Abstract
In the diagnosis of femoral fractures, Radiodiagnostic has a role in the different phases of the natural history of these lesions:
- in diagnosis and characterization of fractures,
- in follow up of the efficacy of therapy, evolution of fractures and any complications,
- in studies of risk factors of fractures.
Diagnostic imaging employs method of investigation as Conventional Radiology, still crucial in detection, characterization and control of fracture, Computed Tomography (CT) and Magnetic Resonance (MR), essential in doubt of occult fracture and in differential diagnosis between the possible causes of pathologic fracture. Finally, Dual X-ray Absorptiometry (DXA is still the fundamental methodic in diagnosis and assessment of osteoporosis, while QCT, pQCT and HR-CT are experimental techniques used to study in vivo bone microarchitecture and its metabolic and pathological changes.
Keywords: osteoporosis fractures, radiodiagnostic and fractures, occult fractures.
Introduction
Hip fracture is a bone injury of soaring importance because of its increasing incidence and relative mortality and morbility rates as well as management costs. In 2002, in Italy 85.000 admissions in Hospitals for proximal femur fractures were estimated in patients over 45 years of age, 77% women, with respective total costs approximately of 1.097.000.000 euros (1). Diagnostic imaging in proximal femur fractures is usually involved in these circumstances: diagnosis and characterization of traumatic injuries, follow up of treatments and possible complications and finally in studies of risk factors, in particular structural characteristics and mechanical properties of bone.
Considering that in the vast majority of cases fragility hip fracture is a proximal femur fracture, we will principally treat about lesions localized at this part of femur.
Diagnosis and characterization of fractures
Fractures of the proximal femur generally occur at level of neck (subcapital, transcervical and basicervical fracture) and trochanteric region (trochanteric, pertrochanteric, and subtrochanteric fracture).
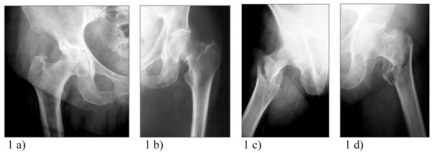
In detection and characterization of femur fractures, Conventional Radiology represents still now the capital method of investigation in bone study for simplicity, low cost and availability in all Radiodiagnostic Units. With correct projections, X-Ray allows diagnosis and characterization of fracture injuries, according to their localization (intra- or extracapsular) and type of fragments: these factors determine the prognosis (i.e. intracapsular fractures have an high incidence of avascular necrosis) and the surgical treatment planning (i.e. screws, nails or prosthesis) (Fig.1).
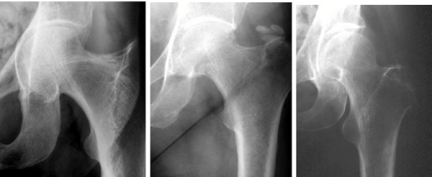
Figure 1.
- Osteoporotic proximal femur fractures: a) proximal femoral neck fracture b) middle femoral neck fracture c) basilar femoral neck fractures d) inter and subtrochanteric fracture.
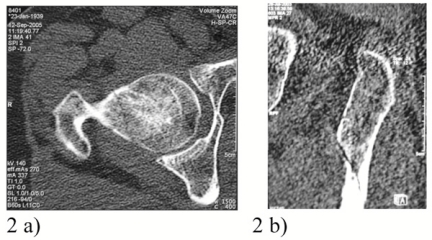
In acute phase, femur fractures may be not always easily detectable by a radiographic examination: when we suspect an occult fracture, we must consider further investigations such as CT and MRI (2,3). Computed Tomography, now commonly available in emergency rooms, is the method of investigation with higher spatial resolution and could evidence even subtile interruption of cortical bone in cases of compound fracture (Fig.2).
Figure 2.
- CT scan imaging a) not displaced femoral neck fracture b) non displaced subtrochanteric spiroid fracture.
