Abstract
Six monoclonal antibodies were isolated that exhibited specificity for a furin cleavage site deletion mutant (V3526) of Venezuelan equine encephalitis virus (VEEV). These antibodies comprise a single competition group and bound the E3 glycoprotein of VEEV subtype I viruses but failed to bind the E3 glycoprotein of other alphaviruses. These antibodies neutralized V3526 virus infectivity but did not neutralize the parental strain of Trinidad donkey (TrD) VEEV. However, the E3-specific antibodies did inhibit the production of virus from VEEV TrD-infected cells. In addition, passive immunization of mice demonstrated that antibody to the E3 glycoprotein provided protection against lethal VEEV TrD challenge. This is the first recognition of a protective epitope in the E3 glycoprotein. Furthermore, these results indicate that E3 plays a critical role late in the morphogenesis of progeny virus after E3 appears on the surfaces of infected cells.
Viruses in the Alphavirus genus of the family Togaviridae are composed of an icosahedral nucleocapsid surrounded by a lipid envelope studded with a distinctive lattice of glycoprotein spikes. The structural proteins of alphaviruses arise through co- and posttranslational processing of a polyprotein encoded by a single 26S mRNA (22, 27) in which the order of the gene products is NH2-capsid-PE2-6K-E1-COOH. The capsid (C) protein cleaves itself from the nascent polypeptide soon after emergence from the ribosome. The PE2 glycoprotein is a precursor containing the E3 glycoprotein fused to the amino terminus of the E2 envelope glycoprotein. The PE2 glycoprotein is followed by 6K, a small membrane-associated protein, and E1, the second polypeptide component of glycoprotein spikes. Trimerized heterodimers of the E1 and E2 viral glycoproteins form the surface spikes and contain determinants of viral tropism and virulence (1).
The E3 glycoprotein acts as a signal for transport of PE2 across the membranes of the rough endoplasmic reticulum (22) and may promote the formation and intracellular transport of E1-PE2 heterodimers (12, 23, 46) to the cell surface. The E2 glycoprotein promotes specificity of virus binding to the host cell surface and is a target of protective antibodies (7, 18-20, 39). The E1 glycoprotein mediates fusion of the virion envelope with the membranes of acidified endosomes, allowing release of the nucleocapsid into the cytoplasm and the onset of viral replication (21, 40, 43). Antibodies to the E1 glycoprotein do not typically neutralize virus infectivity in vitro but can protect against lethal challenge in animals (41, 42). During transport to the cell surface, PE2 undergoes a maturational cleavage event by a furin-like protease to produce E2 and E3. The E3 glycoprotein may be subsequently released into the extracellular space (26, 49) or incorporated into the virion (6, 13). At the plasma membrane, trimerized E1-E2 heterodimers are incorporated into the budding virus particle.
Mutations that block cleavage of PE2 of Venezuelan equine encephalitis virus (VEEV) are lethal mutations (3). However, transfection of RNA transcribed from cleavage site deletion genomic cDNA clones results in rescue of pseudorevertant virus due to the appearance of second site mutations arising at a variety of locations in the glycoprotein genes (17). As a consequence of the cleavage site mutation, the spikes of pseudorevertant virions are composed of PE2 and E1.
One cleavage site deletion mutant, V3526, was prepared by mutagenesis of a genomic cDNA clone of Trinidad donkey (TrD). The virus encoded by this clone contains a 12-nucleotide deletion of the sequence encoding the furin cleavage site, as well as a Phe-to-Ser change at position 253 of the E1 glycoprotein (8). V3526 is attenuated and induces a robust protective antibody response against VEEV TrD in rodents, equines, and nonhuman primates (5, 9, 14-16, 37). V3526 also elicits protection in animals against challenge by other VEEV subtypes (9, 15, 37). During the characterization of the immune response elicited by V3526 in mice, a collection of monoclonal antibodies (MAbs) was isolated that preferentially bound V3526 virions compared to VEEV TrD. We report here that these MAbs bind a previously unrecognized epitope on the E3 glycoprotein. In addition, we show that MAbs specific for the VEEV E3 glycoprotein inhibit production of subtype I VEEVs in cell culture and protect mice from lethal challenge with VEEV TrD.
(A portion of this work was submitted in thesis form by M. J. Buckley as a requirement for a Master of Science degree at Hood College, Frederick, MD.)
MATERIALS AND METHODS
Viruses.
The plasmid encoding VEEV strain V3526 was obtained from N. Davis, University of North Carolina, Chapel Hill, NC, and virus was rescued by transfection of BHK-21 cells (8). VEEV subtype I-C strain 686, subtype I-D strain 6880, and subtype I-E strain 68U201 viruses were obtained from S. C. Weaver, University of Texas Medical Branch, Galveston, TX. VEEV TrD, Mucambo virus, Eastern equine encephalitis virus (EEEV) strain Fla91-4679 (28), and Western equine encephalitis virus (WEEV) strain CBA87 (4) were obtained from USAMRIID archives. Working stocks of each virus were prepared by a single passage in BHK-21 cells.
Preparation of MAbs.
BALB/c mice were inoculated intraperitoneally (i.p.) with 2 × 105 PFU of V3526. Four weeks later, an additional 40 μg of Co60-irradiated V3526 were administered by tail vein infusion. Spleen cells were harvested 48 h later and fused with SP2/0-Ag14 myeloma cells as described previously (45). Hybridoma supernatants were screened by enzyme-linked immunosorbent assay (ELISA) for reactivity with purified V3526 and VEEV TrD. VEEV MAb 1A4A-1, specific for epitope E2C (39), was obtained from John Roehrig, Centers for Disease Control and Prevention, Fort Collins, CO. For passive immunization, antibodies were purified by MAbTrap column chromatography (Amersham Biosciences). Plaque reduction neutralization tests (PRNTs) on Vero cells were performed as described previously (36).
Competitive binding assay.
