Abstract
Recent small-scale genomics analyses suggest that physiologic regulation of pro-inflammatory gene expression by endogenous glucocorticoids may be compromised in individuals who experience chronic social isolation. This could potentially contribute to the elevated prevalence of inflammation-related disease previously observed in social isolates. The present study assessed the relationship between leukocyte distributional sensitivity to glucocorticoid regulation and subjective social isolation in a large population-based sample of older adults. Initial analyses confirmed that circulating neutrophil percentages were elevated, and circulating lymphocyte and monocyte percentages were suppressed, in direct proportion to circulating cortisol levels. However, leukocyte distributional sensitivity to endogenous glucocorticoids was abrogated in individuals reporting either occasional or frequent experiences of subjective social isolation. This finding held in both nonparametric univariate analyses and in multivariate linear models controlling for a variety of biological, social, behavioral, and psychological confounders. The present results suggest that social factors may alter immune cell sensitivity to physiologic regulation by the hypothalamic-pituitary-adrenal axis in ways that could ultimately contribute to the increased physical health risks associated with social isolation.
Keywords: social isolation, loneliness, glucocorticoid resistance, hypothalamic-pituitary-adrenal axis, hematology, leukocyte homeostasis, social epidemiology, gerontology
INTRODUCTION
Social isolation is a risk factor for several adverse health outcomes including all-cause mortality (Berkman 1977; House, Landis et al. 1988; Seeman 1996; Berkman and Kawachi 2000; Cacioppo and Hawkley 2003), and specific infectious, neoplastic, and cardiovascular diseases (Reynolds and Kaplan 1990; Krongrad, Lai et al. 1996; Cohen, Doyle et al. 1997; Eng, Rimm et al. 2002; Cole, Kemeny et al. 2003; Soler-Villa, Kasl et al. 2003; Caspi, Harrington et al. 2006; Kroenke, Kubzansky et al. 2006). A recent functional genomics analysis suggests that alterations in immune system regulation by the hypothalamic-pituitary-adrenal (HPA) axis might contribute to these effects (Cole, Hawkley et al. 2007). Endogenous glucocorticoids from the HPA axis play a central role in physiologic control of inflammation by inhibiting the pro-inflammatory transcription factor NF-κB (Munck and Guyre 1986; Ruzek, Pearce et al. 1999; Rhen and Cidlowski 2005; Onard, Schoenveld et al. 2007; Pace, Hu et al. 2007). However, the HPA axis also mediates physiologic stress responses to a variety of other non-inflammatory challenges (e.g., psychological or social stressors) (Weiner 1992; Sapolsky 1994; Dickerson and Kemeny 2004), and those competing functional demands can potentially undermine the optimal control of inflammatory gene expression. Studies in animal models have shown that repeated social disruption can induce a state of glucocorticoid resistance in which the glucocorticoid receptor (GR) becomes less efficient in transducing endogenous glucocorticoid signals (Quan, Avitsur et al. 2003; Pace, Hu et al. 2007). This dynamic is believed to stem from GR phosphorylation by the p38 mitogen-activated protein kinase signaling pathway, which results in decreased receptor affinity for glucocorticoids (Wang, Wu et al. 2004), and subsequent reductions in physiologic control of pro-inflammatory gene expression (Stark, Avitsur et al. 2001; Avitsur, Kavelaars et al. 2005).
Studies of chronically stressed human beings have shown evidence of glucocorticoid resistance in ex vivo assays of leukocyte cytokine response to lipopolysaccharide (LPS) (Miller, Cohen et al. 2002; Miller, Rohleder et al. 2005). Based on those findings, we hypothesized that links between social isolation and inflammation-related disease might stem from underlying alterations in leukocyte sensitivity to regulation by endogenous glucocorticoids. A recent functional genomics analysis supported this hypothesis in showing decreased transcription of GR target genes (e.g., HIST1H2BG, STAT1, TNFRSF17, and TCN1) and increased transcription of NF-κB target genes (e.g., EGR3, FOSB, IL8, and PTGS2) in leukocytes from people reporting chronically high levels of subjective social isolation (loneliness) (Cole, Hawkley et al. 2007). However, it is not clear whether altered glucocorticoid regulation is a common correlate of subjective social isolation, or whether such effects occur only in individuals who show high levels of loneliness over long periods of time (e.g., consistently over 4 years in the extreme groups design employed for the genomics-based analysis) (Cole, Hawkley et al. 2007). It also remains unclear whether the effects previously observed in a small sample of older Americans from the Chicago metropolitan area might generalize to other socio-cultural contexts. To address these questions in the context of large-scale epidemiologic studies, it would be desirable to identify a less technically intensive measure of immune system glucocorticoid sensitivity that might be suitable for use in population-based epidemiologic studies or biosocial surveys (Weinstein, Vaupel et al. 2007).
One of the longest recognized effects of glucocorticoids involves the regulation of leukocyte subset composition within circulating blood (Fauci, Dale et al. 1976). High glucocorticoid levels simultaneously increase the circulating number of neutrophils (neutrophilia) and decrease the circulating number of lymphocytes (lymphopenia) and monocytes (monocytopenia) (Dale, Fauci et al. 1975; Fauci, Dale et al. 1976; Miller, Spencer et al. 1994; Dhabhar, Miller et al. 1996). These effects lag glucorticoid levels by 4–6 hrs (Dale, Fauci et al. 1975) and are driven in large part by altered trafficking of leukocyte subsets between blood and extravascular compartments (e.g., bone marrow) (Fauci and Dale 1975; Fauci, Dale et al. 1976). Because these effects are mediated specifically by activation of the GR (Miller, Spencer et al. 1994; Dhabhar, Miller et al. 1996), glucocorticoid regulation of the circulating neutrophil / lymphocyte ratio or neutrophil / monocyte ratio should provide an efficient biological readout for the GR functional activity in leukocytes. To the extent that leukocyte GRs show normal physiologic sensitivity to endogenous glucocorticoid levels, we would expect to observe the well-established positive correlation between cortisol levels and the neutrophil / lymphocyte ratio or the neutrophil / monoctye ratio. To the extent that leukocyte GRs are functionally desensitized, those positive correlations would be attenuated. Thus, the strength of association between endogenous glucocorticoid levels and circulating lymphocyte subset distributions may provide an efficient hematologic biomarker of leukocyte sensitivity to physiologic regulation by the HPA axis.
In the present study, we utilized this hematologic biomarker to quantify the relationship between subjective social isolation and immune system sensitivity to glucocorticoid regulation in data from SEBAS 2000 – a large population-based survey of older Taiwanese adults (Chang, Glei et al. 2007). This sample has previously been studied for relationships between psychosocial characteristics and hormone levels (Seeman, Glei et al. 2004; Goldman, Glei et al. 2005), but leukocyte sensitivity to hormonal regulation has not been examined. The present analyses sought to, 1.) determine whether loneliness-related impairments in leukocyte sensitivity to glucocorticoid regulation occur in a large population-based sample of older adults, and, 2.) identify the minimal extent of subjective social isolation required for the emergence of such effects.
