Abstract
Maltreated children placed in out-of-home care are at high risk for exhibiting symptoms of psychopathology by virtue of their exposure to numerous risk factors. Research examining cumulative risk has consistently found that the accumulation of risk factors increases the likelihood of mental health problems. The goal of the current study was to elucidate the relation between cumulative risk and mental health symptomatology within a sample of 252 maltreated youths (aged 9–11) placed in out-of-home care. Results confirmed the high-risk nature of this sample and identified seven salient risk variables. The cumulative risk index comprised of these seven indicators was a strong predictor of mental health symptoms, differentiating between children who scored in the clinical range with regard to mental health symptoms and those who did not. Finally, the data supported a linear model in which each incremental increase in cumulative risk was accompanied by an increase in mental health problems. This is the first known study to examine cumulative risk within a sample of youths in out-of-home care.
Keywords: cumulative risk, maltreatment, out-of-home care, preadolescents, mental health
In 2006, 303,000 U.S. children entered out-of-home care, including court-ordered placement with non-relatives, with relatives in kinship care, or in residential treatment (U.S. Department of Health and Human Services, 2008). These children represent an extremely vulnerable segment of society. Children in out-of-home care have high rates of DSM-IV diagnoses (Garland et al., 2001; Harman, Childs, & Kelleher, 2000). The National Survey of Child and Adolescent Well-Being, a large-scale study of children involved in the child welfare system, found that nearly 50% of children aged 2 through 14 who were subjects of maltreatment reports investigated by child welfare agencies exhibited clinical levels of mental health symptoms (Burns et al., 2004). Mental health problems exhibited by these children persist into adulthood, with individuals maltreated as children being four to five times more likely than their non-maltreated counterparts to be hospitalized for suicide attempts or serious psychiatric disorders as young adults (Vinnerljung, Hjern, & Lindblad, 2006). These children are also at risk for other adverse outcomes in adulthood, including incarceration, unemployment, and homelessness (Courtney et al., 2005).
While children placed in out-of-home care are at elevated risk for mental health problems and adverse life outcomes, variability exists within this population; not all children in out-of-home care develop symptoms of psychopathology. Consequently, it is important to identify the subset of maltreated children who are at the greatest risk for developing mental health problems and those who are most likely to benefit from a prevention program, so resources are used efficiently and program benefits are maximized (Davis, MacKinnon, Schultz, & Sandler, 2003). The current study will use a cumulative risk approach to differentiate between levels of risk for mental health symptoms among maltreated children placed in out-of-home care.
The Ecology of Maltreatment
Risk factors contribute to the onset, severity, or duration of a disorder (Coie et al., 1993), and are hypothesized to exist and operate across multiple ecological levels (individual, family, sociocultural). Child maltreatment is a major risk factor for psychopathology in and of itself, as maltreatment, by definition, indicates serious malfunction in the environment most proximal to the child (Luthar, 2006). Maltreatment characteristics influence children's outcomes, with exposure to multiple maltreatment types increasing risk for emotional/behavior problems (Lau et al., 2005; Litrownik et al., 2005; Lynch & Cicchetti, 1998; Manly, Cicchetti, & Barnett, 1994). In addition, child maltreatment is associated with increased exposure to other risk factors, including poverty, high-risk neighborhoods, parental psychopathology, substance use, and domestic violence (Masten & Wright, 1998). Exposure to these additional risks predicts poorer outcomes for maltreated youths. For example, maternal alcohol use increases the likelihood that sexually abused female adolescents will exhibit maladaptive outcomes (Chandy, Blum, & Resnick, 1996), and family mobility is associated with poorer adjustment among maltreated youths (Eckenrode, Rowe, Laird, & Bradshaw, 2006).
Although family-related characteristics exert strong proximal influences, children develop in a number of ecological contexts outside of their immediate families (Bronfenbrenner, 1986). These ecological contexts also influence the development of maltreated children (Zielinski & Bradshaw, 2006). Multiple episodes of foster care placement are related to poorer child adjustment (Kurtz, Gaudin, Howing, & Wodarski, 1993). Similarly, transitions in caretakers and residences are related to behavior problems among maltreated adolescents (Herrenkohl, Herrenkohl, & Egolf, 2003). The sociocultural context may also serve to exacerbate the effects of child maltreatment. For example, rates of maltreatment are positively associated with children's reports of community violence, and exposure to community violence increases maltreated children's risk for depression and traumatic stress (Cicchetti & Lynch, 1998).
Of course, children are not simply products of their environmental contexts, and research indicates that personal characteristics of the child are an important class of vulnerability factors in the face of adversity. Child cognitive ability has long been recognized as an important protective factor (Masten et al., 1988). Conversely, research has also demonstrated that low intellectual functioning is associated with increased risk in the face of stress (Luthar, 1991).
Cumulative Risk
As demonstrated by the literature reviewed above, risk factors tend to amass within individuals (Masten & Wright, 1998). What often differentiates high-risk children from lower-risk children is the presence of multiple adversities in their life histories. Thus, researchers have considered the cumulative effects of these factors in a manner that may better characterize the lives of high-risk children. Cumulative risk indices are typically created by summing the number of hypothesized risk factors (coded as “present” or “absent”) in a child's background. A drawback to this strategy is that some information is sacrificed via the dichotomization of continuous measures of risk. For this reason, cumulative risk approaches do not take the place of research that identifies the mechanisms through which specific risk factors operate. However, the cumulative risk strategy permits simultaneous consideration of co-occurring risks, and numerous studies have demonstrated that the number of risk factors (cumulative risk) is a better predictor of a variety of developmental outcomes than any single risk factor (Appleyard, et al., 2005; Deater-Deckard, Dodge, Bates, & Pettit, 1998; Fergusson & Horwood, 2003; Gutman, Sameroff, & Cole, 2003). Children with high cumulative risk scores have worse outcomes than those with low cumulative risk scores, regardless of the specific risks that are included in the cumulative risk score (Deater-Deckard, et al., 1998; Sameroff et al., 1993), illustrating the impact of multiple risk exposure on development. Finally, one study found that the cumulative risk score was a better predictor of longitudinal outcomes than was a regression consisting of multiple continuously-measured risk variables (Deater-Deckard et al., 1998).
