Abstract
The extent to which light-intensity physical activity contributes to health in older adults is not well known. The authors examined associations between physical activity across the intensity spectrum (sedentary to vigorous) and health and well-being variables in older adults. Two 7-day assessments of accelerometry from 2005 to 2007 were collected 6 months apart in the observational Senior Neighborhood Quality of Life Study of adults aged >65 years in Baltimore, Maryland, and Seattle, Washington. Self-reported health and psychosocial variables (e.g., lower-extremity function, body weight, rated stress) were also collected. Physical activity based on existing accelerometer thresholds for moderate/vigorous, high-light, low-light, and sedentary categories were examined as correlates of physical health and psychosocial well-being in mixed-effects regression models. Participants (N = 862) were 75.4 (standard deviation, 6.8) years of age, 56% female, 71% white, and 58% overweight/obese. After adjustment for study covariates and time spent in moderate/vigorous physical activity and sedentary behavior, low-light and high-light physical activity were positively related to physical health (all P < 0.0001) and well-being (all P < 0.001). Additionally, replacing 30 minutes/day of sedentary time with equal amounts of low-light or high-light physical activity was associated with better physical health (all P < 0.0001). Objectively measured light-intensity physical activity is associated with physical health and well-being variables in older adults.
Keywords: aged, epidemiologic measurements, motor activity, quality of life, sedentary lifestyle
Considerable evidence exists suggesting the beneficial effects of moderate/vigorous physical activity (MVPA) and the independent negative effects of sedentary behavior on health outcomes (1–3). The extent to which “light”-intensity activities (i.e., >1 and <3 metabolic equivalent task hours, such as easy walking) may contribute to health is less well known. Light-intensity activities are particularly important for older adults because they tend to spend a greater portion of their day performing light-intensity activities than any other age group (4), report easy walking (<3 miles per hour (1 mile = 1.61 km)) as their most common mode of physical activity (5), and often find it difficult to initiate or maintain MVPA (6). Lighter intensity activities could be recommended to older adults if replacing sedentary time with light-intensity activity confers health benefits.
Older adults often find light-intensity activity difficult to recall (7) and tend to misreport time spent in such activities when compared with objective measures such as motion sensors, indirect calorimetry, and doubly labeled water (8, 9). Objective measures of light physical activity are therefore needed to examine the impact of such activities on health and well-being. Indeed, only a few accelerometry validation studies have been conducted in samples of older adults (10, 11), with results generally suggesting that “meaningful” activity (adequate to confer health benefits) among older adults may fall below the commonly used Freedson threshold (12). Thus, intensity thresholds validated in general adult populations may be overly high for older adults and may not fully capture important physical activity–health associations falling below this threshold. The purpose of this study was to describe time spent in light-intensity physical activity, obtain 6-month reliability estimates for accelerometry metrics of activity time by intensity, and explore whether light-intensity activity was associated with self-rated health variables after accounting for moderate-intensity activity and sedentary time in a large sample of community-dwelling older adults.
MATERIALS AND METHODS
Study design and procedure
The Senior Neighborhood Quality of Life Study was an observational study of ambulatory adults 66 years of age or older in 2 major US metropolitan regions (Seattle/King County, Washington, and Baltimore, Maryland). The primary aim of the study was to examine multiple health outcomes among residents living in neighborhoods differing in geographic information system–derived “walkability” characteristics and household income. Study methods have been described elsewhere (13). The study was approved by appropriate institutional review boards.
After providing informed consent, participants were mailed an accelerometer and survey packet. They were instructed to wear the accelerometer for 7 consecutive days, complete the survey after wearing the accelerometer, and mail the accelerometer and survey packet back to research staff. Six months later, the accelerometer and a second survey were mailed to participants with similar instructions. Participants were recruited and enrolled year-round from 2005 through 2007. This 2-phase data collection strategy reduced participant burden, provided two 7-day periods of objective physical activity assessment, and controlled for seasonality effects. Upon completion of each assessment, participants were given US $25.
Participants
A commercial marketing firm provided contact information for all households in the designated 2000 US Census block groups comprising the neighborhoods of interest. Invitation letters were mailed to 3,911 randomly selected households, followed by recruitment telephone calls. Eligibility criteria were being aged 66 years or older, able to walk ≥10 feet (1 foot = 30.5 cm) alone (with or without assistive devices), and able to complete written surveys and informed consent in English. A total of 975 (25%) individuals were identified as eligible and willing to participate. Complete and valid accelerometry and survey data were collected for 88% (n = 862) and 78% (n = 765) of enrolled participants for the first and second assessments, respectively.
Measures
Covariates.
Individual-level covariates included age, gender, race, educational status, marital status, senior housing status, and current smoking status. Because the study sampling strategy was based on neighborhood-level income (using 2000 US Census median annual household income data) and a validated geographic information system–based walkability index (14), these factors also were included as covariates. Neighborhood (i.e., block group) was included as a clustering variable to account for potential lack of independence among neighbors regarding physical activity and health status.
Physical activity.
All participants wore an Actigraph accelerometer (model 7164 or 71256; Actigraph, LLC, Fort Walton Beach, Florida). The Actigraph was chosen because it has been used previously in large epidemiologic studies (15, 16) and extensive validation data are available in laboratory (10, 12) and field (10, 11, 17) settings. Participants were instructed to a) secure the unit over the right hip on a provided elasticized belt, b) wear the device while they were awake, and c) take off the unit for swimming or bathing. Data were collected in 1-minute epochs.
Data compliance and cleaning procedures were consistent with those from other published studies (15, 16). Data were visually screened to identify malfunctioning accelerometer units (e.g., sequences of maximum recordable value or repeated nonzeros). For compliance, a valid hour was defined as <30 consecutive “zero”-intensity counts and a valid day contained ≥10 valid hours/day. Participants were asked to rewear the accelerometer if an assessment contained either <5 valid days or <66 valid hours across 7 days or if the accelerometer had malfunctioned during data collection. Data were cleaned and scored using MeterPlus version 4.0 software from Santech, Inc. (www.meterplussoftware.com). Some individuals wore the accelerometer for >7 days; these data were retained if determined to be valid based on compliance criteria. All statistical models were adjusted for differences in accelerometer wear time.
Time spent in physical activity by intensity level was based on application of existing count-based intensity thresholds. The thresholds chosen for MVPA (≥1,952 counts/minute) and sedentary behavior (<100 counts/minute) have been used extensively in calibration studies (12, 17, 18), large epidemiologic studies (2, 3, 15, 16, 19), and intervention trials (20–23). The remaining activity fell within the “light” range of activity intensity (100–1,951 counts/minute). Given the wide range of activities in this category (e.g., standing, engaging in household activities, walking at <4.0 km/hour), it is possible that time spent in the upper, versus lower, end of the light-intensity category may have a differential effect on health. Therefore, the Copeland threshold (10) was used to distinguish “high-light” physical activity (HLPA; 1,041–1,951 counts/minute) from “low-light” physical activity (LLPA; 100–1,040 counts/minute). The Copeland threshold was chosen pragmatically given that it roughly divides the light range of activity equally. Copeland et al. have suggested that this threshold represents the lower bound of moderate-intensity physical activity in older populations, while others (24) have found the Freedson threshold adequate across a wide age range, including older adults. Because the Copeland threshold has been evaluated specifically in older populations, it was chosen for further evaluation in the current investigation.
