Abstract
The aim of this study was to assess the epidemiological characteristics of a representative sample of subsidized low-cost housing communities in the City of Cape Town in relation to their living conditions and their health status. Four subsidized low-cost housing communities were selected within the City of Cape Town in this cross-sectional survey. Structured interviews were administered in 336 dwellings on 173 plots. Data was obtained from 1,080 persons with a response rate of 100%. Almost all of the state-subsidized houses had one or more shacks in the backyard, increasing the occupation density and putting the municipal sanitation infrastructure under pressure. In 40% of main houses, one or more cases of diarrhea were reported during the two weeks preceding the survey, in contrast to 23% of shacks (p < 0.0007). Of the total group, 1.7% willingly disclosed that they were HIV positive, while 3.5% reported being tuberculosis (TB) positive. One of them reported having multiple drug-resistant TB. None of the HIV positive or TB positive persons was on any treatment. A reported 6.3% of the families admitted regularly eating only one meal per day, whereas 18.5% reported having only two meals per day. The shack dwellers had significantly higher education and employment status (p < 0.01), since they had to pay rent. Improvements in health intended by the rehousing process did not materialize for the recipients of low-cost housing in this study. The health vulnerability of individuals in these communities had considerable implications for the curative health services. Sanitation failures, infectious disease pressure, and environmental pollution in these communities represent a serious public health risk. The densification caused by backyard shacks, in addition, has municipal service implications and needs to be better managed. Urgent intervention is needed to allow the state-funded housing schemes to deliver the improved health that was envisaged at its inception.
Keywords: Low-cost housing, Backyard dwelling, Health vulnerability, Community health, Epidemiology
Introduction
Adequate shelter with access to safe water and sanitation are essential elements of community health.1 However, in developing countries, suitable and affordable housing is often in short supply.2 Urbanization, in the form of the rural–urban drift, has affected South Africa,3 contributing to the housing backlog and posing major challenges in aspects of economics, education, housing, and public health.4
The South African government responded to the demand for low-cost housing with large-scale housing initiatives, such as the Breaking New Ground initiative, previously known as the Reconstruction and Development Programme. These mass, state-sponsored housing schemes are partially funded by the central government, but the actual provision of the houses as well as the building and upkeep of utilities and services rest with the local municipalities.
In South Africa, the recipients of low-cost housing are usually selected from the ranks of those who occupy the many informal settlements surrounding our cities and towns. Unfortunately, ownership of a subsidized house was in most cases not accompanied by an improvement in income. The owners of low-cost houses soon exploited one of the few resources they had—i.e., space—by allowing others to build informal structures (called “shacks” by the inhabitants) in the backyard, which are rented out for income.
The importance of adequate housing for the maintenance of health is one of the basic tenets of public health, yet the association between them remains difficult to quantify.5 It is still not known whether re-housing previously disadvantaged groups will improve their health. Although many studies found an improvement, most studies did not adjust for potential confounding factors.6 This lack of evidence of what appears to be self-evident can be attributed to the multi-factorial and complex nature of low-cost housing, the accompanying poverty, and environmental degradation.6
The almost universal presence of informal structures in the backyards of low-cost housing in Cape Town presented an opportunity to investigate yet another factor in this complex causal chain. This scenario comprised two groups of disadvantaged people (those living in formal housing and those living in shacks) on the same premises. This survey analysed the characteristics of a representative sample of low-cost housing communities in the City of Cape Town, where almost all state-sponsored houses had backyard dwellings, in order to assess the relationship between their living conditions and their health vulnerability.
Methods
This study was approved by the Committee for Human Research at the Faculty of Health Sciences of Stellenbosch University and was conducted according to the ethical guidelines and principles of the International Declaration of Helsinki,7 the South African Guidelines for Good Clinical Practice, and the Ethical Guidelines for Research of the Medical Research Council of South Africa.8 All respondents were informed of the objective of the study in one of three languages (English, Afrikaans or isiXhosa) of their choice and signed informed consent. A copy of the informed consent was provided to all participating households. The survey was conducted anonymously. All participants could inspect the completed questionnaire answer sheet for anonymity. They then posted the form into a sealed box with a postal slot. The box was only unsealed at the end of the study.