Sucrose gradient purified virus was diluted to 4 μg/ml in sodium carbonate buffer (15 mM Na2CO3 and 35 mM NaHCO3 in distilled water [pH 9.6]) and 50 μl/well were added to 96-well Flexplates, which were incubated at 4°C overnight. Plates were washed five times with wash buffer (1% fish gelatin, phosphate-buffered saline [PBS], 0.5% Tween 20). Residual binding sites were blocked with 300 μl of blocking buffer (5% fish gelatin, PBS, 0.5% Tween 20), and plates were incubated at 37°C for 1 h. Blocking buffer was aspirated from the wells. Unlabeled MAbs were serially diluted 3-fold from 2 μg/well to 0.001 μg/ml in bovine serum albumin (BSA)-PBS blocking diluents (KPL, Inc.). Diluted unlabeled MAbs were added to the plates at 50 μl/well, followed by incubation at 37°C for 1 h. Plates were washed five times with wash buffer as described above. Biotin-labeled MAbs were added at a concentration of 2 ng/well (50 μl) to all wells of a single 96-well plate, followed by incubation at 37°C for 1 h. After a washing step, 100 μl of a 1:2,000 dilution of peroxidase-labeled Strep-Avidin (Amersham) was added/well, followed by incubation at 37°C for 1 h. Plates were washed and developed with ABTS [2,2′azinobis(3-ethylbenzthiazolinesulfonic acid)] substrate (KPL, Inc.) for 30 min at room temperature. Absorbance was measured by utilizing dual wavelengths of 410 to 490 nm. Any dilution of unlabeled MAb showing an optical density at 410 nm (OD410) value of <0.3 was considered to show competition with the biotin-labeled MAb. The mean OD410 values with no subtraction of background were obtained for duplicate wells at each concentration tested.
Plaque reduction neutralization assay.
Aliquots (100 μl) of virus containing 100 PFU were combined with an equal volume of Dulbecco modified Eagle medium (DMEM) containing the serially diluted antibody indicated and held overnight at 4°C. The virus antibody mixtures were then added to confluent monolayers of Vero cells, followed by incubation at 37°C at 5% CO2 for 1 h. The monolayers were then overlaid with 2 ml of 0.6% agarose in DMEM containing 10% fetal bovine serum (FBS). After 24 h, a second overlay of 0.6% agarose in DMEM containing 5% FBS and neutral red was added, and the plates were incubated at 37°C at 5% CO2. Plaques were enumerated the following day. Virus infectivity was considered neutralized if the number of plaques was decreased by 80% compared to controls that contained FBS or an irrelevant MAb.
Virus infection and protein blotting.
BHK-21 cells were infected at a multiplicity of infection (MOI) of 10. At 12 h after infection, lysates were analyzed on 10% sodium dodecyl sulfate (SDS)-polyacrylamide gels. The gels were electroblotted onto nitrocellulose and probed with primary antibody overnight at room temperature, followed by a peroxidase-conjugated anti-mouse IgG (KPL, Inc.). The membrane was developed with TMB membrane peroxidase substrate and membrane enhancer (KPL, Inc.) in a ratio of 9:1.
E3 glycoprotein expression.
An expression cassette encoding amino acids 1 to 45 of the VEEV E3 glycoprotein fused to amino acids 18 to 565 of the hemagglutinin (HA) protein of influenza virus A/PR/8/34 (accession no. EF190974) was prepared by overlap extension PCR (48). Primer sequences are available on request. Flanking ClaI sites and an ATG codon were added to the cassette in the final amplification step, and the fragment was cloned into a VEE replicon, designated VRP-E3HA, for expression in BHK-21 cells (35). At 16 h posttransfection of VRP-E3HA RNA, the cells were collected, and lysates were analyzed by immunoblotting with MAb 13D4 or antisera to the HA protein of influenza virus A/PR/8/34 (Genetex, Inc.).
Indirect immunofluorescence analysis.
Lab-Tek chamber slides (Fisher) containing baby hamster kidney (BHK) cells were mock infected or infected with VEE-TrD or V3526 (MOI of 1, 50 μl) at 37°C. After 1 h, complete medium was added to the wells, followed by incubation at 37°C overnight. Approximately 18 h postinfection, cells were washed with PBS and fixed in 2% paraformaldehyde in PBS for 15 min. Slides were washed in several changes of PBS and allowed to air dry. Cells were incubated at room temperature for at least 1 h with primary antibody, MAb 13D4 or 1A4A-1, diluted 1:250 in PBS plus 5% fetal bovine serum (FBS). The slides were washed in several changes of PBS and incubated at least 30 min with goat anti-mouse fluorescein isothiocyanate serum (1:80; KPL, Inc.). The slides were then washed in PBS, and each coverslip was mounted with Vectashield (Vector Labs). Slides were viewed on a Nikon Eclipse E800 microscope, and images were captured with SPOT software (Diagnostic Instruments, Inc.).
Inhibition of virus yield by MAbs.
Monolayers of BHK-21 cells were infected at an MOI of 0.1 at 37°C. One hour later, the monolayers were washed twice, and culture medium containing MAbs was added. The medium was harvested at the times indicated, and the virus yield was determined by using a plaque assay. As an alternate measure of virus particles released from the cells, viral genome equivalents were quantitated by reverse transcription-PCR (RT-PCR). RNA was extracted from a 0.25-ml sample of cell culture supernatant with TRIzol LS (Invitrogen). A 92-bp fragment representing nucleotides 7293 to 7383 of the nSP4 gene of the VEEV TrD genome (accession no. J04332) was amplified in 20-μl volumes using a R.A.P.I.D. system (Idaho Technologies). Each reaction contained 1× Invitrogen SuperScript One-Step RT-PCR with Platinum Taq PCR buffer, 25 μg of BSA/ml, 6 mM MgSO4, 0.9 nM concentrations of each primer, and 0.06 nM probe. The amplification program for the LightCycler consisted of one cycle at 50°C for 15 min and one cycle at 95°C for 5 min, followed by 45 cycles of 95°C for 1 s and 60°C for 20 s. A fluorescence reading was taken at the end of each 60°C step. Each capillary was read in channel 1 (F1) at a gain setting of 8, with data being analyzed by using LightCycler data analysis software (version 3.5.3). Sample curves were analyzed by using the “Second Derivative Maximum” with the baseline adjustment set to “Arithmetic”. The relative number of virus genomes in each sample is reported as the crossing point (Cp), indicating the number of cycles at which fluorescence rose above background levels.
Passive immunization and virus challenge.
BALB/c mice were administered 2, 20, or 50 μg of purified MAbs in 0.2 ml of PBS by i.p. injection. The animals were bled 20 h later, and the level of serum antibody in each mouse was measured by ELISA. At 25 h after antibody administration, the mice were challenged by i.p. administration of 104 PFU of VEEV TrD. Mice were observed for signs of illness daily for 2 weeks, and serum was collected using retro-orbital bleed from surviving mice at 4 weeks postchallenge.
RESULTS
Specificity of the MAbs to V3526.
