Abstract
Background
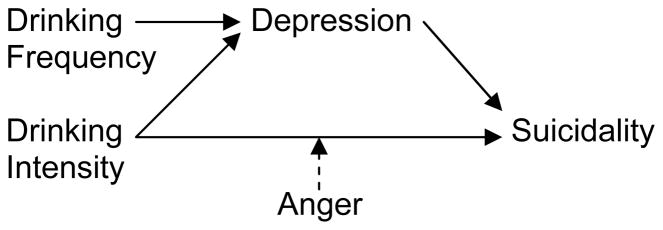
There are few data on the role of drinking patterns in suicidal thoughts or behavior among alcohol dependent individuals (ADIs), and meager data on variables that may influence the role of drinking in suicidal thoughts and behavior. This study tested a heuristic model that predicts that drinking promotes suicidal thoughts and behavior, the association is mediated (accounted for) by depressive symptoms, and that anger moderates (increases) the risk associated with intense drinking.
Methods
Data from Project MATCH, a multi-site alcohol use disorders treatment trial, were analyzed using structural equation modeling. There were 1,726 participants including 24% women and a mean age of 40.2 ± 11.0 years. Subjects were assessed at baseline and at 3-, 9-, and 15-month follow-up. Two categorical measures (presence/absence) of suicidal ideation (SI) were used that were analyzed in separate models. Predictors of interest were continuous assessments of average drinking intensity (i.e., drinks per drinking day or DDD), drinking frequency (i.e., percent days abstinent or PDA), depression, and anger.
Results
Both DDD and PDA were associated with SI at a statistically significant level, with PDA showing an inverse association. Depression scores served as a partial mediator or a full mediator of the drinking – SI relationship depending on the measure of SI used in the analysis. The models testing anger scores as a moderator fit the data poorly and did not support that anger serves as a moderator of the drinking – SI association.
Conclusions
Greater drinking intensity and drinking frequency predict SI among ADIs and depression serves as a mediator of these associations but anger does not appear to serve as a moderator. Further research is required to clarify if depression serves as a partial- or full mediator and to see if the results herein extend to suicidal behavior (i.e., suicide attempt, suicide).
Keywords: suicide, alcohol dependence, drinking, depression
INTRODUCTION
Alcohol dependent individuals (ADIs) are at elevated risk for suicide attempts (Kessler et al., 1999) and suicide (Yoshimasu and Miyashita, 2008), and more severe clinical populations are especially vulnerable (Wilcox et al., 2004). Suicidal ideation (SI) is critical to address in the prevention of suicidal behavior among treated ADIs. First, clinical suicide risk assessment protocols (Center for Substance Abuse Treatment, 2009; American Association of Suicidology, 2006) emphasize the need to screen for SI, assess SI (suicide plan? intent to act?), and track SI in the management of suicide risk. Second, SI is one of only two preconditions for suicidal behavior, the other being the availability of a method. Therefore, SI provides a common pathway through which all patients pass prior to carrying out a suicidal behavior, inspiring research on SI as a pathway to suicidal behavior (Conner et al., 2007; Joe et al., 2006; Kessler et al., 1999; Nock et al., 2009). Third, SI has consistently been demonstrated to confer prospective risk for suicidal behavior in adult clinical populations (Brown et al., 2000) including studies of alcohol and drug dependence (Britton and Conner, 2010; Darke et al., 2005; Darke et al., 2007; Ilgen et al., 2007).
Drinking and Suicidal Thoughts and Behavior
ADIs are most vulnerable to suicide during active drinking periods (Conner et al., 2000); ADIs with more severe drinking patterns are at higher long-term risk (Roy and Janal, 2007; Roy et al., 1990) and are at higher short-term risk for suicidal behavior compared to less severely drinking ADIs (Cornelius et al., 1996; Murphy et al., 1992). These data lead to the conclusion that “more drinking is worse,” yet a more refined understanding of drinking and suicidal thoughts and behavior will require the use of more specific measures of drinking. Two well-researched and relatively independent measures of drinking are the frequency of drinking and the average intensity of drinking (Babor et al., 1994). An analysis of Project MATCH data (Project MATCH Research Group, 1993) suggests that drinking intensity is more robustly associated with SI than drinking frequency (Conner et al., 2003). As well, an analysis of a large cohort of men followed prospectively for 16 years showed that high drinking intensity, defined in the study as > 2 standard drinks per drinking day, conferred risk for suicide whereas other measures of drinking including alcohol use frequency did not contribute to risk (Mukamal et al., 2007), although the generalization of these results to ADIs is unclear. Overall, studies on patterns of drinking and suicidal thoughts and behavior are few but available research suggests that drinking intensity more so than drinking frequency confers risk.
Clinical Model of Drinking and Suicidal Thoughts and Behavior
Beyond identification of the drinking variables (e.g., intensity, frequency) that promote suicidal thoughts and behavior, a comprehensive understanding of the role of drinking in suicidal thoughts and behavior requires the understanding of the interrelationship of drinking with other risk factors, including potential mediating and moderating relationships (Bagge and Sher, 2008). Studies of ADIs have firmly established that drinking promotes depressive symptoms and depressive disorders (Conner et al., 2009), and that depression stands out as a highly prevalent and potent risk factor for suicidal thoughts and behavior (Conner et al., 2003; Murphy et al., 1992; Preuss et al., 2002). These findings lead to a hypothesis that drinking promotes depression, which in turn promotes SI (and suicidal behavior), consistent with a conceptualization of mediation (Baron and Kenny, 1986). However, the extent to which depression mediates suicidal thoughts and behavior among ADIs is unknown, with implications for prevention and treatment. If, on the one hand, depression fully mediates the association between drinking and suicidal thoughts and behavior, it would suggest a dominant role of depression in the development of drinking-related risk among ADIs. On the other hand, if depression is a partial mediator, then it would suggest a more complex relationship and the need to explicate other mediators.
