Abstract
The Canadian Digestive Health Foundation initiated a scientific program to assess the incidence, prevalence, mortality and economic impact of digestive disorders across Canada in 2009. The current article presents the updated findings from the study concerning inflammatory bowel diseases – specifically, Crohn’s disease and ulcerative colitis.
Keywords: Burden of disease, Chronic disease, Crohn’s disease, Inflammatory bowel diseases, Ulcerative colitis
Abstract
La Fondation canadienne pour la promotion de la santé digestive a lancé un programme scientifique pour évaluer l’incidence, la prévalence, la mortalité et les conséquences économiques des maladies digestives au Canada en 2009. Le présent article expose les résultats à jour de l’étude au sujet des maladies inflammatoires de l’intestin, notamment la maladie de Crohn et la colite ulcéreuse.
The Canadian Digestive Health Foundation (CDHF) launched a scientific project to define the incidence, prevalence, mortality and economic impact of digestive disorders across Canada. Detailed information on 19 digestive disorders was compiled through systematic reviews, government documents and Internet sites. This information was published as ‘Establishing Digestive Health as a Priority for Canadians, The Canadian Digestive Health Foundation National Digestive Disorders Prevalence and Impact Study Report’, and released to the press and government in late 2009 (www.CDHF.ca). The CDHF Public Impact Series presents a full compilation of the available statistics for the impact of digestive disorders in Canada.
Crohn’s disease (CD) and ulcerative colitis (UC) are collectively referred to as inflammatory bowel diseases. Although the etiology of CD and UC is unknown, the current hypothesis is that the immune system becomes dysregulated in response to environmental stimuli, such as intestinal microflora, and causes it to attack the intestinal tissues. Genetics are believed to play an important role because incidence rates for both CD and UC are higher in families with a history of these diseases.
Previous studies have reported that CD and UC are important and costly diseases that represent a considerable burden to health care systems, the individual and, by extension, their families. Although data are available, this information has not been extrapolated to the Canadian context in an accessible format. Aimed at both medical professionals and patients, the present review aims to increase awareness of CD and UC through a comprehensive overview of disease incidence and prevalence, and the implications for the Canadian health care system and its socioeconomics.
METHODS
A systematic literature review was conducted to retrieve peer-reviewed scholarly literature written in English using the databases PubMed, Medline, EMBASE, Scopus and EvaluatePharma (United Kingdom). The following search terms were used: “Crohn’s disease”, “ulcerative colitis” and “inflammatory bowel disease”, with a specific focus on epidemiological and economic studies from developed countries. Additional information was retrieved from government sources, the WHO and not-for-profit organizations.
INCIDENCE
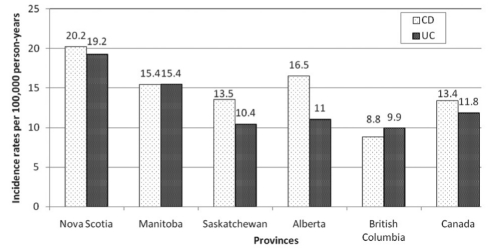
Canada has one of the highest incidence rates of CD and UC in the world (Figure 1) (1). Based on incidence data collected during 1998 through to 2000 (1), the national averages were 13.4 and 11.8 cases of CD and UC per 100,000 person-years, respectively. With a national population estimated to be 34 million (at April 2010 [2]), there will be approximately 4500 new cases of CD and 4000 new cases of UC diagnosed in Canada in 2010. Using data from a medical database study by Lowe et al (3), the incidence of CD in Quebec was 20.2 cases per 100,000 person-years, a rate similar to that for Nova Scotia, which has the highest incidence rate in the country (1). When considering the combined CD incidence data, the national average equates to 17.16 cases per 100,000 population (1,3). No historical information is available for trend analysis of incidence rates of inflammatory bowel diseases in Canada. Globally, Canada has one of the highest incidences of CD, second to New Zealand (16.5 cases per 100,000 population) and slightly higher than Scotland (11.7 cases per 100,000 population) and England/Wales (5.9 to 11.1 cases per 100,000 population) (4). The rates for the United States, Denmark and Sweden range from 7 to 8.9 cases per 100,000 population (4). For UC, the Canadian incidence rate is considered to be modestly high when compared with rates in northern Europe, which range from 6.3 to 15.1 cases per 100,000 population (1).