While research examining cumulative risk has consistently found that the accumulation of risk factors increases the likelihood of mental health problems, two different models of the relationship between cumulative risk and outcomes have been supported. In one such model, risk for psychiatric disorder increases dramatically after a certain threshold of risk factors has been reached (e.g., Rutter, 1979). In other words, a multiplicative rather than additive relationship among risk factors exists, with the presence of multiple concurrent stressors increasing risk for the occurrence of mental health problems beyond the summation of their separate effects (Rutter, 1979). Alternatively, a linear model in which changes in emotional/behavioral symptoms mirror increases in risk has been supported (e.g., Appleyard et al., 2005; Sameroff, et al., 1993). Identification of the model that best describes the relation between risk factors and mental health outcomes among maltreated youths placed in out-of-home care will shed additional light on whether there is a particular segment of this population (e.g., those who display a certain number of risk factors) that is at particularly high risk for poorer psychological adjustment (as in the threshold model), or whether risk for mental health problems increases in a relatively steady fashion commensurate with risk factor exposure.
Current Study
The overarching goal of the current study is to elucidate the relation between cumulative risk and mental health symptomatology within a sample of maltreated youths placed in out-of-home care. By virtue of their exposure to maltreatment that necessitated removal from their families of origin, all participants in this sample are at the high end of the risk continuum. This study will determine whether cumulative risk findings hold true with respect to this high risk sample. The current research will also examine whether a linear or threshold model better describes the relationship between cumulative risk and mental health outcomes.
Method
Participants
Recruitment
Each summer between 2002 and 2007, all 9–11 year olds from participating Denver metro area counties who were court-ordered into any type of out-of-home care due to substantiated maltreatment during the preceding 12 months, and who remained in out-of-home care at the time of the interview, were recruited for participation in a randomized controlled trial of the Fostering Healthy Futures preventive intervention (see Taussig, Culhane, & Hettleman, 2007 for a description of the intervention). The protocol used was approved by the Colorado Multiple Institutional Review Board. Ninety-three percent of children meeting eligibility requirements were recruited. The children provided their assent and informed consent was obtained from their legal guardians. The sample for this study includes 252 youths and caregivers (out of the 286 interviewed at baseline). Participants were excluded for the following reasons: 28 children were siblings of others included in the sample (when siblings were interviewed, one was chosen at random to be included in the current study's analyses); four children were excluded because they were not proficient enough in English to comprehend study questions; and two participants were excluded because either the child or the caregiver did not complete the interview. Youths and caregivers were interviewed at the child's out-of-home placement (e.g., foster care, kinship care, group home) with the stipulation that the child had been at the placement for at least three weeks.
Participant characteristics
The final sample of 252 youths (M age = 9.86; SD = .90) was 48% female. Youths were 48.0% Caucasian, 46.4% Hispanic, and 28.2% African American (non-exclusive categories). At the time of the interview, 47.6% were in foster care, 46.4% were in kinship care, and the remaining 5.6% resided in shelters, group homes, or residential treatment centers. The sample of caregivers was predominantly female (89%). The average length of time in out-of-home care at the time of the interview was 6.5 months (SD = 4.0). They had been at their current placement an average of 5.3 months (SD = 3.8).
Measures of Risk
Eighteen variables were proposed for inclusion in the cumulative risk index. These variables were chosen a priori based on evidence from previous studies suggesting that these factors are implicated in the development of mental health problems among children. Thirteen of the risk variables were dichotomously coded as “present” (1) or “absent” (2). Five of the risk variables were continuous and were dichotomized such that a score of “zero” indicated no or low risk and a score of “one” indicated the presence of risk. For four of these continuous variables, a score of 1 (high risk) was assigned if the participant had a score that was in the upper quartile of the distribution in this sample, consistent with previous research (e.g., Appleyard et al., 2005). The only exception to this method of dichotomization was the intellectual functioning variable, for which the conventional clinical criterion (IQ scores below 85) was used to differentiate between high versus low risk.
Maltreatment Experiences
Narrative descriptions of maltreatment allegations found in child welfare case records and Dependency and Neglect (D&N) legal petitions leading to the child's removal from the home were coded by trained research assistants in accordance with the Maltreatment Classification System (Barnett, Manly, & Cicchetti, 1993). All records were consensus coded by at least two trained staff, and discrepancies were resolved through consultation with one of the senior investigators. Manly and colleagues report an overall kappa of .60 for subtype coding and adequate estimates of interrater agreement (.67–1.0; Manly, et al., 1994). Each record was coded for the presence (1) or absence (0) of seven types of maltreatment: physical abuse, sexual abuse, failure to provide, educational neglect, lack of supervision, emotional abuse, and moral/legal abuse.
Other Characteristics of the Child's Family of Origin
Child welfare records were coded to ascertain the presence of a criminal history, alcohol abuse, and substance abuse on the part of the parent/caregiver from whom the child had been removed. Each of these 3 variables was dichotomous (present = 1, absent = 0). If the child had been removed from more than one caregiver (e.g., both biological parents, biological mother and step-father), the variable was coded as 1 if records indicated the presence of the risk factor for either or both caregivers. The child's exposure to domestic violence was also coded as present (1) or absent (0). Death in the family was coded as present if child welfare records indicated that the child's biological mother, biological father, or a sibling had died. Single parent household was coded as present if the child was removed from a single parent/caregiver with no domestic partner or spouse living in the home.
Finally, the number of previous Dependency and Neglect (D&N) Petitions (legal petitions filed on the family in order to remove children from their custody) was coded based on records. This continuous variable ranged from 0 to 10 (M = .49, SD = 1.02). To dichotomize this measure, participants scoring in the upper quartile of this sample (those participants with 1 or more previous D&N petitions) were assigned a score of 1, while all other participants were assigned a score of 0.
Intellectual Functioning
The Kaufman Brief Intelligence Test (KBIT; Kaufman & Kaufman, 1990) is a screening measure of intelligence that yields Verbal, Nonverbal, and Composite estimates of IQ. The KBIT was administered to all participants entering the study before 2007 (n = 187). A revision of the KBIT, the Kaufman Brief Intelligence Test-2 (KBIT-2; Kaufman & Kaufman, 2004), was administered to participants entering the study in 2007 (n = 65). Both versions were normed on nationally-representative samples. The two versions of the KBIT are highly correlated (rs = .80 to .86; Kaufman & Kaufman, 2004). The mean score for this sample was 94.65 (SD = 13.99). Children with a composite IQ score of 84 or below (one standard deviation or more below the published mean) were assigned a score of 1, while all other participants were assigned a score of 0. Due to concerns about the validity of the self-report data of children with IQs below 70, 6 children were not included in analyses using child self-report mental health data.
