Abstract
Osteoporotic bone, structurally altered because of reduction of bone mineral density and quality deterioration, can easily head for fracture after minimum mechanical stress.
The most common sites of fracture, other than spine and hip, are, in decreasing order: distal radius, forearm, proximal humerus, other femoral sites, ribs, pelvis, tibia and fibula, metatarsal bone and calcaneum. The role of diagnostic imaging is essential in detecting fractures for their immediate and correct assessment, which is necessary to the planning of treatment, whether conservative or surgical. Imaging is also important in fracture monitoring, evaluation of healing and relief of any complications.
Conventional radiology is the most widely used technique in the diagnosis of fracture, although its low sensitivity, mainly in anatomically complex sites; the role of radiology is undisputed in monitoring the healing bone callus formation. Multidetector Computed Tomography (MDCT) is of great help in doubtful cases, especially in locations as “critical”; its diagnostic accuracy is very elevated with 3D and multi-planar reconstructions, allowing the surgeon to implement an appropriate therapeutic strategy.
Magnetic Resonance (MR) is the most sensitive technique in the relief of minimal structural alteration of the cancellous bone, as it reveals both fracture line and surrounding bone marrow oedema.
Its specificity is higher compared to MDCT and conventional radiology in the differential diagnosis between osteoporotic and malignancy pathological fracture.
Bone scintigraphy is complementary to MRI in detecting occult fractures, crucial in finding metastatic disease in other locations.
Ultrasound is used in limited districts, and its role is confined to the relief of cortical interruption in the fractured bone segment.
In the future, technological advances with three-dimensional techniques (hr-CT, hr-MRI) may improve in vivo the diagnostic potential with an earlier detection of the ultrastructural alterations that predispose to the risk of bone fracture.
Keywords: Osteoporosis, NHNV fractures.
Fractures classification
A bone fracture occurs when bone elastic strength is overcome; it is determined by both extrinsic factors (high and low energy mechanical stress) and intrinsic factors, such as bone density, macroarchitecture and cortical-trabecular geometry, trabecular microarchitecture, matrix composition and characteristics of turnover (1).
From an etiological point of view, bone fractures are divided into: by efficient trauma, by stress and pathologic fractures insufficiency and tumorous fractures (2).
Stress fractures occur when a normal bone is subjected to abnormal mechanical stress; pathologic fractures occur when a structurally altered bone undergoes a normal mechanical stress.
The most common causes of pathological fracture are:
- Tumors (benign, primitive malignant tumors, metastasis and pseudotumoral lesions) (3)
- Primitive and Secondary Osteoporosis
- Metabolic bone diseases (osteomalacia, hyperparathyroidism, M. Paget, etc.)
- Joint infections and inflammations
- Radiotherapy.
Epidemiology
In 1994 the World Health Organization (4) established that severe osteoporosis is diagnosed when a value of T score <-2.5 SD obtained with DXA is associated with the presence of one or more fragility fractures (4, 5).
As a large number of fractures occurs in subjects with T-score above -2.5, to reflect entirely the spectrum of severity of this condition, a new definition of severe osteoporosis proposes to consider not only densitometric measurements, but also the number and severity of fragility fractures (6).
Fractures are the most serious consequence of osteoporosis and occur when negligible mechanical stresses are applied on a bone with low bone mineral density and deterioration of the microarchitecture.
The typical sites of osteoporosis fracture (Table 1) are hip, vertebra and wrist, but they obviously are not the only affected. Kanis et al. described as osteoporotic the fracture which occurs in a place with a low bone mineral density (BMD) and which determines an increase in its incidence in individuals over 50 years; a table of locations was therefore drawn up in order of decreasing frequency (7).
Table I.
