Abstract
Purpose
To evaluate the long-term safety of polyethylene glycol (PEG) 4000 in children with constipation, particularly the biochemical aspects of safety.
Methods
Medical records were evaluated, and 100 children, who had been taking PEG 4000 for more than 6 months, and who had been under clinical and biochemical monitoring, were enrolled. Ages; 6.11±3.12 years, Duration of therapy; 16.93±7.02 months, dose of PEG 4000; 0.72±0.21 g/kg/d.
Results
None of the children complained of clinical adverse effect. The first biochemical test was performed at 8.05 months after beginning of PEG 4000. Serum phosphate (SP) value was high in 10 children, and leucopenia was noted in one child. The second test was performed in 44 children at 7.57 months after the first test. The SP value was high in four children, including the three children whose initial SP value was high and one new child. Six out of 10 children with high initial SP value became normal and one was lost. Hypernatremia was noted in one child. The third test was done in 15 children at 7.5 months after the second test. The SP value of the new child from the second test was high, but became normal after finishing treatment. Two out of 3 children with high SP value at the second test became normal and one was lost. The fourth test was done in 2 children few months after the third test. All of the results were normal. There were no relation between duration of therapy and hyperphosphatemia, or between dose of PEG 4000 and hyperphosphatemia.
Conclusions
PEG 4000 is safe for long-term therapy in children with constipation with respect to biochemical parameters.
Keywords: Child, Constipation, Polyethylene Glycol 4000, Safety
Introdction
Various medications can be applied to children with chronic constipation, and lactulose/sorbitol, mineral oil, and magnesium hydroxide have been considered to be safe for long-term use in children1-3). Recently, polyethylene glycol (PEG) products for children gained in public favor. PEG 3350 solution with electrolytes was introduced for colonoscopic preparation in the late 1990's, and for disimpaction in children with chronic constipation4, 5). However, use of a large amount of PEG 3350 solution with electrolytes imposes some limitations, given its awful taste and potential risk for causing electrolyte imbalance in children. Recently, PEG products without electrolytes have been introduced for children with constipation in order to overcome the problems of PEG with electrolytes6-11).
Concern about the long-term safety of PEG without electrolytes products in children with chronic constipation is one of the most important issues now. However, there are very few studies on the long-term safety of PEG products without electrolytes in children with chronic constipation that address both clinical and biochemical aspects. Those studies that have been performed are mainly on PEG 3350 from North America, and the duration of the studies is about one year6, 7, 11-13), while studies of PEG 4000 are even rarer and the duration of the latter studies is not long8-10, 14). In the present study, the long-term safety of PEG 4000 was evaluated with a large number of children and for a long time, focusing on the biochemical aspect of treatment safety.
Materials and methods
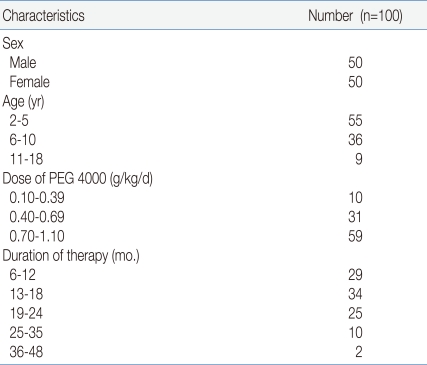
Medical records were evaluated {350 children, 153 boys, 197 girls, mean age 8.43±4.56 yr (2-19)} and children who had been taking PEG 4000 (Forlax®, Beaufour Ipsen Pharma., Paris, France) for more than 6 months, under the diagnosis of chronic constipation of ROME III criteria15), between July, 2007 and March, 2010 at Konkuk University Hospital, and who had been under clinical and biochemical monitoring, were enrolled. One hundred of children (50 boys, 50 girls) were enrolled in this study. Their ages were 6.11±3.12 years (2-17 years), and the duration of the therapy was 16.93±7.02 months (7-46 months) and the initial maintenance dose of PEG was 0.72±0.21 g/kg/d (0.18-1.14 g/kg/d) (Table 1).
Table 1.
The Demographic Features of the Children
Abbreviation: PEG, polyethylene glycol
The compliance and effect of medication were guaranteed with defecation diary which was kept by the patient or guardian. The children had been under clinical monitoring (urticaria, diarrhea, nausea, abdominal pain, headache, dizziness, tingling sensation, convulsion, change in consciousness)16-18), and biochemical monitoring, such as, complete blood count with reticulocyte, liver function test, glucose, blood urea nitrogen, creatinine, calcium, phosphate, electrolytes (including tCO2) and serum osmolality, per several months.
