Abstract
Background
The German Standing Committee on Vaccination recommends annual vaccination for persons in high-risk groups in order to lower the disease burden associated with seasonal influenza. The stated target is 75% vaccination coverage of people over age 60 by the year 2010. We present statistics based on billing data of the German associations of statutory health insurance physicians regarding vaccination coverage for influenza in the three seasons from 2004/05 to 2006/07.
Methods
We analyzed anonymous data from 14 of the 17 associations of statutory health insurance physicians in Germany. The study population consisted of all persons covered by statutory health insurance in the geographical areas under study (61.5 million persons, or 86% of the total population of these areas). Vaccination coverage was calculated as the number of vaccinated persons divided by the number of persons covered by statutory health insurance.
Results
The influenza vaccination coverage of the overall study population was 19% in 2004/05, 22% in 2005/06, and 21% in 2006/07. The coverage of persons over age 60 was 45% in 2004/05, 50% in 2005/06, and 49% in 2006/07 and was higher in areas that were formerly part of East Germany than in the rest of the country. More than a third of all vaccinated persons were vaccinated in all three seasons, as were almost half of the vaccinated persons over age 60.
Conclusion
There was no secular increase in influenza vaccination coverage over the period 2005/06 to 2006/07. The stated target of 75% vaccination coverage for persons over age 60 by the year 2010 would thus seem to represent a major challenge for all persons involved. The analysis of data of the associations of statutory health insurance physicians enables continuous monitoring of influenza vaccination coverage.
Influenza is a viral disease that is transmitted mainly via large-droplets. The pandemic potential of influenza viruses was illustrated by the subtype influenza A (H1N1), which occurred de novo in 2009. The seasonal influenza wave usually starts in January or February and lasts for about 8 to 10 weeks. Severe disease courses and complications usually affect elderly patients or persons with chronic underlying conditions (1).
Since the German Protection against Infection Act (Infektionsschutzgesetz, IfSG) was introduced in 2001, an average of 8400 cases per year of confirmed influenza virus were reported to the Robert Koch Institute (RKI) in the context of the law on notifiable diseases (2), but it can be assumed that the actual number of influenza patients is much higher than that (3). To lower the overall disease burden due to influenza, the German Standing Vaccination Committee (Ständige Impfkommission, STIKO) therefore recommends annual vaccination against the currently circulating influenza strain for persons older than 60 and particular risk groups. These include persons with an increased health risk owing to underlying conditions, medical personnel, persons in institutions with comprehensive contacts with the public, or persons who might act as possible sources of infection for other, unvaccinated individuals under their care who are at increased risk of infection and developing severe disease (4). The RKI and Paul Ehrlich Institute recommend the months of October and November for the vaccination campaigns (5). Germany is following the recommendations of the World Health Organization (WHO), which aim to achieve vaccination coverage of 50% of the elderly population by 2006 and 75% by 2010 (6).
Influenza vaccinations undertaken by doctors are not centrally captured. The main method to determine the vaccination rate for influenza that has been available thus far are cross sectional telephone surveys, whose results are published regularly (7, 8). Compared with France, Italy, Spain, and the United Kingdom, Germany had the lowest vaccination rate (50.2%) in people older than 65 in the 2006/07 influenza season (9). The rates for the four other countries were between 60.5% and 69.5%. In a comparison with 10 European countries, Germany reached the 6th place for those older than 65 in the 2007/08 influenza season (10). Further, the number of doses of influenza vaccine is used to estimate vaccination rates (11). Thus far it is not exactly known how many people are vaccinated against influenza every year and how many people are vaccinated at irregular intervals. The latter are part of a target group for a recall system, which doctors can use to remind their patients of the required vaccinations and thus increase influenza vaccination rates (12).
All vaccinations conducted in members of statutory health insurance schemes are billed to the associations of statutory health insurance physicians (Kassenärztliche Vereinigungen, KV). The associations’ data therefore represent a hitherto unused data source that can be used to determine age specific vaccination rates. This is relevant not only for influenza vaccination but for all other types of vaccinations that are recommended by the Standing Vaccination Committee.