- (from Kanis et al. 2001 modified).
| Common sites of osteoporotic fractures: |
| - Vertebral |
| - Hip |
| - Wrist-Forearm |
| Other sites: |
| - Homer |
| - Other femoral |
| - Rib |
| - Pelvic (pelvis and sacrum) |
| - Tibia and Fibula |
| - Foot: Metatarsal bone and Calcaneum |
| - Clavicle, Scapula, Sternum |
Ankle fractures are more difficult to place among those by osteoporosis: the incidence does not increase with age and they are associated with alteration of biomechanical factors (i.e. twisting force and abnormal loading, such as overweight), not with BMD decrease (8).
Importance of Non-Hip Non-Vertebral (NHNV) Fractures
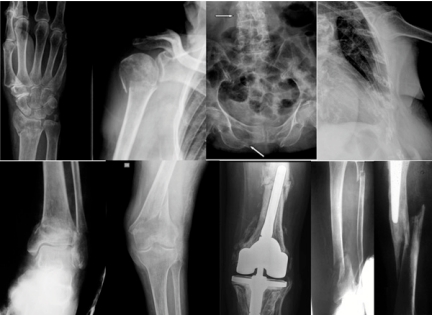
(Figure 1) European and American Studies (9,10) found that overall health care costs of non-hip non-vertebral fractures exceed those for femoral and vertebral fractures because the incidence of first is greater and because they occur in a segment of the population aged between 50 and 65 years, period of employment (10). Although peripheral fractures have a lower per-patient cost than hip and vertebral fractures, women with fracture of distal radius, humerus, ankle and foot spend a consistent period of incapacity, so NHNV fractures cost 1/3 of health expenditure attributed to osteoporotic fractures (9).
Figure 1.
- NHNV most common sites of fractures.
This type of fracture closely related to a condition of osteoporosis is therefore likely to have inadequate diagnosis and therapy.
Assignment of the clinician and the radiologist is to recognize when non-hip non-vertebral fractures are attributable to bone fragility in order to properly characterize and treat them.
Diagnostic Imaging
The key role of Diagnostic Imaging is:
- relief of the fracture
- characterization of the fracture
- representation of fracture for treatment planning
- evaluation of the healing process
- relief and monitoring of complications
Diagnostic Imaging emploies different techniques: first of all conventional X-rays, fundamental imaging investigation used on skeleton, easily available and low cost. More advanced 3D-techniques make use of multiplanar reconstructions: Multidetector Computed Tomography (MDCT), with elevated spatial resolution and wide field of view, Magnetic Resonance Imaging (MRI) with high contrast resolution and ability to characterize different tissues. A secondary role is played by Bone Scintigraphy and Ultrasound.
Conventional X-ray
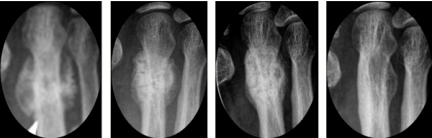
Conventional radiology is the method of first instance and crucial in the diagnosis of fracture. A radiographic evaluation for a suspected fractured shall include two standard projections, antero-posterior and lateral, in the case of long bone, to highlight any features of dislocation, cortical interruption and misalignment. Oblique projections can be useful in doubtful case or in absence of clear fracture lines. Primary objective for conventional radiology becomes the bone callus monitoring. Standard radiographs allow fracture follow up through different stages of healing during the treatment, either conservative or surgical.The stages of bone healing are (Figure 2): Enlargement of fracture line with blurred edges
Figure 2.
- Bone healing stages of metatarsal bone fracture monitored by plain radiographs.
- Appearance of peripheral amorphous calcification in the callus surrounding the fracture line
- Increase the quantity and density of callus that grows towards the edge of fracture
- Bone bridges formation in the callus until line obliteration.
The appropriate treatment planning, especially surgical fixation, must take in account that postmenopausal and senile osteoporosis alters some of the biomechanical factors which are important for bone healing process (11).
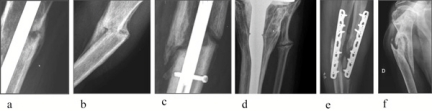
The bone repair process may result in: union, delayed union, non-union (hypertrophic and atrophic) or pseudoarhtrosis (12) (Figure 3).