Health variables.
Details regarding self-reported health outcomes assessed are displayed in Table 1. Health indicators were assessed on either the first or second survey. Body mass index and lower-extremity function were reported on both surveys.
Table 1.
Details and Validity Information for Health Indicators Assessed in the Senior Neighborhood Quality of Life Study, United States, 2005–2007
| Health Indicator | Detail | Author(s) (Reference No.) | Selected Validity Evidence (Reference No.) |
| No. of medications | “How many medications do you currently take regularly,” on a scale of 0–6, none to ≥5. | ||
| No. of chronic medical conditions | Number of medical conditions was chosen from a list of chronic conditions including rheumatoid arthritis, osteoarthritis, lupus, Parkinson's disease or other neurologic disorder, high blood pressure, diabetes, heart attack (or heart condition or angina), or cancer. Adapted from the Alameda County Study. | Roberts et al. (39) | Depression (39); medication use (40) |
| No. of falls in the past year | “Have you fallen in the past 12 months (includes falling on the ground or some other level, such as a chair),” on a scale of 0–1, no to yes. | Gibson et al. (41) | Medication use (42); depression (43); grip strength (44) |
| Confusion | “In the past year, about how often did you get confused?” on a scale of 0–4, never to frequently. | Lee (45) | Functional decline (45); mortality (45) |
| Feeling depressed/blue | “During the past year, have you had 2 consecutive weeks or more during which you felt sad, blue, or depressed or lost pleasure in things you usually cared about or enjoyed?” on a scale of 0–1, no to yes. Adapted from the Kidney Disease and Quality of Life Short Form. | Hays et al. (46) | Mortality (46, 47); hospitalization (47) |
| General health rating | “In general, how would you say your health is?” on a scale of 1–5, excellent to poor, from 12-item short-form health survey. | Ware et al. (48) | Survival (49); functional limitations (49); objective physical/mental health symptoms (48) |
| Pain interference | “During the past 4 weeks, how much did pain interfere with your normal work [including both work outside the home and housework]?”), on a scale of 1–5, not at all to extremely, from 12-item short-form health survey. | Ware et al. (48) | Objective physical/mental health symptoms (48) |
| Life satisfaction | “All things considered, how satisfied are you with your life as a whole?”; on a scale of 1–5, very satisfied to very dissatisfied. | Andrews and Withey (50) | Social support (51) |
| Isolation | “How often do you feel isolated from others?”, on a scale of 1–3, hardly ever to often. | Hughes et al. (52) | Blood pressure (53); depressive symptoms (52) |
| Cognitive ability | 13-item Cognitive Assessment Screening Test (CAST) measuring perceptions of cognitive ability, on a scale of 0–1, no to yes. | Swearer et al. (54) | Neuropsychological battery (54) |
| Perceived stress | 4-item perceived stress short form, on a scale of 0–4, never to often. | Cohen et al. (55) | Respiratory illness (56); coronary artery disease (57) |
| Body mass index | Weight and height were self-reported. | Objective height and weight (58) | |
| Lower-extremity function | 11-item advanced lower-extremity subscale of the Late-Life Function and Disability Instrument assessed a broad range of functioning capabilities requiring lower-body function, on a scale of 1–5, cannot do to no difficulty (higher score = better). | Haley et al. (59) | Short Physical Performance Battery (30); 400-m walk test (30) |
Data analysis
Age- and gender-specific descriptive analyses were used to examine sample differences by study covariates and patterns of physical activity across intensity categories. Test-retest reliability of intensity categories was assessed by calculating one-way random-effects intraclass correlation coefficients (25) between the 2 assessments.
To reduce type I error, an exploratory factor analysis of the self-reported health parameters was performed prior to formal data analysis. Principal components extraction was used to derive the fewest number of relevant and distinct factors. A promax rotation method was used to enhance interpretability of the resultant factors and allow for nonorthogonality given that health domains are likely to be correlated (26). Visual analysis of the scree plot, communality estimates for individual items, and eigenvalues of ≥1.0 were used as criteria to identify relevant factors. Factor scoring coefficients from each item were used to generate composite factor scores for formal data analysis. Because most parameters had a negative valence, factor scores were reflected (multiplied by −1) so that higher scores represented more positive health and well-being.
Mixed-effects regression models (using SAS PROC MIXED; SAS Institute, Inc., Cary, North Carolina) were fitted to the composite factor scores generated from the exploratory factor analysis. A repeated-measures framework was used to account for factors that were measured twice (6-month interval), including body mass index, lower-extremity function, and accelerometry data. The analyses also took neighborhood clustering (i.e., block group) into account; thus, 3-level multilevel models were fitted to account for repeated measures nested within subjects and subjects nested within neighborhoods. All models were adjusted for study covariates (described earlier).
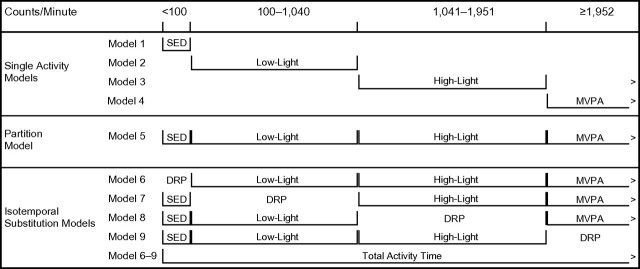
Three regression models were fitted to assess associations between intensity categories and health variables. Refer to Figure 1 for graphic depictions of these models. First, single activity models were used to estimate the “total effect” for MVPA, HLPA, LLPA, and sedentary activity (Figure 1, models 1–4). These models depict the raw associations between each intensity category and the health variables. Second, partition models were used to estimate the “unique effect” of each intensity category while holding time in other intensities constant (Figure 1, model 5). These models depict the unique association of each intensity category with health variables. Finally, isotemporal substitution models were used to estimate the “substitution effect” of replacing activity from one intensity category for an equal amount of time in a different category (Figure 1, models 6–9). This was accomplished by entering a total activity time variable (i.e., sedentary + LLPA + HLPA + MVPA) and unique activity for each intensity category to the models simultaneously. The intensity category of interest is then dropped from the model. These models depict the effect of replacing activity from the dropped category with other categories entered in the model. By including a summary total activity variable in the model, total time is constrained and allows direct comparisons to be made between activity categories and their impacts on a health variable of interest. Greater detail on isotemporal substitution models is presented elsewhere (27).
Figure 1.