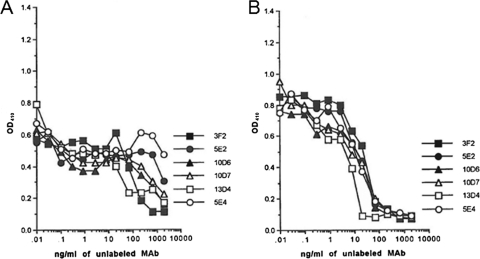
A total of 138 MAbs prepared after vaccination with V3526 were tested for reactivity with VEEV by ELISA using purified VEEV TrD or V3526 as target antigens. Six exhibited significantly increased binding to immobilized V3526 compared to VEEV TrD. These antibodies belonged to the IgG2a (MAbs 13D4, 5E2, 5E4, and 3F2) or IgG2b (MAbs 10D6 and 10D7) isotype. Competitive binding assays established that four unlabeled anti-V3526 MAbs (3F2, 13D4, 10D6, and 10D7) effectively competed with all six labeled MAbs. Fig. 1A shows the competitive binding curve for MAb 13D4 as a representative of these four MAbs. Unlabeled MAbs 5E2 and 5E4 competed with themselves, and each other but much less effectively with the other four labeled anti-V3526 MAbs, especially 10D6 and 13D4. The decreased competition seen may have been due to differences in affinity. Figure 1B shows the competitive binding curve for MAb 5E2 as a representative of these two MAbs. MAb 13D4 was the most effective at competing with the other five MAbs. Thus, these six MAbs bind to the same or closely related antigenic determinant(s).
FIG. 1.
Competitive binding curves for anti-V3526 MAbs. ELISA data obtained on V3526 virus are shown using unlabeled MAbs that were serially diluted 3-fold from 2 μg/well and biotin-labeled MAbs that were diluted to 2 ng/well. Binding curves are shown for the unlabeled MAbs against the biotin-labeled 13D4 (A) and 5E2 (B). The mean OD410 values (with no subtraction of background) obtained for duplicate wells at each tested concentration are shown.
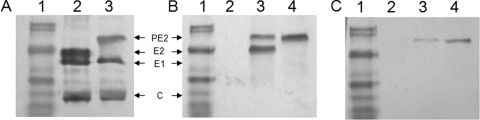
The specificity of these antibodies was investigated by probing immunoblots of V3526 and VEEV TrD viruses and lysates of virus-infected BHK-21 cells. Virions of VEEV TrD are composed of E2 and E1 envelope glycoproteins and C protein, as shown in Fig. 2A, lane 2. The cleavage site deletion in V3526 results in the incorporation of PE2 glycoprotein in the virus particle (8) and a lack of detectable E2 (Fig. 2A, lane 3). In lysates of BHK-21 cells infected with VEEV TrD, MAb 1A4A-1, which is an E2c-specific MAb, bound both PE2 and E2 (Fig. 2B, lane 3). In lysates of V3526-infected cells, 1A4A-1 bound only a single polypeptide corresponding to PE2 (Fig. 2B, lane 4). In the same lysates, MAb 13D4, one of six antibodies exhibiting preferential binding to V3526 virus, bound only PE2 of both V3526 and VEEV TrD (Fig. 2C, lanes 3 and 4). The remaining five MAbs exhibited the same specificity (data not shown). These findings demonstrated that MAb 13D4 recognized an epitope specific to the PE2 glycoprotein, presumably located in the E3 glycoprotein. Although equivalent amounts of protein were loaded onto the gels shown in Fig. 2B and 2C, the decreased amount of PE2 in VEEV TrD- versus V3526-infected cells was expected reflecting the continued furin protease processing of PE2 in TrD-infected cells. In addition, the slightly decreased mobility of PE2 of TrD compared to that of V3526 was likely due to the presence of the -RRTR- furin cleavage site which was absent from the PE2 of V3526.
FIG. 2.
V3526-specific MAbs bind PE2. Protein samples were separated by SDS-PAGE, and immunoblot analyses were performed with anti-VEEV ascites fluid or PE2-specific MAb 13D4. (A) Immunoblot of purified VEEV viruses probed with murine anti-VEEV ascites fluid. Lanes: 1, prestained molecular mass markers; 2, VEEV TrD; 3, V3526. (B) Immunoblot of lysates of VEEV-infected BHK cells probed with anti-E2C MAb 1A4A-1. Lanes: 1, prestained molecular mass markers; 2, uninfected BHK cells; 3, TrD-infected BHK cells; 4, V3526-infected BHK cells. (C) Immunoblot of VEEV-infected cells probed with MAb 13D4. Lanes: 1, prestained molecular mass markers; 2, uninfected BHK cells; 3, TrD-infected BHK cells; 4, V3526-infected BHK cells.
We have been unable to consistently detect E3 glycoprotein by immunoblotting lysates of VEEV-infected BHK-21 cells with MAbs or polyclonal sera from vaccinated mice. Therefore, to definitively identify the target of the MAbs, the sequence encoding the E3 glycoprotein of VEEV was fused to the HA gene of influenza virus A/PR/8/34 in place of the HA signal sequence in the VEEV replicon system (35). This E3-HA fusion protein was expressed in BHK-21 cells. As shown in Fig. 3A, murine antiserum to the influenza virus HA bound both the influenza virus HA protein and the E3-HA fusion protein. In the same lysates, MAb 13D4 bound only the E3-HA fusion protein (Fig. 3B). These results confirmed that the epitope bound by MAb 13D4 is located in the E3 glycoprotein. Identical results were obtained with the remaining five V3526-specific MAbs (data not shown).
FIG. 3.
MAbs specific for VEEV PE2 glycoprotein bind an epitope in the E3 glycoprotein. Lysates of BHK cells expressing influenza virus A/PR/8/34 HA or an E3-HA fusion protein were resolved by SDS-PAGE and blotted to nitrocellulose. (A) Reactivity with MAb to influenza virus HA. (B) Reactivity with MAb13D4. Lanes: 1, prestained molecular mass markers; 2, uninfected BHK cells; 3, BHK cells expressing influenza virus HA; 4, BHK cells expressing E3-HA fusion protein.