Figure 1.
Incidence rates of Crohn’s disease (CD) and ulcerative colitis (UC) in Canada. Data from reference 1
With respect to pediatric patients (zero to 19 years of age), the average incidence rates of CD and UC in Alberta, British Columbia, Manitoba, Nova Scotia and Saskatchewan were 8.32 and 4.34 cases per 100,000 population, respectively. Using the population according to age information for July 2009 (5), there were 654 and 341 reported new cases of pediatric CD and UC, respectively. Within the province of Quebec, the annual incidence rate for CD in youth zero to 19 years of age was 13.9 cases per 100,000 person-years determined from data spanning the years 1993 to 2002 (3). By combining the incidence data for CD in these six provinces, the mean rate was 9.25 cases per 100,000 person-years, resulting in an additional 73 cases per year for a total of 727. However, the Canadian incidence rates for both pediatric CD and UC were very high compared with those reported for northern California (USA) in 2010, which were 2.7 and 3.2 cases per 100,000 children, respectively (6). Although trend analyses using historical pediatric incidence data are unavailable in Canada, this American study found increasing incidence rates for both CD and UC; however, the increase was only statistically significant for UC (1.8 cases per 100,000 population, which increased to 4.9 cases per 100,000 population; P<0.001). As such, it is possible that the Canadian incidence rate for inflammatory bowel diseases in pediatric patients is also increasing.
Each year, Canadians are diagnosed with CD and UC at rates that are among the highest in the world.
PREVALENCE
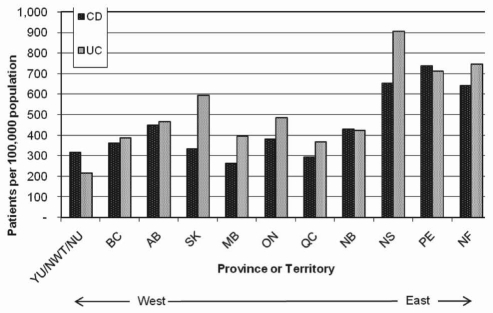
The Canadian Common Household Survey (CCHS) is a national, population-based survey that collects health and lifestyle information and is conducted by Statistics Canada. Cycle 4.1 of the CCHS for 2007/2008 (7) specifically collected prevalence information concerning different types of medically diagnosed bowel disorders. At that time, there were 105,000 Canadians with CD and 128,000 with UC. The provinces with the highest prevalence of CD and UC were Prince Edward Island and Nova Scotia, respectively. An examination of the data according to province shows a distinct increase in the prevalence of both CD and UC moving from west to east (Figure 2).
Figure 2.