Selected physical activity intensity thresholds and 3 types of regression models used to test associations with health metrics in the Senior Neighborhood Quality of Life Study, United States, 2005–2007. Single activity models tested the “total effect” of each threshold, unadjusted for activity in other thresholds. Partition models tested the “unique effect” of each threshold adjusted for activity in other thresholds. Isotemporal substitution models tested the “substitution effect” of each threshold holding time constant. DRP, parameter dropped from model; MVPA, moderate/vigorous physical activity; SED, sedentary; >, no upper threshold set.
Prior to entry into the models, all intensity categories were divided by a constant of 30 such that a unit increase in the activity variable represented an increase of 30 minutes/day within the given intensity category. This step was performed to improve interpretability of the results in light of national guidelines for physical activity (28). The health variable scores derived from the exploratory factor analysis were standardized such that the mean was 0 and a unit increase was equal to 1 standard deviation (i.e., z-score metric). All analyses were completed using SAS Enterprise Guide 4.2 software (SAS Institute, Inc.).
RESULTS
Descriptive and accelerometer wear data
Study sample demographics by age group and gender are presented in Table 1. Demographics were similar by gender (albeit with more women than men, as expected in older age categories), with participants generally overweight/obese, white/Caucasian, living independently, not currently smoking, and well educated. By design, the sample was balanced by neighborhood income level, geographic information system–derived walkability, and region.
Descriptive statistics for accelerometry data by age group and gender are presented in Table 2. Activity was monitored during a range of 3–13 valid days during each assessment period, with 91.5% of the sample having ≥7 valid days. We found no differences in valid days of wear time by age or gender; however, compared with women, men had more valid hours of wear time per valid day at both assessments. Significant trends (all P < 0.001) were present such that LLPA, HLPA, and MVPA decreased and sedentary time increased with age; and, compared with women, men had more minutes of sedentary time, HLPA, and MVPA and fewer minutes of LLPA.
Table 2.
Demographic Characteristics by Age Group and Gender, Senior Neighborhood Quality of Life Study, United States, 2005–2007
| Variable | Age 66–69 Years |
Age 70–79 Years |
Age ≥80 Years |
Total | |||
| Men | Women | Men | Women | Men | Women | ||
| No. of participants | 109 | 106 | 182 | 229 | 89 | 147 | 862 |
| Mean age, years | 67.4 | 67.4 | 74.4 | 74.3 | 84.4 | 84.6 | 75.4 |
| Mean body mass index, a % | 27.2 | 27.3 | 26.8 | 26.6 | 25.4 | 25.0 | 26.4 |
| Normal | 24.8 | 37.7 | 33.5 | 46.3 | 51.7 | 54.4 | 41.8 |
| Overweight | 56.0 | 38.7 | 50.5 | 28.4 | 34.8 | 32.7 | 39.2 |
| Obese | 19.3 | 23.6 | 15.9 | 25.3 | 13.5 | 12.9 | 19.0 |
| Race, % | |||||||
| White/Caucasian | 70.6 | 61.0 | 69.6 | 65.1 | 88.8 | 81.0 | 71.4 |
| Black/African American | 20.2 | 28.6 | 17.7 | 27.9 | 4.5 | 16.3 | 20.5 |
| Other | 9.2 | 10.5 | 12.7 | 7.0 | 6.7 | 2.7 | 8.1 |
| Educational status, % | |||||||
| ≤High school diploma | 5.6 | 7.5 | 7.7 | 8.7 | 4.5 | 6.1 | 6.7 |
| Some college | 39.8 | 58.5 | 33.0 | 50.7 | 31.5 | 59.9 | 45.9 |
| ≥College diploma | 54.6 | 34.0 | 59.3 | 40.6 | 64.0 | 34.0 | 47.4 |
| Married or living with a partner, % | 80.6 | 41.9 | 78.0 | 37.1 | 69.7 | 17.0 | 51.7 |
| Senior housing resident, % | 5.5 | 17.9 | 8.2 | 15.7 | 30.3 | 41.5 | 19.0 |
| Current smoker, b % | 11.0 | 8.5 | 8.2 | 15.7 | 6.7 | 3.4 | 6.4 |
| Neighborhood characteristics, % | |||||||
| High income | 54.1 | 47.2 | 53.8 | 43.7 | 56.2 | 50.3 | 50.0 |
| High walkability | 47.7 | 57.5 | 47.8 | 53.3 | 59.6 | 59.2 | 53.6 |
| Region, % | |||||||
| Seattle, Washington | 50.5 | 39.6 | 52.7 | 45.0 | 68.5 | 61.9 | 52.0 |
| Baltimore, Maryland | 49.5 | 60.4 | 47.3 | 55.0 | 31.5 | 38.1 | 48.0 |
Body mass index classification: normal (<25 kg/m2), overweight (25–29 kg/m2), obese (≥30 kg/m2).
Defined as smoking a cigarette, cigar, or pipe in the past 7 days.
Results from exploratory factor analyses of health variables
From the original 13 self-reported health variables, 3 were eliminated from the analysis given exploratory factor analysis–derived communality estimates of ≤0.20. Descriptive data for the remaining 10 variables and factor loadings are displayed in Table 3. The exploratory factor analysis yielded 2 factors with eigenvalues of ≥1.0, which together accounted for 49% of the total variance. These factors appeared to broadly represent physical health and psychosocial well-being. Three items showed evidence of cross-loadings (general health rating, lower-extremity function, and pain interference). These items were retained and permitted to load on both factors because these domains have displayed previous associations with other objective measures of physical health (29, 30) and well-being factors (31), and they have strong factorial relevance for each of these composite factors. Despite the cross-loadings, the 2 composite factors were only modestly correlated at r = 0.32. To illustrate how individual health indicator data were reflected in the composite factors, descriptive data are presented in Table 4 for individuals >1 standard deviation from the composite factors means.
Table 3.
Mean Accelerometer Wear Data by Age and Gender, Senior Neighborhood Quality of Life Study, United States, 2005–2007
| Variable | Age 66–69 Years |
Age 70–79 Years |
Age ≥80 Years |
Total | P for Age Trenda | P for Gendera | |||
| Men | Women | Men | Women | Men | Women | ||||
| Time 1 (N = 862) | |||||||||
| Valid days of wear | 7.0 | 7.1 | 7.0 | 7.0 | 7.0 | 6.9 | 7.0 | 0.337 | 0.776 |
| Valid hours per valid day | 14.7 | 14.2 | 14.8 | 14.5 | 14.4 | 14.2 | 14.5 | 0.075 | 0.007 |
| Intensity category, minutes/day | |||||||||
| Sedentary | 544.8 | 518.5 | 581.8 | 546.6 | 604.3 | 585.7 | 563.0 | <0.001 | <0.001 |
| Low-light | 282.1 | 293.7 | 264.3 | 289.9 | 227.6 | 247.9 | 270.0 | <0.001 | <0.001 |
| High-light | 35.5 | 25.1 | 24.1 | 21.8 | 17.8 | 11.8 | 22.2 | <0.001 | <0.001 |
| MVPA | 21.3 | 15.2 | 15.3 | 10.4 | 11.6 | 4.0 | 12.3 | <0.001 | <0.001 |
| Time 2 (N = 765) | |||||||||
| Valid days of wear | 6.8 | 7.0 | 6.8 | 6.9 | 7.1 | 6.8 | 6.9 | 0.872 | 0.501 |
| Valid hours per valid day | 14.6 | 14.0 | 14.6 | 14.3 | 14.8 | 14.2 | 14.4 | 0.785 | 0.001 |
| Intensity category, minutes/day | |||||||||
| Sedentary | 549.0 | 504.4 | 575.9 | 543.7 | 629.9 | 588.6 | 562.1 | <0.001 | <0.001 |
| Low-light | 272.4 | 296.2 | 259.6 | 286.1 | 232.3 | 249.9 | 268.6 | <0.001 | <0.001 |
| High-light | 33.1 | 25.2 | 24.5 | 20.9 | 16.2 | 11.4 | 21.8 | <0.001 | <0.001 |
| MVPA | 22.3 | 14.4 | 14.2 | 9.8 | 10.7 | 4.5 | 12.2 | <0.001 | <0.001 |
Abbreviation: MVPA, moderate/vigorous physical activity.