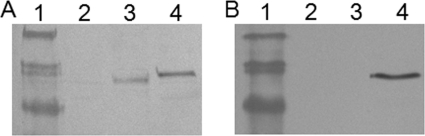
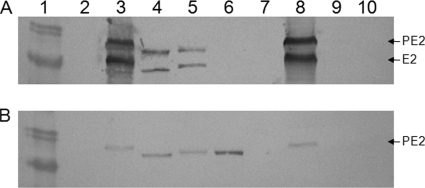
To further characterize the specificity of these MAbs, 13D4 was used to probe the lysates of BHK-21 cells infected with other subtypes of VEEV, EEEV, and WEEV. Lysates of virus-infected cells served as the source of PE2 because cleavage deletion mutants were not available for all viruses. As shown in Fig. 4, E2c-specific MAb 1A4A-1 bound to denatured and reduced E2 and PE2 proteins of VEEV subtypes IA/B, IC, and ID (Fig. 4, lanes 3, 4, 5, and 8) but failed to bind either polypeptide in lysates of cells infected with subtype IE VEEV 68U201, Mucambo virus (previously classified as VEEV subtype IIIA), EEEV, or WEEV. MAb 13D4 was able to bind the PE2 protein of VEEV subtypes IA/B (TrD), IC, ID, and IE (Fig. 4B, lanes 3 to 6 and 8). These results indicate that although the VEEV IE strain 68U201 has diverged from the other subtype I viruses with respect to the E2c-epitope recognized by 1A4A-1, the epitope bound by MAb 13D4 in E3 appeared to be conserved. In addition, 13D4 did not bind analogous targets in BHK-21 cells infected with Mucambo virus, EEEV, or WEEV (Fig. 4B, lanes 7, 9, and 10).
FIG. 4.
Reactivity of lysates of Alphavirus virus-infected BHK cells with MAbs specific for E3 and E2. Infected cell lysates were subjected to SDS-PAGE and electroblotted to nitrocellulose. (A) Lysates probed with E2c-specific MAb 1A4A-1. (B) The same lysates reacted with E3-specific MAb 13D4. Lanes: 1, prestained molecular mass marker; 2, uninfected BHK cells; 3, VEEV subtype IA/B (TrD); 4, VEEV subtype IC; 5, VEEV subtype ID; 6, VEEV subtype IE; 7, Mucambo virus; 8, TrD virus; 9, EEEV; 10, WEEV.
In vitro neutralization of infectivity by E3-specific MAbs.
In order to determine the effect of anti-E3 antibody binding on the infectivity of the virus, PRNTs were performed with all of the E3 specific MAbs. As reported previously (25), MAb 1A4A-1 neutralized VEEV TrD. Low concentrations of MAb 1A4A-1 also neutralized V3526 (Table 1). All six anti-E3 MAbs neutralized V3526 in vitro to various extents. However, 13D4 was the most efficient, requiring at least 7-fold less than the other MAbs. When tested against VEEV TrD, only 13D4 appeared to exhibit plaque-reducing ability at a concentration of ≥10 μg/ml. We subsequently found that if monolayers were washed twice with PBS before the addition of the first agarose overlay, plaque formation by VEEV TrD was not inhibited by 13D4 (data not shown). This indicated that the apparent neutralization of TrD VEEV plaque formation by MAb 13D4 was due to postinfection inhibition evident only when high concentrations of antibody remained in the agarose overlay during the course of the plaque assay. In contrast, washing of the monolayers prior to addition of the agarose overlay had no effect on the reduction of plaque formation by V3526, demonstrating that infectivity of V3526 was neutralized by preincubation with MAb 13D4.
TABLE 1.
Neutralization of VEEV by anti-E3 MAb
| Antibody | Antibody concn (μg/ml)a |
|
|---|---|---|
| V3526 | TrD | |
| 3F2 | 0.2 | >10 |
| 5E2 | 0.6 | >10 |
| 10D6 | 0.3 | >10 |
| 10D7 | 0.3 | >10 |
| 13D4 | 0.04 | 10 |
| 5E4 | 1 | >10 |
| 1A4A-1 | 0.001 | 0.02 |
| IgG2a and IgG2bb | >10 | >10 |
That is, the antibody concentration resulting in 80% plaque reduction.
Isotype controls were individually tested, and all produced the same results.
Inhibition of virus yield.
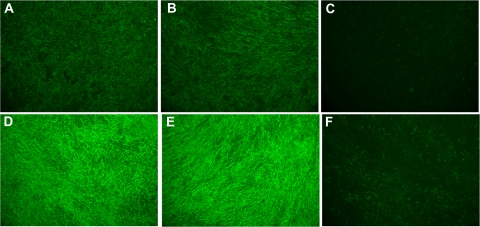
Immunofluorescence analysis of TrD-infected BHK-21 cells with Mab13D4 demonstrated that the E3 protein, either in its free form or still in the form of PE2, was present on the surfaces of infected cells (Fig. 5). To determine whether anti-E3 antibody would impact progeny virus production, we measured the effect of 13D4 on the yield of VEEV TrD in cell culture. BHK-21 cells were infected with VEEV TrD at an MOI of 0.1 at 37°C to allow for binding and internalization of the virus. One hour later, medium was added containing 10 μg of purified 13D4/ml, 10 μg of E2-specific MAb 1A4A-1/ml, or an irrelevant MAb to Ebola virus glycoprotein. The supernatants were collected at increasing times after infection, and progeny virus was quantitated by plaque assay on Vero cells.
FIG. 5.
The E3 protein is present on the surface of VEEV-infected cells. Indirect immunofluorescence assay performed with MAb 13D41 (A to C) or MAb 1A4A-1 (D to F) on BHK cells infected with VEE TrD (A and D), V3526 (B and E), or mock infected (C and F).
As shown in Table 2, VEEV TrD reached an extracellular titer exceeding 108 PFU/ml by 24 h after a low-multiplicity infection of BHK-21 cells. The presence of a MAb against the glycoprotein of Ebola virus had no effect on the production of progeny VEEV (data not shown). When the medium contained 10 μg of MAb 13D4/ml, the extracellular virus titer was reduced to ca. 105 PFU/ml, a 103-fold decrease. In repeated assays, equivalent levels of inhibition were evident at MAb 13D4 concentrations as low as 0.5 μg/ml (data not shown). The remaining E3-specific MAbs consistently inhibited virus production by 100-fold (not shown). Including MAb 1A4A-1, which neutralizes viral infectivity, also reduced virus production to 105 PFU/ml. Therefore, although MAb 13D4 exhibited little plaque-reducing activity against the parental VEEV TrD compared to MAb 1A4A-1 (Table 1), MAb 13D4 was as effective as MAb 1A4A-1 in reducing production of progeny virus. Similar results were obtained when the cells were infected at an MOI of 10, suggesting that the reduced yield of virus was due to inhibition of virus formation or release rather than an inability to disseminate the infection throughout the cell monolayer.
TABLE 2.