Like its counterpart depression in the internalizing spectrum, aggression stands out in the externalizing spectrum for the consistency with which it is shown to confer suicide-related risk in a variety of populations (Brezo et al., 2006; Conner et al., 2001), including clinical samples of ADIs (Koller et al., 2002; Oquendo et al., 2006; Sher et al., 2005; Windle, 2004). Conceptually, anger is a particularly promising aspect of aggression for suicide research studies, because it represents the affective component of aggression (Buss and Perry, 1992), and negative affect is presumed to be a hallmark of an acutely suicidal state (Shneidman, 1985). We hypothesize that the propensity for anger serves to moderate (increase) risk for suicidal thoughts and behavior conferred by drinking. We offer this hypothesis because suicidal behavior is known to occur reactively during intense drinking bouts (Berman et al., 2009; Hufford, 2001), and ADIs with heightened anger are conceptually more vulnerable to this scenario. In addition, anger has been shown to enhance the association between drinking and aggression (Giancola, 2002). Whether these findings generalize to suicidal thoughts or behaviors among ADIs (or other populations) is unknown. Note that the data showing associations of aggression and anger with suicidal thoughts and behavior are based overwhelmingly on general measures of aggression and anger and not on measures of “self-directed” aggression/anger (Brezo et al., 2006; Conner et al., 2001), suggesting that the findings are not circular, in other words they do not merely reflect a propensity for suicidal thoughts and behavior tapped by assessments of “self-directed” aggression/anger.
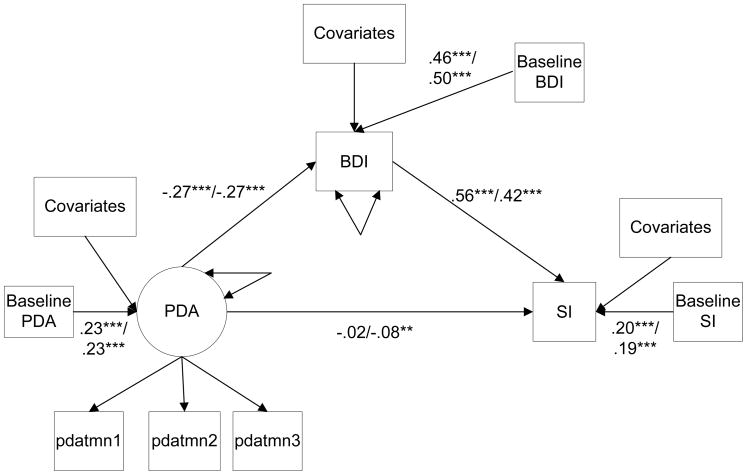
Integrating these ideas, we propose a heuristic model of drinking and suicidal thoughts and behavior among treated ADIs that proposes that drinking promotes risk, and that the association is mediated by depressive symptoms and it is moderated by anger. The model is based in part on the findings of an early study of suicide attempts among ADIs that described suicidal acts preceded by a chronic process marked by steady drinking and depression as well as suicidal acts that occurred during intense drinking bouts that were triggered by acute interpersonal conflict (Mayfield and Montgomery, 1972). These observations suggest the importance of integrating depression and steady alcohol use (i.e., drinking frequency) as well as intense drinking and anger proneness into a model of suicidal thoughts and behavior among ADIs. They further suggest that anger may serve as a moderator of the relationship between intense drinking in particular and suicidal thoughts and behavior. Figure 1 depicts a conceptual model that incorporates these ideas that depicts direct or mediating paths using solid lines and moderating paths using broken lines. Although research studies have consistently implicated drinking, depression, and anger in suicidal thoughts and behavior among ADIs as we have discussed, to our knowledge no suicide research study has examined the interrelationship of these variables in an adult alcohol dependent sample.
Figure 1.
Clinical Model of Drinking and Suicidality
Purpose
The study’s goals are addressed through a re-analysis of Project MATCH data (Project MATCH Research Group, 1993). MATCH assessed SI (but not suicidal behavior) prospectively, allowing for the longitudinal examination of SI. The first goal of the current study is to test depression as a mediator of the drinking – SI association, with a focus on determining if there is partial or full mediation of drinking frequency and drinking intensity respectively. The second goal is to test anger as a moderator of the relationship between these drinking variables and SI, and we hypothesized that anger moderates the association between drinking intensity and SI. Although an earlier analysis of drinking and SI using the MATCH sample examined drinking and SI (Conner et al., 2003), the study did not consider the mediating role of depression or the moderating role of anger.
MATERIALS AND METHODS
Procedure
Project MATCH (Project MATCH Research Group, 1993) was a large, multi-site, randomized clinical trial. Substance abuse patients were eligible if they were ages 18 and older, had a primary alcohol use disorder, read English at a 6th grade level of higher, and did not have co-occurring intravenous drug use, drug dependence (except cannabis), psychosis, organic impairment, or acute suicide risk. Participants entered the study through inpatient rehabilitation programs, representing the aftercare arm, or came directly to outpatient treatment, representing the outpatient arm. They were randomly assigned to one of three treatments that were provided on an outpatient basis over three months: cognitive behavioral treatment, motivational enhancement, and twelve-step facilitation. We refer to the sample as alcohol dependent individuals (ADIs) because 96% of participants met DSM-III-R criteria for alcohol dependence with or without alcohol abuse (American Psychiatric Association, 1987), with the remaining meeting criteria for alcohol abuse only. We analyzed the Project MATCH Public Use dataset that includes a pre-treatment interview (baseline) and three reassessments at 3-, 9-, and 15 months. There are 1,726 participants including 24% women and a mean age of 40.2 ± 11.0 years.
Measures
Suicidal ideation (SI)
SI is the outcome in all analyses. We derived two measures of SI to provide the ability to examine the consistency of results. The Beck Depression Inventory (BDI; (Beck et al., 1961) item #9 was used to create a categorical assessment of SI (“I have thoughts of killing myself but I would not carry them out” or “I would like to kill myself” or “I would kill myself if I had the chance”) and no SI (“I don’t have any thoughts of killing myself”). This item, that we refer to as BDI-SI, has been used to assess SI in several secondary analysis studies and is correlated with the detailed, multi-item Beck Scale for Suicide Ideation (Beck et al., 1997; Beck and Steer, 1991), supporting validity.
We also assessed SI using a modified item from the Addiction Severity Index (ASI (McLellan et al., 1980) that asks “During the past 30 days, have you had a period (even during a time when you were using drugs/alcohol) in which you experienced serious thoughts of suicide?” Responses were coded yes or no. We refer to this item as ASI-SI. Supporting validity, an SI item taken from the ASI has been shown to predict suicide attempts in treated substance abusers (Britton and Conner, 2010).