Characterization of Housing Type
Four subsidized housing communities were selected within the City of Cape Town Metropole (CCTM) to participate in this cross-sectional survey. The low-cost housing communities identified as study sites were: Driftsand, Greenfields, Masipumelela and Tafelsig. These sites were selected to represent the best geographic spread of all the subsidized housing settlements within the city. The settlements were selected regardless of the local or central authority under whose jurisdiction the housing schemes were originally erected. They had to be older than three years. This was important because in some of the newer settlements, structural wear and tear of the houses had not yet become evident to the same extent as in the older settlements. The settlements selected had to have distinct boundaries that did not blend into informal settlement areas (so-called squatter settlements) in order to avoid garbage and water pollution introduced from neighboring areas. All four settlements had numerous low-cost houses (hereafter referred to as main houses) with informal dwellings made of temporary building materials in the back yard (hereafter referred to as shacks). A legacy of the previous spatial disparities in the city resulted in communities with predominantly only one ethnic group. There were three settlements with predominantly black inhabitants and one settlement with predominantly coloured (mixed ancestry) inhabitants in the survey. This selection was representative of the overall demographic profile of the settlements in the city.
Structured Interview Questionnaires
Data were collected by means of structured interview questionnaires during home visits to all selected dwellings by the senior author, assisted by a registered nurse who spoke all three languages prevalent in the area. All dwellings on a selected plot (main house and shack(s) in the back yard) were included but recorded separately. Overall, 321 dwellings on 165 plots were selected for participation in the study. A systematic random sampling procedure was used to select the plots in the four study sites. Data were obtained from 1,020 persons in total with a response rate of 100%.
The questionnaires were piloted in two different settlements (predominantly coloured and predominantly black) in the CCTM. The pilot study sites were situated in Mfuleni and Westbank. The survey was administered to 15 dwellings with data obtained from 60 persons. The results from the pilot sites met the same criteria as the study sites. No problems or confusing questions were encountered and these interviews were carried out under the same conditions as the main study. The data from the dwellings in these pilot sites were therefore included in the total group, i.e. 1,080 participants living in 336 dwellings (173 main houses and 163 shacks).
The questionnaire was designed to record data from all dwellings on a plot. These questionnaires were administered in the language of preference during an on-site interview with the head of the household. The questionnaire comprised sections on demographics, health, and home ownership as well as a section to note the condition of the sanitation infrastructure (tap, toilet, waste disposal, etc.) and the condition of the dwelling and its surrounding yard. All toilets were inspected and noted as non-functional if the toilet was blocked, could not flush, or showed serious leaks or had a badly cracked cistern or bowl. Home ownership included questions formulated specifically for the main house and the shack.
Characterization of Demographic and Housing-Related Factors
Demographic and socioeconomic variables included age, gender, physical handicaps, educational attainment, citizenship, social grant recipients, employment status, and household monthly income. No questions or annotations on race were included in the questionnaire. The household monthly income was arrived at by the interviewed persons adding the income of all employed members of their dwellings. Health variables included HIV and tuberculosis (TB) status (voluntary), as well as ailments suffered in the two weeks preceding the survey. Home attainment and ownership in the main houses and backyard shacks, rental paid and operational costs incurred by these previously disadvantaged inhabitants were explored.
Statistical Analysis
Data were recorded in a database created in Statistica version 9.0 (StatSoft Inc. 2009, USA). Descriptive statistics, mainly means and standard deviations for continuous variables and frequency distributions for categorical variables, were computed. Bivariate analysis testing for differences in proportions of main houses and backyard shacks were performed using the test for probability values.
Results
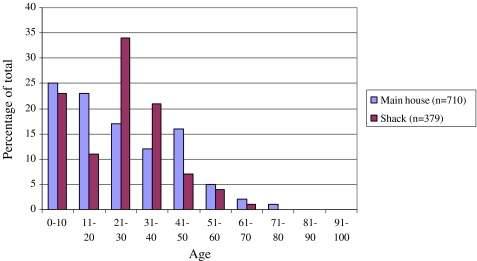
The age distribution (Figure 1) of household members indicated a young population (43% younger than 20 years) with a mean age of 25 years. The age of inhabitants of the main houses did not differ significantly from the occupants of the shacks (Mann–Whitney U test, p = 0.69). The occupancy of people living in a main house ranged between one and 12 persons per dwelling, and in shacks between one and 13 persons per dwelling (means reported in Table 1), giving a significantly greater occupancy rate in the main houses (Mann–Whitney test, p < 0.01). According to the number of occupants per square meter however, the backyard shacks were significantly more densely occupied (Table 1).
FIGURE 1.