Figure 3.
- Bone repair types: a) union; b) malunion; c) delayed union; d) non-union (pseudoarthrosis); e) atrophic pseudoarthrosis. f) ipertrophic pseudoarthrosis.
Therefore, a fundamental point is that the evaluation of bone healing must include either radiographic methods (bone callus monitoring until complete morphostructural repair) and clinical parameters, such as resolution of pain/tenderness when bearing weight and fracture stiffness evaluation (13),
Conventional Radiology shows limits in detecting fracture lines in critical locations, such as pelvis and middle-foot with complex anatomy for the overlap of intestinal loops or multiple skeletal segments.
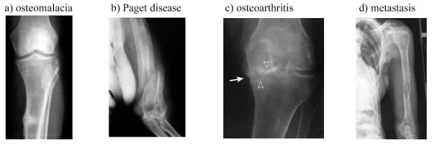
Moreover, conventional radiographs can fail in the differential diagnosis of diseases causing bone transparency and fracture lines, when radiological signs are not pathognomonic (such as those of osteomalacia, Paget disease, some malignant lesions), so that malignant fractures can be misinterpreted (Figure 4).
Figure 4.
- Fractures are easily characterized by plain radiographs when pathognomonic signs are present.
Multidetector Computed Tomography (MDCT)
Computed tomography, with its intrinsic characteristic of high spatial resolution and wide field of view, is a very useful technique for visualizing occult fractures (Figure 5), its diagnostic accuracy is high in representing the size of fracture line and its extension to the joint surface.
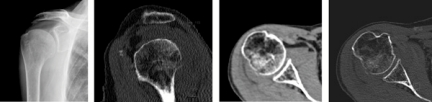
Figure 5.
- Fine cortical interruption of homerus head seen only in CT scans; joint effusion with fluid level image noticeable also in the plain radiograph
Multiplanar and three-dimensional reconstructions can provide synthetic images of fracture lines in their complete extension, bone fragments placement and also potential environment of joint surface which are all essential elements for therapeutic strategy (Figure 6).
Figure 6.
- Joint surface interruption and fragments’ placement are well defined by reformatted 2D and 3D images, helpful to the orthopedic surgeon for therapeutic strategy.
The limit of this technique is lack of sensitivity in demonstrating fracture line on an extremely rarefied bone background.
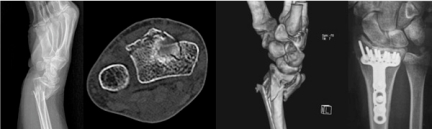
Moreover MDCT is the primary imaging tool for bone healing evaluation as it relieves clearly bone bridging by axial scans integrated by 2D reformatted images (Figure 7).
Figure 7.
- MDCT shows the absence of bone bridging – non union outcome – at distal ulna fracture, not evident in plain radiograph.
In case of suspected pathologic fracture by a malignant process, CT is fundamental to identify both bone tissue destruction and the associated soft tissue mass. CT is the first method used to distinguish insufficiency fracture of the pelvis from metastatic disease (14).
At the same time, volume coverage in spiral acquisition provided by MDCT identify primitive malignancy and allow tumor stadiation detecting other secondary lesions when metastatic bone diseases are recognized.
Not less important is the employment of CT-guided biopsy procedure for the histological characterization of bone lesions whose nature cannot be determined by imaging techniques (Figure 8).
Figure 8.
- CT-guided biopsy.
Magnetic Resonance Imaging (MRI)
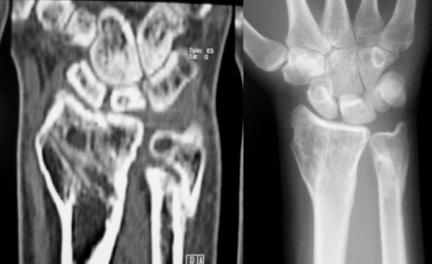
Magnetic Resonance assumes great importance because of its high sensitivity in assessing even slight structural alterations of tissues, especially cancellous bone. The possibility of multi-parametric and multi-planar acquisition allows to visualize both the fracture line (Figure 9) and above all cancellous bone and surrounding soft tissues oedema, (Figure 10) so that MRI is particularly important in early diagnosis of occult insufficiency fracture. This technique becomes crucial in the differential diagnosis of acute pain causes, such as osteoporotic fracture, malignant fracture, algodystrophy, osteonecrosis, osteomyelitis.