Drinking
We calculated average drinks per drinking day (DDD) and percent days abstinent (PDA) to quantify drinking intensity and frequency respectively (Babor et al., 1994). DDD and PDA were derived from data collected on the Form 90, a validated retrospective interview of daily alcohol use (Miller and Del Boca, 1994). Baseline drinking was based on a summary assessment of DDD and PDA in the three months prior to study entry. DDD and PDA for each of the follow-up assessments were calculated using the preceding three months of drinking data. We derived square-root transformed measures of DDD and arcsin-transformed measures of PDA to stabilize the variance as recommended (Babor et al., 1994).
Depressive symptoms
The Beck Depression Inventory (BDI; Beck, 1978) provided a continuous measure of depression severity. We removed the suicide item from the BDI scores to create a 20-item measure.
Anger
Total scores on the 44-item State-Trait Anger Expression Inventory provided a validated, summary measure of general anger (STAXI; (Spielberger, 1996). STAXI total scores are widely used to assess anger including in research of ADIs (Waldron et al., 2001; Witkiewitz and Villaroel, 2009).
Covariates
All analyses are adjusted for age, sex, race (white, non-white), treatment assignment (cognitive behavioral treatment, motivational enhancement, and twelve step facilitation), and study arm (aftercare, outpatient). In addition, the analyses of the DDD – SI association covary baseline PDA and the analyses of the PDA – SI association covary baseline DDD.
Analyses
General description
The analyses were performed using a constrained longitudinal Structural Equation Model (SEM) in MPlus (Muthen and Muthen, 2006). We assumed multinormality of the error terms. We formed latent measures of DDD such that a latent construct DDDj (j=3, 9, 15) at each follow-up assessment was formed from the respective prior three months of DDD variables using confirmatory factor analyses (Roberts, 1999). For example, DDD3 (at 3 months) was formed from DDD month 1, DDD month 2, and DDD month 3. A comparable latent construct was formed for the PDAj (j=3, 9, 15) variables. The factor variance was fixed at one for all of the latent constructs. We generated standardized estimates for all predictors in the models as follows: covariate X with raw estimate β and standard deviation=SD(X), with standard deviation of the response Y=SD(Y), was computed as so that the standard error of βstandardized is close to zero.
Each three month time period represented a time point (3-, 9-, and 15 months). If any covariate or response for a model at a given time point was missing, the subject was omitted from an analysis at that particular time point. The final estimates used in the models are constrained to be the same at each time point. Due to the SEM structure of the models, multiple equations were run simultaneously. Therefore a subject could be missing from one equation, but observed in another. To describe missing data (through counts of observations), we focus on the model with the response (outcome), either BDI-SI or ASI-SI, as this is the most informative. Model fits were assessed using the Chi-Square Test of Model Fit, Comparative Fit Index, CFI (Bentler, 1990), Tucker-Lewis index, TLI (Tucker and Lewis, 1973), and Root Mean Square Error of Approximation, RMSEA (Browne and Cudeck, 1993).
Specific models
We assessed the direct associations between each drinking variable (DDD, PDA) with each outcome (BDI-SI, ASI-SI) in separate models, after adjusting for the covariates. The analyses examining the mediating role of depression on the drinking variables were performed for four causal structures: 1) DDD→BDI→BDI-SI, 2) DDD→BDI→ASI-SI, 3) PDA→BDI→BDI-SI, and 4) PDA→BDI→ASI-SI. First, a path diagram was drawn to clarify the relationship. Three mediation models were run for each of the three month periods, under the constraint that all respective parameters should have the same estimate. Four models examining the moderating role of anger on the drinking variables were performed as follows: 1) logit(BDI-SI)= DDD + Anger + DDD*Anger, 2) logit(ASI-SI)= DDD + Anger + DDD*Anger, 3) logit(BDI-SI) = PDA + Anger + PDA*Anger, and 4) logit(ASI-SI) = PDA + Anger + PDA*Anger. For these models, latent constructs of DDD and PDA were formed as previously described, with the factor variance fixed to one and under the constraint that all the parameters would have the same estimates for all three time points (consisting of each three month period). Anger was observed at each assessment time and was also included under the constraint that all the parameters would have the same estimates for all three time points.
RESULTS
Descriptive Data
Of 1,726 participants, BDI-SI data are available at baseline for 96.3% of the sample, at 3 months 90.0%, at 9 months 87.4%, and at 15 months 89.2%. ASI-SI data are available at baseline for 100% of the sample, at 3 months 91.5%, at 9 months 89.2%, and at 15 months 90.1%. Demographic characteristics of participants stratified by SI status (present or absent) at baseline assessment are presented in Table 1. Using both outcomes (BDI-SI, ASI-SI), participants with SI are more likely to be female, younger, and white (p<.05). The percentage of subjects with SI at each assessment is shown in Table 2 (denominator is based on subjects with available data on SI at a given assessment). These measures show a similar prevalence of SI at baseline and the prevalence of SI at follow-ups is higher based on the BDI-SI than the ASI-SI. Descriptive data on the predictors of interest (DDD, etc.) at each wave are also shown in Table 1.
Table 1.
Descriptive Data on SI and Demographic Characteristics at Baseline Assessment
| BDI-SI Results | |||||
|---|---|---|---|---|---|
| SI Status | Male (%) | Female (%) | Age (M ± SD) | White (%) | Nonwhite (%) |
| Present | 10.5 | 13.0 | 38.6 ± 10.3 | 11.8 | 9.3 |
| Absent | 89.5 | 87.0 | 40.5 ± 11.0 | 88.2 | 90.7 |
| ASI-SI Results | |||||
| SI Status | Male (%) | Female (%) | Age (M ± SD) | White (%) | Nonwhite (%) |
| Present | 9.9 | 14.6 | 39.3 ± 10.6 | 11.3 | 9.9 |
| Absent | 89.1 | 85.4 | 40.4 ± 11.0 | 88.7 | 90.1 |
Table 2.