The relations between duration of therapy and hyperphosphatemia, and between dose of PEG 4000 and hyperphophatemia were evaluated with Student's t-test.
Results
During therapy, none of the children complained of clinical symptoms associated with PEG, such as urticaria, diarrhea, abdominal pain, headache, dizziness, numbness, seizure, or change of consciousness.
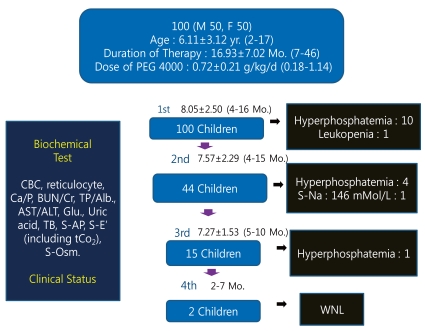
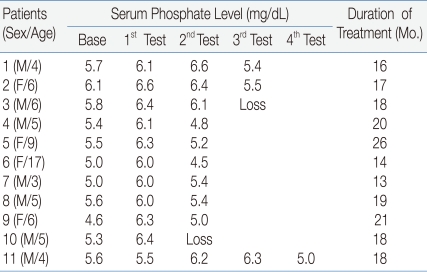
One hundred children underwent biochemical testing more than once. The first biochemical test was performed at 8.05±2.50 (4-16 months) after the beginning of the PEG 4000. Serum phosphate values were more than 6.0 mg/dL in 10 children, and leucopenia was noted in one child. The second test was performed in 44 children at 7.57±2.29 (4-15 months) after the first test. The serum phosphate value was more than 6.0 mg/dL in four children, including the three children with a high initial phosphate value and one new child. Six out of 10 children whose initial phosphate values were high became normal and one was lost. Serum sodium value was high in one child (146 mMol/L). The third test was done in 15 children at 7.27±1.53 (5-10 months) after the second test. Serum phosphate value of the new child from the second test was high, but became normal after finishing 2 more months of treatment. Two out of 3 children with high phosphate value at the second test became normal and one was lost. The fourth test was done in 2 children at 2-7.5 months after the third test. All of the results were normal (Fig. 1, Table 2).
Fig. 1.
Overall flow of the study. During polyethylene glycol (PEG) 4000 treatment for constipation in children, biochemical testing was performed serially. Hyperphosphatemia developed in some children, but most resolved spontaneously despite continuance of treatment except in one child. Abbreviations: CBC, Complete blood count; Ca, Calcium: P, Phosphorus; BUN, Blood urea nitrogen; Cr, Creatinine; TP, Total protein; Alb, Albumine; AST/ALT, Aspartate aminotransferase/Alanine aminotransferase; Glu, Glucose; TB, Total bilirubin; S-AP, Serum alkaline phosphatase; S-E', Serum electrolytes; S-Osm, Serum osmolarity.
Table 2.
The Change of Serum Phosphate Levels in Children with Hyperphosphatemia during PEG* 4000 Treatment for Constipation
Abbreviation: PEG, polyethylene glycol
Overall, 10% (11/100) of children who have been treated with PEG 4000 for more than 6 months experienced hyperphosphatemia during therapy. However, significant clinical problems were not noted in children with hyperphosphatemia.
The relations between duration of therapy and hyperphosphatemia (P=0.738), and between dose of PEG 4000 and hyperphosphatemia (P=0.384), were not statistically significant.
Discussion
Generally, the duration of treatment for functional constipation is considered to be 6 to 24 months3). Considering a long duration of therapy, the safety of the medicine is more important than the efficacy of the medication, when the pediatrician selects a drug for functional constipation in children. Lactulose/Sorbitol, mineral oil, magnesium hydroxide, and PEG have been considered to be safe for long-term use in children1-3). Furthermore, fiber can be included in this category, on the basis of theoretical consideration.