Provincial distribution of Crohn’s disease (CD) and ulcerative colitis (UC) patients in 2007/2008. AB Alberta; BC British Columbia; MB Manitoba; NB New Brunswick; NF Newfoundland and Labrador; NS Nova Scotia; NU Nunavut; NWT Northwest Territories; ON Ontario; PE Prince Edward Island; QC Quebec; SK Saskatchewan; YU Yukon. Data from the Canadian Common Household Survey, cycle 4.1 (7)
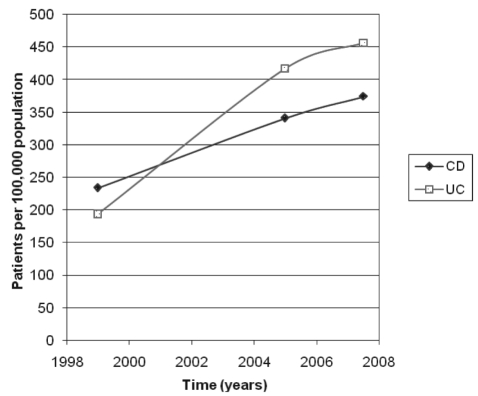
Previously, two population-based surveys (1,8) also examined the prevalence of CD and UC in Canada: the study by Bernstein et al (1) for the years 1998 to 2000, and cycle 3.1 of the CCHS for 2005 (8). Based on these studies, the prevalence rates for both CD and UC over the past 10 years have been steadily increasing, with CD cases nearly doubling within this period (Figure 3). Within the province of Quebec between 1993 and 2002, the prevalence of CD increased from 83 to 270 cases per 100,000 population (3). This 3.25-fold increase in prevalence equates to an additional 36,500 CD patients within 10 years. Using population estimate data from April 2010 (9) and the prevalence rates reported in cycle 4.1 of the CCHS (7), there are nearly 280,000 Canadians with medically diagnosed inflammatory bowel disease, which corresponds to 0.8% of the population (CD: n=127,188; UC: n=155,089).
Figure 3.
Growth of Crohn’s disease (CD) and ulcerative colitis (UC) populations in Canada. Data compiled and adapted from three population based surveys: Bernstein et al (1) (1998 to 2000), 2007/2008 Canadian Common Household Survey cycle 4.1 (7) and the 2005 Canadian Common Household Survey cycle 3.1 (8)
Similar to the rankings for CD and UC incidence rates in Canada, Canada has one of the highest prevalence rates for CD and UC in the world, with 374 and 456 cases per 100,000 population, respectively (7). Within the United States, the rates are only 201 and 238 cases per 100,000 population for CD and UC, respectively (10). Northern European rates range from 27 to 48 per 100,000 population for CD, and 58 to 157 per 100,000 population for UC (1). Canadian rates are even higher when compared with countries from southern regions such as Spain, Italy, Cuba and South America, which have rates of less than 1.0, and 1.5 to 5.8 per 100,000 population for CD and UC, respectively (1).
The prevalence rates of CD and UC in Canadian children (zero to 19 years of age) were 43.38 cases and 22.36 cases per 100,000 population, respectively. Using the population estimate according to age group for July 2009 (5), there were a total of 5200 children with inflammatory bowel disease living in Canada at that time (CD: n=3411; UC: n=1758). For comparative purposes, prevalence rates in the United States for this age range for both CD and UC were 43 and 28 per 100,000 population, respectively (10).
CD and UC compared with other chronic conditions
Cycle 4.1 of the CCHS specifically addressed the prevalence of 18 common, medically diagnosed, chronic diseases affecting Canadians including back problems, arthritis, asthma, diabetes, emphysema, CD and UC (7). In total, there were more than 30 million cases of chronic conditions, with many individuals having multiple issues. The most prevalent chronic condition was back problems, while bowel disorders including CD and UC were ranked 10th with 1.2 million cases, which represented 4% of all chronic conditions.
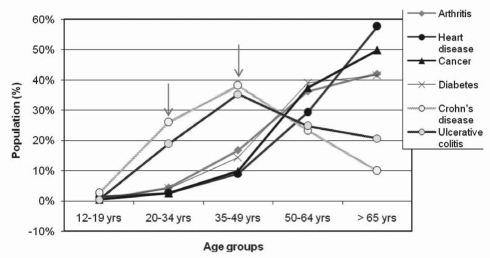
Unlike other common chronic conditions, such as arthritis and heart disease, which occur later in life, CD and UC occur in late adolescence or early adulthood, and persists through to the twilight years. Figure 4 shows the percentage of cases with common chronic diseases according to age group for 2007/2008 (7). The exponential increase in the percentage of arthritis, cancer, heart disease and diabetes cases between the age groups of 35 to 49 years and 50 to 64 years contrasts sharply with the shallow bell curves of CD and UC that affect the age groups 20 to 34 years through to 65 years of age and older. Unlike other patients with chronic conditions, those with CD and UC may compromise early life activities such as education, career development or family planning, regardless of their symptoms.