Exposure to Community Violence
An adapted, 8-item version of the youth-report Things I Have Seen and Heard scale (Richters & Martinez, 1993) was used as a measure of community violence exposure. Sample items include, “How many times have you heard guns being shot?” and, “How many times have you seen gangs in your neighborhood?” Responses were provided on a five-point scale (0 = never, to 4 = four or more times), with the overall score representing a mean of the eight items. The internal consistency for the items was acceptable (α = .77). Scores on this scale ranged from 0 to 3.75 (M = 1.11). The upper quartile of this sample (those with scores of 1.63 and higher) was assigned a score of 1, while all other participants were assigned a score of 0.
Number of Caregiver Transitions
Youths were asked to report on each caregiver with whom they had lived since birth. Interviewers asked children where they had lived at birth and then reconstructed caregiver history by asking children where and with whom they had lived next. Based on the information provided by children, the interviewer coded the total number of caregivers with whom each child had lived since birth (range = 2–12, M = 4.17, SD = 2.29). Participants in the upper quartile, or those who had experienced six or more caregiver transitions, were assigned a risk score of 1, while all other participants were assigned a score of 0.
Number of School Transitions
A similar interview procedure was utilized to assess the number of school transitions that the child had experienced (range = 1–23, M = 4.31, SD = 2.80). Participants in the upper quartile had experienced six or more school transitions and were assigned a score of 1 for this risk variable, while all other participants were assigned a score of 0.
Dependent Variables
Anxiety
Youths completed the Revised Children's Manifest Anxiety Scale (RCMAS; Reynolds & Richmond, 2000), a 37-item self-report measure of anxiety that yields a total anxiety score. In this sample of maltreated children, 11.5% of youths scored in the clinical range (T-score ≥ 65) with regard to anxiety symptoms. Approximately 7% of individuals in a representative sample would be expected to receive scores in this range.
Trauma Symptoms
Children completed the Trauma Symptom Checklist for Children (TSCC; Briere, 1996), a 54-item measure of posttraumatic stress and related symptomatology. It includes six clinical scales (Anxiety, Depression, Anger, Posttraumatic Stress, Dissociation, and Sexual Concerns). These six scales have demonstrated adequate reliability (α = .77 to .89). To avoid duplication with the RCMAS, the Anxiety scale of the TSCC was not used in the current study. On this measure, T-scores of 65 or higher on the Depression, Anger, Posttraumatic Stress, and Dissociation scales are considered to be clinically significant; a T-score of 70 or higher on the Sexual Concerns scale is considered clinically significant. Between 4.8% and 9.5% of children in this sample scored in the clinical range on each of the five subscales of the TSCC, while between 2% and 7% of individuals would be expected to receive scores within the clinical range based on the normal distribution.
Internalizing and Externalizing Problems
Caregivers completed the Child Behavior Checklist (CBCL; Achenbach & Rescorla, 2001), a widely-used measure of child emotional and behavior problems; reliability and validity are well established (Achenbach & Rescorla, 2001). Caregivers rated 113 items on a 3-point scale to yield data on Internalizing and Externalizing Problems. In this sample, 45.6% of youths scored in the clinical range on the Internalizing Problems subscale and 48.0% of youths scored in the clinical range on the Externalizing Problems subscale (T-scores ≥ 64), while only 8% of individuals in a representative sample would be expected to receive scores within the clinical range based on the normal curve.
Results
Prevalence of Risk Exposure
The prevalence of the dichotomous risk variables is displayed in Table 1. There was a high frequency of exposure to many of the variables coded for presence/absence. Specifically, 50% or more of the sample had experienced: emotional abuse, neglect in the form of lack of supervision and/or failure to provide, a single parent household, caregiver substance abuse and/or criminal involvement, and domestic violence exposure.
Table 1.
Prevalence of Dichotomous Risk Variables (N = 252)
| Risk Variables | Percent of Sample |
|---|---|
| Physical Abuse | 29.8 |
| Sexual Abuse | 11.5 |
| Failure to Provide | 50.8 |
| Lack of Supervision | 76.6 |
| Emotional Abuse | 65.9 |
| Moral/Legal Abuse | 32.5 |
| Educational Neglect | 29.8 |
| Death in the family | 8.3 |
| Single parent household | 62.3 |
| Exposure to domestic violence | 51.2 |
| Caregiver abuse of alcohol | 41.7 |
| Caregiver abuse of substances | 66.3 |
| Caregiver criminal history | 67.1 |
Correlations among Proposed Risk Factors
The correlations (Pearson's product moment or point-biserial) among the risk variables were examined to determine the degree to which risk factors co-occurred in this sample. Where possible, continuous variables were used to estimate correlations to maximize variability; estimating the correlations with dichotomized risk variables did not substantively change the results. With the exception of the seven categories of abuse and neglect, many of the risk factors proposed for inclusion in the cumulative risk variable were not significantly correlated with one another in this sample. On the whole, correlations that were significant among risk factors were in the low-to-moderate range (ranging from .13 to .33). Of note is that five risk variables (lack of supervision, emotional abuse, educational neglect, caregiver criminal history, and caregiver substance use) were associated with better cognitive functioning (rpb = .15). Two other unexpected correlations emerged, indicating that children with substance abusing caregivers were less likely to be physically and sexually abused (−.27 and −.19, respectively). On the other hand, parental substance use was associated with a higher likelihood that the child had been neglected in the form of lack of supervision or educational neglect or had experienced moral/legal abuse (.30 and .33, respectively).
Associations among Proposed Risk Factors and Child Mental Health
Table 2 displays the correlations between the risk variables and the mental health variables as well as the means and standard deviations of the outcome variables. As in the previous set of correlations, continuous variables were used where possible and using dichotomized risk variables did not substantively change the results. Of the 18 proposed risk factors, seven (physical abuse, sexual abuse, coming from a single parent household, number of caregiver transitions, number of school transitions, exposure to community violence, and intellectual functioning) were significantly correlated in the expected direction with at least one of the mental health variables. Correlations indicated that four variables (neglect in the form of lack of supervision, educational neglect, caregiver use of alcohol, and caregiver use of substances) were associated with fewer mental health symptoms in this sample.