Descriptive data on SI and predictors of interest
| Measure | Baseline | 3 months | 9 months | 15 months |
|---|---|---|---|---|
| BDI SI item (%) | 11.1% | 9.3% | 11.7% | 13.8% |
| ASI SI item (%) | 11.0% | 5.2% | 3.9% | 4.7% |
| DDD (Mean, SD) | 16.6 (10.6) | 4.4 (7.1) | 4.5 (7.1) | 4.6 (7.0) |
| PDA (Mean, SD) | .31 (.30) | .80 (.31) | .79 (.32) | .78 (.32) |
| BDI (Mean, SD) | 10.1 (8.1) | 7.5 (7.7) | 7.7 (7.8) | 7.8 (8.2) |
| STAXI (Mean, SD) | 30.1 (7.5) | 27.7 (7.1) | 27.0 (7.2) | 26.4 (7.2) |
Notes. BDI SI item = Suicidal ideation (SI) based on Beck Depression Inventory (BDI) suicide item, ASI SI item = SI based on Addiction Severity Index (ASI) suicide item, DDD = drinks per drinking day, PDA = percent days abstinent, BDI = BDI score minus suicide item, STAXI = State-Trait Anger Expression Inventory score. DDD and PDA raw scores are shown here but they are transformed (log, arcsine) in analyses.
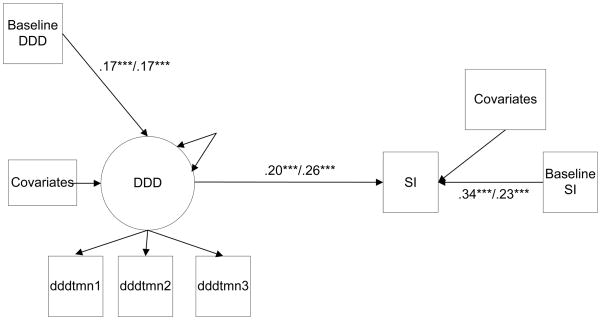
DDD Analyses
The basic SEM models (i.e., that do not consider mediation or moderation) that examine DDD as a predictor of SI over follow-up are shown in Figure 2. Both models adequately fit the data, with model fit information provided in the figure. In the models, the standardized coefficients between DDD scores (log transformed) and SI were positive and statistically significant (p<.001), supporting the association between DDD and SI. In the models baseline DDD is also predictive of DDD over follow-up (p<.001), and baseline SI is predictive of SI over follow-up (p<.001). The BDI-SI models are based on 87.1% of the total sample at 3 months follow-up, 84.4% at 9 months, and 85.7% at 15 months. The ASI-SI models are based on 90.9% of the total sample at 3 months, 89.0% at 9 months, and 90.4% at 15 months.
FIGURE 2.
Constrained longitudinal logistic Structural Equation Models (SEM) examining drinks per drinking day (DDD) and suicidal ideation (SI). Standardized estimates of the coefficients for the BDI-SI outcome are presented before the slash; estimates for the ASI-SI are presented after the slash. Covariates include gender, age, race, treatment assignment, study arm and baseline PDA.
χ 2BDI (47) = 189.113,p =< .001; comparative fit index (CFI)=.924; Tucker-Lewis index (TLI)=.906; root mean square error of approximation (RMSEA)=.044.
χ2ASI (47) = 129.157,p =< .001; CFI=.952; TLI=.941; RMSEA=.033.
***p<.001.
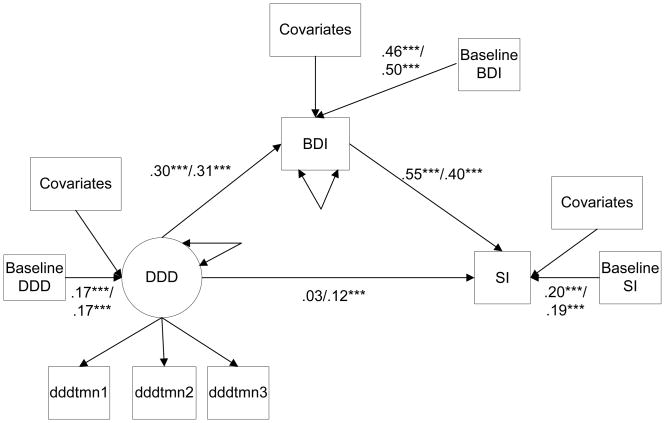
The models that examine depression (BDI score) as a mediator of the DDDshown in Figure 3. Both models adequately fit the data as shown in the figure. In the models, there are statistically significant paths from DDD over follow-up to depression over follow-up (p<.001) and from depression over follow-up to SI over follow-up (p<.001). There are somewhat different mediation results when depression is examined as a mediator in the BDI-SI model compared to the ASI-SI model. In the BDI-SI model, the path from DDD to BDI-SI is greatly reduced and is non-significant (p=.209) compared to the basic model. These results suggest that when depression is added to the model it acts as a full mediator of the association between DDD and SI. However, in the ASI-SI model, the path from DDD to SI is somewhat reduced compared to the basic model but nonetheless it remains statistically significant (p<.001), suggesting that when depression is added to the model it acts as a partial (but not full) mediator of the association between DDD and SI. The BDI-SI mediation models are based on 86.0% of the total sample at 3 months follow-up, 82.7% at 9 months, and 83.7% at 15 months. The ASI-SI mediation models are based on 87.8% of the total sample at 3 months, 85.1% at 9 months, and 86.3% at 15 months.
FIGURE 3.
Constrained longitudinal logistic Structural Equation Models (SEM) examining Beck Depression Inventory (BDI) scores, with the BDI suicide item removed, as a mediator of the association between drinks per drinking day (DDD) and suicidal ideation (SI). Standardized estimates of the coefficients for the BDI-SI outcome are presented before the slash; estimates for the ASI-SI are presented after the slash. Covariates include gender, age, race, treatment assignment, study arm and baseline PDA.
χ2BDI (59) = 218.288,p =< .001; CFI=.947; TLI=.933; RMSEA=.042.
χ2ASI (65) = 240.790,p =< .001; CFI=.941; TLI=.928; RMSEA=.042.