Comparison of age of inhabitants in main house (mean age 25.02 ± 17.33 years) and shack (mean age 24.5 ± 14.28 years)
Table 1.
Sociodemographic characteristics of the study population
| Characteristic | Main house | Percentagea | Shack | Percentagea | Total group | Percentagea | p value |
|---|---|---|---|---|---|---|---|
| Study population | 710 | 65.7 | 370 | 34.3 | 1,080 | 100 | |
| Gender | |||||||
| Male | 322 | 29.8 | 184 | 17.1 | 506 | 46.9 | 0.17 |
| Female | 388 | 35.9 | 186 | 17.2 | 574 | 53.1 | |
| Female-headed households | 92 | 8.5 | 11 | 1.0 | 103 | 9.5 | <0.01 |
| Disabled individuals | 18 | 1.7 | 2 | 0.2 | 20 | 1.9 | <0.01 |
| Nationality | |||||||
| South Africans | 695 | 64.4 | 329 | 30.5 | 1,024 | 94.9 | <0.01 |
| Non-South Africans | 18 | 1.7 | 38 | 3.5 | 56 | 5.2 | |
| Highest education level | |||||||
| No schooling | 103 | 9.5 | 73 | 6.8 | 176 | 16.3 | <0.01 |
| Grade 0–4 | 152 | 14.1 | 32 | 3.0 | 184 | 17.1 | |
| Grade 5–7 | 154 | 14.3 | 65 | 6.0 | 219 | 20.3 | |
| Grade 8–10 | 138 | 12.8 | 90 | 8.3 | 228 | 21.1 | |
| Grade 9–12 | 158 | 14.6 | 100 | 9.3 | 258 | 23.9 | |
| Tertiary level | 5 | 0.5 | 10 | 0.9 | 15 | 1.4 | |
| Mean occupancy (persons per dwelling) | 4.1 | – | 2.3 | – | 3.2 | – | <0.01 |
| Density—mean number of persons per 10 m2 | 1.1 | – | 2 | – | 1.95 | – | <0.01 |
aAll percentages calculated from the total group (n = 1,080)
The possession of a main house by any person other than a South African citizen is not in accordance with the regulations, yet four main houses were occupied by non-South Africans. According to Table 1, the number of non-South African citizens occupying shacks was significantly higher than those occupying main houses. The shack rental market fulfils this housing need among non-South Africans.
When analyzing the total distribution of education categories as included in the survey, the educational level attained by the inhabitants of the main houses was significantly lower than that of the shack dwellers (Table 1). Of all the adults in the total group, 8% were illiterate or functionally illiterate (defined as schooling up to grade 4), and 22% have only a primary school education (defined as schooling up to and including grade 7).
The high level of unemployment is reflected in the low percentage of respondents in the survey who were employed full time (Table 2). When analysed over all categories of employment status and income, the occupants of the shacks reported a significantly higher income than those living in main houses (Table 2). The modal income group was R1,200–2,500 per household (US$160–333) with almost half of the total group having a monthly household income that is below the official South African poverty line of R322 (US$43) per person per month.9 The survey only included a question on the total household income and no information was available on individual income.
Table 2.
Aspects of economic status of the study population per dwelling type
| Characteristic | Main house (n = 173 dwellings) | Percentage | Shack (n = 163 dwellings) | Percentage | Total group (n = 336 dwellings) | Percentage | p value |
|---|---|---|---|---|---|---|---|
| Employment status | |||||||
| Full time | 122 | 11.3 | 76 | 7.0 | 198 | 18.3 | <0.01* |
| Part time | 8 | 0.8 | 33 | 3.0 | 41 | 4.8 | |
| Irregular | 50 | 4.6 | 32 | 3.0 | 82 | 7.6 | |
| Unemployed | 210 | 19.4 | 112 | 10.4 | 322 | 29.8 | |
| Pensioner | 14 | 1.3 | 13 | 1.2 | 27 | 2.5 | |
| Child at home | 104 | 9.6 | 66 | 6.1 | 170 | 15.7 | |
| Scholar | 202 | 18.7 | 38 | 3.5 | 240 | 22.2 | |
| Household monthly income | |||||||
| <R600 | 25 | 7.4 | 27 | 8.1 | 52 | 15.5 | <0.01* |
| R600–R1,200 | 29 | 8.6 | 59 | 17.6 | 88 | 26.2 | |
| R1,200–R2,500 | 58 | 17.3 | 52 | 15.4 | 110 | 32.7 | |
| >R2,500 | 23 | 6.8 | 60 | 17.9 | 83 | 24.7 | |
| Unsure | 1 | 0.3 | 2 | 0.6 | 3 | 0.9 | |
| Households living below South African poverty line (R322 per month) | 114 | 33.9 | 40 | 11.9 | 154 | 45.8 | <0.01* |
| Households receiving a social grant | 93 | 27.7 | 66 | 19.6 | 159 | 47.3 | <0.01* |
*Significant difference between respective characteristic and dwelling type
Again in keeping with the finding that the shack dwellers had a higher mean income than the inhabitants of the main houses, the number of main house families receiving an income grant was significantly higher than those in the shacks (Table 2).