Since 2004, the German associations of statutory health insurance physicians have been reporting pseudonymized data on billed vaccinations to the Robert Koch-Institute in the context of a sentinel project.
Our secondary analysis of these data aims to determine vaccination rates in the population of persons older than 60 in the areas covered by 14 (of 17) associations of statutory health insurance physicians for the seasons 2004/05, 2005/06, and 2006/07. We investigated in which months vaccine uptake is highest and which proportions of people are regularly vaccinated against influenza every year.
Method
The collected data are part of the quarterly listing of services provided by physicians in private practice and hospital doctors authorized by the associations for statutory health insurance physicians for the purpose of billing the statutory health insurers. The associations reported data on billed influenza vaccinations to the Robert Koch Institute. The data are pseudonymized but reported on a case by case basis, so it is possible to assign different vaccinations to the same recipient. The data are subjected to structural and substantial checking, and a plausibility check for completeness is undertaken. The methods of the KV sentinel projects, including quality assurance of the data and data protection, have been described in detail elsewhere (13).
Complete billing data for 2004 to 2007 are available for 14 of the 17 associations of statutory health insurance physicians: Bavaria, Berlin, Brandenburg, Bremen, Hamburg, Mecklenburg–Western Pomerania, Lower Saxony, North Rhine, Saarland, Saxony, Saxony-Anhalt, Schleswig-Holstein, Thuringia, and Westphalia-Lippe. Since North Rhine–Westphalia has two associations (North Rhine and Westphalia-Lippe), the 14 areas represent 13 federal states.
The study population comprises all persons with membership of statutory health insurance schemes who live in the 14 areas (some 61.5 million) (14). This accounts for about 86% of the total populations living in those areas. Someone is counted as a vaccinated person if they have received at least one influenza vaccination per season. An influenza season is defined as the time period from 1 July of every year to 30 June of the following year. The vaccination rates are calculated from the numbers of vaccinated persons in the respective populations.
Results
Influenza vaccination rates in the seasons 2004/05, 2005/06, and 2006/07
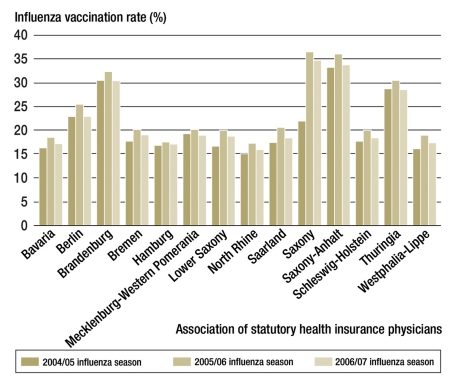
In the areas included in the study, a total of 9 942 583 persons were vaccinated against influenza in the 2004/05 influenza season, compared with 11 707 327 persons in 2005/06 and 10 813 618 in 2006/07. The influenza vaccination rate in the population rose from 19% (2004/05) to 22% (2005/06) and then fell slightly to 21% (2006/07). The rates in the individual areas differed markedly (figure 1); they ranged from 15% for North Rhine for 2004/05 to 36% for Saxony and Saxony-Anhalt in 2005/06. The vaccination rate peaked in 2005/06 in all areas under study. The biggest increase in the vaccination rate was observed in Saxony: from 22% in the 2004/05 season to 36% in the 2005/06 season. The average rate was higher in the new German states than in the old states: 26% versus 16% (2004/05), 31% versus 19% (2005/06), and 29% versus 17% (2006/07).
Figure 1.