**p .01/ ***p<.001.
We also examined anger (STAXI score) as a moderator of the DDD–SI association by use of M-Plus (models not shown). The interaction term for DDD and anger in the BDI-SI model (estimate=0, p=.006) does not support statistical moderation, because an estimate of ‘0’ in MPlus is not consistent with an interaction effect. Moreover, the statistically significant result in this instance is misleading because of the poor model fit (χDDD 2 (53)=13272.642, p=<.001;CFI=.07; TLI= −.211; RMSEA=.419). Similarly, the interaction term for DDD and anger in the ASI-SI model (estimate=0, p=.432) analyzed using MPlus does not support statistical moderation, and the model fit is poor (χDDD2 (54)=13663.149, p=<.001; CFI=.042; TLI= −.241; RMSEA=.420). There are a similar number of observations (i.e., similar missing data) in these models compared to the meditational models.
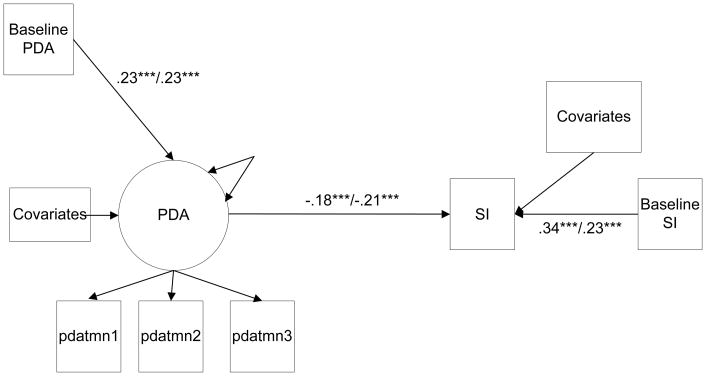
PDA Analyses
The basic SEM models (i.e., that do not consider mediation or moderation) that examine PDA as a predictor of BDI-SI and ASI-SI respectively over follow-up are shown in Figure 4. Both models show adequate fit as shown in the figure. In the models, the coefficients between PDA scores (arc sine transformed) and SI are negative and statistically significant (p<.001), supporting that PDA is inversely associated with SI. In both models baseline PDA is also predictive of PDA over follow-up (p<.001), and baseline SI is predictive of SI over follow-up (p<.001). These models contain the same number of observations as the basic DDD models.
FIGURE 4.
Constrained longitudinal logistic Structural Equation Models (SEM) examining percent days abstinent (PDA) and suicidal ideation (SI). Standardized estimates of the coefficients for the BDI-SI outcome are presented before the slash; estimates for the ASI-SI are presented after the slash. Covariates include gender, age, race, treatment assignment, study arm and baseline DDD.
χ2BDI (39) =162.563,p =<.001; CFI=.939; TLI=.920; RMSEA=.045.
χ2ASI (39) =116.996,p =< .001; CFI=.959; TLI=.947; RMSEA=.035.
***p<.001.
The models that examine depression (BDI score) as a mediator of the PDA – SI association are shown in Figure 5. Both models adequately fit the data as shown in the figure. In the models, there are statistically significant negative correlations from PDA over follow-up to depression over follow-up (p<.001), and there are positive correlations from depression over follow-up to SI over follow-up (p<.001). Similar to the findings for the analyses of DDD, there are somewhat different mediation results in the BDI-SI and the ASI-SI models. In the BDI-SI model, the absolute correlation from PDA to SI is greatly reduced compared to the basic model, and it is statistically non-significant (p=.303). The results suggest that when depression is added to the model it acts as a full mediator of the association between PDA and SI. However, in the ASI-SI model, the absolute correlation from PDA to SI is somewhat reduced compared to the basic model but nonetheless a statistically significant, inverse association between PDA and SI remains (p=.010); this suggests that when depression is added to the model, it acts as a partial (but not full) mediator of the association between PDA and SI. These models contain the same number of observations as the DDD models that consider mediation.
FIGURE 5.
Constrained longitudinal logistic Structural Equation Models (SEM) examining Beck Depression Inventory (BDI) scores, with the BDI suicide item removed, as a mediator of the association between percent days abstinent (PDA) and suicidal ideation (SI). Standardized estimates of the coefficients for the BDI-SI outcome are presented before the slash; estimates for the ASI-SI are presented after the slash. Covariates include gender, age, race, treatment assignment, study arm and baseline DDD.
χ2BDI (52) =175.256,p =<.001; CFI=.960; TLI=.947; RMSEA=.039.
χ 2ASI (57) = 208.896,p =< .001; CFI=.951; TLI=.937; RMSEA=.042.
**p ≤.01/ ***p<.001.
We also examined anger (STAXI score) as a moderator of the PDA–SI association (models not shown). Analyses using M-Plus showed that the interaction term for PDA and anger in the BDI-SI model (estimate=0, p=.055) does not support statistical moderation. Moreover, there is a poor model fit (χPDA 2 (53)=3249.439, p=<.001; CFI=.262; TLI= .068; RMSEA=.206). Similarly, the interaction term for PDA and anger in the ASI-SI model (estimate=− .02, p=.252) analyzed using MPlus does not support statistical moderation, and the model fit is also poor (χPDA 2 (53)=3180.494, p=<.001; CFI=.227; TLI= .023; RMSEA=.203). These models contain the same number of observations as the DDD models that consider mediation.
DISCUSSION
In the simple models without mediation or moderation, higher average drinking intensity as measured by DDD predicted greater likelihood of SI, and less frequent drinking as measured by PDA predicted lower likelihood of SI. The findings implicate both greater drinking intensity and greater drinking frequency in the promotion of suicidal thoughts and behavior among treated ADIs.
The results also showed that depression mediates the relationship between drinking frequency and drinking intensity with SI. Moreover, the degree of mediation (partial or full) by depression was sensitive to the assessment of SI. When BDI-SI was the outcome, depression fully mediated the association between the drinking variables and SI. However, when ASI-SI was the outcome, depression served as a partial mediator. These somewhat differing results are most likely attributable to measurement. The BDI-SI outcome variable was created using the suicide item from the BDI, and the BDI served as the measure of depression to test mediation. Therefore, although we removed the BDI suicide item from the BDI when we examined the latter as a mediator, greater similarity between the modified BDI (with the suicide item removed) and the BDI-SI outcome may be expected than with the use of a measure of SI derived using another scale (i.e., ASI-SI). Moreover, SI is a cognitive variable, and the BDI is weighted to assess the cognitive features of depression, consistent with Beck’s cognitive theory of depression (Beck, 1967). In retrospect, these measure characteristics made it more likely that depression would more strongly mediate the relationship between drinking and SI assessed using the BDI-SI than the ASI-SI, consistent with the findings.