All P values are 2-sided.
Table 4.
Mean (SD), Factor Loadings, and Scores for Participants Exceeding ±1.0 SD on Factor Scores for Self-reported Health Outcomes, Senior Neighborhood Quality of Life Study, United States, 2005–2007
| Variable | Mean (SD) | Factor Loadingsa,b |
Factor Score |
||||
| Physical Health |
Psychosocial Well-Being |
||||||
| Physical Health | Psychosocial Well-Being | ≤−1.0 SD | ≥1.0 SD | ≤−1.0 SD | ≥1.0 SD | ||
| Eigenvalue | 3.39 | 1.50 | |||||
| No. of medical conditions | 1.30 (1.03) | 0.80 | 2.04 (1.16) | 0.18 (0.39) | |||
| No. of medications | 3.23 (1.68) | 0.79 | 4.13 (1.34) | 0.93 (1.06) | |||
| General health rating | 2.55 (0.92) | 0.62c | 0.45c | 3.58 (0.71) | 1.70 (0.71) | 3.33 (0.82) | 1.79 (0.65) |
| Body mass index | 26.4 (4.7) | 0.46 | 28.76 (6.01) | 23.69 (2.88) | |||
| Lower-body physical function | 52.42 (16.74) | −0.65c | −0.32c | 41.75 (18.14) | 71.59 (12.81) | 46.28 (18.34) | 68.10 (16.70) |
| Stress | 3.53 (2.75) | 0.72 | 6.74 (2.31) | 0.50 (0.79) | |||
| Life satisfaction | 1.71 (0.82) | 0.68 | 2.65 (1.04) | 1.02 (0.13) | |||
| Isolation | 1.30 (0.53) | 0.67 | 1.96 (0.64) | 1.00 (0.00) | |||
| Feeling depressed/blue | 0.11 (0.31) | 0.59 | 0.35 (0.48) | 0.00 (0.00) | |||
| Pain interference | 2.01 (1.10) | 0.49c | 0.50c | 3.19 (1.08) | 1.28 (0.60) | 3.05 (1.27) | 1.15 (0.38) |
Abbreviation: SD, standard deviation.
Factor loadings of ≤0.20 are not shown.
Items for confusion, number of falls in the past year, and perceptions of cognitive ability were eliminated because of communality estimates of ≤0.20.
Factor loadings for cross-loading items.
Test-retest stability and bivariate correlations among intensity thresholds and health factors
Bivariate correlations among the different intensity categories, physical health, and well-being are displayed in Table 5. Associations between LLPA, HLPA, and MVPA were positive and showed stronger associations among adjacent categories than nonadjacent categories (i.e., a simplex pattern). The correlations between sedentary time and the other intensity categories were negative and also followed a simplex pattern. The correlations between the intensity categories and the physical health factor were positive (higher scores = better physical health) and generally of moderate magnitude (however, they were weak for LLPA). The correlations among physical activity categories and the psychosocial factor were also positive but generally weaker in magnitude. Sedentary time was not statistically correlated with the physical or psychosocial health factors. The intraclass correlation coefficient values were acceptable for all intensity categories.
Table 5.
Pearson Product Moment Correlation Coefficients and Intraclass Correlation Coefficients for Sedentary, Low-Light, High-Light, and Moderate/Vigorous Physical Activity Categories and Health Factors, Senior Neighborhood Quality of Life Study, United States, 2005–2007
| Sedentary | LLPA | HLPA | MVPA | Factora |
ICC | ||
| Physical Health | Psychosocial Well-Being | ||||||
| Sedentary | 1.00 | −0.36** | −0.31** | −0.12** | −0.07* | 0.04 | 0.69 |
| LLPA | 1.00 | 0.50** | 0.16** | 0.29** | 0.12** | 0.68 | |
| HLPA | 1.00 | 0.54** | 0.40** | 0.19** | 0.74 | ||
| MVPA | 1.00 | 0.37** | 0.13** | 0.80 | |||
Abbreviations: HLPA, high-light physical activity; ICC, intraclass correlation coefficient; LLPA, low-light physical activity; MVPA, moderate/vigorous physical activity.
*P < 0.05; **P < 0.001.
Factor scores have been reflected (multiplied by −1), so higher scores represent better health and well-being.
Intensity category associations with physical and psychosocial health factor scores
Three statistical models—single, partition, and isotemporal substitution (refer to the “Data analysis” section of the text and Figure 1)—were used to examine associations between each intensity category and physical health and well-being. Results are presented in Table 6, where model numbers represent the analytical approach (refer to Figure 1), and lowercase letters represent the outcome (a = physical health; b = psychosocial well-being). The total effects of MVPA, HLPA, LLPA, and sedentary time were tested using the single activity models. For physical health, sedentary time (model 1a) was negatively associated with physical health, whereas LLPA (model 2a), HLPA (model 3a), and MVPA (model 4a) were positively associated with physical health. The strongest association with physical health was with HLPA, where an increase of 30 minutes/day was associated with a 0.46 standard deviation increase in physical health score. For well-being, sedentary time (model 1b) was modestly, but negatively, associated with well-being, whereas HLPA (model 3a) was positively associated with well-being. MVPA (model 4a) and LLPA (model 2a) were unrelated to well-being.
Table 6.