Inhibition of virus production by MAb to VEEV glycoproteins
| Antibody and time postinfection (h) | TrD VEEV (IA/B) |
VEEV subtypes |
||||||
|---|---|---|---|---|---|---|---|---|
| MAb concn (μg/ml) |
PFU/ml | Cpa | MAb 13D4 concn (μg/ml) | PFU/ml |
||||
| 13D4 | 1A4A-1 | IC | ID | IE | ||||
| No antibody | ||||||||
| 0 | 102 | 28.84 | 3.4 × 102 | 3.6 × 102 | 5 × 102 | |||
| 24 | 7 × 108 | 9.97 | 3.6 × 109 | 5 × 108 | 2 × 109 | |||
| 13D4 | ||||||||
| 0 | 10 | <102 | 29.79 | 10 | 2.7 × 102 | 4 × 102 | 5 × 102 | |
| 24 | 10 | 4 × 104 | 26.59 | 10 | 1.4 × 106 | 1.2 × 108 | 2.3 × 105 | |
| 1A4A-1 | ||||||||
| 0 | 10 | 102 | 30.35 | NA | NA | NA | NA | |
| 24 | 10 | 4 × 104 | 28.98 | NA | NA | NA | NA | |
Cp, crossing point.
The observation that MAb 13D4 decreased the yield of infectious virus did not exclude the possibility that noninfectious particles were produced in the presence of the antibody. Therefore, portions of the supernatant collected from infected BHK cells incubated with 13D4 or 1A4A-1 were analyzed by quantitative RT-PCR (qPCR) (Table 2). In the absence of antibody or in the presence of an anti-Ebola virus MAb (data not shown), the decreasing Cp values reflected the rising titer of virus in the culture supernatant. The decrease in extracellular titers in cultures incubated with MAbs 13D4 or 1A4A-1 was reflected by increased Cp values, confirming that the decrease in extracellular virus was not due to neutralization of extracellular virus by the MAbs or production of noninfectious viral particles. Taken together, these results demonstrate that the decrease in virus production mediated by MAb 13D4 was due to antibody-mediated inhibition of morphogenesis or release of infectious progeny.
As indicated previously (Fig. 4B), MAb 13D4 bound the PE2 glycoprotein of all of the VEEV subtype I viruses when analyzed by immunoblotting. Coincident with the specificity for the PE2 proteins of subtype I VEEVs, as shown in Fig. 4, MAb 13D4 also significantly inhibited the production of virus from BHK-21 cells infected with subtype IC (by 103) and IE (by 104) viruses and had a modest effect on the production of 1D virus (Table 2).
In vivo activity of anti-E3 antibody.
The dramatic inhibition of virus production from infected cells by anti-E3 antibody suggested that MAb 13D4 might impact the course of disease in an infected host. Therefore, BALB/c mice were passively immunized i.p. with purified MAb 1 day before i.p. challenge with 104 PFU of VEEV TrD. ELISA measurements of serum antibody demonstrated that all mice were successfully passively immunized, and the geometric mean titers for each group are indicated in Table 3. Passive transfer of 20 or 50 μg of 13D4 to BALB/c mice protected the mice from lethal challenge (Table 3). The other E3 MAbs, all of which exhibited no plaque-reducing activity against TrD virus at 10 μg/ml and were less effective at reducing the number of progeny viruses, provided much less protection to the recipient mice, even when 50 μg of antibody was administered before challenge. However, in each case, the mean time to death was extended significantly (P < 0.001) compared to the control mice. MAb 1A4A-1 protected BALB/c mice as previously reported (33), and irrelevant isotype-matched MAb at either 20- or 50-μg doses failed to provide protection. Serum collected from MAb 13D4 passively immunized mice surviving 1 month after challenge contained high titers of VEEV-specific antibodies of all four IgG isotypes. In contrast, mice passively immunized with 50 μg of MAb 1A4A-1 showed no serological evidence of infection (data not shown). These results indicate that anti-E3 MAbs did not protect mice against infection but suggests that they moderated disease progression until the adaptive response was able to resolve the infection.
TABLE 3.
Protection of BALB/c mice by passive transfer of MAbs to VEEV glycoproteins
| Antibody | Protection of BALB/c mice (GMT)a at an antibody concn of: |
MDD (P)b | ||
|---|---|---|---|---|
| 2 μg | 20 μg | 50 μg | ||
| 13D4 | 1/9 (ND) | 9/9 (5,432); 7/7 (2,400) | 5/5 (8,778) | NA |
| 5E2 | 1/9 (2,208) | 0/5 (1,949) | 10.56 (0.0002) | |
| 5E4 | 1/9 (2,208) | 6/6 (1,949); 1/5 (2,208) | 11.0 (0.006) | |
| 10D6 | 1/9 (1,808) | 1/5 (5,653) | 9.78 (0.001) | |
| 10D7 | 2/9 (1,998) | 2/5 (6,400) | 11.89 (0.004) | |
| 3F2 | 0/9 (ND) | 8/9 (9,897); 0/8 (1,258); 0/5 (1,596) | 1/5 (1,600) | NA |
| 1A4A-1 | 13/13 | 5/5 (2,441) | NA | |
| IgG2a and IgG2bc | 0/18 (<100) | 0/5 (<100) | 7.0 | |
Protection is expressed as the number of protected mice/number of mice tested. The geometric mean titer (GMT) prior to challenge is indicated in parentheses. ND, not determined.
The mean day of death (MDD) for each antibody was evaluated for significant differences from the results obtained with irrelevant isotype-matched antibody. NA, not applicable.
Isotype-matched irrelevant antibody.
DISCUSSION
The alphavirus E3 glycoprotein is a multifunctional component of the process of synthesis and maturation of the viral surface glycoprotein spikes. In addition to acting as a signal to initiate translocation of viral glycoproteins across the membranes of the rough endoplasmic reticulum, E3 also promotes the heterodimerization and intracellular processing of E1 and PE2 glycoproteins (23, 46). Furin cleavage of PE2 into E2 and E3 activates the spikes to a metastable state capable of initiating infection (52). By analogy with the prM protein of dengue Flavivirus (51), furin cleavage of PE2 may begin after transit of an acidic late component of the Golgi body, where E3 is thought to suppress the acid pH-triggered activation of glycoprotein E1 fusion capability. Although the pr fragment produced by furin cleavage of prM of dengue is released after return to neutral pH, in the case of alphaviruses E3 may be released (2, 49) or retained on the mature virus particles (32).