This study did not support the hypothesis that anger serves as a moderator of the relationship between drinking intensity (or drinking frequency) and SI in treated ADIs. Several features of the study make it ideal for examining this hypothesis, including the large sample size; reliable and valid assessments of drinking intensity, drinking frequency, and anger; and the use of two assessments of SI that maximized the opportunity to uncover moderation. Although anger does not appear to moderate the drinking –SI relationship, it is important to note that the generalizability of these results to suicidal behavior (i.e., suicide attempt, suicide) is unclear. Whether or not anger (and related constructs) potentiates the risk for suicidal behavior associated with drinking requires further study. For example anger may be hypothesized to promote unplanned (impulsive) acts of suicidal behavior during acute drinking bouts. In this context, suicidal behavior may occur with little forethought, a process that may be insensitive to detection with assessments of SI that are presumably better at capturing more persistent ideation. Along these lines, a study of ADIs showed that a measure of alcohol-related aggression was uniquely related to a history of unplanned suicide attempts but was not associated at a statistically significant level with SI or planned attempts (Conner et al., 2007), although the study was limited by the retrospective research design.
Limitations
There are limitations of the study that are important to note. Although prior studies support the validity of the BDI-SI and ASI-SI as assessments of SI, neither measure is considered a gold standard. The BDI-SI is taken from an item on the BDI which likely served to increase the association between depression (assessed with the BDI) and SI as well as the mediating role of depression in the models using the BDI-SI outcome. Given our hypothesis that anger moderates the relationship between drinking and suicidal thoughts and behavior, it would have been ideal to also analyze a measure of anger while drinking, although the fact that individuals who are prone to anger in general also appear to be most prone to anger while drinking tempers this limitation somewhat (Giancola, 2002). The generalizability of results to suicidal behavior is unclear. Patients at acute risk for suicidal behavior, a group of keen interest, were excluded in MATCH, although we do not know how many patients were excluded for this reason. Although a model of drinking and sucidal thoughts and behavior featuring depression and anger in mediation and moderation is a logical starting point, additional mediators and moderators should be examined as guided by theory and future studies. We also did not exhaustively examine all potential directional pathways. In this regard, depression may also lead to drinking consistent with a negative affect model of drinking (Cooper et al., 1995). Finally, the results consider drinking pattern, and relevance to drinking in the event is unclear.
Conclusion and Future Directions
We tested a clinical model of drinking and suicidal thoughts and behavior among ADIs (see Figure 1). As hypothesized, measures of average drinking intensity and drinking frequency predicted SI and these associations were mediated by depression. However, inconsistent with our hypotheses, anger did not moderate the association between drinking intensity and SI, suggesting the need for refinement of the model. Unresolved questions raised by the analyses can be addressed in future studies including use of a gold standard measure of SI such as the Scale for Suicidal Ideation (Beck et al., 1979) to more definitively determine whether depression partially or fully mediates the association between drinking and SI. As well, the conceptual model should be tested with suicidal behavior (i.e., suicide attempt, suicide). More definitive results may be obtained with the use of experience sampling (Hussong, 2007) or a related strategy to gather real-time assessments of drinking, affect, and suicidal thoughts or behavior. Until such data become available, it is essential to take advantage of available resources including secondary datasets to advance the field.
Acknowledgments
The work supported in part by NIH Grant R01 AA016149 (Conner, PI)
Reference List
- American Association of Suicidology. Assessment and Management of Suicide Risk: Core Competencies for Mental Health Professionals. Educational Developmental Center; Washington, DC: 2006. [Google Scholar]
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. American Psychiatric Association; Washington, DC: 1987. [Google Scholar]
- Babor TF, Longabough R, Zweben A, Fuller RK, Stout RL, Anton RF, Randall CL. Issues in the definition and measurement of drinking outcomes in alcoholism treatment research. J Stud Alcohol Drug. 1994;12 (suppl):101–111. doi: 10.15288/jsas.1994.s12.101. [DOI] [PubMed] [Google Scholar]
- Bagge CL, Sher KJ. Adolescent alcohol involvement and suicide attempts: Toward the development of a conceptual framework. Clin Psychol Rev. 2008;28:1283–1296. doi: 10.1016/j.cpr.2008.06.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baron RM, Kenny DA. The moderator-mediator variable distinction in social psychological research: Conceptual, strategic, and statistical considerations. J Pers Soc Psychol. 1986;51:1173–1182. doi: 10.1037//0022-3514.51.6.1173. [DOI] [PubMed] [Google Scholar]
- Beck AT. Depression: Causes and Treatment. University of Pennsylvania Press; Philadelphia: 1967. [Google Scholar]