Table 2.
Correlations between Risk Variables and Mental Health Variables
| Variables | RCMAS | TSCC DEP | TSCC ANG | TSCC PTS | TSCC DIS | TSCC SC | CBCL Int. | CBCL Ext. |
|---|---|---|---|---|---|---|---|---|
| 1. Physical abusea | .12 | .07 | .05 | .10 | .05 | .05 | .02 | .20* |
| 2. Sexual abusea | .00 | .11 | .01 | .09 | .13* | .32* | −.05 | .08 |
| 3. Failure to provideb | .06 | .03 | −.02 | −.11 | .01 | −.04 | .12 | .00 |
| 4. Lack of supervisionb | −.07 | −.03 | −.04 | −.04 | .00 | .00 | −.08 | −.13* |
| 5. Emotional abusea | −.01 | .00 | −.02 | .08 | .01 | .00 | −.08 | −.01 |
| 6. Moral/legal abusea | −.07 | −.04 | .00 | −.05 | −.03 | .07 | .05 | −.06 |
| 7. Educational Neglecta | −.04 | .01 | −.05 | −.11 | .00 | −.09 | −.01 | −.15* |
| 8. Number of previous D&Nsb | −.06 | .01 | .00 | −.06 | −.06 | −.07 | .12 | .10 |
| 9. Deaths in the familya | −.02 | −.05 | −.07 | −.03 | −.07 | −.01 | −.01 | −.03 |
| 10. Single parent householda | .13* | .01 | .02 | .08 | .03 | −.03 | .02 | −.01 |
| 11. Domestic violencea | −.10 | −.11 | −.07 | −.09 | −.05 | −.04 | .07 | .10 |
| 12. Caregiver alcohol abusea | −.03 | −.14* | −.09 | −.10 | −.09 | −.04 | −.01 | −.01 |
| 13. Caregiver substance abusea | −.15* | −.11 | −.06 | −.12 | −.09 | −.04 | −.10 | −.16* |
| 14. Caregiver criminal historya | −.11 | −.10 | −.06 | −.09 | −.01 | −.04 | .05 | −.01 |
| 15. Caregiver transitionsb | .09 | .17* | .16* | .13* | .10 | .06 | .07 | .14* |
| 16. School transitionsb | .04 | .09 | .09 | .12 | .13* | .06 | .08 | .07 |
| 17. Community violenceb | .24* | .33* | .32* | .29* | .31* | .16* | .05 | .14* |
| 18. Intellectual functioningb | −.25* | −.10 | −.05 | .02 | .03 | −.08 | −.01 | −.09 |
| M | 51.79 | 46.43 | 46.02 | 48.98 | 49.07 | 51.52 | 61.04 | 62.49 |
| SD | 10.49 | 10.07 | 9.75 | 9.88 | 10.17 | 12.22 | 10.80 | 12.02 |
Note.
Dichotomous risk variable.
Continuous risk variable. For dichotomous variables, (1 = presence; 0 = absence), we computed the point-biserial coefficient. RCMAS: Revised Children's Manifest Anxiety Scale. TSCC: Trauma Symptom Checklist for Children. DEP: Depression. ANG: Anger. PTS: Post Traumatic Stress. DIS: Dissociation. SC: Sexual Concerns. CBCL: Child Behavior Checklist. Int.: Internalizing. Ext.: Externalizing. Correlations and means and standard deviations were computed using T-scores.
p < .05.
Constructing the Cumulative Risk Variable
Given the results outlined above, two separate cumulative risk variables were constructed. The first was theoretical, including all 18 a priori hypothesized risk variables. The second was empirical, including only the seven variables that were significantly associated in bivariate analyses with mental health symptoms in the expected direction (i.e., conferring greater risk). For both variables, scores on the dichotomized risk variables were summed to create the cumulative risk index. Scores on the theoretical cumulative risk variable ranged from 2 to 13 out of the possible 18, with a mean of 7.13 (SD = 2.07). Scores on the empirical cumulative risk variable ranged from 0 to 5 out of the possible 7, with a mean of 1.92 (SD = 1.21). Youth who received scores of four or five on the empirical cumulative risk variable were combined into a single group for analyses due to small sample sizes in these categories (n = 15 and n = 10, respectively). The empirical cumulative risk variable was significantly correlated with all mental health variables with the exception of CBCL Internalizing. Significant correlations ranged from r = .17 to r = .25. The theoretical cumulative risk variable did not demonstrate significant correlations with any of the mental health outcomes.
Identifying the Nature of the Relation between Cumulative Risk and Mental Health
Analyses exploring whether a threshold (quadratic) or linear model best fit the data were conducted using the empirical cumulative risk variable. One-way analyses of variance compared five groups that represented cumulative risk scores of 0, 1, 2, 3, and 4/5. Tests of the linear trend indicated that the empirical cumulative risk score predicted all mental health variables with the exception of caregiver-reported internalizing symptoms (see Table 3). These results indicated that children with more risk factors were more likely to experience self-reported symptoms of anxiety, depression, post-traumatic stress, dissociation, and sexual concerns as well as externalizing behaviors, with symptom levels increasing on average with increases in the number of risk factors. Post hoc tests revealed patterns of significant differences primarily between 0 risks as compared to 4 or 5 risks for most outcomes (effect sizes ranged from .59 to 1.04). On TSCC Anger and TSCC Sexual Concerns, post hoc comparisons revealed significant differences primarily between 1 risk as compared to 4 or 5 risks (effect sizes = .67 and .52, respectively). None of the post hoc comparisons were significant for CBCL Internalizing symptoms. One-way analyses of variance including a quadratic term were utilized to investigate whether a threshold effect was supported by the data. A statistically significant quadratic effect did not exist for the relation between cumulative risk and any of the mental health variables, with the exception of sexual concerns, indicating that a threshold effect was only supported for this single outcome. Examination of the shape of the significant quadratic effect for TSCC sexual concerns indicated that it was a U-shaped curve (see Table 3), rather than the shape that would be expected by a threshold model in which risk for mental health problems increases dramatically after a certain threshold of risk factors has been reached (e.g., Rutter, 1979).