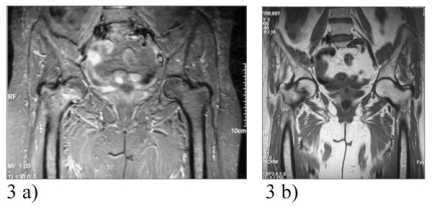
MRI is the method of investigation with higher contrast resolution, able to detect early edema and bleeding of bone narrow, always present in even minimal bone injuries; though less immediate for limited availability and costs, MRI allows to evaluate not only bone but also eventually associated muscle, tendon and cartilage lesions (4-6) (Fig.3).
Figure 3.
- MR imaging a) edema of not displaced femoral neck fracture in a fat-suppressed sequence b) borders of the same not displaced femoral neck fracture in a T1-weighted sequence.
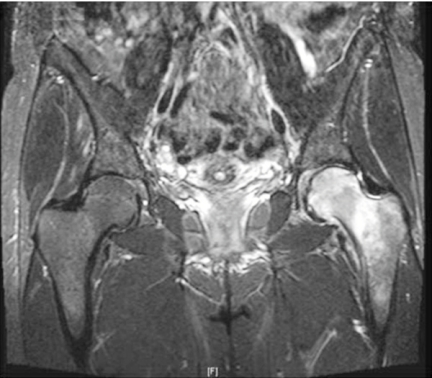
Intravenous medium contrast in MRI is indicated in case of differential diagnosis between fragility and neoplastic fractures. Moreover, in some recent experiences, medium contrast is used to assess femoral head vascularization in subacute phase of intracapsular femoral neck fractures, to predict the risk of avascular necrosis of femoral head (7,8) (Fig.4).
Figure 4.

CT reconstruction of pathologic fracture of femoral neck.
All the above-mentioned methods of investigation are employed also to follow-up treatments and complications of fractures. X-rays are most commonly used to evaluate bone healing the fixation devices (cannulated screws, intramedullary nails, prosthesis, etc.) applied; along with CT and MRI, x-rays, are used in detection and assessment of fractures complications i.e. devices mobilization, non union and infection (Figs.5-8).
Figure 5.
- MR imaging (IR fat-suppressed sequence) of pathologic basilar femoral neck fractures.
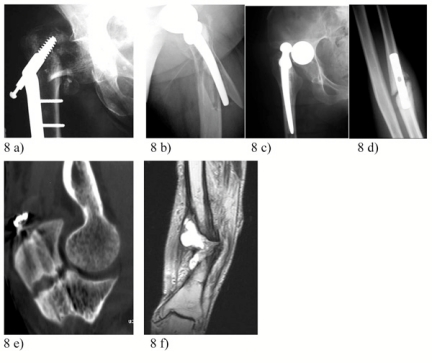
Figure 8.
- Complications of surgical treatment: a) through-cut of plates, b) fracture in limb with prothesis, c) arthroprothesis dislocation, d) non union, e) CT control of a delayed union, f) MRI evidence of osteomyelitis and pseudoarthrosis.
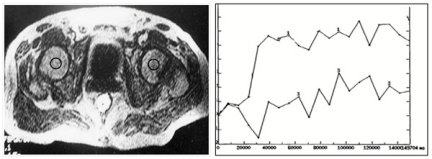
Figure 6.
- Post-fracture contrast enhancement evaluation of femural heads.
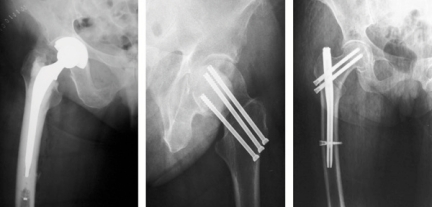
Figure 7.
- X-ray examples of osteosynthesis a) arthroprothesis b) cannulated screws c) intramedullary nailing.