Figure 4.
Canadians with chronic diseases categorized according to age group for 2008. Arrows highlight the age groups uniquely affected by Crohn’s disease and ulcerative colitis. yrs Years. Data adapted from the Canadian Common Household Survey cycle 4.1 (7)
Globally, Canada has high prevalence rates for both CD and UC. On a national level, bowel diseases affect one in 300 persons.
MORTALITY
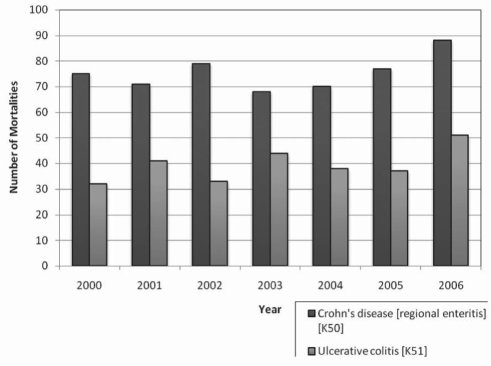
For the years 2000 to 2006, the annual mean mortality rate primarily due to CD and UC was 75 and 39 deaths per year, respectively (Figure 5) (11). Compared with deaths in Canada due to all causes, CD and UC deaths collectively accounted for 0.05% of the annual total. Although the annual mortality rate for both CD and UC has been slowly increasing, the ratio of these deaths to deaths due to all causes has been constant at 0.05%.
Figure 5.
Number of mortalities each year primarily attributed to Crohn’s disease (disease code K50) or ulcerative colitis (disease code K51). Data adapted from reference 11
An independent meta-analysis of 13 articles (12) found that CD patients have an age-adjusted risk of premature death that is 50% greater than the general population (standardized mortality ratio [SMR] 1.52; 95% CI 1.32 to 1.74; P<0.0001). A subsequent meta-analysis of nine articles (13) found an overall SMR of 1.39 for CD patients relative to the general population. Cause-specific mortalities included cancer, particularly pulmonary cancer, chronic obstructive pulmonary disease and genitourinary disease in addition to the main cause being gastrointestinal disease (13). For comparative purposes, the risk of premature death is higher for CD patients than for tobacco users who smoke fewer than 15 cigarettes per day (SMR 1.15 to 1.24), asthma patients (SMR 1.2) and celiac disease (SMR 1.17) (12). The SMR for CD is similar to that reported for patients with rheumatoid arthritis (SMR 1.28 to 2.644) and individuals who smoke more than 15 cigarettes per day (SMR 2.14 to 2.26) (12). Conversely, diabetic patients have a higher SMR range (1.73 to 2.10) than CD patients. Regression analysis found that the premature risk of death for CD patients has not changed statistically within the past 30 years. This stability is associated with the use of immunomodulators such as azathioprine, methotrexate and corticosteroids, beginning in the 1970s, which led to the improved management of severe disease flares (12).
The age-standardized mortality rate for patients with UC is considerably lower than that for CD patients (12). A meta-analysis of 10 studies (14) reported an SMR range of between 0.7 and 1.4, while the overall pooled estimate was 1.1 (95% CI 0.9 to 1.2), which was not statistically different from that of the general population (P=0.42). Cause-specific mortalities were highest for nonalcoholic liver diseases, pulmonary embolisms and respiratory disease in addition to the primary cause being gastrointestinal diseases (14).
Each year, 114 deaths in Canada are attributed to CD and UC.
ECONOMICS
The economic cost of CD in the United States was recently estimated to be USD$10 billion to USD$15 billion per year. Within Canada, the economic burden of CD and UC has been estimated to be $753 million for direct costs and $1.064 billion for indirect costs (15).