Although elimination of the furin cleavage site from PE2 in VEEV is a lethal mutation (8), pseudorevertant viruses were rescued after transfection of transcripts of cleavage deletion genomic cDNA clones due to second-site suppressor mutations in the E1, E2, or E3 glycoprotein genes (17, 44, 47). The stability of the cleavage deletion mutation (24) and attenuated phenotype of the virus prompted the evaluation of V3526 as a vaccine for animals and humans (34, 37, 52, 53). In the course of preclinical evaluation of V3526 as a live vaccine, a series of MAbs were generated to further characterize the immune response elicited by vaccination with V3526.
The MAbs described in this report bound a previously unrecognized epitope on the E3 glycoprotein. Reconstructions of a cleavage-site deletion mutant of Sindbis virus revealed that the E3 portion of the PE2 molecule in the virus forms a prominent lobe on the distal portion of the glycoprotein spike (32). The potent neutralization of V3526 infectivity by MAb 13D4 was likely due to interference with cell surface binding or penetration as previously reported for the E2c-specific MAbs (38).
The furin cleavage of alphavirus PE2 glycoprotein begins in the trans-Golgi network (29). The binding of MAb 13D4 to wild-type virus-infected cells indicates that E3 is present on the cell surface, but we were unable to determine whether the target is E3 or residual PE2. The observation that furin cycles between the Golgi body and the cell surface (30, 31) provides for the possibility that some processing occurs after PE2 appears on the plasma membrane. If true, this suggests several possible mechanisms by which anti-E3 antibodies may inhibit virus production. First, MAb 13D4 bound to PE2 might interfere with furin cleavage (10, 11). However, the incorporation of PE2 into nascent Alphavirus spikes does not prevent the budding of particles (8, 40), and the qPCR analysis indicates that 13D4 reduces particle formation to very low levels, as shown in Table 2. Alternatively, antibody binding of PE2 on the cell surface may inhibit formation of the glycoprotein spike matrix and coalescence of the envelope required for viral budding. Finally, if MAb 13D4 is bound to E3 after its cleavage from PE2, the potent inhibition of wild-type virus production by 13D4 would suggest the existence of an undescribed role for E3 in a critical late event preceding release of the virion from the cell. Efforts are ongoing to identify the nature of the E3 entity present on the cell surface.
Protection against lethal Alphavirus challenge by passive immunization with antibodies that do not inhibit plaque formation was demonstrated previously (41, 50). The ability of the six E3-specific MAbs described here to inhibit plaque formation by V3526 virus is not directly relevant to protection against wild-type viral challenge. However, it does correspond to the level of protection afforded by passive immunization. The expanded repertoire of antibody isotypes detected after challenge indicates that a significant level of viral replication occurs in passively immunized mice. These observations indicate anti-E3 MAb likely protects animals against wild-type VEEV by inhibiting the amplification of the challenge virus, subsequently moderating viremia and the progression of disease until the adaptive immune response is capable of resolving the infection. In contrast, the E2c MAb provided apparent sterile immunity when passively transferred to mice, based on the lack of de novo antibody responses following challenge.
This study is the first in which the E3 protein has been demonstrated to contain protective epitopes. These findings are directly relevant to ongoing efforts toward developing licensable equine encephalitis virus vaccines and therapeutics. TC-83 is a live VEEV vaccine currently available for limited use in humans. The vaccine has a variable reactogenicity rate but also fails to induce a detectable serum neutralizing antibody response in ca. 20% of recipients. Because a neutralizing antibody response is currently accepted as the surrogate marker of protection against laboratory infection by VEEV, TC-83 nonresponders receive subsequent vaccinations with C-84 vaccine, an inactivated vaccine also available for use in at-risk laboratory investigators. However, C-84 is prepared by formalin inactivation of TC-83 and therefore, is unlikely to contain detectable E3 glycoprotein. Although the lack of E3 is unlikely to be responsible for the failure rate, an inactivated vaccine developed from a cleavage mutant virus, such as V3526, might be expected to elicit a broadened antibody response and provide an additional level of protection due to antibody to the E3 epitope. In addition, development of inactivated vaccines from cleavage-site mutants of WEEV and EEEV may likewise increase their effectiveness, since we found that an anti-E3 MAb specific for the WEEV E3 glycoprotein also affords protection in mice (unpublished observation). In addition to vaccine considerations, MAbs to this protective epitope on the E3 glycoprotein could be a promising component of an antibody-based therapeutic for alphaviruses.
Acknowledgments
We acknowledge Shawn Guest for his assistance in the preparation of the hybridomas. Housing and care of animals was carried out in accordance with the American Association for Accreditation of Laboratory Animals Animal Care standards.
The opinions, interpretations, conclusions, and recommendations are those of the author and not necessarily endorsed by the U.S. Army or the Department of Defense.
Footnotes
Published ahead of print on 6 October 2010.
REFERENCES
- 1.Anishchenko, M., R. A. Bowen, S. Paessler, L. Austgen, I. P. Greene, and S. C. Weaver. 2006. Venezuelan encephalitis emergence mediated by a phylogenetically predicted viral mutation. Proc. Natl. Acad. Sci. U. S. A. 103:4994-4999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bell, J. R., C. M. Rice, M. W. Hunkapiller, and J. H. Strauss. 1982. The N terminus of PE2 in Sindbis virus-infected cells. Virology 119:255-267. [DOI] [PubMed] [Google Scholar]
- 3.Berglund, P., M. Sjobereg, H. Garoff, G. Atkins, B. Sheahan and Pl. Liljestrom. 1993. Semliki Forest virus expression system: production of conditionally infectious recombinant particles. Biotechnology 11:916-920. [DOI] [PubMed] [Google Scholar]