Table 3.
Means, Standard Deviations, and One-way Analyses of Variance for Effects of the Cumulative Risk Factor on Mental Health Functioning
| Empirical Cumulative Risk Score | |||||||
|---|---|---|---|---|---|---|---|
| Measure | 0 (n = 26) | 1 (n = 70) | 2 (n = 87) | 3 (n = 43) | 4/5 (n = 25) | Linear Term | Quadratic Term |
| RCMAS Total | 47.15 (10.07) | 49.83 (9.93) | 52.48 (10.25) | 53.16 (10.64) | 57.79 (10.32) | F(4, 237) 16.08** | F(4, 237) .09 |
| TSCC Depression | 44.00 (9.73) | 44.49 (8.51) | 45.94 (8.89) | 49.95 (12.06) | 50.75 (12.79) | F(4, 237) 10.21** | F(4, 237) .25 |
| TSCC Anger | 44.81 (9.89) | 44.81 (9.73) | 45.27 (8.92) | 47.63 (11.39) | 50.96 (8.48) | F(4, 237) 6.84* | F(4, 237) 1.94 |
| TSCC Post-traumatic Stress | 45.65 (7.80) | 47.04 (9.80) | 49.58 (9.66) | 49.74 (10.16) | 54.83 (10.24) | F(4, 237) 13.15** | F(4, 237) .67 |
| TSCC Sexual Concerns | 53.19 (14.79) | 48.64 (8.18) | 49.77 (10.32) | 53.67 (14.50) | 61.26 (16.39) | F(4, 233) 8.78** | F(4, 233) 12.71** |
| TSCC Dissociation | 46.00 (8.41) | 48.07 (10.00) | 49.19 (9.77) | 48.89 (9.87) | 55.08 (12.43) | F(4, 237) 9.96** | F(4, 237) 1.14 |
| CBCL Internalizing | 59.15 (13.05) | 62.59 (10.06) | 58.80 (10.25) | 62.40 (11.33) | 64.28 (10.09) | F(4, 246) 2.52 | F(4, 246) .41 |
| CBCL Externalizing | 57.12 (10.46) | 63.42 (11.76) | 59.94 (12.03) | 65.95 (11.68) | 68.48 (10.88) | F(4, 246) 13.41** | F(4, 246) .07 |
Note. RCMAS: Revised Children's Manifest Anxiety Scale. TSCC: Trauma Symptom Checklist for Children. CBCL: Child Behavior Checklist. All reported means are T-scores.
p < .05.
p < .01.
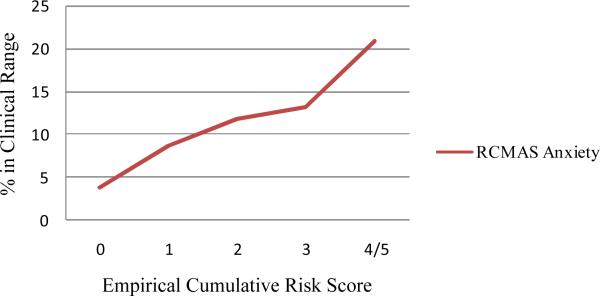
To further examine the clinical utility of the cumulative risk variable, logistic regressions were conducted to determine whether the cumulative risk variable differentiated between those who scored within the clinical range with regard to mental health symptomatology versus those who did not. Results indicated that the empirical cumulative risk variable was associated with scoring in the clinical range on RCMAS Anxiety (b = .36, χ2 (1, N = 242) = 3.92, p = .05). The odds ratio (OR) was 1.43 (95% CI 1.00 to 2.05), indicating that a one unit increase in the cumulative risk variable (e.g., moving from having no risks to having one risk variable) was associated with a 57% increase in the odds of scoring in the clinical range on the RCMAS. Figure 1 displays the percentage of participants scoring in the clinical range on RCMAS Anxiety based on the cumulative risk score. The empirical cumulative risk variable was also significantly associated with scoring in the clinical range on the TSCC Depression (b = .51, OR = 1.67 (95% CI 1.10 to 2.53), χ2 (1, N = 242) = 6.08, p = .01), CBCL Internalizing (b = .22, OR = 1.25 (95% CI 1.00 to 1.56), χ2 (1, N = 251) = 4.11, p = .04), and CBCL Externalizing (b = .28, OR = 1.29 (95% CI 1.03 to 1.62), χ2 (1, N = 251) = 6.77, p = .01).
Figure 1.
Rates (%) of Participants Scoring in the Clinical Range on RCMAS Anxiety by Cumulative Risk Score
Discussion
This study contributes to our knowledge about patterns of risk among maltreated youths placed in out-of-home care. Findings demonstrate that although all children placed in out-of-home care have experienced serious life adversities, they are not identical with regard to their exposure to risk factors—nor are they homogeneous with regard to their likelihood of experiencing mental health symptoms. Results also replicate previous research and support the cumulative risk hypothesis. Even in this high-risk sample (in which 48% of children in the overall sample were in the clinical range with regard to externalizing behaviors according to caregiver report), the empirically-derived cumulative risk index significantly predicts mental health symptoms. Furthermore, the cumulative risk index differentiates between children who score in the clinical range with regard to mental health symptoms versus those who do not. The data support a linear model in which each incremental increase in cumulative risk is accompanied by a similar increase in mental health problems.
Although not surprising, one of the most striking findings of this study is the catastrophic accumulation of risks faced by maltreated children placed in out-of-home care. In addition to exposure to various types of maltreatment, over half the sample came from a single parent household, had been removed from caregivers with a history of substance abuse and/or criminal involvement, and had been exposed to domestic violence. As compared to other studies, these rates are quite high. For example, Fergusson & Horwood (2003) report that approximately 33% of their urban community sample was born into a single-parent family, approximately 20% had experienced inter-parental violence, 12.1% of parents had a history of alcohol problems, 13.3% had a history of criminal involvement, and 24.8% had a history of substance abuse. Furthermore, the cutpoints for assignment to a high-risk group within the context of our sample of children are also considerably higher than those found in studies of cumulative risk conducted with community samples. Given the prevalence of risk exposure and elevated thresholds for being considered high risk within this sample, any cumulative risk index constructed for this population by definition differs substantially from cumulative risk indices used with more heterogeneous samples. Nevertheless, the empirical risk index created for the present study was useful in predicting participants' mental health functioning.