METHODS
Study sample
Data come from the Social Environment and Biomarkers of Aging Study in Taiwan 2000 (SEBAS) (Seeman, Glei et al. 2004; Goldman, Glei et al. 2005; Chang, Glei et al. 2007). SEBAS is a multi-site study of 1,497 Taiwanese adults aged 54 and older drawn from a nationally representative sample and assessed for social, economic, psychological and health parameters through an in-home interview in the year 2000. 1,023 participants provided overnight urine specimens in the context of a hospital-based clinical examination. Institutionalized individuals (including hospitalized) and those with serious illness were excluded from this examination. Following initial publication of study results, de-identified data were archived for secondary analysis through the Inter-University Consortium for Political and Social Research (http://www.icpsr.umich.edu/, ICPSR 3792) (Chang, Glei et al. 2007; Weinstein and Goldman 2007). Data were collected under the supervision of Institutional Review Boards at Princeton University, the RAND Corporation, Georgetown University, the University of California at Los Angeles, and the Bureau of Health Promotion, Taiwan.
Biological parameters
12-hour overnight urine collections were collected at 7 AM and assayed for cortisol, epinephrine, and norepinephrine by Union Clinical Laboratories (Taipei, Taiwan) using high performance liquid chromatography with ultraviolet absorbance detection according to established protocols (Krstulovic 1982; Samaan, Porquet et al. 1993). Assay lower limits of detection were 2 pg/ml for catecholamines and 4 pg/ml for cortisol (Seeman, Glei et al. 2004). To control for individual differences in body size, urinary hormone values were normalized to creatinine concentrations as measured by alkaline picrate assay on a Beckman CX7 instrument (sensitivity = 10 mg/dl) (Goldman, Glei et al. 2005). White blood cell (WBC) counts, percent neutrophils, percent lymphocytes, and percent monocytes were determined in peripheral blood samples collected at 9 AM, maintained at room temperature, and assayed within 2 hrs by complete blood count with 5-part differential using a Coulter Gen-S automated hematology analyzer (Union Clinical Laboratories) according to the manufacturer protocol (Coulter, Fullerton CA) (Seeman, Glei et al. 2004; Goldman, Glei et al. 2005). 9 AM blood samples are functionally contemporaneous with cortisol levels assessed several hours earlier because hematological effects lag glucocorticoid fluctuations by 4–6 h (Dale, Fauci et al. 1975). Leukocyte sensitivity to glucocorticoid regulation was quantified by the strength of relationship between measured cortisol levels and measures of leukocyte subset distribution (log10-transformed neutrophil / lymphocyte ratios and neutrophil / monocyte ratios, and individual percentages of neutrophils, lymphocytes, and monocytes).
Psychological, social, behavioral, and health parameters
SEBAS measures of psychosocial, behavioral, and health parameters have previously been described (Seeman, Glei et al. 2004; Goldman, Glei et al. 2005; Chang, Glei et al. 2007; Weinstein and Goldman 2007). For the present analysis, subjective social isolation was assessed by SEBAS item B14-5, which asks respondents how often they felt lonely during the past week (not at all, rarely = 1 day during the past week, sometimes = 2–3 days during the past week, often = 4 or more days during the past week). This one-item indicator has been shown to be a valid measure of subjective social isolation in previous studies (Hughes, Waite et al. 2004). Objective social isolation was measured by SEBAS items A1 (not married), A3-A (lives alone), and B9-A–H (does not participate in a neighborhood, religious, political, social service, village/lineal, elderly club, or elderly education organization). Depressive symptoms were assessed by a 9-item variant of the Center for Epidemiologic Studies Depression scale (CESD) that has been validated for Taiwanese adults (Cheng and Chan 2005) and omits one item directly tapping social isolation. Socioeconomic status (SES) was measured as a composite of (z-transformed) measures of male/husband’s education (MANED00), perceived SES relative to other Taiwanese (D1), and low personal economic stress (C3-B). Physical health was represented as a composite of (z-transformed) subjective physical health (B1) and absence of medically significant chronic illness (including diabetes, cancer, renal disease, cardiovascular disease, respiratory disease, and cerebrovascular disease). Alcohol consumption and cigarette smoking were assessed by items ALC and SMK.
Statistical analyses
Relationships between hematologic parameters and hormone levels were analyzed using Spearman rank correlations estimated by SAS PROC CORR and general linear models fit using SAS PROC GLM (SAS Institute, Cary NC) (McCullagh and Nelder 1991). Linear models analyzed variation in the distribution of hematological parameters (log10-transformed neutrophil / lymphocyte and neutrophil / monocyte ratios, and individual percentages of neutrophils, lymphocytes, and monocytes) as a function of measured cortisol levels while controlling for any potential confounding between loneliness and other biological, social, psychological, behavioral, or health parameters. Glucocorticoid sensitivity was quantified by the linear model parameter relating leukocyte subset distributions to cortisol levels, and differences in the strength of that relationship for high- vs. low-lonely participants were quantified by a Cortisol × Loneliness interaction term (in a model including a main effect of Loneliness). Residual plots verified that results met the distributional assumptions of general linear models (Miller 1986). The lowest level of subjective social isolation at which altered leukocyte sensitivity to glucocorticoid regulation could be detected was identified using profile contrasts. Among the total 1,023 SEBAS participants, data on loneliness were missing for 20 individuals and hematologic measures were unavailable for 8, leaving a final analyzed sample size of 995. All available data were analyzed, and all reported p-values represent two-sided significance levels.
RESULTS
Table 1 presents demographic, behavioral, psychosocial, and endocrine characteristics of the SEBAS 2000 sample. As previously detailed (Seeman, Glei et al. 2004; Goldman, Glei et al. 2005; Chang, Glei et al. 2007), this sample represents a relatively healthy cohort of older, community-dwelling Taiwanese adults. Socioeconomic status varied widely, but was generally satisfactory to respondents. Rates of depressive symptoms were low, and endocrine and hematologic parameters fell within established reference ranges (Seeman, Glei et al. 2004; Weinstein and Goldman 2007).
TABLE 1.
SEBAS 2000 sample characteristics.
| Characteristic | Distribution |
|---|---|
| Age | 68.3 (8.5) years* |
| Sex | 57.7 % Male 42.3 % Female |
| SES | 73.8 % no economic stress 26.2 % economic stress 6.8 (4.5) years education* 9.2 % college or post-graduate 11.6 % high school 56.1 % primary school 15.3 % illiterate 7.8 % information unavailable |
| Physical health | 75.2 % no medical condition 24.8 % medical condition 96.5 % good health 3.5 % poor health |
| Loneliness (subjective social isolation) | 81.5 % none 7.1 % rare (1 day / wk) 6.9 % occasional (2–3 day / wk) 4.5 % frequent (≥ 4 day /wk) |
| Objective social isolation | 96.0 % integrated 4.0 % isolated |
| Depression (CESD10) | 7.9 ± 5.5 units (0–30 scale) * 20.7 % score depressed |
| Smoking | 76.4 % none 1.4 % occasionally with friends 0.2 % only after meals 22.0 % every day |
| Alcohol consumption | 77.0 % none 16.4 % sometimes 1.6 % frequently 5.1 % every day |
| Cortisol | 28.3 (51.9) µg / g creatinine* |
| Epinephrine | 21.9 (9.9) µg / g creatinine* |
| Norepinephrine | 2.6 (2.6) µg / g creatinine* |
| WBC count | 6,120 (1,597) cells / µL* |
| Leukocyte subset distributions | 32.6 (8.8) % Lymphocytes* 7.3 (2.0) % Monocytes* 56.7 (9.5) % Neutrophils* |
Mean (SD)
The vast majority of respondents reported no subjective sense of social isolation, with fewer than 10% reporting either rare loneliness (1 day per week), occasional loneliness (2–3 days per week), or frequent loneliness (4 or more days per week). Subjective social isolation was weakly correlated with objectively measured social isolation (Spearman rS = .106, p = .0008), age (rS = .134, p = .0001), and poor physical health (rS = .189, p < .0001), and more strongly correlated with low SES (rS = .228, p = .0001), and depressive symptoms (rS = .415, p < .0001). Females reported marginally higher rates of loneliness (biserial r = .061, p = .054). Each of these potential confounders was controlled for in subsequent multivariate analyses relating loneliness to glucorticoid sensitivity. Loneliness was not significantly correlated with any of the other risk factors listed in Table 1 (including smoking and alcohol consumption).