Direct costs
Direct costs include prescription medications, hospitalizations, surgeries, emergency and physician clinic visits, laboratory and endoscopic investigations as well as the services of allied health care personnel (eg, dieticians, inflammatory bowel disease nurses and social workers). Although some of these costs can be more easily ascertained than others, in 2008, the average cost was estimated to be at least $3,750/patient/year (11).
Pharmaceuticals
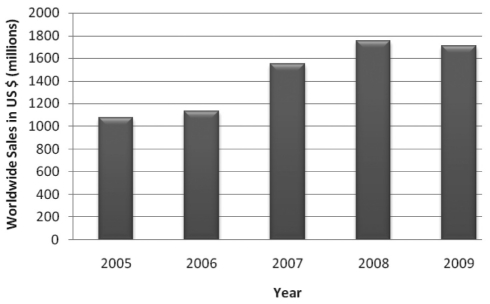
In 2009, there were 244 and 264 pharmaceutical medications available globally for the treatment of CD and UC, respectively (16). Combined sales for gastrointestinal anti-inflammatories including mesalamine, hydrocortisone, balsalazide, budesonide and others (representing 19% to 31% of total annual sales) (16) are presented in Figure 6. In the past five years, there have been 15 worldwide launches of new products for the treatment of CD compared with 20 for UC; three products have been launched for the treatment of inflammatory bowel diseases (16). In 2008, it was estimated that the mean cost for prescription drugs was $809/year/UC or CD patient (15).
Figure 6.
Global sales of gastrointestinal anti-inflammatories including mesalamine, hydrocortisone, balsalazide, budesonide and others (representing 19% to 31% of total annual sales). Sales for 2005 and 2006 represent 246 products, while sales figures for 2007 to 2009 represent the combined total for 315 products. Data from reference 16
Based on a national survey (17), complimentary alternative medicines (CAMs) have been used by 47% of patients with inflammatory bowel disease in Canada. Costs for CAMs are not typically covered by health insurance plans in Canada. These out-of-pocket expenses amount to an estimated $523/year/CAM user (11).
Physician services
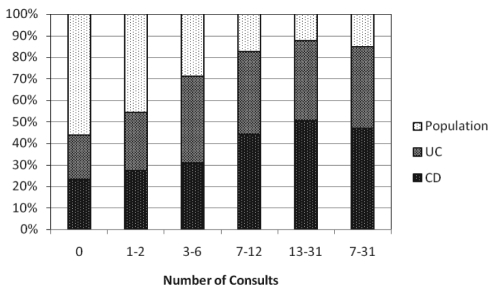
A study of Manitoban residents found that, on average, CD and UC patients visited physicians and out-patient clinics twice as often as the rest of the population (15). According to the CCHS cycle 4.1 for 2007/2008 (8), this trend has continued. An examination of the number of consultations for CD and UC patients compared with the general Canadian population highlights the unusually high frequency of physician visits for these patients (Figure 7). In turn, it is not surprising that the second greatest health care expense category for CD and UC is for physician services. In 2008, physician visits were estimated to cost the Canadian health care system $80 million/year for CD and $54 million/year for UC (15).
Figure 7.
Number of physician consultations (Consults) for Crohn’s disease (CD) and ulcerative colitis (UC) compared with the number of physician consults among the general population in 2007/2008. Data from the Canadian Common Household Survey, cycle 4.1 for 2007/2008 (7)
Hospitalization
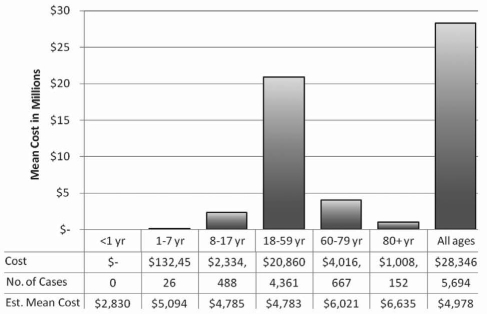
For both CD and UC, hospitalization represents a major burden for the Canadian health care system mainly because they frequently involve surgery (15). Compared with the general population, CD and UC patients are hospitalized twice as often (15), with a single admission costing an average of $5,000 (18). Figure 8 details the annual expenses incurred for inpatients according to disease type. Interestingly, in 2004/2005, the hospitalization cost for 9374 CD and UC patients was $87,778,136, which corresponds to approximately $9,000/patient (19). Due to differences in data collection, these two values are only loosely comparable, yet they suggest that hospital costs are being reduced. In the 1980s, the average length of hospital stay for CD and UC patients was 14 days; however, with new therapies and treatment algorithms, this has been reduced to a mean of 9.3 days/CD or UC inpatient (20).