Single Activity, Partition, and Isotemporal Substitution Models per a 30-Minute/Day Increase in Sedentary, Low-Light, High-Light, and Moderate/Vigorous Physical Activity and Physical Health and Psychosocial Well-Being Factors, Senior Neighborhood Quality of Life Study, United States, 2005–2007
| Analysis Method (Modela) | Sedentary |
Low-Light |
High-Light |
MVPA |
||||
| βb | 95% CI | βb | 95% CI | βb | 95% CI | βb | 95% CI | |
| Physical health (a)c | ||||||||
| Single activity (models 1a–4a) | −0.09 | −0.10, −0.06 | 0.07 | 0.05, 0.09 | 0.46 | 0.37, 0.54 | 0.37 | 0.28, 0.46 |
| Partition (model 5a) | −0.02 | −0.00, −0.03 | 0.08 | 0.06, 0.11 | 0.32 | 0.21, 0.44 | 0.38 | 0.28, 0.48 |
| Isotemporal substitutiond | ||||||||
| Replace sedentary (model 6a) | Dropped | 0.07 | 0.04, 0.09 | 0.30 | 0.19, 0.42 | 0.34 | 0.23, 0.44 | |
| Replace low-light (model 7a) | −0.07 | −0.09, −0.04 | Dropped | 0.24 | 0.11, 0.36 | 0.21 | 0.10, 0.32 | |
| Replace high-light (model 8a) | −0.30 | −0.42, −0.19 | −0.24 | −0.36, −0.11 | Dropped | −0.27 | −0.55, 0.01 | |
| Replace MVPA (model 9a) | −0.17 | −0.22, −0.12 | −0.10 | −0.16, −0.05 | 0.14 | −0.06, 0.27 | Dropped | |
| Psychosocial well-being (b)c | ||||||||
| Single activity (models 1b–4b) | −0.03 | −0.05, −0.01 | 0.02 | −0.00, 0.05 | 0.23 | 0.13, 0.32 | 0.08 | −0.02, 0.18 |
| Partition (model 5b) | 0.04 | 0.02, 0.05 | 0.04 | 0.02, 0.07 | 0.27 | 0.16, 0.40 | 0.06 | −0.05, 0.17 |
| Isotemporal substitutiond | ||||||||
| Replace sedentary (model 6b) | Dropped | 0.01 | −0.02, 0.04 | 0.24 | 0.12, 0.36 | −0.02 | −0.13, 0.10 | |
| Replace low-light (model 7b) | −0.01 | −0.04, 0.02 | Dropped | 0.24 | 0.10, 0.37 | −0.03 | −0.15, 0.08 | |
| Replace high-light (model 8b) | −0.24 | −0.36, −0.12 | −0.24 | −0.37, −0.10 | Dropped | −0.50 | −0.81, −0.19 | |
| Replace MVPA (model 9b) | 0.01 | −0.05, 0.07 | 0.02 | −0.04, 0.08 | 0.25 | 0.10, 0.41 | Dropped | |
Abbreviations: CI, confidence interval; MVPA, moderate/vigorous physical activity.
Model numbers refer to those specified in Figure 1, and parenthetical letters refer to physical health (a) and psychosocial well-being (b) factors.
All models were adjusted for age (years), gender, race (white, African American, other), education (≤high school diploma, some college, ≥college diploma), senior housing resident status, current smoking status, site (Baltimore, Maryland, or Seattle, Washington), marital status (married/living with a partner or single/widowed), neighborhood-level walkability, neighborhood-level income, and accelerometer wear time (valid hours/valid days). Neighborhood clustering was adjusted for in all models. Models were adjusted to account for repeated measurement of all accelerometer variables, the Late-Life Physical Disability Inventory-Advanced lower extremity score, and body mass index.
Post-hoc models were conducted for selected single indicators contained in health factors (body mass index, general health rating, lower-extremity function). Single indicators followed similar pattern of results, except for body mass index, which had greater inverse associations with MVPA than high-light and low-light activity did.
Total activity time was entered in the isotemporal substitution models.
The unique effect of each intensity category on the health factors was also examined using partition models. For physical health, MVPA, HLPA, LLPA, and sedentary behavior retained significance in the expected direction (model 5a), suggesting that activity in each category was associated with physical health. For well-being, sedentary activity, LLPA, and HLPA were positively associated, whereas MVPA was not (model 5b).
The effect of substituting one physical activity category with another was tested using isotemporal substitution models. For physical health, the sedentary model (model 6a) suggested that substituting 30 minutes/day of sedentary activity with MVPA, HLPA, and LLPA resulted in a 0.34 standard deviation, 0.30 standard deviation, and 0.07 standard deviation increase in physical health, respectively. Models comparing HLPA with MVPA (models 8a–9a) showed no substitution effects for these activity intensities, suggesting that the 2 were interchangeable with respect to their associations with physical health. HLPA conferred a positive effect on well-being over all other activity intensities (model 8b). No other substitution effects were significant for well-being.
Finally, exploratory post-hoc analyses were conducted to examine selected health indicators individually (body mass index, general health rating, lower-extremity function). The single indicators followed patterns similar to the composite health score, with the exception of body mass index. Sedentary behavior, LLPA, HLPA, and MVPA were each independently associated with body mass index in the expected directions; however, MVPA had a stronger association with body mass index than did other intensity categories.
DISCUSSION
There were 4 primary results from this investigation. First, older adults spent considerable time performing activities not captured in the sedentary and MVPA categories (approximately 4.9 hours/day), with the majority of this time spent in LLPA. Furthermore, the amount of time spent engaging in light activities was reasonably stable over 6 months. Second, when their unique effects were examined (i.e., partition models), both LLPA and HLPA were positively associated with physical health and well-being. Third, in the isotemporal substitution models, replacing 30 minutes/day of sedentary time with an equal amount of LLPA, HLPA, or MVPA was associated with a higher physical health score. Fourth, the physical health benefits of HLPA were in the same range as those for MVPA, and HLPA appeared to confer greater psychosocial well-being benefits than all other forms of activity.
The descriptive accelerometry data presented in Table 2 showed, as expected, that older adults spent the majority of their day in the sedentary range of activities. Among other categories, older adults spent the most time in LLPA, a range that represented approximately half the intensity range between sedentary and MVPA. This profile of activity appeared to be similar for each age group and gender combination examined, and the expected age and gender differences observed for MVPA were also present for LLPA and HLPA. These data are consistent with nationally representative data from the National Health and Nutrition Examination Survey for sedentary behavior (19) and MVPA (16), despite minor differences in how MVPA was defined.
The single activity, partition, and isotemporal substitution models offered generally consistent results indicating that light-intensity physical activity, particularly HLPA, was associated with better physical health and well-being. These associations held even after adjusting for time spent in other intensity categories. These models did, however, offer important distinctions within these associations that warrant discussion. The partition models represented the unconfounded “unique effect” between each intensity category and physical health and well-being. For physical health, all intensity categories were significantly related to this factor. This finding replicates those from other studies using objective physical activity measurement indicating that moderate (32), sedentary (3), and light (33) activities have unique associations with various health parameters.
The present study extends previous findings in 2 important ways. First, in one of the few studies we are aware of that examined objectively measured light-intensity activity in relation to health (33), light activity was broadly specified to account for all activity between sedentary and MVPA (100–1,951 counts/minute). The present study provides a more refined analysis utilizing an intermediate threshold with empirical support in older populations (10). This disaggregation of light activity into “low-light” and “high-light” appears to be important, because we found that the majority of health benefits for light-intensity activity seemed to occur in the HLPA range. In the absence of well-established thresholds for MVPA in older populations, it is not currently clear whether the HLPA associations we observed actually represent age-adjusted moderate-intensity activity or, alternatively, activity falling below moderate-intensity into the “light” category. Future research should continue exploring this issue and specifically examine relative activity intensity and accelerometer thresholds in older populations.
