID) Initiative. http://www.cdc.gov/SIDS/SUID.htm.
- 2.Cruz AT, Starke JR. Clinical manifestations of tuberculosis in children. Paediatric Respiratory Reviews. 2007;8:107–117. doi: 10.1016/j.prrv.2007.04.008. [DOI] [PubMed] [Google Scholar]
- 3.Gögüş S, Umer H, Akçören Z, Sanal O, Osmanlioglu G, Cimbiş M. Neonatal tuberculosis. Pediatr. Pathol. 1993;13:299–304. doi: 10.3109/15513819309048216. [DOI] [PubMed] [Google Scholar]
- 4.Hesseling AC, Cotton MF, Jennings T, Whitelaw A, Johnson LF, Eley B, Roux P, Godfrey-Faussett P, Schaaf HS. High Incidence of Tuberculosis among HIV-Infected Infants: Evidence from a South African Population-Based Study Highlights the Need for Improved Tuberculosis Control Strategies. Clinical Infectious Diseases. 2009;48:108–114. doi: 10.1086/595012. [DOI] [PubMed] [Google Scholar]
- 5.Hesseling AC, Rabie H, Marais BJ, Manders M, Lips M, Schaaf HS, Gie RP, Cotton MF, van Helden PD, Warren RM, Beyers N. Bacille Calmette-Guérin Vaccine–Induced Disease in HIV-Infected and HIV-Uninfected Children. Clin. Infect. Dis. 2006;42:548–558. doi: 10.1086/499953. [DOI] [PubMed] [Google Scholar]
- 6.Kinney HC, Thach BT. The sudden infant death syndrome. N Engl J Med. 2009 Aug 20;361(8):795–805. doi: 10.1056/NEJMra0803836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Madhi SA, Huebner RE, Doedens L, Aduc T, Wesley D, Cooper PA. HIV-1 co-infection in children hospitalized with tuberculosis in South Africa. Int. J. Tuberc. Lung Dis. 2000;4:448–454. [PubMed] [Google Scholar]
- 8.Marais BJ. Tuberculosis in children. Pediatr. Pulmonol. 2008;43:322–329. doi: 10.1002/ppul.20787. [DOI] [PubMed] [Google Scholar]
- 9.Mathews TJ, MacDorman MF. Infant mortality statistics from the 2005 period linked birth/infant death data set. Natl. Vital Stat. Rep. 2008;57:1–32. [PubMed] [Google Scholar]
- 10.Molteno CD, Ress E, Kibe MA. Early childhood mortality in Cape Town. S. Afr. Med. J. 1989;75:570–574. [PubMed] [Google Scholar]
- 11.Nelson LJ, Wells CD. Tuberculosis in children: Considerations for children from developing countries. Semin. Pediatr. Infect. Dis. 2004;15:150–154. doi: 10.1053/j.spid.2004.05.007. [DOI] [PubMed] [Google Scholar]
- 12.Newton SM, Brent AJ, Anderson S, Whittaker E, Kampmann B. Paediatric tuberculosis. Lancet Infectious Diseases. 2008;8:498–510. doi: 10.1016/S1473-3099(08)70182-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Schaaf HS, Marais BJ, Whitelaw A, Hesseling AC, Eley B, Hussey GD, Donald PR. Culture-confirmed childhood tuberculosis in Cape Town, South Africa: a review of 596 cases. BMC Infect. Dis. 2007;7:140–147. doi: 10.1186/1471-2334-7-140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Smith KC. Congenital tuberculosis: a rare manifestation of a common infection. Current Opinion in Infectious Diseases. 2002;15:269–274. doi: 10.1097/00001432-200206000-00009. [DOI] [PubMed] [Google Scholar]
- 15.Vallejo JG, Ong LT, Starke JR. Clinical features, diagnosis and treatment of tuberculosis in infants. Pediatrics. 1994;94:1–7. [PubMed] [Google Scholar]
- 16.Willinger M, James LS, Catz C. Defining the sudden infant death syndrome (SIDS): Deliberations of an expert panel convened by the National Institute of Child Health and Development. Pediatr. Pathol. 1991;11:677–684. doi: 10.3109/15513819109065465. [DOI] [PubMed] [Google Scholar]