- 4.Bianchi, T. I., G. Aviles, T. P. Monath, and M. S. Sabattini. 1993. Western equine encephalomyelitis: virulence markers and their epidemiologic significance. Am. J. Trop. Med. Hyg. 49:322-328. [DOI] [PubMed] [Google Scholar]
- 5.Charles, P. C., K. W. Brown, N. L. Davis, M. K. Hart, and R. E. Johnston. 1997. Mucosal immunity induced by parenteral immunization with a live attenuated Venezuelan equine encephalitis virus vaccine candidate. Virology 228:153-160. [DOI] [PubMed] [Google Scholar]
- 6.Cheng, R. H., R. J. Kuhn, N. H. Olson, M. G. Rossmann, H. K. Choi, T. J. Smith, and T. S. Baker. 1995. Nucleocapsid and glycoprotein organization in an enveloped virus. Cell 80:621-630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Dalrymple, J. M., S. Schlesinger, and P. K. Russell. 1976. Antigenic characterization of two Sindbis envelope glycoproteins separated by isoelectric focusing. Virology 69:93-103. [DOI] [PubMed] [Google Scholar]
- 8.Davis, N. L., K. W. Brown, G. F. Greenwald, A. J. Zajac, V. L. Zacny, J. F. Smith, and R. E. Johnston. 1995. Attenuated mutants of Venezuelan equine encephalitis virus containing lethal mutations in the PE2 cleavage signal combined with a second-site suppressor mutation in E1. Virology 212:102-110. [DOI] [PubMed] [Google Scholar]
- 9.Fine, D. L., B. A. Roberts, M. L. Teehee, S. J. Terpening, C. L. Kelly, J. L. Raetz, D. C. Baker, A. M. Powers, and R. A. Bowen. 2007. Venezuelan equine encephalitis virus vaccine candidate (V3526) safety, immunogenicity and efficacy in horses. Vaccine 25:1868-1876. [DOI] [PubMed] [Google Scholar]
- 10.Forsell, K., G. Griffiths, and H. Garoff. 1996. Preformed cytoplasmic nucleocapsids are not necessary for alphavirus budding. EMBO J. 15:6495-6505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Forsell, K., L. Xing, T. Kozlovska, R. H. Cheng, and H. Garoff. 2000. Membrane proteins organize a symmetrical virus. EMBO J. 19:5081-5091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Garoff, H., D. Huylebroeck, A. Robinson, U. Tillman, and P. Liljestrom. 1990. The signal sequence of the p62 protein of Semliki Forest virus is involved in initiation but not in completing chain translocation. J. Cell Biol. 111:867-876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Garoff, H., K. Simons, and O. Renkonen. 1974. Isolation and characterization of the membrane proteins of Semliki Forest virus. Virology 61:493-504. [DOI] [PubMed] [Google Scholar]
- 14.Hart, M. K., K. Caswell-Stephan, R. Bakken, R. Tammariello, W. Pratt, N. Davis, R. E. Johnston, J. Smith, and K. Steele. 2000. Improved mucosal protection against Venezuelan equine encephalitis virus is induced by the molecularly defined, live-attenuated V3526 vaccine candidate. Vaccine 18:3067-3075. [DOI] [PubMed] [Google Scholar]
- 15.Hart, M. K., C. Lind, R. Bakken, M. Robertson, R. Tammariello, and G. V. Ludwig. 2001. Onset and duration of protective immunity to IA/IB and IE strains of Venezuelan equine encephalitis virus in vaccinated mice. Vaccine 20:616-622. [DOI] [PubMed] [Google Scholar]
- 16.Hart, M. K., W. Pratt, F. Panelo, R. Tammariello, and M. Dertzbaugh. 1997. Venezuelan equine encephalitis virus vaccines induce mucosal IgA responses and protection from airborne infection in BALB/c, but not C3H/HeN mice. Vaccine 15:363-369. [DOI] [PubMed] [Google Scholar]
- 17.Heidner, H. W., K. L. McKnight, N. L. Davis, and R. E. Johnston. 1994. Lethality of PE2 incorporation into Sindbis virus can be suppressed by second-site mutations in E3 and E2. J. Virol. 68:2683-2692. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hunt, A. R., and J. T. Roehrig. 1995. Localization of a protective epitope on a Venezuelan equine encephalomyelitis (VEE) virus peptide that protects mice from both epizootic and enzootic VEE virus challenge and is immunogenic in horses. Vaccine 13:281-288. [DOI] [PubMed] [Google Scholar]
- 19.Hunt, A. R., W. A. Short, A. J. Johnson, R. A. Bolin, and J. T. Roehrig. 1991. Synthetic peptides of the E2 glycoprotein of Venezuelan equine encephalomyelitis virus. II. Antibody to the amino terminus protects animals by limiting viral replication. Virology 185:281-290. [DOI] [PubMed] [Google Scholar]
- 20.Johnson, B. J., J. R. Brubaker, J. T. Roehrig, and D. W. Trent. 1990. Variants of Venezuelan equine encephalitis virus that resist neutralization define a domain of the E2 glycoprotein. Virology 177:676-683. [DOI] [PubMed] [Google Scholar]
- 21.Levy-Mintz, P., and M. Kielian. 1991. Mutagenesis of the putative fusion domain of the Semliki Forest virus spike protein. J. Virol. 65:4292-4300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Liljestrom, P., and H. Garoff. 1991. Internally located cleavable signal sequences direct the formation of Semliki Forest virus membrane proteins from a polyprotein precursor. J. Virol. 65:147-154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lobigs, M., X. Zhao, and H. Garoff. 1990. Function of SFV E3 peptide in virus assembly: replacement of E3 with an artificial signal peptide abolished spike heterodimerization and surface expression of E1. J. Virol. 64:4346-4355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ludwig, G. V., M. J. Turell, P. Vogel, J. P. Kondig, W. K. Kell, J. F. Smith, and W. D. Pratt. 2001. Comparative neurovirulence of attenuated and non-attenuated strains of Venezuelan equine encephalitis virus in mice. Am. J. Trop. Med. Hyg. 64:49-55. [DOI] [PubMed] [Google Scholar]
- 25.Mathews, J. H., and J. T. Roehrig. 1982. Determination of the protective epitopes on the glycoproteins of Venezuelan equine encephalomyelitis virus by passive transfer of monoclonal antibodies. J. Immunol. 129:2763-2767. [PubMed] [Google Scholar]
- 26.Mayne, J. T., C. M. Rice, E. G. Strauss, M. W. Hunkapiller, and J. H. Strauss. 1984. Biochemical studies of the maturation of the small Sindbis virus glycoprotein E3. Virology 134:338-357. [DOI] [PubMed] [Google Scholar]
- 27.Melancon, P., and H. Garoff. 1987. Processing of the Semliki Forest virus structural polyprotein: role of the capsid protease. J. Virol. 61:1301-1309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Mitchell, C. J., M. L. Niebylski, G. C. Smith, N. Karabatsos, D. Martin, J. P. Mutebi, G. B. Craig, Jr., and M. J. Mahler. 1992. Isolation of eastern equine encephalitis virus from Aedes albopictus in Florida. Science 257:526-527. [DOI] [PubMed] [Google Scholar]