Influenza vaccination rates in the population according to area covered by associations of statutory health insurance physicians in the influenza seasons 2004/05, 2005/06, and 2006/07
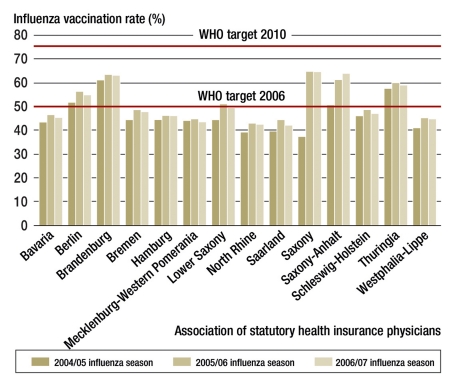
Influenza vaccination rates in persons older than 60 were 45% (2004/05), 50% (2005/06), and 49% (2006/07) (figure 2). In the individual areas covered by the associations for statutory health insurance physicians, vaccination rates ranged from 37% (Saxony, 2004/05) and 64% (Saxony and Saxony-Anhalt, 2005/06). As for the general population, average vaccination rates were higher in the over-60-year-olds in the new German states than in the old states: 50% versus 42% (2004/05), 60% versus 46% (2005/06), and 59% versus 45% (2006/07).
Figure 2.
Influenza vaccination rates in the over-60-year-olds according to area covered by associations of statutory health insurance physicians in the influenza seasons 2004/05, 2005/06, and 2006/07
In all 3 seasons under study, vaccination rates in the over-60-year-olds were increased in tandem with the recipients’ age. In 60- to 64-year-olds, the average rate was 38%; in 65- to 69-year-olds, 46%; in 70- to 74-year-olds, 51%; and in those older than 75, 54%.
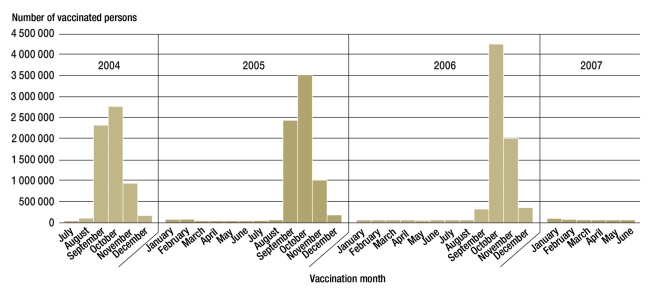
Timing of the influenza vaccination
In the seasons 2004/05, 2005/06, and 2006/07, vaccinations were usually given in September to December (figure 3). Large proportions of the vaccinations were administered in October and November (41% and 18% in 2004/05, 49% and 17% in 2005/06, and 55% and 31% in 2006/07). In September 2006, fewer vaccinations were given than in both September 2004 or September 2005. However, more vaccinations were given in October and November 2006 than in those 2 months in either of the preceding 2 years. Of persons older than 60 who received the vaccine, 98% to 99% were vaccinated by the end of December, compared with 94% to 97% of persons younger than 60.
Figure 3.
Timing of influenza vaccination in the over-60-year-olds in the influenza seasons 2004/05, 2005/06, and 2006/07
Repeated annual influenza vaccination
A total of 16 417 040 individuals were vaccinated against influenza in the influenza seasons 2004/05, 2005/06, and 2006/07. More than half of these (9 080 252) were older than 60 (table). Notable differences existed regarding the proportions of people in the 2 age groups who received an influenza vaccination in 1, 2, or all 3 of the seasons under study. 23% of the under-60-year-olds were vaccinated in all 3 seasons, compared with 48% of those older than 60.
Table. Influenza vaccinations by age group and number of vaccinations in the observation period (influenza seasons 2004/05 to 2006/07).
| Age group | Vaccination given in | No of vaccinated persons | Percentage |
| Total | 16 417 040 | ||
| Younger than 60 | 7 336 788 | 100 | |
| One season | 3 688 367 | 50 | |
| Two seasons | 1 998 431 | 27 | |
| Three seasons | 1 649 990 | 23 | |
| Older than 60 | 9 080 252 | 100 | |
| One season | 2 198 497 | 24 | |
| Two seasons | 2 573 421 | 28 | |
| Three seasons | 4 308 334 | 48 |
For about 60% of vaccinated individuals, information on their sex was included in the data. In both age groups, more women than men were vaccinated (60% and 64%, respectively). The proportion of women in the study population in the under-60-year-olds was 51% and in the over-60-year-olds, 59%. 67% of those who received the vaccine in all 3 seasons under study were women.