Almost 49% of the main houses had a toilet inside the house and all toilets were water-borne. The rest of the houses had a toilet adjacent to the building. No shacks had toilets or taps inside. During the data gathering, it was observed that 59% of the toilets were not in working order. Blocked or overflowing drains were commonly observed (64% of dwellings had pools of drain water outside the house) while the state of the yard was noted as poor and rubbish-strewn in 49% of cases. The number of persons per toilet ranged from two persons to 18 persons.
Diarrhea occurring in the preceding two weeks was reported by 153 persons in the total survey, living in 70 main houses (40.5% of main houses) and 38 shacks (23.3% of shacks). There was a significant difference (chi-square test, p value <0.01) between the number of diarrheal cases of participants living in the main houses and shacks, but not a significant difference between the two housing types when comparing the number of cases (Table 3).
Table 3.
Reported health aspects of participants separated into dwelling types
| Health condition | Main house (n = 710) | Percentage | Shack (n = 370) | Percentage | Total group (n = 1,080) | Percentage | Odds ratio (95% CI) |
|---|---|---|---|---|---|---|---|
| Diarrheaa | 96 | 8.9 | 57 | 5.3 | 153 | 14.2 | 1.16 (0.82–1.66) |
| Diarrhea in femalesb | 54 | 56.3 | 25 | 43.8 | 79 | 51.6 | 1.04 (0.63–1.73) |
| Diarrhea in children <10 yearsb | 31 | 32.2 | 19 | 33.3 | 50 | 32.6 | 1.73 (0.95–3.13) |
| TB positive personsa | 24 | 2.2 | 14 | 1.3 | 38 | 3.5 | 1.12 (0.57–2.20) |
| HIV positive personsa | 8 | 0.7 | 10 | 0.9 | 18 | 1.7 | 3.45 (1.51–7.89) |
aCalculated from the total group (n = 1,080)
bCalculated from total number of diarrhea cases per dwelling type
Significantly more cases (38 cases) of self-reported TB occurred in main houses than in shacks (Table 3) with 21 being female. One of the TB cases reported being diagnosed as multi-drug resistant (MDR) TB. Of the 18 cases reported being HIV positive, 11 were female. There were 12 cases reported being both HIV and TB positive, of which eight were female. All medication in the household was inspected by the survey nurse and no TB or antiretroviral medication in the entire survey was found amongst them.
There was no significant difference in the number of main households reporting eating only one meal a day when compared to the shack dwellers (odds ratio 1.96 95% confidence interval 0.78–4.92). There was no significant difference in the numbers of main and shack households reporting one or more members using drugs (Table 4, odds ratio 1.24, 95% confidence interval 0.64–2.38). Half of the households in the total group had one or more smokers living there, while almost two thirds of the total group had one or more members consuming alcohol. All other diagnoses of illnesses (16 symptoms) were reported in low numbers. This does not imply that the participants in the survey suffered from very few illnesses, but merely very few had their illnesses diagnosed at their local clinic.
Table 4.