Evaluation of bone fragility
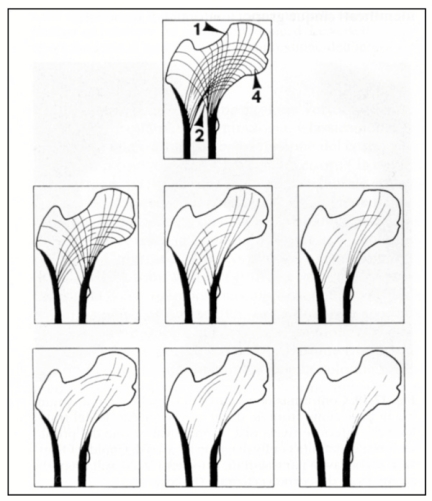
Diagnostic imaging is finally involved in the evaluation of all the morphostructural changes that increase bone fragility, increasing the risk of fractures, the most common of which is osteoporosis (9). Conventional radiology is not an effective method for evaluate osteoporosis, because it only detects more than 30% loss of bone mass radiology is however the base of historical semiquantitative methods such as Singh index that considers gradual depletion of trabecular systems such as primary and secondary compressive and tensive groups present between the epiphysis and metaphysis of proximal femur (Fig.9).
Figure 9.
- Singh index.
The most important exam for effectiveness, low-cost and diffusion to early detect osteoporosis is DXA (Dual X-ray Absorptiometry) that elaborates the absorption curve of a dual energy beam of photons passing through body sites like hip, lumbar spine and distal radio, determininig its Bone Mineral Density (BMD), expressed in g/cm2. WHO defines osteoporosis when BMD is 2.5 times below the peak of bone mass (T-score> -2.5 SD) as this value is significantly correlated with an increased risk of fracture. DXA presents important limits: the areal density (aBMD) is not the real density (expressed in g/cm3); aBMD values may be altered by the presence of arthritis, previous fracture, Paget’s disease etc.; DXA can not distinguish between trabecular and cortical bone; bone structure is not taken in account (Figs.10-11).
Figure 10.
- Progressive trabecular bone rarefaction.
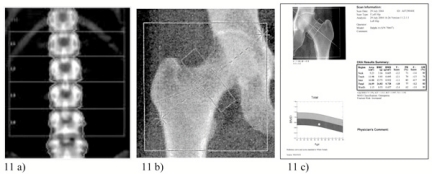
Figure 11.
- DXA: a) lumbar spine scan; b) proximal femur scan; c) BMD results.
To overcome these limitations, clinical trials make use of equipments and specific softwares such as QCT, p-QCT (Quantitative Computed Tomography and peripheral-Quantitative Computed Tomography) vQCT (volumetric-Quantitative Computed Tomography) and High Resolution-pQCT (HR-pQCT) that evaluate volumetric bone density in mg/mm3 of bone, separating trabecular from cortical component and reducing possible artifacts. The limits are represented by the limited availability, costs and, in some cases, the radiation dose to patient (10-15) (Fig.12).
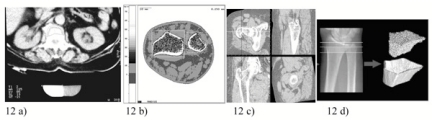
Figure 12.
- a) Lumbar QCT b) radial pQCT evaluation; c) mechanical properties evaluation by vQCT; d) HR-pQCT of distal radius.