Although the empirical risk index operated in ways consistent with the cumulative risk literature, the theoretical risk index did not appear to capture the co-occurring factors that place maltreated youths at risk. As we examined the eighteen hypothesized risk factors, two surprising findings emerged. First, many of the risk factors we proposed did not correlate in expected ways with one another; and second, the risk factors did not correlate in expected ways with the mental health outcome variables, illustrating the importance of considering the characteristics of the sample at hand, rather than generalizing from research conducted with less risky samples.
While a large body of literature has demonstrated that risk factors tend to cluster within individuals (e.g., Masten & Wright, 1998), many of the correlations among the eighteen hypothesized risk factors were low or non-significant. In addition, some counter-intuitive correlations between risk factors emerged. Specifically, although research has documented that the prevalence of physical and sexual abuse is higher in families in which a parent is abusing substances (Walsh, MacMillan, & Jamieson, 2003), in our sample, parental substance use was associated with a lower likelihood that the child had been physically and sexually abused. On the other hand, parental substance use was associated with a higher likelihood that the child had been neglected in the form of lack of supervision or educational neglect or had experienced moral/legal abuse. This suggests that although parental substance use may elevate risk for maltreatment in general within community populations, perhaps patterns of differing etiologies for different types of abuse emerge when examining the population of children removed from their homes due to substantiated abuse or neglect, with substance abusing parents being more likely to neglect children than to physically or sexually abuse them.
Although few people would argue that exposure to adverse life experiences such as neglect in the form of failing to provide or witnessing domestic violence do not pose a risk to children's mental health, many of the proposed risk variables did not demonstrate significant correlations with mental health symptomatology. There are at least two potential explanations for the lack of significant correlations between some well-established risk factors and mental health functioning in this sample. The first possibility is that the high percentage of children in this sample with exposure to certain risk factors limits the predictive value of these variables for this sample and attenuates these correlations. Second, since all participants in this sample are already at high risk for mental health problems, it logically follows that few risk factors would be salient enough to differentiate between participants' levels of risk.
Another reason that context is important to consider in the interpretation of the findings reported herein is that children exposed to some of the proposed risk factors (such as neglect in the form of lack of supervision, educational neglect, and parental alcohol and substance use) do not seem to fare as poorly as maltreated children who were not exposed to these risk factors. Clearly, neglect and parental substance use are not factors that promote positive functioning (e.g., Gilbert, Widom, Browne, Fergusson, Webb, & Janson, 2009). However, there is some evidence that certain profiles of maltreatment (i.e., those that include physical or sexual abuse with or without exposure to additional types of maltreatment) are more highly associated with internalizing and externalizing symptoms than are other profiles (Pears, Kim, & Fisher, 2008). Pears, Kim, and Fisher (2008) found that children who had experienced neglect in the form of lack of supervision had more positive scores on measures of adjustment within their maltreated sample of preschoolers. The authors were careful to note that neglect has serious negative consequences and that their results “…simply suggest that children in this group may not fare as poorly as children who have experienced physical or sexual abuse (or both) in addition to neglect.” (p. 969).
Although 11 of the hypothesized risk factors did not emerge as salient predictors of mental health functioning in this sample, seven risk variables demonstrated significant relations with mental health symptoms: physical abuse, sexual abuse, coming from a single parent household, number of caregiver transitions, number of school transitions, exposure to community violence, and low intellectual functioning. Of these variables, the latter four represent characteristics of the child or of the child's experience that are external to his or her immediate family. This finding is intriguing. Since all children in this sample come from families that are risky by definition, perhaps what differentiates those individuals that are at higher risk is exposure to risk in domains outside of their immediate family. One factor that may link family-related risk factors, such as single parenthood, and sociocultural risk factors, such as exposure to community violence, is poverty. Although we were not able to measure socioeconomic status in the current study, this may be an important intervening variable to consider in future research.
Of the maltreatment variables, physical and sexual abuse emerged as important risk variables, while other maltreatment types did not. One study that classified maltreatment cases according to the predominant type of maltreatment utilized a hierarchy in which “active” forms of abuse (e.g., physical and sexual abuse) were prioritized over “passive” forms of abuse (e.g., neglect). This classification system predicted more mental health symptoms, even after accounting for the co-occurrence of multiple maltreatment subtypes (Lau et al., 2005). This finding lends some support to the notion that, even among maltreated youths who have likely experienced multiple types of maltreatment, maltreatment of commission may have more serious emotional and behavioral consequences than maltreatment by omission. However, this finding requires replication prior to drawing definitive conclusions.
Although some other studies have found certain levels of risk at which the likelihood of adverse outcomes increases dramatically, such a threshold effect is not supported for this sample. The only outcome to demonstrate a significant quadratic relationship to the cumulative risk index was the sexual concerns subscale of the TSCC. However, examination of the shape of this effect indicated that it was U-shaped, and was not consistent with the shape of the relationships posited by a threshold model. The reasons for the existence of a U-shaped curve (and the decrease in scores from a cumulative risk score of 0 to a cumulative risk score of 1) are not clear, and require further investigation and replication prior to drawing conclusions. However, the linear relationship that was supported for all outcomes with the exception of CBCL internalizing symptoms indicates that the effect of risk factors is additive. It is possible that all participants within this high risk sample were above the “threshold” at which risk would increase in a dramatic fashion. Future studies could attempt to determine whether threshold effects are more likely to occur within more heterogeneous or low risk samples.
The empirical cumulative risk index predicted both children's and caregiver's reports of mental health outcomes. Furthermore, different levels of cumulative risk were related to striking differences in the percentage of children scoring in the clinical range with regard to emotional or behavioral problems, indicating that this index has clinical utility. However, several limitations of this study must be noted. First, although the method used for the calculation of cumulative risk replicated that used in multiple previous studies, a potential downside to this procedure is that the cutoffs used to dichotomize continuous risk variables are sample-specific, limiting the generalizability of these findings to other samples. The empirical derivation of the cumulative risk index may also render findings more sample-specific; thus, replication of the results of this study is important. Second, because we coded maltreatment variables and characteristics of the child's family of origin based on child welfare records that were relevant to the current filing, we have little information about the chronicity or timing of exposure to these risk factors. Furthermore, although the Maltreatment Classification System is the gold-standard in the field, all coding techniques are by definition limited by the information that is reported in the child's case files. Third, multiple analyses were conducted with these data, thus inflating the chance of Type I errors. Finally, there are other potentially important risk variables that we were unable to examine due to their unavailability in the current dataset. Most notably, we did not have measures of socioeconomic status/poverty or parental psychopathology.