Lactulose and Sorbitol are non-absorbable disaccharides, and both are easily taken by children, although lactulose is contraindicated in children with galactosemia. Mineral oil is the most commonly used of the lubricant laxatives. A major concern about the long-term use of mineral oil has been that it may interfere with absorption of the fat-soluble vitamins. However, two studies have dismissed this concern19, 20). Magnesium hydroxide is the most commonly used magnesium salt. It can cause hypermagnesemia, hypophosphatemia, secondary hypocalcemia and volume overload in children with renal insufficiency and in young infants.
A few pediatric studies with PEG 3350 have revealed clinical side effects such as atopy, nausea, vomiting, and abdominal pain6, 7, 11-13). In one study with PEG 3350, biochemical follow-up was performed for 12 months, and mild elevation of AST was noted in some children12). A pediatric clinical study with PEG 4000 that was performed in France for 3 months revealed no significant problems clinically8), or biochemically14).
In the present study, 100 children were enrolled and the mean duration of treatment was about 17 months (7-46 months). Significant clinical problems were not noted during observation. Many biochemical parameters were analyzed, and the serum phosphate level was elevated in some children. Generally, serum phosphate increases in cases of acute, chronic renal failure, aggravated catabolic stress, lactic acidosis, hypocalcemia, cytolysis during chemotherapy, administration of a large quantity of phosphate, or hypoparathyroidism21). In the present study, the etiology of hyperphosphatemia remains unclear, and hyperphosphatemia resolved spontaneously despite continuance of treatment except in one child. Although the major human adverse event related to high PEG exposure is renal toxicity (acute renal tubular necrosis)22), the relationship between PEG 4000 at therapeutic dose (0.25-1.0 g/kg/d) and hyperphosphatemia warrants further study.
In pediatric studies with PEG 3350, mild elevation of AST was reported12). However, this phenomenon was not noted in the present study.
PEG 4000 is safe for long-term therapy in children with chronic constipation in terms of biochemical parameters. However, pediatricians are in need of biochemical follow-up, especially for serum phosphate.
Footnotes
This work was supported by the Konkuk University Medical Center Research Grant, (2008-3-05).
This article was presented at 11th Congress of the Asian Pan-Pacific Society of Pediatric Gastroenterology, Hepatology and Nutrition (2009).
References
- 1.Loening-Baucke V. Constipation and encoporesis. In: Wyllie R, Hyams J, editors. Pediatric gastrointestinal and liver disease. 3rd ed. Philadelphia: W.B. Saunders; 2006. pp. 177–191. [Google Scholar]
- 2.Rahhal R, Uc A. Functional constipation. In: Kleiman RE, Sanderson IR, Goulet O, Sherman PM, Mieli-Vergani G, Shneioder BL, editors. Walker's pediatric gastrointestinal disease. 5th ed. Hamilton: BC Decker Inc.; 2008. pp. 675–682. [Google Scholar]
- 3.Kim YM, Choi SY, Bae SH, Ahn YM. A clinical study of chronic functional constipation in children treated for more than five months. Korean J Pediatr. 2004;47:1186–1192. [Google Scholar]
- 4.So HS, Bae SH, Yoon HS, Hwang JS. Efficacy and safety of Polyethylene glycol (PEG) with electrolytes for disimpaction in children with chronic functional constipation. J Korean Pediatr Soc. 2003;46:1089–1094. [Google Scholar]
- 5.Ingebo KB, Heyman MB. Polyethylene glycol-electrolyte solution for intestinal clearance in children with refractory encoporesis. Am J Dis Child. 1988;142:340–344. doi: 10.1001/archpedi.1988.02150030114035. [DOI] [PubMed] [Google Scholar]
- 6.Youssef NN, Peters JM, Henderson W, Shultz-Peters S, Lockhart DK, Di Lorenzo C. Dose response of PEG 3350 for the treatment of childhood fecal impaction. J Pediatr. 2002;141:410–414. doi: 10.1067/mpd.2002.126603. [DOI] [PubMed] [Google Scholar]