Discussion
The World Health Organization has set a target for 2006 for influenza vaccination rates in the elderly population of above 50% and for 2010 of above 75% (6). In Germany, the average vaccination rate for influenza in the over-60-year-olds in the areas under study came to 50% only in the 2005/06 season. In the individual German states, the situation was heterogeneous. Berlin, Brandenburg, Saxony, Saxony-Anhalt, and Thuringia had vaccination rates of 54% to 64%. Of the western states, only Lower Saxony reached a vaccination rate of 50% in the 2005/06 season. In 2005/06, vaccination rates peaked in all German states, which may be explained with the severe influenza season 2004/05 and the generally raised awareness owing to avian influenza. In the seasons under study, vaccinations against influenza were administered mainly in the months of October (at an average of 48%) and November (at an average of 22%). These months are regarded as the ideal months for administering the vaccine (5). After the new year, only 1% to 2% of vaccinations were given in the over-60-year-olds, and 3% to 6% in the under-60-year-olds, although this time marks the onset of the influenza season, and repeat invitations to be vaccinated are issued. In September 2006, fewer vaccinations were given in all age groups than in the same month in the preceding years. The reason was that the vaccine became available only with a few weeks’ delay in the autumn of 2006. This may have contributed to the fact that the vaccination rate in the 2006/07 season did not rise further compared with 2005/06. In Saxony, the vaccination rate in the general population rose by almost two thirds from the 2004/05 season to the 2005/06 season. In each age group, notably more persons were vaccinated, with a particularly big increase in the over-50-year-olds. The vaccination committee for Saxony (Sächsische Impfkommission, SIKO) lowered the recommended age for standard influenza vaccination from older than 60 to older than 50 in 2005 (15). The costs of the vaccines were reimbursed by Saxony’s statutory health insurers without any restrictions being imposed. International comparative studies have shown that the fact that the vaccination was free of charge played an important part in people’s decisions about whether to be vaccinated or not (10). The Saxony State Medical Association and the state’s association of statutory health insurance physicians informed doctors about the changes, which apparently led to a sustained increase in the number of influenza vaccinations.
Vaccination rates in the over-60-year-olds, as determined in the annual cross sectional telephone survey by the Szucs, Blank, et al. working group, were around 41% (2004/05 season), 52% (2005/06 season), and 45% (2006/07 season) (7). Vaccination rates in the over-60-year-olds, which we calculated on the basis of data from the associations of statutory health insurance physicians, were about 45% (2004/05 season), 50% (2005/06), and 49% (2006/07). This means that vaccination rates for 2004/05 and 2006/07 in the cross sectional telephone surveys were 4% below those based on the data from the associations of statutory health insurance physicians. The vaccination rate for the 2005/06 season in the cross sectional telephone survey was 2% above that calculated by us. We were not able to conclusively explain how these deviations arose. The cross sectional studies are based on a sample of persons older than 14 in the German population, whereas the associations’ data cover the population with statutory health insurance. The number of vaccine doses prescribed rose from 17.5 million in 2004 to 20 million in 2007, with the largest number of doses prescribed in 2005 (20.8 million) (11). Relative to the total population in Germany, this means vaccination rates of 21% to 25%, which is in the same order of magnitude as the calculated rates based on the KV data.
Our analysis comprises data from 14 of the 17 associations of statutory health insurance physicians for which complete billing data for influenza vaccination were available for 2004 to 2007. The remaining 3 associations provided data for individual years and/or parts of the respective area covered. In future, all 17 associations will collect complete data, so that vaccination rates can be determined nationwide. It needs to be borne in mind that these data reflect only the vaccination rates of members of statutory health insurance schemes (about 86% of Germany’s population). Data from other sources about vaccinations of people with private health insurance, and vaccinations that were given by occupational health physicians or health offices are not available. If nobody with private health insurance were vaccinated against influenza, then the vaccination rate in the over-60-year-olds for the 3 seasons under study would drop to 39% to 43%. Similarly, the rate would rise to 53% to 57% if everyone with private health insurance were vaccinated against influenza. The influence of vaccinations administered by occupational health physicians or health offices cannot be quantified. It has been shown, however, that the vaccination rate for medical personnel rarely reaches 50% (16).