Second, the present physical health factor represents a broad range of health-related indicators (chronic conditions, physical function, medication use, etc.), unlike other studies that focused on individual factors such as weight change (27), blood glucose (33), and individual self-reported health indicators (34). While understanding specific associations with different health indicators is valuable, the present study demonstrated the breadth of the associations between light physical activity and a more general metric of physical health and is an important first step in exploring light-intensity associations with health.
The isotemporal substitution models indicated that substituting sedentary time with an equal amount of LLPA, HLPA, or MVPA was associated with better physical health, with HLPA and MVPA conferring similar physical health benefits. These results suggest that recommending replacement of sedentary activities (e.g., television viewing, sitting) with HLPA (e.g., leisure walking, active transport), and not necessarily focusing exclusively on MVPA (e.g., brisk walking), may be appropriate. Future longitudinal studies are needed to more formally examine this result.
Associations between various activity categories and psychosocial well-being in the partition model were weaker compared with physical health. Similar to physical health, the well-being factor represented a broad range of indicators tapping aspects of quality of life, stress, and mental health. The finding that only sedentary behavior, LLPA, and HLPA were associated with rated well-being is inconsistent with literature demonstrating the effects of MVPA on depressive symptoms (35) and psychological well-being (36). Our results are, however, consistent with evidence that lighter activities associated with increased socialization in later life are related to indicators of well-being (37). Surprisingly, isotemporal substitution models found that HLPA conferred significant replacement effects on psychosocial well-being compared with all other ranges of activities, suggesting that individuals engaging in more activities in the high-light range (e.g., leisure walking) were more likely to have less stress, increased socialization, and greater quality of life.
Among its strengths, this study included a relatively large sample of older adults from 2 geographically distinct metropolitan US regions that appeared to yield physical activity levels very similar to those of a nationally representative sample (16, 19). There was high compliance with the study protocol, and physical activity was assessed with a commonly used and well-validated accelerometer (Actigraph). The study included two 7-day accelerometry assessment periods 6 months apart, with good test-retest reliability, providing a stable estimate of habitual physical activity.
There are some potential limitations of the present study. First, the study design limited causal inferences between intensity categories and rated health. Second, the study relied on rated health parameters and did not assess objective health indicators. Third, a common association between MVPA and psychosocial well-being was not observed, which may have been due to abbreviated items or greater measurement error when attempting to assess psychosocial constructs as opposed to physical health constructs (38). It may also have been due to the population-based sampling method used in the current study, which reflects a more generalizable population than has typically been enrolled in studies in the field. Fourth, individuals self-selected to participate after initial random recruitment. Although our physical activity estimates seem in line with those from a nationally representative sample, racial minorities and less educated individuals may have been underrepresented, and these groups are likely to report their health more poorly. Finally, the use of accelerometry-based thresholds to define light-intensity activities makes the types/modalities of activities that fit into these categories difficult to determine. More research is needed to understand what specific recommendations can be given to older adults to ensure that activities they are performing are able to meet these thresholds.
The present study adds to broader evidence that increased physical activity and decreased sedentary behavior are associated with health in older adults. A key contribution of the present study was evidence that, after controlling for sedentary time and MVPA, light-intensity activities (defined as falling below the commonly used Freedson threshold), particularly HLPA, were associated with better physical health and that HLPA conferred significant benefits to well-being over other activity intensities. Continued investigation into light-intensity activity, particularly HLPA, is warranted because these activities appeal to and are feasible for older adults.
Acknowledgments
Author affiliations: Stanford Prevention Research Center, Department of Medicine, Stanford University School of Medicine, Stanford, California (Matthew P. Buman, Eric B. Hekler, William L. Haskell, Leslie Pruitt, Abby C. King); Department of Psychology, San Diego State University, San Diego, California (Terry L. Conway, Kelli L. Cain, James F. Sallis); Department of Pediatrics, University of Washington and Seattle Children's Hospital Research Institute, Seattle, Washington (Brian E. Saelens); School of Community and Regional Planning, University of British Columbia, Vancouver, British Columbia, Canada (Lawrence D. Frank); and Health Research and Policy, Department of Medicine, Stanford University School of Medicine, Stanford, California (Abby C. King).
This study was supported by US Public Health Service Grant 5R01HL077141 (to Dr. King) from the National Heart, Lung, and Blood Institute (Bethesda, Maryland). Drs. Buman and Hekler were supported by US Public Health Service Grant 5T32HL007034 from the National Heart, Lung, and Blood Institute.
Conflict of interest: none declared.
Glossary
Abbreviations
- HLPA
high-light physical activity
- LLPA
low-light physical activity
- MVPA
moderate/vigorous physical activity
References
- 1.Katzmarzyk PT, Church TS, Craig CL, et al. Sitting time and mortality from all causes, cardiovascular disease, and cancer. Med Sci Sports Exerc. 2009;41(5):998–1005. doi: 10.1249/MSS.0b013e3181930355. [DOI] [PubMed] [Google Scholar]
- 2.Healy GN, Dunstan DW, Shaw JE, et al. Beneficial associations of physical activity with 2-h but not fasting blood glucose in Australian adults: the AusDiab Study. Diabetes Care. 2006;29(12):2598–2604. doi: 10.2337/dc06-0313. [DOI] [PubMed] [Google Scholar]