Figure 9.
- Calcaneal insufficiency fracture. Sagittal T1-weighted image shows irregular linear band of low signal intensity, representing an insufficiency fracture of the calcaneus.
Figure 10.
- a) A transverse short tau inversion recovery (STIR) image reveals high signal intensity in metatarsal diaphisis and extraosseus soft tissues. c) Coronal STIR acquisition shows a linear fracture of the epiphysis tibial surrounded by extensive
MRI provides a correct evaluation of bone and soft tissues lesions and it’s useful to quantify bone damage extension for planning treatment (Figure 11).
Figure 11.
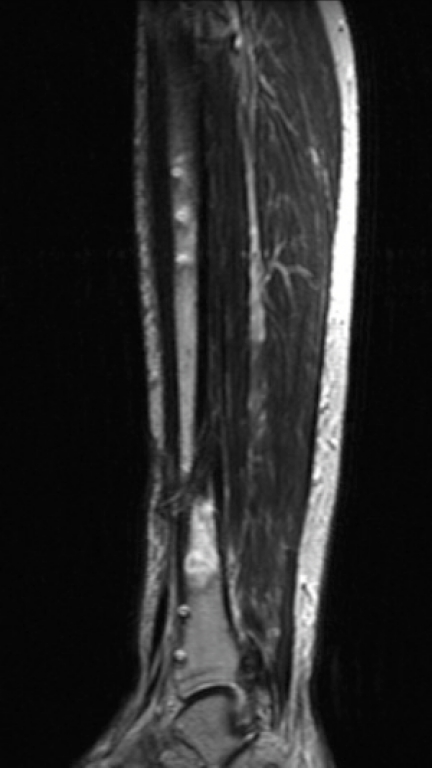
- Sagittal T2-weighted image displays non-union of the tibial diaphisis and area of high signal intensity in the distal fracture fragment which is the expression of inflammatory complication.
Compared to CT and plain radiographs, MRI is more specific in the differential diagnosis between insufficiency fracture and other pathological fractures due to malignant disease (15).
Recent studies (16) show that diffusion-weighted MRI sequences could differentiate benign from malign lesions, although this finding has till now found greater application in spine and pelvis.
Scintigraphy
Scintigraphy with technetium-99m or analogues radioactive molecules may show focal lesions of any skeletal site. However, the radionuclide uptake occurs in presence of any condition of altered bone turnover, such as fractures, cancer, arthritis, infection, Paget’s disease, hiding or simulating a malignant disease. Therefore this method has high sensitivity but low specificity; atypical patterns of radionuclide uptake can be difficulty interpreted as an insufficiency fracture, as the uptake can be hold for several months after a trauma. Occult fractures not evident with conventional X-Rays may be detected by bone scan after 3-5 days after trauma. It must be remembered that in pathologic fracture caused by malignancy, Scintigraphy is important to detect metastatic and metabolic bone lesions in other body sites.
A typical sacral and pubic uptake is found in an osteoporotic fracture when pathognomonic “H-shaped” morphology is observed (15) (Figure 12).
Figure 12.
- MIP reconstruction shows sacral and pelvic fracture “H” shaped and old rib fractures. Bone scintigraphy also allows optimal visualization of a new rib fracture.