Cortisol regulation of leukocyte distribution
Table 2 reports results from multivariate analyses modeling circulating leukocyte subset distributions as a function of cortisol, epinephrine, and norepineprhine levels. Consistent with the established effects of glucocorticoids on leukocyte subset trafficking (Dale, Fauci et al. 1975; Fauci and Dale 1975; Fauci, Dale et al. 1976; Miller, Spencer et al. 1994), results show the expected positive relationship between cortisol levels and circulating neutrophil percentages, and the expected negative relationships between cortisol levels and the percentages of circulating lymphocytes and monocytes. The net effect was a highly significant positive correlation between cortisol levels and the neutrophil / lymphocyte ratio and the neutrophil / monocyte ratio. Those relationships were specific to cortisol, as no significant relationships emerged for norepinephrine or epinephrine levels. Thus, circulating leukocyte subset distributions provide a specific biomarker of immune cell regulation by endogenous glucocorticoids.
TABLE 2.
Neuroendocrine correlates of circulating leukocyte subset distributions.
| WBC count (103 cells / µL) |
Lymphocytes (% WBC) |
Monocytes (% WBC) |
Neutrophils (% WBC) |
Neut / Lym ratioa |
Neut / Mono ratioa |
|
|---|---|---|---|---|---|---|
| Cortisolb | 1.0 (0.9)c p = .3008 |
−16.1 (5.3) p = .0024 |
−2.9 (1.2) p = .0203 |
21.5 (5.7) p = .0002 |
0.42 (0.12) p = .0005 |
0.34 (0.09) p = .0004 |
| Epinephrineb | −30.7 (20.2) p = .1286 |
−59.0 (110.3) p = .5929 |
−31.3 (25.5) p = .2200 |
120.9 (119.4) p = .3111 |
1.45 (2.50) p = .5364 |
3.17 (2.00) p = .1122 |
| Norepinephrineb | 9.8 (5.4) p = .0697 |
−45.3 (29.4) p = .1238 |
0.9 (6.8) p = .8949 |
41.3 (31.8) p = .1943 |
1.13 (0.67) p = .0895 |
0.29 (0.53) p = .5913 |
Units = log10(ratio)
Units = g hormone / g creatinine
Partial regression coefficient point estimate (standard error) from multivariate analysis of each hematologic parameter as a function of cortisol, epinephrine, and norepinephrine levels
Effects of loneliness on glucocorticoid regulation of leukocyte distributions
To determine whether subjective social isolation was associated with reduced leukocyte sensitivity to glucocorticoid regulation, we carried out two types of analyses assessing the sensitivity of circulating leukocyte subset distributions to cortisol levels in lonely vs. non-lonely individuals. Initial non-parametric analyses stratified data from lonely vs. non-lonely individuals and quantified the association between cortisol level and leukocyte distributional parameters within each stratum (Table 3). Results from the 812 non-lonely individuals showed the generally observed positive relationship between cortisol levels and circulating neutrophil / lymphocyte ratios and neutrophil / monocyte ratios. However, consistent with the hypothesis of reduced leukocyte sensitivity to glucocorticoid regulation, data from the 183 lonely individuals showed no statistically significant relationship between cortisol and either hematologic ratio. The difference in the magnitude of sensitivity correlations was statistically significant for both neutrophil / lymphocyte ratios (p = .0359 by z-test for independent correlations) and neutrophil / monocyte ratios (p = .0370). Similar effects emerged in analyses distinguishing those who reported the highest level of loneliness (frequent) from others. High-lonely individuals showed non-significant correlations between leukocyte distributional parameters and cortisol levels (all p > .25), whereas leukocyte subset distributions showed highly significant correlations with cortisol levels in the remainder of the sample (all p < .0001). The use of rank-based non-parametric measures ensures that these results are robust to assumptions regarding statistical distribution (Miller 1986).
TABLE 3.
Loneliness-related differences in hematologic biomarkers of glucocorticoid sensitivity: Non-parametric univariate analyses.
| WBC count (103 cells / µL) |
Lymphocytes (% WBC) |
Monocytes (% WBC) |
Neutrophils (% WBC) |
Neut / Lym ratio |
Neut / Mono ratio |
|
|---|---|---|---|---|---|---|
| Non-lonely |
r = −.069a p = .0509b |
r = −.136 p = .0001 |
r = −.195 p < .0001 |
r = .196 p < .0001 |
r = .159 p < .0001 |
r = .236 p < .0001 |
| Lonely |
r = −.101 p = .1740 |
r = −.002 p = .9733 |
r = −.103 p = .1645 |
r = .025 p = .7380 |
r = .012 p = .8675 |
r = .093 p = .2098 |
r = Spearman rank correlation between cortisol concentration (g / g creatinine) and the indicated hematologic parameter
p = 2-tailed significance level
Biological, social, behavioral, and psychological confounders
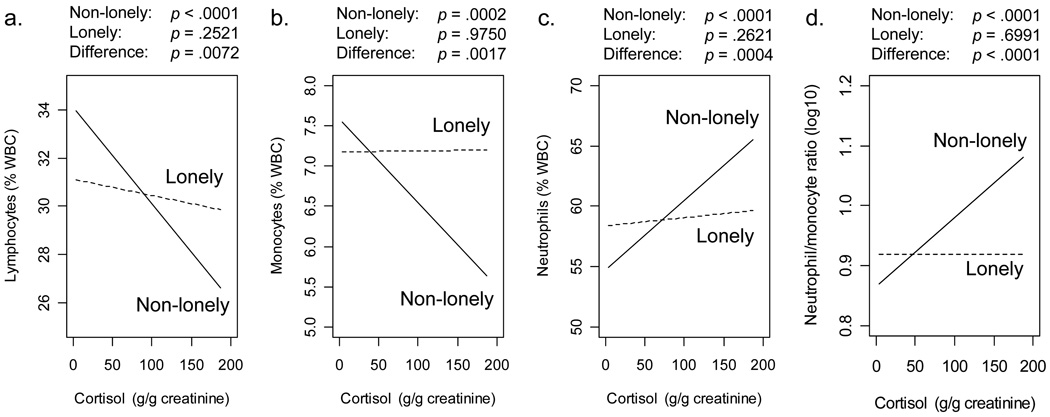
To ensure that the differential linkage of cortisol to circulating leukocyte subset distributions in lonely vs. non-lonely individuals did not stem from confounded differences in other biological, social, behavioral, or psychological characteristics, a second set of analyses used general linear models to quantify relationships between cortisol and leukocyte distributions while controlling for body mass index (BMI), Age, Sex, Age × Sex interaction (to accommodate sex differences in age trends observed for some hematologic parameters), objective social isolation, depression, SES, smoking, alcohol consumption, and physical health. As shown in Figure 1, Cortisol × Loneliness interaction terms remained statistically significant. To confirm that effects of subjective loneliness were not attributable to the objective absence of social contact, glucocorticoid sensitivity analyses were repeated substituting measures of objective social isolation for loneliness. None of the leukocyte distributional parameters showed a significant Cortisol × Isolation interaction (all p > .2126).