Meal frequency and substance usage per dwelling type
| Main house (n = 173) | Percentagea | Shack (n = 163) | Percentagea | Total group (n = 336) | Percentagea | Odds ratio (95% CI) | |
|---|---|---|---|---|---|---|---|
| 1 meal per day | 14 | 4.2 | 7 | 2.1 | 21 | 6.3 | 1.96 (0.78–4.92) |
| 2 meals per day | 36 | 10.7 | 26 | 7.7 | 62 | 18.4 | 1.38 (0.79–2.41) |
| Substance use | |||||||
| Smoke cigarettes | 89 | 26.5 | 80 | 23.8 | 169 | 50.3 | 1.10 (0.72–`1.69) |
| Consume alcohol | 106 | 31.5 | 110 | 32.7 | 216 | 64.2 | 1.31 (0.84–2.05) |
| Had a member using drugsb | 23 | 6.8 | 18 | 5.4 | 41 | 12.2 | 1.24 (0.64–2.38) |
aPercentage calculated out of total dwellings (n = 336)
bThe nature of the drugs were not explored
Some qualitative results noted during the data gathering included participants’ responses to problems in keeping their homes clean and repaired, as well as an inspection of sanitation facilities (tap, toilet, waste disposal, etc.) in all homes. The lack of education among adults in the study contributed to the homeowners’ lack of knowledge on how to keep up their new home. This lack of knowing how to keep their homes clean and how to fix broken infrastructure were strongly verbally communicated by the respondents. In addition, their acquisition of an improved home was not accompanied by an improvement in employment status and that resulted in many being unable to afford the repairs or the cleaning materials required to keep the homes clean. Within a short space of time, the sanitation facilities in their new home fell into a state of disrepair and were left uncleaned because of lack of both awareness and resources.
Discussion
Very few studies have described the phenomenon of informal housing (so-called shack in the backyard) interspersed within low-cost housing settlements, particularly with a focus on health. The participants in the present survey living in state-sponsored housing schemes reflect an epidemiologically young population. There is a virtual absence of aged persons in the survey. There is consequently a lack of role models in these urban environments contributing to the disintegration of the social fabric of these communities. McMichael10 argues that “urbanism, increased mobility and relaxation of traditional cultural norms yield new patterns of human behaviour, which includes changes in sexual behaviour and the use of illicit drugs.”
The high unemployment in these communities prevents the inhabitants from fulfilling their potential. These communities are impoverished and there is significant employment insecurity. The average household income of both the main house and shack reflects this economic reality. There were a large number of families with only one female breadwinner. One consequence of this adverse economic situation is that many families are living below the poverty line. This is compounded by the 25% of families who reported eating fewer than three meals a day. “Poor socio-economic status is linked to deficiencies in prenatal and early nutrition as malnourished children develop differently, have lower educational achievement and are more likely to live a poorer quality of life compared with children who received proper nutrition.”11 The lack of nutrition adds significantly to the vulnerability of this population to infectious disease pressure which is worsened by their dirty environment. A study undertaken by Bomela12 confirmed that “stunting or chronic malnutrition is the most prevalent amongst children under 5 years of age in South Africa (25%), much fewer though when compared to other developing countries such as Mozambique (41%), Angola (45%) and Lesotho (46%).”
The low level of education and lack of basic hygiene practiced by the inhabitants of government-subsidized housing will have to be taken into account when future housing schemes are designed. Education campaigns designed to improve the cleanliness of their homes and surroundings should reflect these realities faced by low-income inhabitants of government-subsidized housing.
There were a high proportion of households reporting alcohol, tobacco or drug use. Use of these substances would have impacted negatively on the already constrained household income. The “crowding out effect” of such expenditure on the already scant household budget in poor areas had also been reported by Thomson et al.13
The survey revealed crowding, more so in the case of the backyard shacks, which were of necessity much smaller. Crowded living conditions have been associated with increased infectious disease transmission, spread by the respiratory route, such as tuberculosis, rheumatic fever,14 and meningococcal disease.15 The majority of self-reported TB cases in this survey were female, while the majority of persons who reported having both TB and HIV were also female. The occurrence of at least one MDR-TB case is of special concern, given the poverty, crowding, and poor nutrition prevailing in these communities.
All the inhabitants on a particular plot had to use the only toilet on the property which was in or just outside the main house. This high rate of usage and resultant broken infrastructure and blocked or overflowing drains explains the poor state of sanitation encountered in this survey. This increased the health risks to individuals in these communities due to infectious disease pressure and environmental pollution. This partly counteracted the supposed increase in living standards of those families fortunate enough to receive a low-cost house.
The number of persons who reported one or more attacks of diarrhea over the two weeks preceding the survey comprised 14%, while 4.6% were children less than 10 years of age. Diarrhoea affected more than a third of the total dwellings. We observed that diarrhoea occurred more frequently in the main house (where the toilet is located) when compared to the shacks. In a survey carried out during 2001 in an informal settlement in Kayamandi outside the nearby town of Stellenbosch, the number of cases of diarrhoea during the month preceding the survey was reported to be 13.1%.16 The diarrhoea prevalence found in the present study was also comparable to that reported by D’Souza17 where in the two-week period before a cross-sectional study in Karachi, prevalence of diarrhoea was 14.4%. These results indicate that children under 10 years are at additional risk because of poor environmental conditions.