The most important measures to increase vaccination rates in the population over 60 years of age include information campaigns to the public and health care providers, availability of information brochures for physicians in private practice, and the use of systems that enable doctors to remind risk groups for which influenza vaccination is recommended of their annual appointment. Physicians in private practice have a key role in influenza vaccination (17, 18). In addition to the severity of the disease, motivation provided by practice staff or the primary care physician are reportedly the most important reasons for having the influenza vaccine (10). However, a recent survey of physicians in private practice has shown that only half of the participating doctors advises all 3 patient groups with the highest risk (over-60-year-olds, people with chronic diseases, and medical personnel) to have the influenza vaccine (18). Our analysis of the statutory health insurance data showed that only 36% of vaccinated persons received the influenza vaccine in each of the 3 influenza seasons under study, and only 23% of the over-60-year-olds. Most of the people, especially men, received the vaccine in only 1 or 2 of the influenza seasons under study. In addition to the patients who remained unaware of influenza vaccination, these constitute the target group for a recall system on the part of the physicians in private practice. The German Federal Centre for Health Education and the Robert Koch-Institute have been running a joint campaign since 2006 in order to raise influenza vaccination rates, among others in the over-60-year-olds, with the aim of achieving a rate of 75% in 2010.
In order to support physicians in private practice in helping to achieve improved vaccination coverage, doctors have been provided with several posters and an information brochure (19).
Conclusion and recommendation
The WHO-recommended influenza vaccination rate of 50% in the elderly population for 2006 was reached only in the new German states. Since the 2005/06 influenza season, vaccination rates have not increased. It is therefore a particular challenge to all involved to ensure that the target of 75% vaccination coverage in the over-60-year-olds is reached by 2010. Regular evaluation of the data of the associations of statutory health insurance physicians enables continuous monitoring of influenza vaccination rates.
Key Messages.
Germany follows the recommendations of the World Health Organization (WHO) and is thus aiming to reach influenza vaccination coverage of 75% in the elderly population by 2010.
In Germany, influenza vaccinations are not centrally captured. Regular analyses of data from the associations of statutory health insurance physicians that are conducted by the Robert-Koch-Institute in the context of its “KV sentinel” project enable continuous monitoring of influenza vaccination rates.
Evaluation of data from 14 German associations of statutory health insurance physicians shows that influenza vaccination rates in members of statutory health insurance schemes aged over 60 were between 45% and 50% in the influenza seasons 2004/05, 2005/06, and 2006/07.
Of the vaccinated over-60-year-olds, 52% received the vaccination in only 1 or 2 of the influenza seasons under study. In addition to the patients that have not participated in any influenza vaccination campaigns at all, these persons are a target group for a recall system by physicians in private practice.
Physicians in private practice have a key role in the context of influenza vaccination. Further to the severity of the disease, motivation provided by the primary care physician or practice assistant is regarded as the most important reason for seeking vaccination.
Acknowledgments
Translated from the original German by Dr Birte Twisselmann.
Footnotes
Conflict of interest statement
The authors declare that no conflict of interest exists according to the guidelines of the International Committee of Medical Journal Editors.