FIGURE 1. Sensitivity of circulating leukocyte subset distributions to cortisol level.
Regression lines indicate the variation in hematologic paramters as a function of cortisol level in 812 non-lonely participants (solid line) and 183 lonely participants (dashed line) for (a.) percent lymphocytes, (b.) percent monocytes, (c.) percent neutrophils, and (d.) neutrophil / monocyte ratios. p-values give statistical significance of the slope of regression lines for non-lonely individuals, lonely individuals, and the difference between groups (Cortisol × Loneliness interaction) in analyses controlling for BMI, Age, Sex, Age × Sex interaction, smoking, alcohol consumption, SES, physical health status, depression, and objective social isolation.
Threshold of regulatory alterations
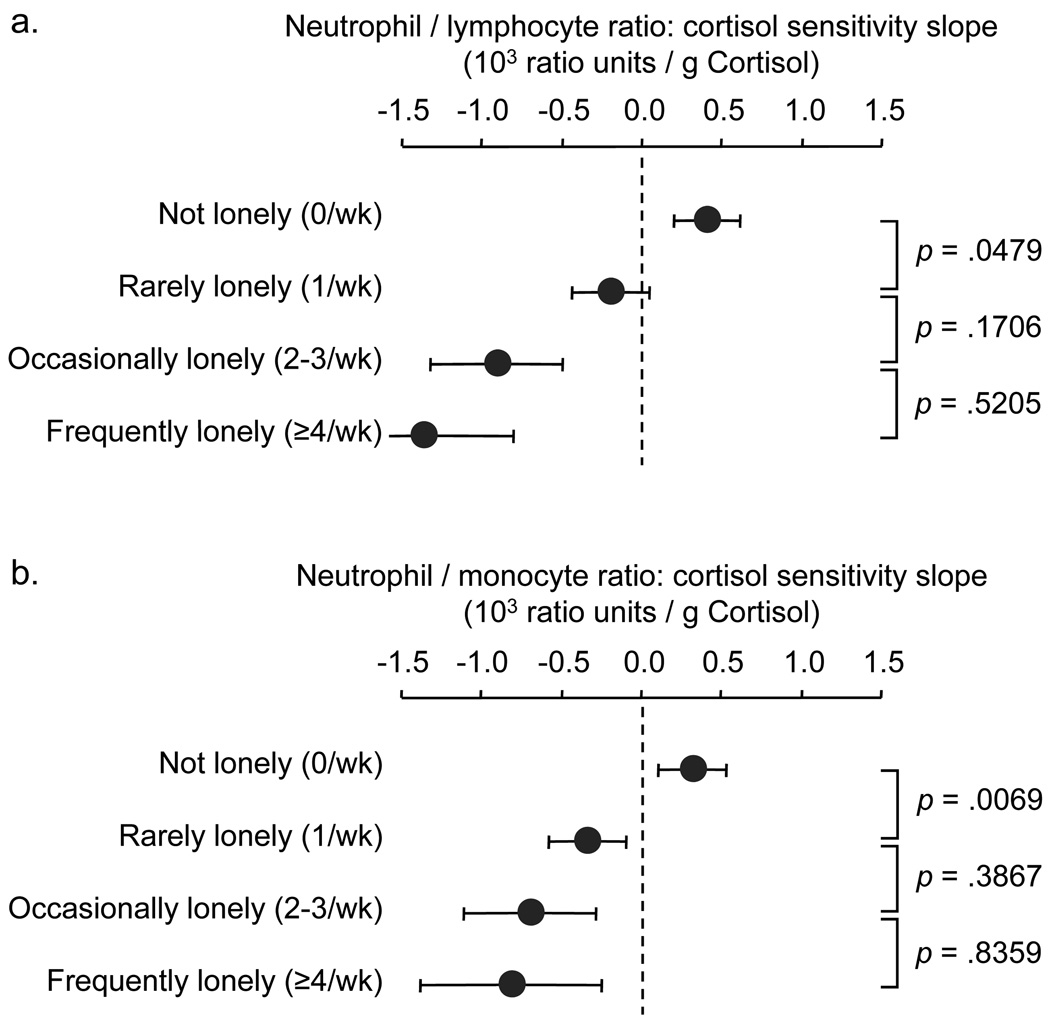
To identify the threshold level of loneliness at which alterations in leukocyte sensitivity to glucocorticoid regulation become detectable, a set of profile contrasts compared cortisol sensitivity parameters for respondents who reported not being lonely at all vs. rarely lonely (1 day / week), rarely vs. occasionally lonely (2–3 days / week), and occasionally lonely vs. frequently lonely (≥4 days / week). As shown in Figure 2, this analysis showed a mildly decelerating dose-response relationship between frequency of subjective isolation and reduced leukocyte distributional sensitivity to cortisol. A statistically significant decrement occurred between “not lonely” and “rarely lonely” for both neutrophil / lymphocyte ratios and neutrophil / monocyte ratios. No other pair-wise profile contrast was statistically significant in either analysis. Thus, even minimal levels of subjective social isolation are associated with alterations in leukocyte sensitivity to glucocorticoid regulation.
FIGURE 2. Relationship between subjective social isolation and magnitude of leukocyte distributional sensitivity to cortisol level.
Data represent mean ± standard error of sensitivity coefficients relating variation in cortisol concentration to (a.) neutrophil / lymphocyte ratios, and (b.) neutrophil / monocyte ratios at varying levels of loneliness. p-values denote statistical significance of profile contrasts comparing adjacent sensitivity coefficients.
DISCUSSION
The present study used a novel cell trafficking-based measure to assess the relationship between subjective social isolation and leukocyte sensitivity to glucocorticoid regulation. Motivated by previous functional genomics studies indicating altered glucocorticoid regulation of genome-wide transcriptional profiles in a small sample of lonely older Americans (Cole, Hawkley et al. 2007), this analysis sought to verify those findings in a larger population-based study of older Taiwanese adults showing a broad range of loneliness levels. Initial biomarker analyses found the ratio of circulating neutrophils / monocytes and neutrophils / lymphocytes to be particularly sensitive to physiologic variation in the endogenous glucocorticoid, cortisol. Substantive analyses found reduced leukocyte distributional sensitivity to cortisol in people who experienced frequent loneliness, with significant effects detectable even among people who report feeling lonely as little as one day per week. These effects were specific to the experience of subjective social isolation, and could not be attributed to any correlated differences in physical health, SES, depression, smoking, alcohol consumption, or objective social isolation. Thus, the present findings are consistent with previous observations (Cole, Hawkley et al. 2007) in suggesting that subjective social isolation represents an independent social risk factor for alterations in leukocyte sensitivity to glucocorticoid regulation.