Figure 8.
Estimated hospitalization costs for treatment of inflammatory bowel disease in 2008. Values obtained from the Patient Cost Estimator for 2008 (18). Est Estimated; No Number; yr Year(s)
Indirect costs
In 2008, total indirect costs for Canadians with CD and UC were estimated to be $595 million and $469 million, respectively (15). In 2008, individuals with CD and UC missed an average of 7.2 days of work due to disease symptoms, which equated to approximately $140 million in lost time incurred by Canadian employers (15). Twice as many individuals with CD or UC reported activity restriction due to disease while at work than the general population (7). This reduction in productivity while at work is difficult to evaluate and analyze. However, in recognition of this, the dollar amount attributed to absenteeism due to disease should be regarded as an underestimate.
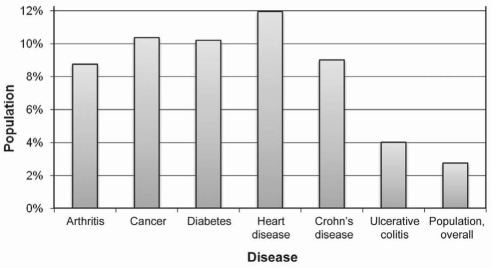
The proportion of CD and UC patients who are permanently unable to work because of their medical condition are 9% and 4%, respectively, compared with only 3% of the general population (Figure 9) (7). Interestingly, this measure for CD patients is similar to that for arthritis, cancer and diabetes. For comparison, 12% of heart disease patients are permanently unable to work.
Figure 9.
Percentage of Canadians permanently unable to work categorized according to chronic disease type. Data obtained from the Canadian Common Household Survey, cycle 4.1 (7)
Premature deaths due to inflammatory bowel disease are estimated to cost $7 million per year in lost productivity (15). Personal expenses incurred due to CD or UC, such as non-prescription medicines, supplements and travel for medical care, have been estimated to be $240 million/year (15).
The combined economic burden for direct and indirect costs for CD and UC is conservatively estimated to be $1.75 billion each year.
REFERENCES
- 1.Bernstein CN, Wajda A, Svenson LW, et al. The epidemiology of inflammatory bowel disease in Canada:A population-based study. Am J Gastroenterol. 2006;101:1559–68. doi: 10.1111/j.1572-0241.2006.00603.x. [DOI] [PubMed] [Google Scholar]
- 2.Statistics Canada. Quarterly Demographic Estimates. [Accessed on July 28, 2010]. < http://www.statcan.gc.ca/daily-quotidien/100628/dq100628a-eng.htm>.
- 3.Lowe AM, Roy PO, Poulin MB, et al. Epidemiology of Crohn’s disease in Quebec, Canada. Inflamm Bowel Dis. 2009;15:429–35. doi: 10.1002/ibd.20756. [DOI] [PubMed] [Google Scholar]
- 4.Economou M, Pappas G. New global map of Crohn’s disease: Genetic, environmental, and socioeconomic correlations. Inflamm Bowel Dis. 2008;14:709–20. doi: 10.1002/ibd.20352. [DOI] [PubMed] [Google Scholar]
- 5.Statistics Canada. Population by sex and age group, CANSIM, Table 051-0001. [Accessed on May 14, 2010]. < http://www40.statcan.gc.ca/l01/cst01/demo10a-eng.htm>.