People living in poor areas often lack preventative health care or the means to manage chronic diseases.18 All of the respondents who admitted having HIV or TB were diagnosed at a healthcare facility. During an inspection of the medication in each dwelling, no antiretroviral drugs or TB medication was encountered. While some of the persons diagnosed with TB may have been enrolled in a directly observed treatment strategy programme at their nearest clinic, none of these cases reported visiting a clinic in the past two weeks. This has serious implications for the management of the disease which introduced additional risks to other inhabitants sharing the house. In the present study, one case of MDR-TB was reported from a study population of 1,080 persons. Should this proportion prevail in the rest of these low-cost housing communities, that would translate into 93 cases per 100,000 people living in such communities in the City of Cape Town. The risk of MDR-TB (a communicable disease that is difficult to control)19 spreading in low-cost housing communities should be addressed by much more active community intervention than is the case at present.
The escalation in number of shacks within low-cost housing communities resulted in a huge increase in population density (1.95 persons per 10 m2 living space), which was above the numbers used during the planning of these housing schemes. This placed municipal infrastructure under significant strain. The resultant breakdown in infrastructure (blocked drains, dispersal of sewage and contaminated storm water, flooding, etc.) caused widespread environmental damage and increased infection risk. These home owners do not have the finances to maintain their homes, placing them under a greater risk for disease, as lack of income and poverty is the most consistent predictor of disease and premature death.10,19
Comparisons on various indicators of health between inhabitants of the main houses and the shacks in the back yard yielded very few significant differences. The income of the shack dwellers was significantly higher, but that could be explained by the fact that they had to rent their shacks while the main house owners acquired their houses for free. Although there were more persons aged between 21 and 40 years of age living in shacks, the overall age distributions did not differ significantly. This lack of difference in important health characteristics implies that the acquisition of an improved dwelling with more space and supposed better sanitation did not translate into improved health for the inhabitants of those houses when compared to the shack dwellers in the back yard. Degrading the aims of low-cost housing programs by allowing backyard overcrowding is an important factor to keep in mind when assessing the health improvements associated with re-housing of the urban poor. There is a dearth of studies investigating this dynamic and the present study aimed to illustrate that the supposed improvements in health brought about by improved housing did not materialize under these conditions.
The reality of large numbers of persons housed in informal dwellings side-by-side with the state-subsidized low-cost houses cannot be legislated away at this late stage since the problem is so widespread. The laws of the country place the onus on any municipality who evicts these inhabitants to find alternative accommodation for them—an impossible task. The planning of urban design and service delivery in these settlements however need to be far more cognizant of the particular challenges and needs arising from these communities. Attention is at present focussed solely on the population who are not yet rehoused, but the inhabitants housed in these low-cost settlements are not by any means properly catered for regarding sanitation, health, and living conditions. These communities ought not to be written off as “taken care of” by the authorities.
Low-cost housing programs in South Africa has been highly cost-inefficient and the present policies driving these initiatives are giving rise to significant numbers of low income strata of the population experiencing threats to their health. Thus, the underlying assumption that improved housing will result in improved health has been subverted by allowing the new recipients of improved housing to bring slum conditions with them—quite literally in their own backyards.
Acknowledgements
We thank the Harry Crossley Foundation, the German Academic Exchange Service (DAAD), the National Research Foundation, and Stellenbosch University for the funding of this project, Sister N. Lethuka for help in administering the survey, and Professor M. Kidd from the Centre for Statistical Consultation at Stellenbosch University for statistical support.
Contributor Information
Thashlin Govender, Phone: +27-83-7302846, FAX: +27-21-9389166, Email: govender.thashlin@gmail.com.
Jo M. Barnes, Email: jb4@sun.ac.za
Clarissa H. Pieper, Email: clarissa.pieper@uct.ac.za
References
- 1.United Nations Human Settlement Programme (UN-HABITAT). The Challenge of Slums. Global Report on Human Settlements. London: Earthscan Publications Limited; 2003. http://www.unhabitat.org/downloads/docs/GRHS.2003.0.pdf. Accessed June 4, 2009.