The present findings are consistent with data from experimental animal models indicating that social stress can influence immune cell sensitivity to glucocorticoid regulation (Stark, Avitsur et al. 2001; Bailey, Avitsur et al. 2004; Engler, Bailey et al. 2004), and with data from human clinical studies linking social risk factors to ex vivo measures of leukocyte glucocorticoid resistance (Miller, Cohen et al. 2002; Miller, Rohleder et al. 2005). However, it is unclear how closely the present study’s in vivo cell trafficking-based biomarker of glucocorticoid regulatory sensitivity corresponds to the benchmark measure of “glucocorticoid resistance” based on pharmacologic inhibition of LPS-induced cytokine production ex vivo. No data are currently available to directly correlate these two approaches, and each is likely to reflect some unique features in addition to whatever variance they share due to the common role of GR signaling in regulating their expression. For example, circulating leukocyte subset distributions may be affected by several other factors in addition to endogenous cortisol levels, including inflammation (subset-specific chemotaxis) (Mackay 1993), hematopoiesis (differential production of leukocyte subsets) (Fey 2007), and autonomic nervous system activity (catecholamine modulation of subset trafficking) (Ottaway and Husband 1994; Carlson 2001). Likewise, ex vivo cytokine production assays are sensitive to variations in LPS signal-transduction pathways and the presence of plasma glucocorticoids in cell cultures (Arbour, Lorenz et al. 2000; Bhattacharyya, Brown et al. 2007; Bower, Ganz et al. 2007; Jaekal, Abraham et al. 2007; MacRedmond, Greene et al. 2007). Despite these differences, leukocyte distribution and cytokine inhibition measures of glucocorticoid regulatory sensitivity are likely to covary substantially because both depend centrally on the ability of the GR to transduce glucocorticoid signals into functional alterations in leukocyte biology (Miller, Spencer et al. 1994). Direct comparison of these two approaches is an important target for future research.
The utility of hematologic biomarkers of glucocorticoid sensitivity might be substantially improved by intra-individual assessments over time (e.g., repeated measurements of cortisol and leukocyte subset distributions over their diurnal cycle (Winkel, Statland et al. 1981)). That would hold constant other hematologic influences that likely added substantial noise to the present cross-sectional analysis (and likely explain why relationships between cortisol levels and hematologic parameters rarely exceeded r = .20 in magnitude). The present cross-sectional measures can only identify group-level factors that influence glucocorticoid sensitivity (e.g., degree of loneliness) and cannot support individual-specific inferences about biologic function or physical health. The present data do suggest that neutrophil / monocyte ratios constitute the most sensitive hematologic biomarker of glucocorticoid sensitivity, as that parameter showed the strongest quantitative relationship to endogenous cortisol levels. The biological basis for that advantage remains to be defined, but neutrophil / monocyte ratios may control for hematopoietic variation more effectively than other distributional summaries because neutrophils and monocytes differentiate from a common myeloid progenitor cell (Friedman 2002) that is subject to regulation by glucocorticoids (Motomura, Katsuno et al. 1983; Suda, Miura et al. 1983; Rinehart, Keville et al. 1997). The neutrophil / monocyte ratio is also comparatively insensitive to potential biological confounders such as BMI, whereas neutrophil / lymphocyte ratios were significantly correlated with BMI (data not shown). Despite these complexities, hematologic assessment of glucocorticoid sensitivity provides substantial cost and feasibility advantages over previous measures such as ex vivo cytokine stimulation assays (Stark, Avitsur et al. 2001; Miller, Cohen et al. 2002; Bailey, Avitsur et al. 2004; Miller, Rohleder et al. 2005; Pace, Hu et al. 2007) and bioinformatic analysis of genome-wide transcriptional profiles (Cole, Hawkley et al. 2007).
Several additional limitations need to be considered when interpreting the substantive results of this study. First, these data come from a correlational analysis that cannot decisively establish causal direction. Previous experimental studies show that glucocorticoid manipulation can influence circulating leukocyte distributions (Dale, Fauci et al. 1975; Fauci and Dale 1975; Fauci, Dale et al. 1976; Miller, Spencer et al. 1994; Dhabhar, Miller et al. 1996). Moreover, correlations between endogenous glucocorticoid levels and hematologic parameters cannot be attributed to a reverse causal effect because experimental alteration of leukocyte subset distributions does not affect circulating cortisol levels (Rovelli, Barni et al. 1995; Schuld, Mullington et al. 1999). Thus, circulating leukocyte subset distributions represent a causally valid biomarker of leukocyte sensitivity to glucocorticoid signaling. However, the relationship between glucocorticoid sensitivity and social risk factors requires careful interpretation. The present study was motivated by the hypothesis that subjective social isolation influences immune system sensitivity to regulation by endogenous GCs (Cole, Hawkley et al. 2007), but a reverse causal influence is conceivable in the possibility that altered glucocorticoid regulation of inflammation might affect social perception or behavior (e.g., via cytokine effects on the brain (Dantzer, O'Connor et al. 2008)). It is also possible that the observed correlation between reduced glucocorticoid sensitivity and social isolation is a spurious consequence of those variables’ common relationship to a third causal variable. The present study ruled out some of the most plausible potential confounders, including demographic characteristics, SES, physical health status, smoking, alcohol consumption, depression, and objective social isolation. Nonetheless, it is conceivable that other determinants which remain unmeasured in this study could potentially affect both neuroendocrine-immune dynamics and experienced social isolation. Another limitation of this study involves its analysis of subjective social isolation based on a single assessment of a one-item measure. Although that measure has been shown to correlate well with multi-item loneliness scales in previous studies (Hughes, Waite et al. 2004), future research would benefit from more extensive assessment of subjective social isolation across multiple occasions.
The present findings are consistent with the general theory that social factors can modulate immune system sensitivity to regulation by the nervous system (Amdam, Aase et al. 2005; Cole 2005; Cole, Hawkley et al. 2007; Sloan, Capitanio et al. 2007; Sloan, Capitanio et al. 2008). The implications of such effects for immunologic effector functions or disease pathophysiology remain unclear because SEBAS lacks direct measures of those processes. However, the pattern of decreasing leukocyte functional sensitivity to HPA regulation with increasing levels of subjective social isolation is consistent with the profile of increased inflammatory disease risk observed in human epidemiologic studies (Berkman 1977; House, Landis et al. 1988; Reynolds and Kaplan 1990; Krongrad, Lai et al. 1996; Seeman 1996; Cohen, Doyle et al. 1997; Berkman and Kawachi 2000; Cacioppo and Hawkley 2003; Cole, Kemeny et al. 2003; Soler-Villa, Kasl et al. 2003; Caspi, Harrington et al. 2006; Kroenke, Kubzansky et al. 2006) and in animal models (Sklar and Anisman 1980; Ben-Nathan, Lustig et al. 1989; Shively, Clarkson et al. 1989; Clausing, Bocker et al. 1994; Hilakivi-Clarke and Dickson 1995; Villano Bonamin, Barbuto et al. 2001; Wu, Murata et al. 2001; McClintock, Conzen et al. 2005; Hermes, Rosenthal et al. 2006; Thaker, Han et al. 2006). A significant challenge for future research lies in understanding the teleologic basis for these relationships. Why has evolution selected for the development of an immune system that escapes its chief counter-regulatory influence when individuals are bereft of close social ties? The fact that the HPA axis has evolved to serve as both a primary regulator of endogenous inflammation (Munck and Guyre 1986; Ruzek, Pearce et al. 1999; Rhen and Cidlowski 2005; Onard, Schoenveld et al. 2007) and a primary regulator of physiologic responses to social threat (Dickerson and Kemeny 2004) implies that there may be a significant selective benefit from the dynamic alteration of immune biology in response to changing social conditions (e.g., as noted for development of the nervous and endocrine systems (Hofer 1984; Panksepp 1998; Zhang, Bagot et al. 2006)). Defining the nature of individual physiologic threats and resources that are conferred by the close presence of conspecifics (e.g., as analyzed in (Cole 2005)) could help unravel the evolutionary basis for the epidemiologic relationship between social factors and physical health (Berkman 1977; House, Landis et al. 1988; Seeman 1996; Berkman and Kawachi 2000).