Despite these limitations, to our knowledge, the present study is the first to examine the relation between cumulative risk among maltreated children in out-of-home care and their mental health functioning and suggests several directions for future research as well as implications for intervention. The cumulative risk index was developed within the context of a prevention program. We intend to use this index in future studies to investigate whether initial levels of cumulative risk may moderate the effects of the prevention program. Although all maltreated children who have been removed from their homes require some type of intervention to optimize their outcomes, the results of moderational analyses could help allocate resources more effectively, by shedding light on the effectiveness of interventions for maltreated children who are at relatively lower versus higher risk. Specifically, in the current study, nearly three-quarters of individuals with high cumulative risk scores exhibited clinical levels of externalizing behaviors. In addition, these children were likely to be exposed to risk factors in multiple domains. Thus, children with high cumulative risk scores may require immediate stabilization of problem behaviors combined with multi-systemic interventions. On the other hand, those children with lower cumulative risk scores may be more likely to reap benefits from more traditional types of interventions, including individual or group programs. It is our hope this research will help inform prevention and intervention efforts that will mitigate some of the destructive effects of child maltreatment.
Acknowledgments
This study was supported by grants from The Children's Hospital of Denver's Research Institute, the Pioneer Fund, the Daniels Fund and the Kempe Foundation for the Prevention and Treatment of Child Abuse and Neglect. This work was also supported by the Berger Fellowship through the Kempe Foundation awarded to the first author. Federal funding for the study was provided through award numbers 1R21MH067618 and 5R01MH076919 (H. Taussig, PI). The content is solely the responsibility of the authors and does not represent the official views of the National Institute of Mental Health or the National Institutes of Health.
References
- Achenbach TM, Rescorla LA. Manual for the ASEBA School-Age Forms and Profiles. University of Vermont, Research Center for Children, Youth, & Families; Burlington, VT: 2001. [Google Scholar]
- Appleyard K, Egeland B, van Dulmen MHM, Sroufe LA. When more is not better: The role of cumulative risk in child behavior outcomes. Journal of Child Psychology and Psychiatry. 2005;46:235–245. doi: 10.1111/j.1469-7610.2004.00351.x. [DOI] [PubMed] [Google Scholar]
- Barnett D, Manly JT, Cicchetti D. Defining child maltreatment: The interface between policy and research. In: Cicchetti D, Toth SL, editors. Child abuse, child development, and social policy. Ablex; Norwood, MY: 1993. pp. 7–74. [Google Scholar]
- Briere J. Trauma Symptom Checklist for Children – Professional manual. Psychological Assessment Resources, Inc.; Odessa, FL: 1996. [Google Scholar]
- Bronfenbrenner U. Ecology of the family as a context for human development: Research perspectives. Developmental Psychology. 1986;22:723–742. [Google Scholar]
- Burns BJ, Phillips SD, Wagner HR, Barth RP, Kolko DJ, Campbell Y, Landsverk J. Mental health need and access to mental health services by youths involved with child welfare: A national survey. Journal of the American Academy of Child and Adolescent Psychiatry. 2004;43:960–970. doi: 10.1097/01.chi.0000127590.95585.65. [DOI] [PubMed] [Google Scholar]
- Chandy JM, Blum RW, Resnick MD. Female adolescents with a history of sexual abuse. Journal of Interpersonal Violence. 1996;11:503–518. [Google Scholar]
- Cicchetti D, Lynch M. An ecological-transactional analysis of children and contexts: The longitudinal interplay among child maltreatment, community violence, & children's symptomatology. Development and Psychopathology. 1998;13:677–693. doi: 10.1017/s095457949800159x. [DOI] [PubMed] [Google Scholar]
- Coie JD, Watt NF, West SG, Hawkins JD, Asarnow JR, Markman HM, Ramey SL, Shure MB, Long B. The science of prevention: A conceptual framework and some directions for a national research program. American Psychologist. 1993;48:1013–1022. doi: 10.1037//0003-066x.48.10.1013. [DOI] [PubMed] [Google Scholar]
- Courtney ME, Dworsky A, Ruth G, Keller T, Havlicek J, Bost N. Midwest evaluation of the adult functioning of former foster youth: Outcomes at age 19. Chapin Hall Center for Children at the University of Chicago; Chicago: 2005. [Google Scholar]
- Davis CH, MacKinnon DP, Schultz A, Sandler I. Cumulative risk and population attributable fraction in prevention. Journal of Clinical Child and Adolescent Psychology. 2003;32:228–235. doi: 10.1207/S15374424JCCP3202_7. [DOI] [PubMed] [Google Scholar]
- Deater-Deckard K, Dodge KA, Bates JE, Pettit GS. Multiple risk factors in the development of externalizing behavior problems: Group and individual differences. Development and Psychopathology. 1998;10:469–493. doi: 10.1017/s0954579498001709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dodge KA, Pettit GS, Bates JE. Mechanisms in the cycle of violence. Science. 1990;250:1678–1683. doi: 10.1126/science.2270481. [DOI] [PubMed] [Google Scholar]
- Eckenrode J, Rowe E, Laird M, Brathwaite J. Mobility as a mediator of the effects of child maltreatment on academic performance. Child Development. 1995;66:1130–1142. [PubMed] [Google Scholar]
- Fergusson DM, Horwood LJ. Resilience to childhood adversity: Results of a 21-year study. In: Luthar SS, editor. Resilience and vulnerability: Adaptation in the context of childhood adversities. Cambridge; New York: 2003. pp. 130–155. [Google Scholar]
- Garland AF, Hough RL, McCabe KM, Yeh M, Wood PA, Aarons GA. Prevalence of psychiatric disorders in youths across five sectors of care. Journal of the American Academy of Child and Adolescent Psychiatry. 2001;40:409–418. doi: 10.1097/00004583-200104000-00009. [DOI] [PubMed] [Google Scholar]