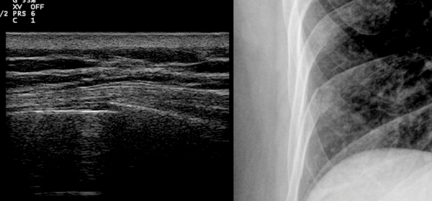
Ultrasonography
Ultrasonography is easily approachable and low cost; its role is limited to certain skeletal districts when plain radiographs don’t show the fracture line (e.g. rib fractures). This technique is capable to detect small cortical bone interruption in typical sites as distal radius, metatarsal bone and calcaneum earlier than MRI or Scintigraphy (17, 18). This method presents the intrinsic limit of the only evaluation of cortical profile, which should be considered in association with operator experience and the difficulty of monitoring bone healing (particularly in patients with cast) (Figure 13).
Figure 13.
- Ultrasound of the rib reveals focal interruption of hyperechoic layer corresponding to cortical profile and slight effusion in contiguous soft tissues.
Advanced 3D techniques in assessing bone status
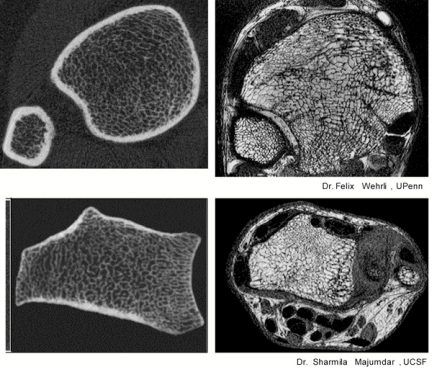
Considerable progresses have been made in the development of 3D methods for visualizing in vivo bone microarchitecture so that, in a patient with severe osteoporosis fracture, high spatial resolution techniques - hr-CT and hr-MR- can demonstrate the real rarefaction rate of cancellous bone and the cortical thickness decrease, essential elements for bone status evaluation (see Figure 14). These new sophisticated diagnostic imaging combined with finite element analysis used for clinical research will enhance the comprehension of biomechanical parameters and will improve the prediction of fragility fractures (19, 20).
Figure 14.
- Hr-CT and hr-MR can provide excellent representation of real trabecular structure and are able to predict fracture risk in porotic bone with good accuracy.
Conclusion
NHNV fractures have an important social and economic impact, considering the long inability periods they cause in working population; their global health cost is higher than hip and vertebral fractures, even if their cost per-patient is lower. First detection of fragility fracture in the majority of cases is made by standard radiographs; they are also helpful in monitoring bone healing.
MDCT (more used) and MRI (less employed) are more sensitive in the diagnosis of occult or complex fractures and in the differential diagnosis of their origin. CT scans show a better placement of bone fragments and a better view of bone bridging; they visualize bone disruption and extra-skeletal pathologic tissue in case of malignancy and allow tumor stadiation. MRI, with dedicated sequences, provides an accurate depiction of fracture line and optimally demonstrates cancellous bone and surrounding soft tissue oedema; it is the examination of choice in differential diagnosis between benign and malignant diseases and in evaluation of lesion spread and involvement of bone and soft tissues in pathological fractures complications.
Scintigraphy and Ultrasonography are less important in fragility facture diagnosis, but they can be useful if applied in particular cases.
Hr-CT and hr-MRI, till now used for clinical research, provide subtle visualization of bone architecture allowing a better assessment of bone status and prediction of fracture risk.