ACKNOWLEDGEMENTS
SEBAS data collection was supported by the National Institute on Aging (AG16790, AG16661) and the Taiwan National Health Research Institute (DD01-86IX-GR601S). The present analyses were supported by the United States National Cancer Institute (CA116778) and the James B. Pendelton Charitable Trust. Thanks to Dr. Noreen Goldman and Dr. Maxine Weinstein for heading SEBAS data collection and promoting its use as a public scientific resource, to Dr. Teresa Seeman and Dr. Lis Neilson for facilitating biosocial survey research at the 2007 National Institute on Aging Workshop on Allostaic Load, and to the Interuniversity Consortium for Political and Social Research at the University of Michigan for data distribution.
REFERENCES
- Amdam GV, Aase AL, et al. Social reversal of immunosenescence in honey bee workers. Exp Gerontol. 2005;40(12):939–947. doi: 10.1016/j.exger.2005.08.004. Epub 2005 Oct 5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arbour NC, Lorenz E, et al. TLR4 mutations are associated with endotoxin hyporesponsiveness in humans. Nat Genet. 2000;25(2):187–191. doi: 10.1038/76048. [DOI] [PubMed] [Google Scholar]
- Avitsur R, Kavelaars A, et al. Social stress and the regulation of tumor necrosis factor-alpha secretion. Brain Behav Immun. 2005;19(4):311–317. doi: 10.1016/j.bbi.2004.09.005. Epub 2004 Nov 21. [DOI] [PubMed] [Google Scholar]
- Bailey MT, Avitsur R, et al. Physical defeat reduces the sensitivity of murine splenocytes to the suppressive effects of corticosterone. Brain Behav Immun. 2004;18(5):416–424. doi: 10.1016/j.bbi.2003.09.012. [DOI] [PubMed] [Google Scholar]
- Ben-Nathan D, Lustig S, et al. The influence of cold or isolation stress on neuroinvasiveness and virulence of an attenuated variant of West Nile virus. Arch Virol. 1989;109(1–2):1–10. doi: 10.1007/BF01310513. [DOI] [PubMed] [Google Scholar]
- Berkman LF. Social Networks, Host Resistance and Mortality: A Follow-Up Study of Alameda County Residents. Berkeley: University of California; 1977. [DOI] [PubMed] [Google Scholar]
- Berkman LF, Kawachi I. Social Epidemiology. New York: Oxford University Press; 2000. [Google Scholar]
- Bhattacharyya S, Brown DE, et al. Macrophage glucocorticoid receptors regulate Toll-like receptor 4-mediated inflammatory responses by selective inhibition of p38 MAP kinase. Blood. 2007;109(10):4313–4319. doi: 10.1182/blood-2006-10-048215. Epub 2007 Jan 25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bower JE, Ganz PA, et al. Inflammatory responses to psychological stress in fatigued breast cancer survivors: relationship to glucocorticoids. Brain Behav Immun. 2007;21(3):251–258. doi: 10.1016/j.bbi.2006.08.001. Epub 2006 Sep 27. [DOI] [PubMed] [Google Scholar]
- Cacioppo JT, Hawkley LC. Social isolation and health, with an emphasis on underlying mechanisms. Perspect Biol Med. 2003;46(3 Suppl):S39–S52. [PubMed] [Google Scholar]
- Carlson SL. Neural influences on cell adhesion molecules and lymphocyte trafficking. In: Ader R, Felten DL, Cohen N, editors. Psychoneuroimmunology. Vol. 1. San Diego: Academic Press; 2001. pp. 231–240. [Google Scholar]
- Caspi A, Harrington H, et al. Socially isolated children 20 years later: risk of cardiovascular disease. Arch Pediatr Adolesc Med. 2006;160(8):805–811. doi: 10.1001/archpedi.160.8.805. [DOI] [PubMed] [Google Scholar]
- Chang M-C, Glei D, et al. The Taiwan biomarker project. In: Weinstein M, Vaupel JW, Wachter KW, editors. Biosocial surveys. Washington D. C.: The National Academies Press; 2007. [PubMed] [Google Scholar]
- Cheng ST, Chan AC. The Center for Epidemiologic Studies Depression Scale in older Chinese: thresholds for long and short forms. Int J Geriatr Psychiatry. 2005;20(5):465–470. doi: 10.1002/gps.1314. [DOI] [PubMed] [Google Scholar]
- Clausing P, Bocker T, et al. Social isolation modifies the response of mice to experimental Mengo virus infection. J Exp Anim Sci. 1994;36(2–3):37–54. [PubMed] [Google Scholar]
- Cohen S, Doyle WJ, et al. Social ties and susceptibility to the common cold. Journal of the American Medical Association. 1997;227:1940–1944. [PubMed] [Google Scholar]
- Cole SW. The complexity of dynamic host networks. In: Deisboeck TS, Kresh JY, editors. Complex Systems Science in BioMedicine. New York: Kluwer Academic - Plenum Publishers; 2005. pp. 605–629. [Google Scholar]
- Cole SW, Hawkley LC, et al. Social regulation of gene expression in human leukocytes. Genome Biology. 2007;8(9):R189. doi: 10.1186/gb-2007-8-9-r189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cole SW, Kemeny ME, et al. Psychological risk factors for HIV pathogenesis: Mediation by the autonomic nervous system. Biological Psychiatry. 2003;54:1444–1456. doi: 10.1016/s0006-3223(02)01888-7. [DOI] [PubMed] [Google Scholar]
- Dale DC, Fauci AS, et al. Comparison of agents producing a neutrophilic leukocytosis in man. Hydrocortisone, prednisone, endotoxin, and etiocholanolone. J Clin Invest. 1975;56(4):808–813. doi: 10.1172/JCI108159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dantzer R, O'Connor JC, et al. From inflammation to sickness and depression: when the immune system subjugates the brain. Nat Rev Neurosci. 2008;9(1):46–56. doi: 10.1038/nrn2297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dhabhar FS, Miller AH, et al. Stress-induced changes in blood leukocyte distribution. Role of adrenal steroid hormones. J Immunol. 1996;157(4):1638–1644. [PubMed] [Google Scholar]
- Dickerson SS, Kemeny ME. Acute stressors and cortisol responses: a theoretical integration and synthesis of laboratory research. Psychol Bull. 2004;130(3):355–391. doi: 10.1037/0033-2909.130.3.355. [DOI] [PubMed] [Google Scholar]
- Eng PM, Rimm EB, et al. Social ties and change in social ties in relation to subsequent total and cause-specific mortality and coronary heart disease incidence in men. Am J Epidemiol. 2002;155(8):700–709. doi: 10.1093/aje/155.8.700. [DOI] [PubMed] [Google Scholar]