- 29.Moehring, J. M., N. M. Inocencio, B. J. Robertson, and T. J. Moehring. 1993. Expression of mouse furin in a Chinese hamster cell resistant to Pseudomonas exotoxin A and viruses complements the genetic lesion. J. Biol. Chem. 268:2590-2594. [PubMed] [Google Scholar]
- 30.Molloy, S. S., L. Thomas, J. K. VanSlyke, P. E. Stenberg, and G. Thomas. 1994. Intracellular trafficking and activation of the furin proprotein convertase: localization to the TGN and recycling from the cell surface. EMBO J. 13:18-33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Nakayama, K. 1997. Furin: a mammalian subtilisin/Kex2p-like endoprotease involved in processing of a wide variety of precursor proteins. Biochem. J. 327(Pt. 3):625-635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Paredes, A. M., H. Heidner, P. Thuman-Commike, B. V. Prasad, R. E. Johnston, and W. Chiu. 1998. Structural localization of the E3 glycoprotein in attenuated Sindbis virus mutants. J. Virol. 72:1534-1541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Phillpotts, R. J., L. D. Jones, and S. C. Howard. 2002. Monoclonal antibody protects mice against infection and disease when given either before or up to 24 h after airborne challenge with virulent Venezuelan equine encephalitis virus. Vaccine 20:1497-1504. [DOI] [PubMed] [Google Scholar]
- 34.Pratt, W. D., N. L. Davis, R. E. Johnston, and J. F. Smith. 2003. Genetically engineered, live attenuated vaccines for Venezuelan equine encephalitis: testing in animal models. Vaccine 21:3854-3862. [DOI] [PubMed] [Google Scholar]
- 35.Pushko, P., M. Parker, G. V. Ludwig, N. L. Davis, R. E. Johnston, and J. F. Smith. 1997. Replicon-helper systems from attenuated Venezuelan equine encephalitis virus: expression of heterologous genes in vitro and immunization against heterologous pathogens in vivo. Virology 239:389-401. [DOI] [PubMed] [Google Scholar]
- 36.Reed, D. S., T. Larsen, L. J. Sullivan, C. M. Lind, M. G. Lackemeyer, W. D. Pratt, and M. D. Parker. 2005. Aerosol exposure to western equine encephalitis virus causes fever and encephalitis in cynomolgus macaques. J. Infect. Dis. 192:1173-1182. [DOI] [PubMed] [Google Scholar]
- 37.Reed, D. S., C. M. Lind, M. G. Lackemeyer, L. J. Sullivan, W. D. Pratt, and M. D. Parker. 2005. Genetically engineered, live, attenuated vaccines protect nonhuman primates against aerosol challenge with a virulent IE strain of Venezuelan equine encephalitis virus. Vaccine 23:3139-3147. [DOI] [PubMed] [Google Scholar]
- 38.Roehrig, J. T., A. R. Hunt, R. M. Kinney, and J. H. Mathews. 1988. In vitro mechanisms of monoclonal antibody neutralization of alphaviruses. Virology 165:66-73. [DOI] [PubMed] [Google Scholar]
- 39.Roehrig, J. T., and J. H. Mathews. 1985. The neutralization site on the E2 glycoprotein of Venezuelan equine encephalomyelitis (TC-83) virus is composed of multiple conformationally stable epitopes. Virology 142:347-356. [DOI] [PubMed] [Google Scholar]
- 40.Salminen, A., J. M. Wahlberg, M. Lobigs, P. Liljestrom, and H. Garoff. 1992. Membrane fusion process of Semliki Forest virus. II. Cleavage-dependent reorganization of the spike protein complex controls virus entry. J. Cell Biol. 116:349-357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Schmaljohn, A. L., E. D. Johnson, J. M. Dalrymple, and G. A. Cole. 1982. Non-neutralizing monoclonal antibodies can prevent lethal alphavirus encephalitis. Nature 297:70-72. [DOI] [PubMed] [Google Scholar]
- 42.Schmaljohn, A. L., K. M. Kokubun, and G. A. Cole. 1983. Protective monoclonal antibodies define maturational and pH-dependent antigenic changes in Sindbis virus E1 glycoprotein. Virology 130:144-154. [DOI] [PubMed] [Google Scholar]
- 43.Smit, J. M., R. Bittman, and J. Wilschut. 1999. Low-pH-dependent fusion of Sindbis virus with receptor-free cholesterol- and sphingolipid-containing liposomes. J. Virol. 73:8476-8484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Smit, J. M., W. B. Klimstra, K. D. Ryman, R. Bittman, R. E. Johnston, and J. Wilschut. 2001. PE2 cleavage mutants of Sindbis virus: correlation between viral infectivity and pH-dependent membrane fusion activation of the spike heterodimer. J. Virol. 75:11196-11204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Stiles, B. G., B. C. Lidgerding, F. W. Sexton, and S. B. Guest. 1991. Production and characterization of monoclonal antibodies against Naja naja atra cobrotoxin. Toxicon 29:1195-1204. [DOI] [PubMed] [Google Scholar]
- 46.Syvaoja, P., J. Peranen, M. Suomalainen, S. Keranen, and L. Kaariainen. 1990. A single amino acid change in E3 of ts1 mutant inhibits the intracellular transport of SFV envelope protein complex. Virology 179:658-666. [DOI] [PubMed] [Google Scholar]
- 47.Tubulekas, L., and P. Liljestrom. 1998. Suppressors of cleavage-site mutations in the p62 envelope protein of Semliki Forest virus reveal dynamics in spike structure and function. J. Virol. 72:2825-2831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Urban, A., S. Neukirchen, and K. E. Jaeger. 1997. A rapid and efficient method for site-directed mutagenesis using one-step overlap extension PCR. Nucleic Acids Res. 25:2227-2228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Welch, W. J., and B. M. Sefton. 1979. Two small virus-specific polypeptides are produced during infection with Sindbis virus. J. Virol. 29:1186-1195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Wust, C. J., J. A. Nicholas, D. Fredin, D. C. Dodd, R. J. Brideau, M. E. Levely, and A. Brown. 1989. Monoclonal antibodies that cross-react with the E1 glycoprotein of different alphavirus serogroups: characterization including passive protection in vivo. Virus Res. 13:101-112. [DOI] [PubMed] [Google Scholar]
- 51.Yu, I. M., W. Zhang, H. A. Holdaway, L. Li, V. A. Kostyuchenko, P. R. Chipman, R. J. Kuhn, M. G. Rossmann, and J. Chen. 2008. Structure of the immature dengue virus at low pH primes proteolytic maturation. Science 319:1834-1837. [DOI] [PubMed] [Google Scholar]
- 52.Zhang, X., M. Fugere, R. Day, and M. Kielian. 2003. Furin processing and proteolytic activation of Semliki Forest virus. J. Virol. 77:2981-2989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Zhang, X., and M. Kielian. 2004. Mutations that promote furin-independent growth of Semliki Forest virus affect p62-E1 interactions and membrane fusion. Virology 327:287-296. [DOI] [PubMed] [Google Scholar]