References
- 1.Rothberg MB, Haessler SD, Brown RB. Complications of viral influenza. Am J Med. 2008;121:258–264. doi: 10.1016/j.amjmed.2007.10.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Robert Koch-Institut. Survstat, http://www3rki.de/survstat, Datenstand. 2009. Aug 28,
- 3.Buchholz U. Influenza-assoziierte Mortalität in Deutschland 1985-2006. Epid Bull. 2007;35:325–327. [Google Scholar]
- 4.RKI. Empfehlungen der Ständigen Impfkommission (STIKO) am Robert Koch-Institut. Epid Bull. 2009;30:279–298. [Google Scholar]
- 5.RKI. Auftakt der jährlichen Influenza-Impfaktion: Kommen Sie der Grippe zuvor. Jedes Jahr. Epid Bull. 2006;43 [Google Scholar]
- 6.World Health Organization. WHA 10th plenary meeting. 2003. May 28, Resolution of the World Health Assembly (WHA 56.19). Prevention and control of influenza pandemics and annual epidemics. [Google Scholar]
- 7.Blank PR, Freiburghaus AU, Ruf BR, Schwenkglenks MM, Szucs TD. Entwicklung der Influenzaimpfraten in Deutschland von 2001/02 bis 2006/07. Med Klin (Munich) 2008;103:761–768. doi: 10.1007/s00063-008-1121-0. [DOI] [PubMed] [Google Scholar]
- 8.Holm MV, Blank PR, Szucs TD. Trends in influenza vaccination coverage rates in Germany over five seasons from 2001 to 2006. BMC Infect Dis. 2007;7 doi: 10.1186/1471-2334-7-144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Blank PR, Schwenkglenks M, Szucs TD. Influenza vaccination coverage rates in five European countries during season 2006/07 and trends over six consecutive seasons. BMC Public Health. 2008;8 doi: 10.1186/1471-2458-8-272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Blank PR, Schwenkglenks M, Szucs TD. Vaccination coverage rates in eleven European countries during two consecutive influenza seasons. J Infect. 2009;58:446–458. doi: 10.1016/j.jinf.2009.04.001. [DOI] [PubMed] [Google Scholar]
- 11.Arbeitsgemeinschaft Influenza. http://influenza.rki.de/saisonbericht/2008.pdf. Berlin: 2009. Abschlussbericht der Influenzasaison 2008/09. [Google Scholar]
- 12.Jacobson VJ, Szilagyi P. Patient reminder and patient recall systems to improve immunization rates. Cochrane Database Syst Rev. 2005 doi: 10.1002/14651858.CD003941.pub2. CD003941. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Reuss A, Feig M, Kappelmayer L, Eckmanns T, Poggensee G. Sind Daten der Kassenärztlichen Vereinigungen für die Surveillance von Impfungen und impfpräventablen Erkrankungen geeignet? Gesundheitswesen. 2010;72(6):340–346. doi: 10.1055/s-0030-1249691. [DOI] [PubMed] [Google Scholar]
- 14.Bundesministerium für Gesundheit. Statistik über Versicherte, gegliedert nach Status, alter, Wohnort, Kassenart. www.Bmg.Bund.de/cln_151/nn_1193098/de/gesundheit/statistiken/gesetzliche-krankenversicherung__node.Html?__nnn=true#doc1193102bodytext2.
- 15.Empfehlung der Sächsischen Impfkommisson (SIKO) Impfkalender für Kinder, Jugendliche und Erwachsene im Freistaat Sachsen, Stand. Http://www.Slaek.de/60infos/infosarzt/36impfen/pdf/kalenderallgemein.pdf. 2008. Januar.
- 16.Wicker S, Rabenau HF, Kempf VA, Brandt C. Vaccination against classical influenza in health-care workers: Self-protection and patient protection. Dtsch Arztebl Int. 2009;106:567–572. doi: 10.3238/arztebl.2009.0567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Buchholz U, Szecsenyi J. Influenzaimpfung: Wie sind die WHO-Ziele bis 2010 zu erreichen? Dtsch Arztebl. 2008;105:2508–2509. [Google Scholar]
- 18.Wortberg S, Walter D, Knesebeck M, Reiter S. Niedergelassene Ärzte als Multiplikatoren der Influenzaimpfung bei älteren Menschen, chronisch Kranken und medizinischem Personal. Ergebnisse einer bundesweiten Repräsentativbefragung im Rahmen der nationalen Influenza-Impfkampagne. Bundesgesundheitsblatt Gesundheitsforschung Gesundheitsschutz. 2009;52:945–952. doi: 10.1007/s00103-009-0871-z. [DOI] [PubMed] [Google Scholar]
- 19.Bundeszentrale für gesundheitliche Aufklärung. Infomaterialien zur saisonalen Grippe. www.Bzga.de/?Uid=e454caf4859ce246f0 ee6129fb37d43e&id=medien&sid=148&addinfo=1.