- Engler H, Bailey MT, et al. Effects of repeated social stress on leukocyte distribution in bone marrow, peripheral blood and spleen. J Neuroimmunol. 2004;148(1–2):106–115. doi: 10.1016/j.jneuroim.2003.11.011. [DOI] [PubMed] [Google Scholar]
- Fauci AS, Dale DC. The effect of Hydrocortisone on the kinetics of normal human lymphocytes. Blood. 1975;46(2):235–243. [PubMed] [Google Scholar]
- Fauci AS, Dale DC, et al. Glucocorticosteroid therapy: mechanisms of action and clinical considerations. Ann Intern Med. 1976;84(3):304–315. doi: 10.7326/0003-4819-84-3-304. [DOI] [PubMed] [Google Scholar]
- Fey MF. Normal and malignant hematopoiesis. Ann Oncol. 2007;18 Suppl 1:i9–i13. doi: 10.1093/annonc/mdl444. [DOI] [PubMed] [Google Scholar]
- Friedman AD. Transcriptional regulation of granulocyte and monocyte development. Oncogene. 2002;21(21):3377–3390. doi: 10.1038/sj.onc.1205324. [DOI] [PubMed] [Google Scholar]
- Goldman N, Glei DA, et al. Perceived stress and physiological dysregulation in older adults. Stress. 2005;8(2):95–105. doi: 10.1080/10253890500141905. [DOI] [PubMed] [Google Scholar]
- Hermes GL, Rosenthal L, et al. Social isolation and the inflammatory response: sex differences in the enduring effects of a prior stressor. Am J Physiol Regul Integr Comp Physiol. 2006;290(2):R273–R282. doi: 10.1152/ajpregu.00368.2005. Epub 2005 Oct 6. [DOI] [PubMed] [Google Scholar]
- Hilakivi-Clarke L, Dickson RB. Stress influence on development of hepatocellular tumors in transgenic mice overexpressing TGF alpha. Acta Oncol. 1995;34(7):907–912. doi: 10.3109/02841869509127203. [DOI] [PubMed] [Google Scholar]
- Hofer MA. Relationships as regulators: a psychobiologic perspective on bereavement. Psychosom Med. 1984;46(3):183–197. doi: 10.1097/00006842-198405000-00001. [DOI] [PubMed] [Google Scholar]
- House JS, Landis KR, et al. Social relationships and health. Science. 1988;241:540–545. doi: 10.1126/science.3399889. [DOI] [PubMed] [Google Scholar]
- Hughes ME, Waite LJ, et al. A short scale for measuring loneliness in large surveys: Results from two population-based studies. Research on Aging. 2004;26(6):655–672. doi: 10.1177/0164027504268574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jaekal J, Abraham E, et al. Individual LPS responsiveness depends on the variation of toll-like receptor (TLR) expression level. J Microbiol Biotechnol. 2007;17(11):1862–1867. [PubMed] [Google Scholar]
- Kroenke CH, Kubzansky LD, et al. Social networks, social support, and survival after breast cancer diagnosis. J Clin Oncol. 2006;24(7):1105–1111. doi: 10.1200/JCO.2005.04.2846. [DOI] [PubMed] [Google Scholar]
- Krongrad A, Lai H, et al. Marriage and mortality in prostate cancer. J Urol. 1996;156(5):1696–1670. [PubMed] [Google Scholar]
- Krstulovic AM. Investigations of catecholamine metabolism using high-performance liquid chromatography: analytical methodology and clinical applications. J Chromatogr. 1982;229(1):1–34. doi: 10.1016/s0378-4347(00)86033-8. [DOI] [PubMed] [Google Scholar]
- Mackay CR. Homing of naive, memory and effector lymphocytes. Curr Opin Immunol. 1993;5(3):423–427. doi: 10.1016/0952-7915(93)90063-x. [DOI] [PubMed] [Google Scholar]
- MacRedmond RE, Greene CM, et al. Epithelial expression of TLR4 is modulated in COPD and by steroids, salmeterol and cigarette smoke. Respir Res. 2007;8:84. doi: 10.1186/1465-9921-8-84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McClintock MK, Conzen SD, et al. Mammary cancer and social interactions: identifying multiple environments that regulate gene expression throughout the life span. J Gerontol B Psychol Sci Soc Sci. 2005;60(Spec No 1):32–41. doi: 10.1093/geronb/60.special_issue_1.32. [DOI] [PubMed] [Google Scholar]
- McCullagh P, Nelder JA. Generalized Linear Models. London: Chapman & Hall; 1991. [Google Scholar]
- Miller AH, Spencer RL, et al. Effects of selective type I and II adrenal steroid agonists on immune cell distribution. Endocrinology. 1994;135(5):1934–1944. doi: 10.1210/endo.135.5.7956914. [DOI] [PubMed] [Google Scholar]
- Miller GE, Cohen S, et al. Chronic psychological stress and the regulation of pro-inflammatory cytokines: a glucocorticoid-resistance model. Health Psychol. 2002;21(6):531–541. doi: 10.1037//0278-6133.21.6.531. [DOI] [PubMed] [Google Scholar]
- Miller GE, Rohleder N, et al. Clinical depression and regulation of the inflammatory response during acute stress. Psychosom Med. 2005;67(5):679–687. doi: 10.1097/01.psy.0000174172.82428.ce. [DOI] [PubMed] [Google Scholar]
- Miller RG. Beyond ANOVA: Basics of applied statistics. New York: Wiley; 1986. [Google Scholar]
- Motomura S, Katsuno M, et al. The effect of hydrocortisone on the production and differentiation of granulocyte/macrophage progenitor cells in long-term bone marrow cultures. Exp Hematol. 1983;11(1):56–62. [PubMed] [Google Scholar]
- Munck A, Guyre PM. Glucocorticoid physiology, pharmacology and stress. Advances in Expermental Medicine and Biology. 1986;196:81–96. doi: 10.1007/978-1-4684-5101-6_6. [DOI] [PubMed] [Google Scholar]
- Onard JL, Schoenveld M, et al. Glucocorticoids and Immunity: Mechanisms of Regulation. In: Ader R, editor. Psychoneuroimmunology, Fourth Edition. Vol. 1. Burlington, MA: Elsevier Academic Press; 2007. pp. 45–62. [Google Scholar]
- Ottaway CA, Husband AJ. The influence of neuroendocrine pathways on lymphocyte migration. Immunology Today. 1994;15:511. doi: 10.1016/0167-5699(94)90206-2. [DOI] [PubMed] [Google Scholar]
- Pace TW, Hu F, et al. Cytokine-effects on glucocorticoid receptor function: Relevance to glucocorticoid resistance and the pathophysiology and treatment of major depression. Brain Behav Immun. 2007;21(1):9–19. doi: 10.1016/j.bbi.2006.08.009. Epub 2006 Oct 27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Panksepp J. Affective neuroscience: The foundations of human and animal emotions. New York: Oxford University Press; 1998. [Google Scholar]