- Gilbert R, Widom CS, Browne K, Fergusson D, Webb E, Janson S. Child maltreatment I: Burden and consequences of child maltreatment in high-income countries. The Lancet. 2009;373(9657):68–81. doi: 10.1016/S0140-6736(08)61706-7. [DOI] [PubMed] [Google Scholar]
- Gutman LM, Sameroff AJ, Cole R. Academic growth curve trajectories from 1st grade to 12th grade: Effects of multiple social risk factors and preschool child factors. Developmental Psychology. 2003;39:777–790. doi: 10.1037/0012-1649.39.4.777. [DOI] [PubMed] [Google Scholar]
- Harman JS, Childs GE, Kelleher KJ. Mental health care utilization and expenditures by children in foster care. Archives of Pediatric and Adolescent Medicine. 2000;154:1114–1117. doi: 10.1001/archpedi.154.11.1114. [DOI] [PubMed] [Google Scholar]
- Herrenkohl EC, Herrenkohl RC, Egolf BP. The psychosocial consequences of living environment instability on maltreated children. American Journal of Orthopsychiatry. 2003;73:367–380. doi: 10.1037/0002-9432.73.4.367. [DOI] [PubMed] [Google Scholar]
- Kaufman AS, Kaufman NL. Kaufman Brief Intelligence Test Manual. American Guidance Service; Circle Pines, MN: 1990. [Google Scholar]
- Kaufman AS, Kaufman NL. Kaufman Brief Intelligence Test Second Edition Manual. AGS Publishing; Circle Pines, MN: 2004. [Google Scholar]
- Kurtz PD, Guadin JM, Howing PT, Wodarski JS. The consequences of physical abuse and neglect on the school age child: Mediating factors. Children and Youth Services Review. 1993;15:85–104. [Google Scholar]
- Lau AS, Leeb RT, English D, Graham JC, Briggs EC, Brody KE, Marshall JM. What's in a name? A comparison of methods for classifying predominant type of maltreatment. Child Abuse & Neglect. 2005;29:533–551. doi: 10.1016/j.chiabu.2003.05.005. [DOI] [PubMed] [Google Scholar]
- Litrownik AJ, Lau A, English DJ, Briggs E, Newton RR, Romney S, Dubowitz H. Measuring the severity of child maltreatment. Child Abuse & Neglect. 2005;29:553–573. doi: 10.1016/j.chiabu.2003.08.010. [DOI] [PubMed] [Google Scholar]
- Luthar SS. Vulnerability and resilience: A study of high-risk adolescents. Child Development. 1991;62:600–616. doi: 10.1111/j.1467-8624.1991.tb01555.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luthar SS. Resilience in development: A synthesis of research across five decades. In: Cicchetti D, Cohen DJ, editors. Developmental psychopathology: Risk, disorder, and adaptation. 2nd edition Volume 3. Wiley; New York: 2006. pp. 739–795. [Google Scholar]
- Lynch M, Cicchetti D. An ecological-transactional analysis of children and contexts: The longitudinal interplay among child maltreatment, community violence, and children's symptomatology. Development and Psychopathology. 1998;10:235–257. doi: 10.1017/s095457949800159x. [DOI] [PubMed] [Google Scholar]
- Manly JT, Cicchetti D, Barnett D. The impact of subtype, frequency, chronicity, and severity of child maltreatment on social competence and behavior problems. Development and Psychopathology. 1994;6:121–143. [Google Scholar]
- Masten AS, Wright MO. Cumulative risk and protection models of child maltreatment. In: Rossman BBR, Rosenberg MS, editors. Multiple victimization of children: Conceptual, developmental, research and treatment issues. Haworth Press; NY: 1998. pp. 7–30. [Google Scholar]
- Pears KC, Kim HK, Fisher PA. Psychosocial and cognitive functioning of children with specific profiles of maltreatment. Child Abuse & Neglect. 2008;32:958–971. doi: 10.1016/j.chiabu.2007.12.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reynolds CR, Richmond OB. Revised Children's Manifest Anxiety Scale (RCMAS) Manual. Western Psychological Services; Los Angeles, CA: 2000. [Google Scholar]
- Richters JE, Martinez PE. Violent communities, family choices, and children's chances: An algorithm for changing the odds. Development and Psychopathology. 1993;5:609–627. [Google Scholar]
- Rutter M. Protective factors in children's responses to stress and disadvantage. In: Kent MW, Rolf JE, editors. Primary prevention of psychopathology, Vol. 3: Social competence in children. University of New England Press; Hanover, NH: 1979. pp. 49–74. [Google Scholar]
- Sameroff AJ, Seifer R, Baldwin A, Baldwin C. Stability of intelligence from preschool to adolescence: The influence of social and family risk factors. Child Development. 1993;64:80–97. doi: 10.1111/j.1467-8624.1993.tb02896.x. [DOI] [PubMed] [Google Scholar]
- Taussig HN. Doctoral Dissertation, San Diego State University/University of California. Joint Doctoral Program in Clinical Psychology; San Diego: 1998. Risk behaviors in maltreated adolescents. [Google Scholar]
- Taussig HN, Culhane SE, Hettleman D. Fostering Healthy Futures: An innovative preventive intervention for preadolescent youth in out-of-home care. Child Welfare. 2007;86:113–131. [PMC free article] [PubMed] [Google Scholar]
- US Department of Health and Human Services, Administration on Children, Youth, and Families The AFCARS report. 2008 Retrieved February 20, 2009, from http://www.acf.hhs.gov/programs/cb/stats_research/afcars/tar/report14.htm.
- Vinnerljung B, Hjern A, Lindblad F. Suicide attempts and severe psychiatric morbidity among former child welfare clients—a national cohort study. Journal of Child Psychiatry and Psychology. 2006;47:723–733. doi: 10.1111/j.1469-7610.2005.01530.x. [DOI] [PubMed] [Google Scholar]
- Walsh C, MacMillan HL, Jamieson E. The relationship between parental substance abuse and child maltreatment: Findings from the Ontario Health Supplement. Child Abuse & Neglect. 2003;27:1409–1425. doi: 10.1016/j.chiabu.2003.07.002. [DOI] [PubMed] [Google Scholar]
- Zielinsky DS, Bradshaw CP. Ecological influences on the sequelae of child maltreatment: A review of the literature. Child Maltreatment. 2006;11:49–62. doi: 10.1177/1077559505283591. [DOI] [PubMed] [Google Scholar]