References
- 1.Rossigni M, Piscitelli P, Fitto F, et al. Incidenza e costi delle fratture di femore in Italia. Incidence and socioeconomic burden of hip fractures in Italy. Reumatismo. 2005;57(2):97–102. doi: 10.4081/reumatismo.2005.97. [DOI] [PubMed] [Google Scholar]
- 2.Hossain M, Barwick C, Sinha AK, et al. Is magnetic resonance imaging (MRI) necessary to exclude occult hip fracture? Injury. 2007 Oct;38:1204–8. doi: 10.1016/j.injury.2007.04.023. [DOI] [PubMed] [Google Scholar]
- 3.Sankey RA, Turner J, Lee J, et al. The use of MRI to detect occult fractures of the proximal femur: a study of 10 consecutive cases over a ten-year period. J Bone Joint Surg Br. 2009 Aug;91(8):1064–8. doi: 10.1302/0301-620X.91B8.21959. [DOI] [PubMed] [Google Scholar]
- 4.Dupuis MG, Moussaoui A, Douzal V, et al. Imaging of traumatic injuries of the hip. J Radiol. 2007 May;88(5 Pt 2):760–74. doi: 10.1016/s0221-0363(07)91343-8. [DOI] [PubMed] [Google Scholar]
- 5.Hong RJ, Hughes TH, Gentili A, et al. Magnetic resonance imaging of the hip. J Magn Reson Imaging. 2008 Mar;27(3):435–45. doi: 10.1002/jmri.21124. [DOI] [PubMed] [Google Scholar]
- 6.Cabarrus MC, Ambekar A, Lu Y, et al. MRI and CT of insufficiency fractures of the pelvis and the proximal femur. AJR Am J Roentgenol. 2008 Oct;191(4):995–1001. doi: 10.2214/AJR.07.3714. [DOI] [PubMed] [Google Scholar]
- 7.Kaushik A, Sankaran B, Varghese M. To study the role of dynamic magnetic resonance imaging in assessing the femoral head vascularity in intracapsular femoral neck fractures. Eur J Radiol. 2009 Jul 20; doi: 10.1016/j.ejrad.2009.04.045. [DOI] [PubMed] [Google Scholar]
- 8.Kaushik A, Sankaran B, Varghese M. Prognostic value of dynamic MRI in assessing post-traumatic femoral head vascularity. Skeletal Radiol. 2009;38:565–569. doi: 10.1007/s00256-009-0667-0. [DOI] [PubMed] [Google Scholar]
- 9.Gnudi S, Sitta E, Fiumi N. Bone density and geometry in assessing hip fracture risk in post-menopausal women. Br J Radiol. 2007 Nov;80(959):893–7. doi: 10.1259/bjr/37401526. [DOI] [PubMed] [Google Scholar]
- 10.Clowes JA, Eastell R, Peel NF. The discriminative ability of peripheral and axial bone measurements to identify proximal femoral, vertebral, distal forearm and proximal humeral fractures: a case control study. Osteoporos Int. 2005;16:1794–1802. doi: 10.1007/s00198-005-1931-3. [DOI] [PubMed] [Google Scholar]
- 11.Ciarallo A, Barralet J, Panzer M, et al. An approach to compare the quality of cancellous bone from the femoral necks of healthy and osteoporotic patients through compression testing and microcomputed tomography imaging. MJM. 2006;9(2):102–107. [PMC free article] [PubMed] [Google Scholar]
- 12.Genant HK, Engelke K, Prevrhal S. Advanced CT bone imaging in osteoporosis. Rheumatology. 2008;47:9–16. doi: 10.1093/rheumatology/ken180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wu SY, Jia HH, Hans D, et al. Assessment of volumetric bone mineral density of the femoral neck in postmenopausal women with and without vertebral fractures using quantitative multi-slice CT. J Zhejiang Univ Sci B. 2009;10(7):499–504. doi: 10.1631/jzus.B0820409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Adams JE. Quantitative computed tomography. European Journal of Radiology. 2009;71:415–424. doi: 10.1016/j.ejrad.2009.04.074. [DOI] [PubMed] [Google Scholar]
- 15.Wu S, Ji H, Hans D, et al. Assessment of volumetric bone mineral density of the femoral neck in postmenopausal women with and without vertebral fractures using quantitative multi-slice CT. J Zhejiang Univ Sci B. 2009;10(7):499–504. doi: 10.1631/jzus.B0820409. [DOI] [PMC free article] [PubMed] [Google Scholar]