References
- 1.Newitt DC. In vivo assessment of architecture and micro-finite element analysis derived indices of mechanical properties of trabecular bone in the radius. Osteoporos Int. 2002 Jan;13(1):6–17. doi: 10.1007/s198-002-8332-0. [DOI] [PubMed] [Google Scholar]
- 2.Pentecost RL, Murray R, Brindley HH. Fatigue, insufficiency and pathologic fractures. Jama. 1964;187(1001) doi: 10.1001/jama.1964.03060260029006. [DOI] [PubMed] [Google Scholar]
- 3.Resnick D. Bone and Joint Disorders. Traumatic disorders. 2002;3(Section XV):2643–2670. [Google Scholar]
- 4.Johnell O, Kanis J. Epidemiology of osteoporotic fractures. Osteoporos Int. 2005;16:S3–S7. doi: 10.1007/s00198-004-1702-6. [DOI] [PubMed] [Google Scholar]
- 5.World Health Organization. Assessment of fracture risk and its application to screening for post menopausal osteoporosis. Technical Report Series; WHO; Geneva. 1994. [PubMed] [Google Scholar]
- 6.Nuti R, Brandi ML, et al. New perspectives on the definition and the management of severe osteoporosis: the patient with two or more fragility fractures. J Endocrinol Invest. 2009 Oct;32(9):783–8. doi: 10.1007/BF03346537. [DOI] [PubMed] [Google Scholar]
- 7.Kanis JA, et al. The burden of osteoporotic fractures: a method for setting intervention thresholds. 2001. Osteoporos Int. 12:417–427. doi: 10.1007/s001980170112. [DOI] [PubMed] [Google Scholar]
- 8.Guggenbuhl P, et al. Osteoporotic fractures of the proximal humerus, pelvis and ankle: epidemiology and diagnosis. Joint Bone Spine. 2005;72:372–5. doi: 10.1016/j.jbspin.2004.04.002. [DOI] [PubMed] [Google Scholar]
- 9.Delmas PD, et al. Beyond hip: importance of other nonspinal fractures. Am J Med. 2007 May;120(5):381–7. doi: 10.1016/j.amjmed.2006.06.003. [DOI] [PubMed] [Google Scholar]
- 10.Shi N, et al. Direct healthcare costs of hip, vertebral, and non-hip, non-vertebral fractures. Bone. 2009;45(6):1084–90. doi: 10.1016/j.bone.2009.07.086. [DOI] [PubMed] [Google Scholar]
- 11.Augat P, Simon U, Liedert A, Claes L. Mechanics and mechano-biology of fracture healing in normal and osteoporotic bone. Osteoporos Int. 2005 Mar;16(2):S36–43. doi: 10.1007/s00198-004-1728-9. [DOI] [PubMed] [Google Scholar]
- 12.Rockwood and Green’s Fracture in Adults. 2006;1(Chapt. 8):297, 311. [Google Scholar]
- 13.Corrales LA, et al. Variability in the assessment of fracture–healing in orthopaedic trauma studies. J Bone Joint Surg Am. 2008;90:1862–8. doi: 10.2106/JBJS.G.01580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hauge MD, et al. Insufficiency fractures of the pelvis that simulate metastatic disease. Mayo Clin Proc. 1988 Aug;63(8):807–12. doi: 10.1016/s0025-6196(12)62361-1. [DOI] [PubMed] [Google Scholar]
- 15.Krestan C, Hojreh A. Imaging of insufficiency fractures. European Journal of Radiology. 2009;71:398–405. doi: 10.1016/j.ejrad.2008.04.059. [DOI] [PubMed] [Google Scholar]
- 16.Herneth AM, et al. Diffusion weighted imaging of bone marrow pathologies. European Journal of Radiology. 2005;55:74–83. doi: 10.1016/j.ejrad.2005.03.031. [DOI] [PubMed] [Google Scholar]
- 17.Arni D, et al. Insufficiency fracture of the calcaneum Sonographic findings. J Clin Ultrasound. 2009 Sep;37(7):424–7. doi: 10.1002/jcu.20577. [DOI] [PubMed] [Google Scholar]
- 18.Banal F, et al. Sensitivity and specificity of ultrasonography in early diagnosis of metatarsal bone stress fracture: a pilot study of 37 patients. J Rheum. 2009;36(8):1715–19. doi: 10.3899/jrheum.080657. [DOI] [PubMed] [Google Scholar]
- 19.D’Elia G, et al. Bone fragility and imaging techniques. CCMBM. 2009;6(3) [PMC free article] [PubMed] [Google Scholar]
- 20.Bouxsein M. Bone quality: where do we go from here? Osteoporos Int. 2003;14(5):S118–S127. doi: 10.1007/s00198-003-1489-x. [DOI] [PubMed] [Google Scholar]