- 6.Abramson O, Durant M, Mow W, et al. Incidence, prevalence, and time trends of pediatric inflammatory bowel disease in Northern California, 1996 to 2006. J Pediatr. 2010;157:233–9. doi: 10.1016/j.jpeds.2010.02.024. [DOI] [PubMed] [Google Scholar]
- 7.Statistics Canada – Health Statistics Division. Canadian Community Health Survey (CCHS) Cycle 4.1 2007–2008. Ottawa: Statistics Canada; 2009. [Google Scholar]
- 8.Statistics Canada – Health Statistics Division. Canadian Community Health Survey (CCHS) Cycle 3.1 2005. Ottawa: Statistics Canada; 2006. [Google Scholar]
- 9.Statistics Canada. Quarterly Demographic Estimates. [Accessed July 28, 2010]. < http://www.statcan.gc.ca/daily-quotidien/100628/dq100628a-eng.htm>.
- 10.Kappelman MD, Rifas-Shiman SL, Kleinman K, et al. The prevalence and geographic distribution of Crohn’s disease and ulcerative colitis in the United States. Clin Gastroenterol Hepatol. 2007;5:1424–9. doi: 10.1016/j.cgh.2007.07.012. [DOI] [PubMed] [Google Scholar]
- 11.Statistics Canada. CANSIM – Table 102-0531 – Deaths, by cause, Chapter XI: Diseases of the digestive system (K00 to K93), age group and sex, Canada, annual (2000–2006) [Accessed on July 28, 2010]. < http://cansim2.statcan.gc.ca>.
- 12.Canavan C, Abrams KR, Mayberry JF. Meta-analysis: Mortality in Crohn’s disease. Aliment Pharmacol Ther. 2007;25:861–70. doi: 10.1111/j.1365-2036.2007.03276.x. [DOI] [PubMed] [Google Scholar]
- 13.Duricova D, Pedersen N, Elkjaer M, Gamborg M, Munkholm P, Jess T. Overall and cause-specific mortality in Crohn’s disease: A meta-analysis of population-based studies. Inflamm Bowel Dis. 2010;16:347–53. doi: 10.1002/ibd.21007. [DOI] [PubMed] [Google Scholar]
- 14.Jess T, Gamborg M, Munkholm P, Sorensen TI. Overall and cause-specific mortality in ulcerative colitis: Meta-analysis of population-based inception cohort studies. Am J Gastroenterol. 2007;102:609–17. doi: 10.1111/j.1572-0241.2006.01000.x. [DOI] [PubMed] [Google Scholar]
- 15.Crohn’s and Colitis Foundation of Canada. The Burden of Inflammatory Bowel Disease (IBD) in Canada. Toronto: Crohn’s and Colitis Foundation of Canada; 2008. [Google Scholar]
- 16.EvaluatePharma. EvaluatePharma®. [Accessed on October 18, 2010]. < http://www.evaluatepharma.com/Default.aspx>.
- 17.Li FX, Verhoef MJ, Best A, Otley A, Hilsden RJ. Why patients with inflammatory bowel disease use or do not use complementary and alternative medicine: A Canadian national survey. Can J Gastroenterol. 2005;19:567–73. doi: 10.1155/2005/943547. [DOI] [PubMed] [Google Scholar]
- 18.Canadian Institute for Health Information. Patient Cost Estimator. [Accessed on July 28, 2010]. < http://www.cihi.ca>.
- 19.Canadian Institute for Health Information. The Cost of Acute Care Hospital Stays by Medical Condition in Canada: 2004–2005. Ottawa: Canadian Institutes for Health Information; 2008. pp. 1–155. [Google Scholar]
- 20.Organisation for Economic Co-operation and Development (OECD) OECD Health Data. 2008. [Accessed on November 11, 2008]. < http://www.oecd.org>.