- Beck AT, Brown GK, Steer RA. Psychometric characteristics of the scale for suicide ideation with psychiatric outpatients. Behav Res Ther. 1997;35:1039–1046. doi: 10.1016/s0005-7967(97)00073-9. [DOI] [PubMed] [Google Scholar]
- Beck AT, Kovacs M, Weissman A. Assessment of suicidal ideation: The scale for suicidal ideation. J Consult Clin Psychol. 1979;47:343–352. doi: 10.1037//0022-006x.47.2.343. [DOI] [PubMed] [Google Scholar]
- Beck AT, Steer RA. Manual for the Beck Scale for Suicidal Ideation. Psychological Corporation; San Antonio, TX: 1991. [Google Scholar]
- Beck AT, Ward CH, Mendelsohn M, Mock J, Erbaugh J. An inventory for measuring depression. Arch Gen Psychiatry. 1961;4:561–571. doi: 10.1001/archpsyc.1961.01710120031004. [DOI] [PubMed] [Google Scholar]
- Bentler PM. Comparative fit indexes in structural models. Psychol Bull. 1990;107:238–246. doi: 10.1037/0033-2909.107.2.238. [DOI] [PubMed] [Google Scholar]
- Berman ME, Bradley TP, Fanning JR, McCloskey MS. Self-focused attention reduces self-injurious behavior in alcohol-intoxicated men. Sub Use Misuse. 2009;44:1280–1297. doi: 10.1080/10826080902961328. [DOI] [PubMed] [Google Scholar]
- Brezo J, Paris J, Turecki G. Personality traits as correlates of suicidal ideation, suicide attempts, and suicide completion: a systematic review. Acta Pscyh Scand. 2006;113:180–206. doi: 10.1111/j.1600-0447.2005.00702.x. [DOI] [PubMed] [Google Scholar]
- Britton PC, Conner KR. Suicide attempts within 12 months of treatment for substance use disorders. Suic Life-Threat Behav. 2010;40:14–21. doi: 10.1521/suli.2010.40.1.14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown GK, Beck AT, Steer RA, Grisham JR. Risk factors for suicide in psychiatric outpatients: A 20-year prospective study. J Consult Clin Psychol. 2000;68:371–377. [PubMed] [Google Scholar]
- Browne MW, Cudeck R. Alternative ways of assessing model fit. In: Bollen KA, Long JS, editors. Testing Structural Equation Models. Sage; Newbury Park: 1993. pp. 136–192. [Google Scholar]
- Buss AH, Perry M. The aggression questionnaire. J Pers Soc Psychol. 1992;63:452–459. doi: 10.1037//0022-3514.63.3.452. [DOI] [PubMed] [Google Scholar]
- Center for Substance Abuse Treatment. Addressing Suicidal Thoughts and Behaviors in Substance Abuse Treatment. Substance Abuse and Mental Health Services Administration; Rockville, MD: 2009. [PubMed] [Google Scholar]
- Conner KR, Duberstein PR, Conwell Y, Herrmann JH, Cox C, Barrington DS, Caine ED. After the drinking stops: Completed suicide in individuals with remitted alcohol use disorders. J Psychoactive Drugs. 2000;32:333–337. doi: 10.1080/02791072.2000.10400457. [DOI] [PubMed] [Google Scholar]
- Conner KR, Duberstein PR, Conwell Y, Seidlitz L, Caine ED. Psychological vulnerability to completed suicide: A review of empirical studies. Suicid Life-Threat Behav. 2001;31:367–385. doi: 10.1521/suli.31.4.367.22048. [DOI] [PubMed] [Google Scholar]
- Conner KR, Hesselbrock VM, Meldrum SC, Schuckit MA, Bucholz KK, Gamble SA, Wines JD, Kramer J. Transitions to, and correlates of, suicidal ideation, plans, and unplanned and planned suicide attempts among 3729 men and women with alcohol dependence. J Stud Alcohol Drugs. 2007;68:654–662. doi: 10.15288/jsad.2007.68.654. [DOI] [PubMed] [Google Scholar]
- Conner KR, Li Y, Meldrum S, Duberstein PR, Conwell Y. The role of drinking in suicidal ideation: Analyses of Project MATCH data. J Stud Alcohol. 2003;64:402–408. doi: 10.15288/jsa.2003.64.402. [DOI] [PubMed] [Google Scholar]
- Conner KR, Pinquart M, Gamble SA. Meta-analysis of depression and substance use among individuals with alcohol use disorders. J Sub Abuse Treat. 2009;37:127–137. doi: 10.1016/j.jsat.2008.11.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cooper LM, Frone MR, Russell M, Mudar P. Drinking to regulate positive and negative emotions: A motivational model of alcohol use. J Pers Soc Psychol. 1995;69:990–1005. doi: 10.1037//0022-3514.69.5.990. [DOI] [PubMed] [Google Scholar]
- Cornelius JR, Salloum IM, Day NL, Thase ME, Mann JJ. Patterns of suicidality and alcohol use in alcoholics with major depression. Alcohol Clin Exp Res. 1996;20:1451–1455. doi: 10.1111/j.1530-0277.1996.tb01148.x. [DOI] [PubMed] [Google Scholar]
- Darke S, Ross J, Williamson A, Mills KL, Havard A, Teesson M. Patterns and correlates of attempted suicide by heroin users over a 3-year period: findings from the Australian treatment outcome study. Drug Alcohol Depend. 2007;87:146–152. doi: 10.1016/j.drugalcdep.2006.08.010. [DOI] [PubMed] [Google Scholar]
- Darke S, Williamson S, Ross J, Teesson M. Attempted suicide among heroin users: 12-month outcomes from the Australian treatment outcome study (ATOS) Drug Alcohol Depend. 2005;78:177–186. doi: 10.1016/j.drugalcdep.2004.10.009. [DOI] [PubMed] [Google Scholar]
- Giancola PR. The influence of trait anger on the alcohol-aggression relation in men and women. Alcohol Clin Exp Res. 2002;26:1350–1358. doi: 10.1097/01.ALC.0000030842.77279.C4. [DOI] [PubMed] [Google Scholar]
- Hufford MR. Alcohol and suicidal behavior. Clin Psychol Rev. 2001;21:797–811. doi: 10.1016/s0272-7358(00)00070-2. [DOI] [PubMed] [Google Scholar]
- Hussong AM. Predictors of drinking immediately following daily sadness: An application of survival analysis to experience sampling data. Addict Behav. 2007;32:1054–1065. doi: 10.1016/j.addbeh.2006.07.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ilgen MA, Harris AHS, Moos RH, Tiet QQ. Predictors of suicide attempt one year after entry into substance use disorder treatment. Alcohol Clin Exp Res. 2007;31:635–642. doi: 10.1111/j.1530-0277.2007.00348.x. [DOI] [PubMed] [Google Scholar]