- Quan N, Avitsur R, et al. Molecular mechanisms of glucocorticoid resistance in splenocytes of socially stressed male mice. J Neuroimmunol. 2003;137(1–2):51–58. doi: 10.1016/s0165-5728(03)00042-0. [DOI] [PubMed] [Google Scholar]
- Reynolds P, Kaplan GA. Social connections and risk for cancer: prospective evidence from the Alameda County Study. Behav Med. 1990;16(3):101–110. doi: 10.1080/08964289.1990.9934597. [DOI] [PubMed] [Google Scholar]
- Rhen T, Cidlowski JA. Antiinflammatory action of glucocorticoids--new mechanisms for old drugs. N Engl J Med. 2005;353(16):1711–1723. doi: 10.1056/NEJMra050541. [DOI] [PubMed] [Google Scholar]
- Rinehart J, Keville L, et al. Corticosteroids alter hematopoiesis in vitro by enhancing human monocyte secretion of granulocyte colony-stimulating factor. Exp Hematol. 1997;25(5):405–412. [PubMed] [Google Scholar]
- Rovelli F, Barni S, et al. Endocrine effects of granulocyte colony-stimulating factor in cancer patients. Tumori. 1995;81(6):438–439. doi: 10.1177/030089169508100611. [DOI] [PubMed] [Google Scholar]
- Ruzek MC, Pearce BD, et al. Endogenous glucocorticoids protect against cytokine-mediated lethality during viral infection. J Immunol. 1999;162(6):3527–3533. [PubMed] [Google Scholar]
- Samaan GJ, Porquet D, et al. Determination of cortisol and associated glucocorticoids in serum and urine by an automated liquid chromatographic assay. Clin Biochem. 1993;26(3):153–158. doi: 10.1016/0009-9120(93)90019-3. [DOI] [PubMed] [Google Scholar]
- Sapolsky RM. Why zebras don't get ulcers: A guide to stress, stress-related diseases, and coping. New York: Freeman; 1994. [Google Scholar]
- Schuld A, Mullington J, et al. Effects of granulocyte colony-stimulating factor on night sleep in humans. Am J Physiol. 1999;276(4 Pt 2):R1149–R1155. doi: 10.1152/ajpregu.1999.276.4.R1149. [DOI] [PubMed] [Google Scholar]
- Seeman T, Glei D, et al. Social relationships and allostatic load in Taiwanese elderly and near elderly. Soc Sci Med. 2004;59(11):2245–2257. doi: 10.1016/j.socscimed.2004.03.027. [DOI] [PubMed] [Google Scholar]
- Seeman TE. Social ties and health: the benefits of social integration. Ann Epidemiol. 1996;6(5):442–451. doi: 10.1016/s1047-2797(96)00095-6. [DOI] [PubMed] [Google Scholar]
- Shively CA, Clarkson TB, et al. Social deprivation and coronary artery atherosclerosis in female cynomolgus monkeys. Atherosclerosis. 1989;77(1):69–76. doi: 10.1016/0021-9150(89)90011-7. [DOI] [PubMed] [Google Scholar]
- Sklar LS, Anisman H. Social stress influences tumor growth. Psychosom Med. 1980;42(3):347–365. doi: 10.1097/00006842-198005000-00005. [DOI] [PubMed] [Google Scholar]
- Sloan EK, Capitanio JP, et al. Stress-induced remodeling of lymphoid innervation. Brain Behav Immun. 2008;22(1):15–21. doi: 10.1016/j.bbi.2007.06.011. Epub 2007 Aug 13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sloan EK, Capitanio JP, et al. Social stress enhances sympathetic innervation of primate lymph nodes: mechanisms and implications for viral pathogenesis. J Neurosci. 2007;27(33):8857–8865. doi: 10.1523/JNEUROSCI.1247-07.2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Soler-Villa H, Kasl SV, et al. Prognostic significance of psychosocial factors in African-American and White breast cancer patients. Cancer. 2003;98(6):1299–1308. doi: 10.1002/cncr.11670. [DOI] [PubMed] [Google Scholar]
- Stark J, Avitsur R, et al. Social stress induces glucocorticoid resistance in macrophages. American J. Physiol. Reg. Int. Comp Physiol. 2001;280:R1799–R1805. doi: 10.1152/ajpregu.2001.280.6.R1799. [DOI] [PubMed] [Google Scholar]
- Suda T, Miura Y, et al. The effect of hydrocortisone on human granulopoiesis in vitro with cytochemical analysis of colonies. Exp Hematol. 1983;11(2):114–121. [PubMed] [Google Scholar]
- Thaker PH, Han LY, et al. Chronic stress promotes tumor growth and angiogenesis in a mouse model of ovarian carcinoma. Nat Med. 2006;12(8):939–944. doi: 10.1038/nm1447. Epub 2006 Jul 23. [DOI] [PubMed] [Google Scholar]
- Villano Bonamin L, Barbuto JA, et al. Effects of social isolation on ehrlich tumor growth and tumor leukocyte infiltration in mice: evidence of participation of the submaxillary salivary gland. Neuroimmunomodulation. 2001;9(6):313–318. doi: 10.1159/000059388. [DOI] [PubMed] [Google Scholar]
- Wang X, Wu H, et al. Interleukin 1alpha (IL-1alpha) induced activation of p38 mitogen-activated protein kinase inhibits glucocorticoid receptor function. Mol Psychiatry. 2004;9(1):65–75. doi: 10.1038/sj.mp.4001339. [DOI] [PubMed] [Google Scholar]
- Weiner H. Perturbing the Organism: The Biology of Stressful Experience. Chicago: University of Chicago Press; 1992. [Google Scholar]
- Weinstein M, Goldman N. Social environment and biomarkers of aging study (SEBAS) in Taiwan, 2000 Codebook. Ann Arbor, MI: Inter-University Consortium for Political and Social Research; 2007. [Google Scholar]
- Weinstein M, Vaupel JW, et al. Biosocial surveys. Washington D. C.: The National Academies Press; 2007. [PubMed] [Google Scholar]
- Winkel P, Statland BE, et al. Within-day physiologic variation of leukocyte types in healthy subjects as assayed by two automated leukocyte differential analyzers. Am J Clin Pathol. 1981;75(5):693–700. doi: 10.1093/ajcp/75.5.693. [DOI] [PubMed] [Google Scholar]
- Wu W, Murata J, et al. Social isolation stress impairs the resistance of mice to experimental liver metastasis of murine colon 26-L5 carcinoma cells. Biol Pharm Bull. 2001;24(7):772–776. doi: 10.1248/bpb.24.772. [DOI] [PubMed] [Google Scholar]
- Zhang TY, Bagot R, et al. Maternal programming of defensive responses through sustained effects on gene expression. Biol Psychol. 2006;73(1):72–89. doi: 10.1016/j.biopsycho.2006.01.009. Epub 2006 Feb 28. [DOI] [PubMed] [Google Scholar]