- 2.Erguden S. Low-cost housing: policies and constraints in developing countries. Paper presented at: International Conference on Spatial Information for Sustainable Development; October 2–5, 2001; Nairobi, Kenya. http://www.fig.net/pub/proceedings/nairobi/erguden-CMTS1-1.pdf. Accessed February 7, 2010.
- 3.Ndegwa D, Horner D, Easu F. The links between migration, poverty and health: evidence from Khayelitsha and Mitchell’s plain. Soc Indic Res. 2006;81:223–224. doi: 10.1007/s11205-006-9008-z. [DOI] [Google Scholar]
- 4.Satterthwaite D. Will most people live in cities? BMJ. 2000;321:1143–1145. doi: 10.1136/bmj.321.7269.1143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Rauh VA, Landrigan PJ, Claudio L. Housing and health: intersection of poverty and environmental exposures. Ann NY Acad Sci. 2008;1136:276–288. doi: 10.1196/annals.1425.032. [DOI] [PubMed] [Google Scholar]
- 6.Thomson H, Pettigrew M, Morrison D. Health effects of housing improvement: systematic review of intervention studies. BMJ. 2001;323:187–190. doi: 10.1136/bmj.323.7306.187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.World Medical Association. Declaration of Helsinki: Ethical Principles for Medical Research Involving Human Subjects. Geneva: World Medical Association; 2000. http://www.fda.gov/ohrms/dockets/dockets/06p0147/06p-0147-c000001-02-vol1.pdf. Accessed January 24, 2009.
- 8.Department of Health. Guidelines for Good Clinical Practice in the Conduct of Clinical Trials in Human Participants in South Africa. Pretoria, South Africa: Department of Health, 2000. http://www.doh.gov.za/docs/policy/trials/trials_01.html. Accessed October 3, 2009.
- 9.Statistics South Africa. Statistics South Africa Income and Expenditure of households 2005/06—Analysis of results. Report no. 01-00-01. Pretoria, South Africa: Statistics South Africa, 2008. http://www.statssa.gov.za/Publications/Report-01-00-01/Report-01-00-012005.pdf. Accessed November 13, 2009.
- 10.McMichael AJ. The urban environment and health in a world of increasing globalization: issues for developing countries. Bull World Health Organ. 2000;78:1117–1126. [PMC free article] [PubMed] [Google Scholar]
- 11.Mechanic D, Tanner J. Vulnerable people, groups and populations: societal view. Health Aff Millwood. 2007;26:1220–1230. doi: 10.1377/hlthaff.26.5.1220. [DOI] [PubMed] [Google Scholar]
- 12.Bomela N. Child nutritional status and household patterns in South Africa. AJFAND. 2007;16:1–18. Available at: http://www.ajfand.net/Issue16/PDFs/Bomela_2140.pdf. Accessed March 15, 2010.
- 13.Thomson GW, Wilson NA, O’Dea D, Reid PJ, Howden-Chapman P. Tobacco spending and children in low income households. Tob Control. 2002;11:372–375. doi: 10.1136/tc.11.4.372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Perry CB, Roberts JAF. Study of the variability and incidence of rheumatic heart disease within the city of Bristol. BMJ. 1937;2:154–158. doi: 10.1136/bmj.2.3994.154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Baker M, McNicholas A, Garrett N, Jones N, Stewart J, Koberstein V, et al. Household crowding a major risk factor for epidemic meningococcal disease in Auckland children. Pediatr Infect Dis J. 2000;19:983–990. doi: 10.1097/00006454-200010000-00009. [DOI] [PubMed] [Google Scholar]
- 16.Barnes JM. The impact of water pollution from formal and informal urban development’s along the Plankenbrug River on water quality and health risk [PhD thesis]. Western Cape, University of Stellenbosch; 2003.
- 17.D’Souza RM. Housing and environmental factors and their effects on the health of children in the slums of Karachi, Pakistan. J Biosoc Sci. 1997;29:271–281. doi: 10.1017/S002193209700271X. [DOI] [PubMed] [Google Scholar]
- 18.Kawachi I, Wamala S. Globalization and health. New York: Oxford University Press; 2007. pp. 122–137. [Google Scholar]
- 19.Connolly MA, Gayer M, Ryan MJ, Salama P, Spiegel P, Heymann DL. Communicable diseases in complex emergencies: impact and challenges. Lancet. 2004;364:1974–1983. doi: 10.1016/S0140-6736(04)17481-3. [DOI] [PubMed] [Google Scholar]