- 3.Healy GN, Wijndaele K, Dunstan DW, et al. Objectively measured sedentary time, physical activity, and metabolic risk: the Australian Diabetes, Obesity and Lifestyle Study (AusDiab) Diabetes Care. 2008;31(2):369–371. doi: 10.2337/dc07-1795. [DOI] [PubMed] [Google Scholar]
- 4.Westerterp KR. Physical activity as determinant of daily energy expenditure. Physiol Behav. 2008;93(4-5):1039–1043. doi: 10.1016/j.physbeh.2008.01.021. [DOI] [PubMed] [Google Scholar]
- 5.Feskanich D, Willett W, Colditz G. Walking and leisure-time activity and risk of hip fracture in postmenopausal women. JAMA. 2002;288(18):2300–2306. doi: 10.1001/jama.288.18.2300. [DOI] [PubMed] [Google Scholar]
- 6.Brawley LR, Rejeski WJ, King AC. Promoting physical activity for older adults: the challenges for changing behavior. Am J Prev Med. 2003;25(3) suppl. 2:172–183. doi: 10.1016/s0749-3797(03)00182-x. [DOI] [PubMed] [Google Scholar]
- 7.Washburn RA. Assessment of physical activity in older adults. Res Q Exerc Sport. 2000;71(2 suppl):S79–S88. [PubMed] [Google Scholar]
- 8.Campbell AJ, Robertson MC, Gardner MM, et al. Randomised controlled trial of a general practice programme of home based exercise to prevent falls in elderly women. BMJ. 1997;315(7115):1065–1069. doi: 10.1136/bmj.315.7115.1065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Starling RD, Matthews DE, Ades PA, et al. Assessment of physical activity in older individuals: a doubly labeled water study. J Appl Physiol. 1999;86(6):2090–2096. doi: 10.1152/jappl.1999.86.6.2090. [DOI] [PubMed] [Google Scholar]
- 10.Copeland JL, Esliger DW. Accelerometer assessment of physical activity in active, healthy older adults. J Aging Phys Act. 2009;17(1):17–30. doi: 10.1123/japa.17.1.17. [DOI] [PubMed] [Google Scholar]
- 11.Pruitt LA, Glynn NW, King AC, et al. Use of accelerometry to measure physical activity in older adults at risk for mobility disability. J Aging Phys Act. 2008;16(4):416–434. doi: 10.1123/japa.16.4.416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Freedson PS, Melanson E, Sirard J. Calibration of the Computer Science and Applications, Inc. accelerometer. Med Sci Sports Exerc. 1998;30(5):777–781. doi: 10.1097/00005768-199805000-00021. [DOI] [PubMed] [Google Scholar]
- 13.Shigematsu R, Sallis JF, Conway TL, et al. Age differences in the relation of perceived neighborhood environment to walking. Med Sci Sports Exerc. 2009;41(2):314–321. doi: 10.1249/MSS.0b013e318185496c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Frank LD, Sallis JF, Saelens BE, et al. The development of a walkability index: application to the Neighborhood Quality of Life Study [published online ahead of print April 29, 2010] Br J Sports Med. doi: 10.1136/bjsm.2009.058701. (doi:10.1136/bjsm.2009.058701) [DOI] [PubMed] [Google Scholar]
- 15.Sallis JF, Saelens BE, Frank LD, et al. Neighborhood built environment and income: examining multiple health outcomes. Soc Sci Med. 2009;68(7):1285–1293. doi: 10.1016/j.socscimed.2009.01.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Troiano RP, Berrigan D, Dodd KW, et al. Physical activity in the United States measured by accelerometer. Med Sci Sports Exerc. 2008;40(1):181–188. doi: 10.1249/mss.0b013e31815a51b3. [DOI] [PubMed] [Google Scholar]
- 17.Nichols JF, Morgan CG, Chabot LE, et al. Assessment of physical activity with the Computer Science and Applications, Inc., accelerometer: laboratory versus field validation. Res Q Exerc Sport. 2000;71(1):36–43. doi: 10.1080/02701367.2000.10608878. [DOI] [PubMed] [Google Scholar]
- 18.Sirard JR, Melanson EL, Li L, et al. Field evaluation of the Computer Science and Applications, Inc. physical activity monitor. Med Sci Sports Exerc. 2000;32(3):695–700. doi: 10.1097/00005768-200003000-00022. [DOI] [PubMed] [Google Scholar]
- 19.Matthews CE, Chen KY, Freedson PS, et al. Amount of time spent in sedentary behaviors in the United States, 2003–2004. Am J Epidemiol. 2008;167(7):875–881. doi: 10.1093/aje/kwm390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Estabrooks PA, Smith-Ray RL. Piloting a behavioral intervention delivered through interactive voice response telephone messages to promote weight loss in a pre-diabetic population. Patient Educ Couns. 2008;72(1):34–41. doi: 10.1016/j.pec.2008.01.007. [DOI] [PubMed] [Google Scholar]
- 21.Fitzgibbon ML, Stolley M, Schiffer L, et al. Obesity Reduction Black Intervention Trial (ORBIT): design and baseline characteristics. J Womens Health (Larchmt) 2008;17(7):1099–1110. doi: 10.1089/jwh.2007.0614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Keyserling TC, Samuel Hodge CD, Jilcott SB, et al. Randomized trial of a clinic-based, community-supported, lifestyle intervention to improve physical activity and diet: the North Carolina enhanced WISEWOMAN project. Prev Med. 2008;46(6):499–510. doi: 10.1016/j.ypmed.2008.02.011. [DOI] [PubMed] [Google Scholar]
- 23.Opdenacker J, Boen F, Coorevits N, et al. Effectiveness of a lifestyle intervention and a structured exercise intervention in older adults. Prev Med. 2008;46(6):518–524. doi: 10.1016/j.ypmed.2008.02.017. [DOI] [PubMed] [Google Scholar]
- 24.Miller NE, Strath SJ, Swartz AM, et al. Estimating absolute and relative physical activity intensity across age via accelerometry in adults. J Aging Phys Act. 2010;18(2):158–170. doi: 10.1123/japa.18.2.158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Shrout PE, Fleiss JL. Intraclass correlations: uses in assessing rater reliability. Psychol Bull. 1979;86(2):420–428. doi: 10.1037//0033-2909.86.2.420. [DOI] [PubMed] [Google Scholar]
- 26.Barth J, Schumacher M, Herrmann-Lingen C. Depression as a risk factor for mortality in patients with coronary heart disease: a meta-analysis. Psychosom Med. 2004;66(6):802–813. doi: 10.1097/01.psy.0000146332.53619.b2. [DOI] [PubMed] [Google Scholar]
- 27.Mekary RA, Willett WC, Hu FB, et al. Isotemporal substitution paradigm for physical activity epidemiology and weight change. Am J Epidemiol. 2009;170(4):519–527. doi: 10.1093/aje/kwp163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Physical Activity Guidelines Advisory Committee. Physical Activity Guidelines Advisory Committee Report. Washington, DC: US Department of Health and Human Services; 2008. [DOI] [PubMed] [Google Scholar]
- 29.Idler EL, Benyamini Y. Self-rated health and mortality: a review of twenty-seven community studies. J Health Soc Behav. 1997;38(1):21–37. [PubMed] [Google Scholar]
- 30.Sayers SP, Jette AM, Haley SM, et al. Validation of the Late-Life Function and Disability Instrument. J Am Geriatr Soc. 2004;52(9):1554–1559. doi: 10.1111/j.1532-5415.2004.52422.x. [DOI] [PubMed] [Google Scholar]