- 7.Loening-Baucke V, Krishna R, Pashankar DS. Polyethylene glycol 3350 without electrolytes for the treatment of functional constipation in infants and toddlers. J Pediatr Gastroenterol Nutr. 2004;39:536–539. doi: 10.1097/00005176-200411000-00016. [DOI] [PubMed] [Google Scholar]
- 8.Dupont C, Leluyer B, Amar F, Kalach N, Benhamou PH, Mouterde O, et al. A dose determination study of polyethylene glycol 4000 in constipated children: factors influencing the maintenance dose. J Pediatr Gastroenterol Nutr. 2006;42:178–185. doi: 10.1097/01.mpg.0000189349.17549.a9. [DOI] [PubMed] [Google Scholar]
- 9.Lee JH, Lee R, Bae SH. Efficacy and safety of electrolytes-free polyethylene glycol (PEG) 4000 for disimpaction in children with chronic functional constipation. Korean J Pediatr. 2008;51:391–395. [Google Scholar]
- 10.Lee SH, Bae SH. Maintenance dose of electrolyte free polyethylene glycol (PEG) 4000 in Korean children with chronic functional constipation. Korean J Pediatr. 2007;50:1212–1216. [Google Scholar]
- 11.Loening-Baucke V. Polyethylene glycol without electrolytes for children with constipation and encopresis. J Pediatr Gastroenterol Nutr. 2002;34:372–377. doi: 10.1097/00005176-200204000-00011. [DOI] [PubMed] [Google Scholar]
- 12.Pashankar DS, Loening-Baucke V, Bishop WP. Safety of polyethylene glycol 3350 for the treatment of chronic constipation in children. Arch Pediatr Adolesc Med. 2003;157:661–664. doi: 10.1001/archpedi.157.7.661. [DOI] [PubMed] [Google Scholar]
- 13.Michail S, Gendy E, Preud'Homme D, Mezoff A. Polyethylene glycol for constipation in children younger than eighteen months old. J Pediatr Gastroenterol Nutr. 2004;39:197–199. doi: 10.1097/00005176-200408000-00014. [DOI] [PubMed] [Google Scholar]
- 14.Dupont C, Leluyer B, Maamri N, Morali A, Joye JP, Fiorini JM, et al. Double-blind randomized evaluation of clinical and biological tolerance of polyethylene glycol 4000 versus lactulose in constipated children. J Pediatr Gastroenterol Nutr. 2005;41:625–633. doi: 10.1097/01.mpg.0000181188.01887.78. [DOI] [PubMed] [Google Scholar]
- 15.Rasquin A, Di Lorenzo C, Forbes D, Guiraldes E, Hyams JS, Staiano A, et al. Child functional gastrointestinal disorders: Child/adolescent. Gastroenterology. 2006;130:1527–1537. doi: 10.1053/j.gastro.2005.08.063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Rose M, Jacob LS. Seizure associated with use of visicol for colonoscopy. N Engl J Med. 2002;347:295–296. doi: 10.1056/NEJM200207253470418. [DOI] [PubMed] [Google Scholar]
- 17.Schroppel B, Segerer S, Keuneke C, Cohen C, Schlondorff D. Hyponatremic encephalopathy after preparation for colonoscopy. Gastrointest Endosc. 2001;53:527–529. doi: 10.1067/mge.2001.113274. [DOI] [PubMed] [Google Scholar]
- 18.Baylis PH. Vasopressin and its neurophysin. In: DeGroot LJ, Besser GM, Gahill GF Jr, Marshall JC, Nelson DH, Odell WD, et al., editors. Endocrinology. 2nd ed. Vol.1. Philadelphia: W.B. Saunders; 1989. pp. 213–229. [Google Scholar]
- 19.Clark JH, Russel GJ, Fitzgerald JF, Nagamori KE. Serum beta-carotene, retinol, and alpha-tocoperol levels during mineral oil therapy for constipation. Am J Dis Child. 1987;141:1210–1212. doi: 10.1001/archpedi.1987.04460110080028. [DOI] [PubMed] [Google Scholar]
- 20.Sharif F, Crushell E, O'Driscoll K, Bourke B. Liquid paraffin: A reappraisal of its role in the treatment of constipation. Arch Dis Child. 2001;85:121–124. doi: 10.1136/adc.85.2.121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Contiguglia SR, Mishell JL, Klein MH. Electrolyte disorder. In: Friedman HH, editor. Problem oriented medical diagnosis. 3rd ed. Boston: Little, Brown and Company Inc.; 1983. pp. 250–256. [Google Scholar]
- 22.Webster R, Didier E, Harris P, Siegel N, Stadler J, Tilbury L, et al. PEGylated proteins: Evaluation of their safety in the absence of definitive metabolism studies. Drug Metab Dispos. 2007;35:9–16. doi: 10.1124/dmd.106.012419. [DOI] [PubMed] [Google Scholar]