- Joe S, Baser RE, Breeden G, Neighbors HW, Jackson JS. Prevalence of and risk factors for lifetime suicide attempts among Blacks in the U.S. JAMA. 2006;296:2112–2123. doi: 10.1001/jama.296.17.2112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler RC, Borges G, Walters EE. Prevalence of and risk factors for lifetime suicide attempts in the National Comorbidity Survey. Arch Gen Psychiatry. 1999;56:617–625. doi: 10.1001/archpsyc.56.7.617. [DOI] [PubMed] [Google Scholar]
- Koller G, Preuss UW, Bottlender M, Wenzel K, Soyka M. Impulsivity and aggression as predictors of suicide attempts in alcoholics. European Arch Psychiatry Clin Neurosci. 2002;252:155–160. doi: 10.1007/s00406-002-0362-9. [DOI] [PubMed] [Google Scholar]
- Mayfield DG, Montgomery D. Alcoholism, alcohol intoxication, and suicide attempts. Arch Gen Psychiatry. 1972;27:349–353. doi: 10.1001/archpsyc.1972.01750270055008. [DOI] [PubMed] [Google Scholar]
- McLellan AT, Luborsky L, Woody GE, O'Brien CP. An improved diagnostic evaluation instrument for substance abuse patients. J Nerv Mental Dis. 1980;178:26–33. doi: 10.1097/00005053-198001000-00006. [DOI] [PubMed] [Google Scholar]
- Miller WR, Del Boca FK. Measurement of drinking behavior using the Form 90 family of instruments. J Stud Alcohol. 1994;12(Suppl):112–118. doi: 10.15288/jsas.1994.s12.112. [DOI] [PubMed] [Google Scholar]
- Mukamal KJ, Kawachi I, Miller M, Rimm EB. Drinking frequency and quantity and risk of suicide among men. Soc Psychiatry Psychiatric Epidem. 2007;42:153–160. doi: 10.1007/s00127-006-0144-1. [DOI] [PubMed] [Google Scholar]
- Murphy GE, Wetzel RD, Robins E, McEvory L. Multiple risk factors predict suicide in alcoholism. Arch Gen Psychiatry. 1992;49:459–463. doi: 10.1001/archpsyc.1992.01820060039006. [DOI] [PubMed] [Google Scholar]
- Muthen BO, Muthen LK. M+ User's Guide. 4. Muthen & Muthen; Los Angeles: 2006. [Google Scholar]
- Nock MK, Hwang I, Sampson NA, Kessler RC. Mental disorders, comorbidity and suicidal behavior: Results from the National Comorbidity Survey Replication. [Accessed June 27, 2009.];Molec Psychiatry. doi: 10.1038/mp.2009.29. [online]. 2009. Available at: http://www.nature.com/mp/journal/vaop/ncurrent/pdf/mp200929a.pdf. [DOI] [PMC free article] [PubMed]
- Oquendo MA, Russo SA, Underwood MD, Kassir SA, Ellis SP, Mann JJ, Arango V. Higher postmortem prefrontal 5-HT2A receptor binding correlates with lifetime aggression in suicide. Bio Psychiatry. 2006;59:235–243. doi: 10.1016/j.biopsych.2005.06.037. [DOI] [PubMed] [Google Scholar]
- Preuss UW, Schuckit MA, Smith TL, Danko GP, Buckman K, Bierut L, Bucholz KK, Hesselbrock MN, Hesselbrock VM, Reich T. Comparison of 3190 alcohol-dependent individuals with and without suicide attempts. Alcohol Clin Exp Res. 2002;26:471–477. [PubMed] [Google Scholar]
- Project MATCH Research Group. Project MATCH: Rationale and methods for a multisite clinical trial matching patients to alcoholism treatment. Alcohol Clin Exp Res. 1993;17:1130–1145. doi: 10.1111/j.1530-0277.1993.tb05219.x. [DOI] [PubMed] [Google Scholar]
- Roberts JK. Basic concepts of confirmatory factor analysis. Paper presented at the Annual Meeting of the Southwest Educational Research Association; San Antonio, TX. 1999. [Google Scholar]
- Roy A, Janal MN. Risk factors for suicide attempts among alcohol dependent patients. Arch Suicid Res. 2007;11:211–217. doi: 10.1080/13811110701250150. [DOI] [PubMed] [Google Scholar]
- Roy A, Lamparski D, DeJong J, Moore V, Linnoila M. Characteristics of alcoholics who attempt suicide. Am J Psychiatry. 1990;147:761–765. doi: 10.1176/ajp.147.6.761. [DOI] [PubMed] [Google Scholar]
- Sher L, Oquendo MA, Galfalvy HC, Grunebaum MF, Burke AK, Zalsman G, Mann JJ. The relationship of aggression to suicidal behavior in depressed patients with a history of alcoholism. Addict Behav. 2005;30:1144–1153. doi: 10.1016/j.addbeh.2004.12.001. [DOI] [PubMed] [Google Scholar]
- Shneidman ES. Definition of Suicide. New York: Wiley; 1985. [Google Scholar]
- Spielberger CD. State-Trait Anger Expression Inventory: Professional Manual. Psychological Assessment Resources; Odessa, TX: 1996. [Google Scholar]
- Tucker LR, Lewis C. The reliability coefficient for maximum likelihood factor analysis. Psychometrika. 1973;38:1–10. [Google Scholar]
- Waldron HB, Miller WR, Tonigan JS. Client anger as a predictor of differential response to treatment. In: Longabaugh R, Wirtz PW, editors. Project MATCH Hypotheses: Results and Causal Chain Analyses. National Institute on Alcohol Abuse and Alcoholism; Bethesda, MD: 2001. pp. 134–148. [Google Scholar]
- Wilcox HC, Conner KR, Caine ED. Association of alcohol and drug use disorders and completed suicide: An empirical review of cohort studies. Drug Alcohol Depend. 2004;76:S11–S19. doi: 10.1016/j.drugalcdep.2004.08.003. [DOI] [PubMed] [Google Scholar]
- Windle M. Suicidal behaviors and alcohol use among adolescents: A developmental psychopathology perspective. Alcohol Clin Exp Res. 2004;28:29S–37S. doi: 10.1097/01.alc.0000127412.69258.ee. [DOI] [PubMed] [Google Scholar]
- Witkiewitz K, Villaroel NA. Dynamic association between negative affect and alcohol lapses following alcohol treatment. J Consult Clin Psychol. 2009;77:633–644. doi: 10.1037/a0015647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yoshimasu K, Miyashita K. Suicidal risk factors and completed suicide: meta-analyses based on psychological autopsy studies. Environ Health Prev Med. 2008;13:243–256. doi: 10.1007/s12199-008-0037-x. [DOI] [PMC free article] [PubMed] [Google Scholar]