- 31.Karp JF, Skidmore E, Lotz M, et al. Use of the late-life function and disability instrument to assess disability in major depression. J Am Geriatr Soc. 2009;57(9):1612–1619. doi: 10.1111/j.1532-5415.2009.02398.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Ekelund U, Griffin SJ, Wareham NJ. Physical activity and metabolic risk in individuals with a family history of type 2 diabetes. Diabetes Care. 2007;30(2):337–342. doi: 10.2337/dc06-1883. [DOI] [PubMed] [Google Scholar]
- 33.Healy GN, Dunstan DW, Salmon J, et al. Objectively measured light-intensity physical activity is independently associated with 2-h plasma glucose. Diabetes Care. 2007;30(6):1384–1389. doi: 10.2337/dc07-0114. [DOI] [PubMed] [Google Scholar]
- 34.Harris TJ, Owen CG, Victor CR, et al. A comparison of questionnaire, accelerometer, and pedometer: measures in older people. Med Sci Sports Exerc. 2009;41(7):1392–1402. doi: 10.1249/MSS.0b013e31819b3533. [DOI] [PubMed] [Google Scholar]
- 35.Dunn AL, Trivedi MH, O'Neal HA. Physical activity dose-response effects on outcomes of depression and anxiety. Med Sci Sports Exerc. 2001;33(6 suppl):S587–S597. doi: 10.1097/00005768-200106001-00027. [DOI] [PubMed] [Google Scholar]
- 36.Spirduso WW, Cronin DL. Exercise dose-response effects on quality of life and independent living in older adults. Med Sci Sports Exerc. 2001;33(6 suppl):S598–S608. doi: 10.1097/00005768-200106001-00028. [DOI] [PubMed] [Google Scholar]
- 37.Pinquart M, Sörensen S. Influences of socioeconomic status, social network, and competence on subjective well-being in later life: a meta-analysis. Psychol Aging. 2000;15(2):187–224. doi: 10.1037//0882-7974.15.2.187. [DOI] [PubMed] [Google Scholar]
- 38.Schmidt FL, Hunter JE. Measurement error in psychological research: lessons from 26 research scenarios. Psychol Methods. 1996;1(2):199–223. [Google Scholar]
- 39.Roberts RE, Kaplan GA, Shema SJ, et al. Prevalence and correlates of depression in an aging cohort: the Alameda County Study. J Gerontol B Psychol Sci Soc Sci. 1997;52(5):S252–S258. doi: 10.1093/geronb/52b.5.s252. [DOI] [PubMed] [Google Scholar]
- 40.Qato DM, Alexander GC, Conti RM, et al. Use of prescription and over-the-counter medications and dietary supplements among older adults in the United States. JAMA. 2008;300(24):2867–2878. doi: 10.1001/jama.2008.892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.The prevention of falls in later life. A report of the Kellogg International Work Group on the prevention of falls by the elderly. Dan Med Bull. 1987;34(suppl 4):1–24. [PubMed] [Google Scholar]
- 42.Leipzig RM, Cumming RG, Tinetti ME. Drugs and falls in older people: a systematic review and meta-analysis: II. Cardiac and analgesic drugs. J Am Geriatr Soc. 1999;47(1):40–50. doi: 10.1111/j.1532-5415.1999.tb01899.x. [DOI] [PubMed] [Google Scholar]
- 43.Ganz DA, Bao Y, Shekelle PG, et al. Will my patient fall? JAMA. 2007;297(1):77–86. doi: 10.1001/jama.297.1.77. [DOI] [PubMed] [Google Scholar]
- 44.Stalenhoef PA, Diederiks JP, Knottnerus JA, et al. A risk model for the prediction of recurrent falls in community-dwelling elderly: a prospective cohort study. J Clin Epidemiol. 2002;55(11):1088–1094. doi: 10.1016/s0895-4356(02)00502-4. [DOI] [PubMed] [Google Scholar]
- 45.Lee Y. The predictive value of self assessed general, physical, and mental health on functional decline and mortality in older adults. J Epidemiol Community Health. 2000;54(2):123–129. doi: 10.1136/jech.54.2.123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Hays RD, Kallich JD, Mapes DL, et al. Kidney Disease Quality of Life Short Form (KDQOL-SF), Version 1.3: A Manual for Use and Scoring. Santa Monica, CA: RAND Corporation; 1997. [Google Scholar]
- 47.Lopes AA, Bragg J, Young E, et al. Depression as a predictor of mortality and hospitalization among hemodialysis patients in the United States and Europe. Kidney Int. 2002;62(1):199–207. doi: 10.1046/j.1523-1755.2002.00411.x. [DOI] [PubMed] [Google Scholar]
- 48.Ware J, Jr, Kosinski M, Keller SD. A 12-Item Short-Form Health Survey: construction of scales and preliminary tests of reliability and validity. Med Care. 1996;34(3):220–233. doi: 10.1097/00005650-199603000-00003. [DOI] [PubMed] [Google Scholar]
- 49.Idler EL, Russell LB, Davis D. Survival, functional limitations, and self-rated health in the NHANES I Epidemiologic Follow-up Study, 1992. First National Health and Nutrition Examination Survey. Am J Epidemiol. 2000;152(9):874–883. doi: 10.1093/aje/152.9.874. [DOI] [PubMed] [Google Scholar]
- 50.Andrews FM, Withey SB. Social Indicators of Well-Being: American’ s Perceptions of Life Quality. New York, NY: Plenum Press; 1976. [Google Scholar]
- 51.Diener E, Suh EM. National differences in subjective well-being. In: Kahneman D, Diener E, Schwartz N, editors. Well-Being: The Foundations of Hedonic Psychology. New York, NY: Russell-Sage; 1999. pp. 434–450. [Google Scholar]
- 52.Hughes ME, Waite LJ, Hawkley LC, et al. A short scale for measuring loneliness in large surveys: results from two population-based studies. Res Aging. 2004;26(6):655–672. doi: 10.1177/0164027504268574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Hawkley LC, Thisted RA, Masi CM, et al. Loneliness predicts increased blood pressure: 5-year cross-lagged analyses in middle-aged and older adults. Psychol Aging. 2010;25(1):132–141. doi: 10.1037/a0017805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Swearer JM, Drachman DA, Li L, et al. Screening for dementia in “real world” settings: the cognitive assessment screening test: CAST. Clin Neuropsychol. 2002;16(2):128–135. doi: 10.1076/clin.16.2.128.13235. [DOI] [PubMed] [Google Scholar]
- 55.Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. J Health Soc Behav. 1983;24(4):385–396. [PubMed] [Google Scholar]
- 56.Cohen S, Tyrrell DA, Smith AP. Psychological stress and susceptibility to the common cold. N Engl J Med. 1991;325(9):606–612. doi: 10.1056/NEJM199108293250903. [DOI] [PubMed] [Google Scholar]
- 57.Labbate LA, Fava M, Oleshansky M, et al. Physical fitness and perceived stress. Relationships with coronary artery disease risk factors. Psychosomatics. 1995;36(6):555–560. doi: 10.1016/s0033-3182(95)71611-5. [DOI] [PubMed] [Google Scholar]
- 58.Stewart AL. The reliability and validity of self-reported weight and height. J Chronic Dis. 1982;35(4):295–309. doi: 10.1016/0021-9681(82)90085-6. [DOI] [PubMed] [Google Scholar]
- 59.Haley SM, Jette AM, Coster WJ, et al. Late Life Function and Disability Instrument: II. Development and evaluation of the function component. J Gerontol A Biol Sci Med Sci. 2002;57(4):M217–M222. doi: 10.1093/gerona/57.4.m217. [DOI] [PubMed] [Google Scholar]